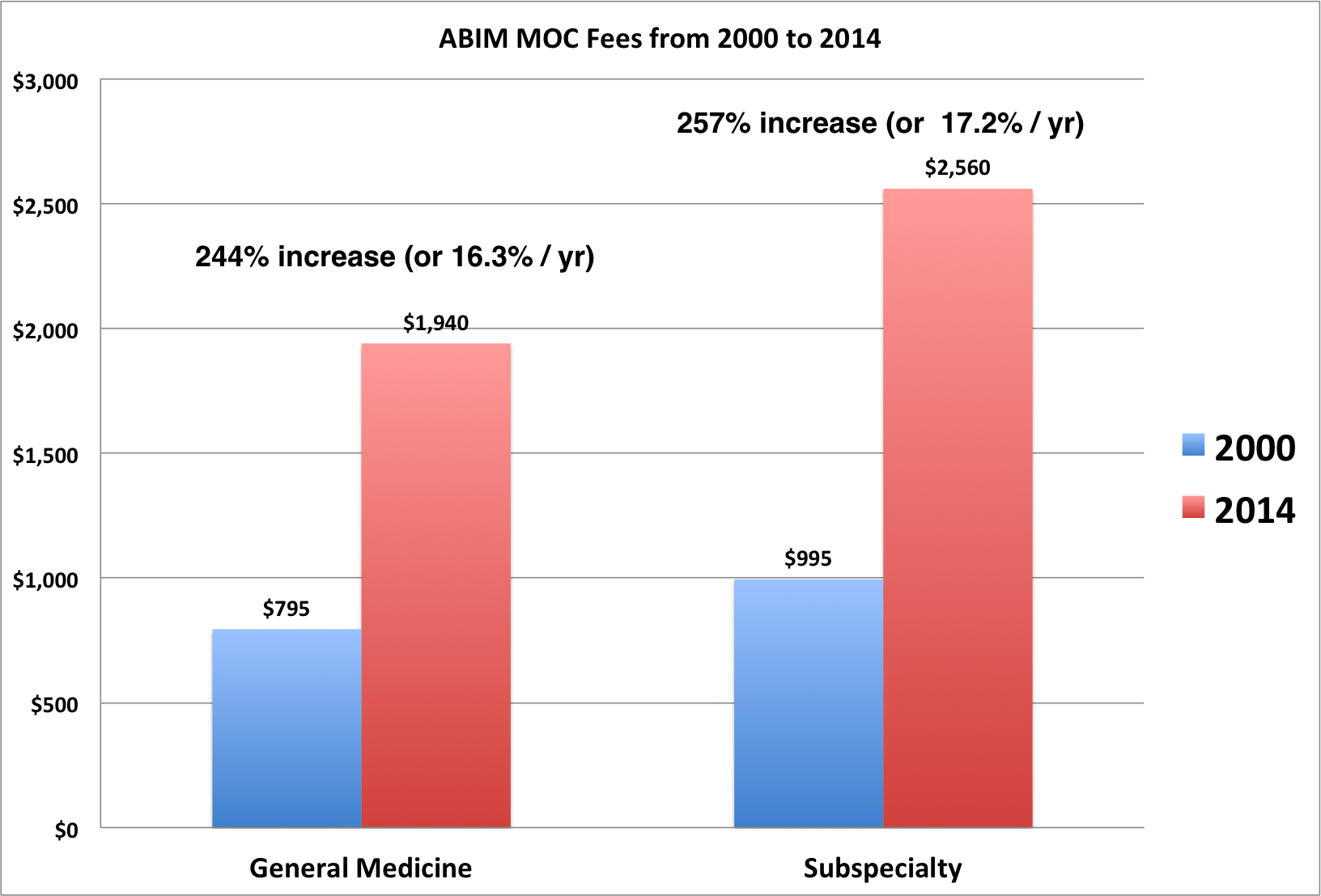
The incredible growth in American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) fees from 2000 to 2014 in one graph:
The growth of these fees far exceed the growth of inflation and the stock market over the same period of time.
-Wes
P.S.: The fee for certification by the ABIM in 1936 was $40. It cost $10 more to obtain your "certificate."
