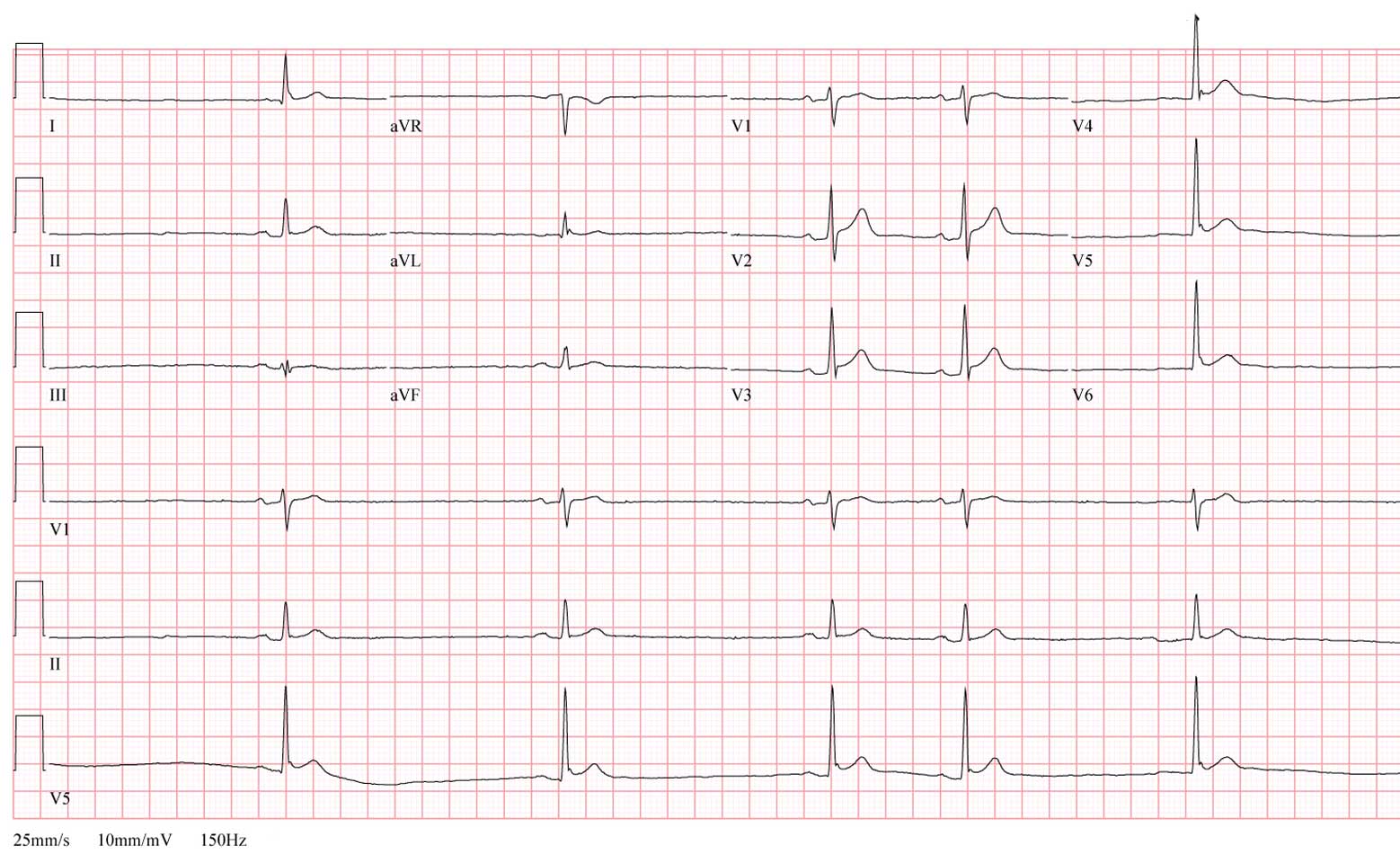
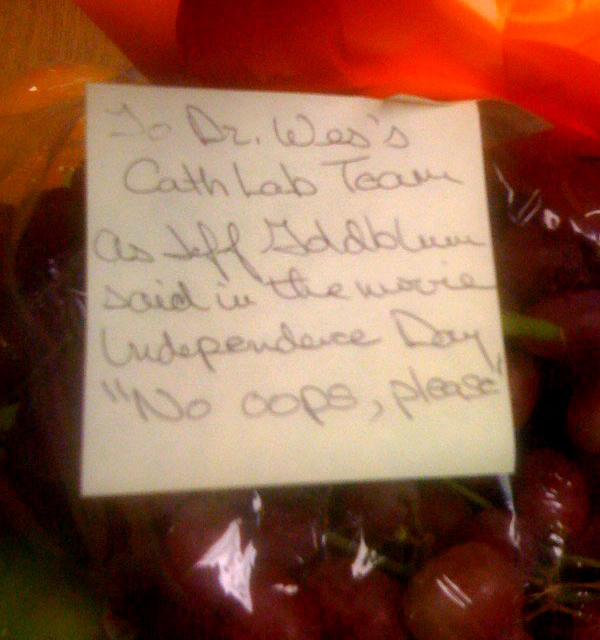
"Heart specialists on Monday filed suit against Secretary of Health and Human Services Kathleen Sebelius in an effort to stave off steep Medicare fee cuts for routine office-based procedures such as nuclear stress tests and echocardiograms.Perhaps other professional organizations will be forthcoming with similar suits as private doctors and their patients pay dearly for the reform efforts underway. Meanwhile hospitals continue to build. Pharmaceutical and medical device companies stocks rise. But did we really think the government's promise to find nearly $500 billion in "wasteful spending" from Medicare and Medicaid to resolve the fiscal realities of the ridiculously expensive legislative reform efforts could happen any other way?
The lawsuit, filed in U.S. District Court for the Southern District of Florida, charges that the government's planned cutbacks will deal a major blow to medical care in the USA, forcing thousands of cardiologists to shutter their offices, sell diagnostic equipment and work for hospitals, which charge more for the same procedures.
No doubt the suit will bring this issue to the forefront for patients. It will be interesting to see how this plays out. Perhaps a compromise. Perhaps a further delay.
But make no mistake. specialists are first in the sights of the health care reformers. They and their technology are the bad guys. They are expensive. Innovation is evil. And while the American College of Cardiology may have significant resources to fight this fight and have a legitimate gripe, the government's legal purse is infinite. Eventually, the ACC's finances will be worn thin.
And so all the great reform efforts underway, America will have "primary care" for most of its citizens lucky enough to find a primary care doctor and specialist care only for those living close enough to a hospital to receive it.
-Wes