Sunday, September 27, 2015
Friday, September 25, 2015
ABIM First-Time MOC Pass Rates 2000-2014
I reviewed the past 15 years of first-time pass (and therefore failure) rates of the American Board of Internal Medicine (ABIM) MOC secure examination for every internal medicine subspecialty. Because of the work involved, I wanted to see if I could get these data published in a major peer-reviewed journal nearly two months ago to no avail.
I first submitted a manuscript with these data to the New England Journal of Medicine and it was rejected immediately before the manuscript even reached the peer review process. (I even gave the editor access to a password protected webpage containing the infographic you will see below). They weren't interested. (Perhaps because this is a retrospective review?)
I then submitted a slightly revised manuscript to JAMA. The after a preliminary review, the editor of JAMA would not submit my manuscript for peer review, but thought the work might warrant review as a 600-word "Research Letter to the Editor" that allowed only one figure and one table and no more than 6 references. Needless to say, nearly a month later, I just learned that my "research letter" was rejected by both JAMA and JAMA Internal Medicine. The reviewers comments were helpful should I ever decide to re-submit these data to a peer-reviewed journal again in a different format. However, given the many changes occuring to the ABMS MOC program recently, I felt time is of the essence and elected to proceed with publishing my data here on this blog. I feel these data are too important to sequester behind a medical journal paywall and encourage physicians to use these data to question the credibility and reproducibility of the American Board of Medical Specialties' (ABMS) MOC secure examination and the remainder of the MOC program as a requirement for maintaining hospital practice credentials. By publishing my data on this blog, I can publish ALL of the data I collected and collated, not just a tiny fraction of it. Also, I have found that this blog's reach is equal to or larger than many medical journals, particularly when a post contains important and credible information.
METHODS: The ABIM's first-time MOC pass rate data were gathered from current and prior archived ABIM web pages for each subspecialty between 2000 and 2014 using the Internet Archive Wayback Machine (https://archive.org/index.php). (Only the past 5-years of pass rate data were available for Hospital Medicine and 10-years of pass rate data were available for Interventional Cardiology because they were "newer" internal medicine subspecialties). The number of physicians failing their examination each year was then calculated by subtracting the product of the total number of physicians who took the examination by the published pass rate from the total number of physicians who took each subspecialty MOC examination. Linear regression trend lines of annual pass rates with their correlation coefficients over time were calculated for each subspecialty. Historical volatility of pass rates was calculated as the standard deviation of the data range of year-to-year percent change of pass rate. For example, published pass rates for General Internal Medicine from 2000-2014 were 89%, 92%, 91%, 85%, 86%, 84%, 79%, 83%, 92%, 90%, 88%, 87%, 84%, 78% and 80% respectively. The percent pass rate change from 2000 to 2001 was calculated as 0.92/0.89 - 1 = 3.37%. The 14-value dataset of percent pass rate annual changes for the years 2000-2014 therefore was 3.37%, -1.09%, -6.59%, 1.18%, -2.33%, -5.95%, 5.06%, 10.84%, -2.17%, 2.22%, -1.14%, -3.45%, -7.14%, 2.56%. The historical volatility of pass rate percent changes for General Internal Medicine equaled the standard deviation of this dataset, or 4.93.
RESULTS: First-time ABIM MOC pass rate trends (and the raw data for each internal medicine subspecialty's first time MOC pass rate) with their linear regression trend lines can be displayed using the interactive infographic below (just click the specialty circle to display the detailed annual pass/fail data):
The total number of physicians who took the test over 15 years and the percentage of physicians who failed their MOC exam on the first try are shown by subspecialty in the table below. Year-to-year historical volatility of pass rates by subspecialty also shown (bolded historical volatility values exceed one standard deviation from the mean of all subspecialty volatilities):
ABBREVIATED DISCUSSION:
A word of caution: the American Gastroenterological Association (AGA) has recently posted a video promising to bring an end to the MOC secure examination for gastroenterologists. Instead of ending the MOC program, however, (and after reviewing the full proposal about to be published in November) the AGA promises to replace MOC with an even more complicated "Continuous Professional Develppment" program "tailored to your needs" called "GAPP", the "Gastroenterologists Accountable Professionalism Pathway." This pathway promises to be an even more complicated 13-step program rather than MOC's 4-step program. It is a spin-off from the ABIM's similar "Continuous Professional Development" program used before by the ABIM that still has no proof of its value to patient care and without any disclosure of the cost this program for working physicians. It maintains the need to participate in their program for physicians to remain credentialed to practice medicine in their hospital. Before leaping for joy that the MOC examination is being phased out, realize that our specialty boards are reeling from the exposure of the financial reality of their "programs" to our health care programs and are creating new "programs" to assure ongoing financial and time-commitments from working physicians without proof that recertification is of any value to patient care over traditional self-directed Contining Medical Education. Worse yet: the AGA uses the term "Professionalism" in the title of their new re-certification proposal - a word defined via a "Task Force" of the corrupt ABIM Foundation.
Please feel free to share this post with interested journalists, friends, and colleagues. If you have further questions or ideas about these data, feel free to leave a comment or send me a note at wes - at - medtees dot com.
-Wes
I first submitted a manuscript with these data to the New England Journal of Medicine and it was rejected immediately before the manuscript even reached the peer review process. (I even gave the editor access to a password protected webpage containing the infographic you will see below). They weren't interested. (Perhaps because this is a retrospective review?)
I then submitted a slightly revised manuscript to JAMA. The after a preliminary review, the editor of JAMA would not submit my manuscript for peer review, but thought the work might warrant review as a 600-word "Research Letter to the Editor" that allowed only one figure and one table and no more than 6 references. Needless to say, nearly a month later, I just learned that my "research letter" was rejected by both JAMA and JAMA Internal Medicine. The reviewers comments were helpful should I ever decide to re-submit these data to a peer-reviewed journal again in a different format. However, given the many changes occuring to the ABMS MOC program recently, I felt time is of the essence and elected to proceed with publishing my data here on this blog. I feel these data are too important to sequester behind a medical journal paywall and encourage physicians to use these data to question the credibility and reproducibility of the American Board of Medical Specialties' (ABMS) MOC secure examination and the remainder of the MOC program as a requirement for maintaining hospital practice credentials. By publishing my data on this blog, I can publish ALL of the data I collected and collated, not just a tiny fraction of it. Also, I have found that this blog's reach is equal to or larger than many medical journals, particularly when a post contains important and credible information.
METHODS: The ABIM's first-time MOC pass rate data were gathered from current and prior archived ABIM web pages for each subspecialty between 2000 and 2014 using the Internet Archive Wayback Machine (https://archive.org/index.php). (Only the past 5-years of pass rate data were available for Hospital Medicine and 10-years of pass rate data were available for Interventional Cardiology because they were "newer" internal medicine subspecialties). The number of physicians failing their examination each year was then calculated by subtracting the product of the total number of physicians who took the examination by the published pass rate from the total number of physicians who took each subspecialty MOC examination. Linear regression trend lines of annual pass rates with their correlation coefficients over time were calculated for each subspecialty. Historical volatility of pass rates was calculated as the standard deviation of the data range of year-to-year percent change of pass rate. For example, published pass rates for General Internal Medicine from 2000-2014 were 89%, 92%, 91%, 85%, 86%, 84%, 79%, 83%, 92%, 90%, 88%, 87%, 84%, 78% and 80% respectively. The percent pass rate change from 2000 to 2001 was calculated as 0.92/0.89 - 1 = 3.37%. The 14-value dataset of percent pass rate annual changes for the years 2000-2014 therefore was 3.37%, -1.09%, -6.59%, 1.18%, -2.33%, -5.95%, 5.06%, 10.84%, -2.17%, 2.22%, -1.14%, -3.45%, -7.14%, 2.56%. The historical volatility of pass rate percent changes for General Internal Medicine equaled the standard deviation of this dataset, or 4.93.
RESULTS: First-time ABIM MOC pass rate trends (and the raw data for each internal medicine subspecialty's first time MOC pass rate) with their linear regression trend lines can be displayed using the interactive infographic below (just click the specialty circle to display the detailed annual pass/fail data):
The total number of physicians who took the test over 15 years and the percentage of physicians who failed their MOC exam on the first try are shown by subspecialty in the table below. Year-to-year historical volatility of pass rates by subspecialty also shown (bolded historical volatility values exceed one standard deviation from the mean of all subspecialty volatilities):
| Subspecialty | Physicians Undergoing MOC Examination (n) | Number of Physicians that failed MOC exam on their first attempt (%) | Pass Rate Historical Volatility (Minimum/Maximum annual percent pass rate change) |
|---|---|---|---|
| General Medicine | 61,050 | 9,212 (15.3%) | 4.93 (-7.14 / 10.84) |
| Cardiology | 10,486 | 1,386 (13.2%) | 3.23 (-3.53 / 6.10) |
| Cardiac Electrophysiology | 1,398 | 113 (8.1%) | 4.33 (-7.45 / 5.49) |
| Critical Care | 5,596 | 552 (9.9%) | 4.62 (-7.69 / 8.33) |
| Endocrine | 2,308 | 310 (13.5%) | 7.48 (-10.4 / 13.16) |
| Gastroenterology | 6,255 | 770 (12.3%) | 4.35 (-6.45 /4.71) |
| Geriatrics | 6,559 | 539 (8.2%) | 7.64 (-14.13 / 20.51) |
| Hematology | 2,427 | 338 (13.9%) | 7.11 (-9.76 / 13.51) |
| Hospital Medicine* | 829 | 113 (13.6%) | 1.09 (-2.27 / 0.00) |
| infectious Disease | 3,520 | 312 (8.9%) | 5.00 (-10.53 / 7.32) |
| Interventional Cardiology | 3,182 | 244 (7.7%) | 2.24 (-5.32 / 2.33) |
| Nephrology | 4,129 | 466 (11.3%) | 3.81 (-8.42 / 5.56) |
| Oncology | 4,568 | 456 (10.0%) | 3.87 (-8.79 / 6.90) |
| Pulmonary | 5,792 | 803 (13.9%) | 6.57 (-11.24 /13.92) |
| Rheumatology | 2,143 | 217 (10.1%) | 3.56 (-6.59 / 5.81) |
| TOTAL | 120,242 | 15,832 (13.2%) |
ABBREVIATED DISCUSSION:
- A very significant 15,832 physicians (13.2%) have failed their MOC secure examination on the first try. This has a significant impact on physician morale without justification and has affected patient access to their physician as a result.
- A large variation in year-to-year pass rates exists for many subspecialties, particularly Endocrinology, Geriatrics, Hematology, and Pulmonary suggesting inconsistent content, irrelevant content, and/or inconsistent setting of pass rate cut-offs year to year using the ABIM's modified Angoff method of determining pass rate cut-offs.
- First-time MOC failure rates vary by as much as 51% between subspecialties, with General Internal Medicine having the highest failure rate (15.3%) and Interventional Cardiology having the lowest (7.7%)
- Fourteen of 15 subspecialties had declining pass rate trends in this 15-year review of ABIM MOC pass rates (see infographic). Was this because the tested material is increasingly irrelevant to patient care? Or might there be another ulterior (financial?) motive for the decline? Or are most physicians simply unable to cram larger and larger amounts of information into their heads and regurgitate the proper answer in a limited time period thanks to the exponential growth of health care information over the last 15 years?
- Year-to-year first-time MOC pass rates could vary by as much as 20.5% (Geriatrics).
- The steepest pass rate decline was interventional cardiology (1.62% decline in pass rate per year), though low numbers of physicians took the exam the first several years it was offered.
- Since MOC participation is increasingly tied to hospital credentials as "board certification" became "time-limited" in 1990, what responsibility does the ABIM assume to patients when they fail a physician? How many physicians of each internal medicine subspecialty had to retake their examination (and how many times did each have to repeat)? What is the total cost to the doctor and the health care system for this unproven "quality" metric in terms of real dollars, patient access, and care delivery?
- Given the large number of physicians that have failed their MOC examination, why has the ABIM not studied the psychological, social, professional, and clinical impact their failure of physicians? Or don't they care?
A word of caution: the American Gastroenterological Association (AGA) has recently posted a video promising to bring an end to the MOC secure examination for gastroenterologists. Instead of ending the MOC program, however, (and after reviewing the full proposal about to be published in November) the AGA promises to replace MOC with an even more complicated "Continuous Professional Develppment" program "tailored to your needs" called "GAPP", the "Gastroenterologists Accountable Professionalism Pathway." This pathway promises to be an even more complicated 13-step program rather than MOC's 4-step program. It is a spin-off from the ABIM's similar "Continuous Professional Development" program used before by the ABIM that still has no proof of its value to patient care and without any disclosure of the cost this program for working physicians. It maintains the need to participate in their program for physicians to remain credentialed to practice medicine in their hospital. Before leaping for joy that the MOC examination is being phased out, realize that our specialty boards are reeling from the exposure of the financial reality of their "programs" to our health care programs and are creating new "programs" to assure ongoing financial and time-commitments from working physicians without proof that recertification is of any value to patient care over traditional self-directed Contining Medical Education. Worse yet: the AGA uses the term "Professionalism" in the title of their new re-certification proposal - a word defined via a "Task Force" of the corrupt ABIM Foundation.
Please feel free to share this post with interested journalists, friends, and colleagues. If you have further questions or ideas about these data, feel free to leave a comment or send me a note at wes - at - medtees dot com.
-Wes
Tuesday, September 15, 2015
Pulling the Plug on ABIM; Pulling the Plug on MOC
Kurt Eichenwald in Newsweek strikes again:
Then ask yourself the real question: why have all of us practicing physicians allowed the American Board of Specialties and it's 24 member boards (including the ABIM) to be unaccountable to us when we pay all the fees?
It is time to change that model and insist out specialty boards have elected officials and not act as a membership society.
It's also time to end the ABMS MOC program - every bit of it. It is hurting doctors and, in turn, hurting patients without any credible proof it improves patient care or quality. When will our professional organizations quit this insanity and return to physicians maintaining continuing medical education credits like before? No other country in the world wastes this much time and money on such an unproven metric.
Not one.
-Wes
Dr. Jones has been a physician for decades. His hundreds of online patient reviews are consistently positive, with an average of just under five stars and raves that he is caring and attentive. Based on those assessments, it’s clear he is the kind of physician who focuses on quality patient care and eases America’s critical shortage of internists.Read the whole thing.
Unfortunately, as a single father with a disabled child, Dr. Jones can’t manage his practice, care for his family and study for the certification exams administered by the American Board of Internal Medicine. The tests purportedly insure doctors’ competence, but, like many physicians, Dr. Jones says the questions often have nothing to with what he sees in his practice and are little more than a game of medical Trivial Pursuit. Dr. Jones can’t afford the thousands of dollars for study guides and classes to learn obscure, often irrelevant information, and has no time to review the material every night for months. He failed the test, so his hospital will no longer allow him to admit patients because he couldn’t answer questions about diseases he will never encounter.
And so, Dr. Jones—who asked me not to use his real name out of fear the ABIM will somehow block him from ever treating patients again—has closed his practice. The patients who love him will have to find someone else, and America’s shortage of primary care physicians has become just a little bit worse. “I’m hoping that maybe I can find a job as a high school science teacher,” he told me.
It’s a horror story that has played out for years throughout the U.S. as the ABIM abuses its monopoly power to force doctors to do whatever it decrees, while ignoring the many doctors who have demanded for years that independent researchers conduct comprehensive studies to determine if ABIM’s requirements do anything to improve patient care. This medical protection racket has made millionaires of ABIM top officers, financed a ritzy condominium, limousines, and first-class travel, all while sucking huge sums of cash out of the health care system.
But now, after decades of unchecked rule by ABIM, cracks are appearing in the organization’s facade of power. Thousands of doctors began a widespread revolt months ago and, in the last few weeks, evidence that their efforts are succeeding has started rolling in. ABIM officials have proclaimed that they are rushing to make changes—and indeed have announced some changes—but it seems they waited too long and are changing too little.
Then ask yourself the real question: why have all of us practicing physicians allowed the American Board of Specialties and it's 24 member boards (including the ABIM) to be unaccountable to us when we pay all the fees?
It is time to change that model and insist out specialty boards have elected officials and not act as a membership society.
It's also time to end the ABMS MOC program - every bit of it. It is hurting doctors and, in turn, hurting patients without any credible proof it improves patient care or quality. When will our professional organizations quit this insanity and return to physicians maintaining continuing medical education credits like before? No other country in the world wastes this much time and money on such an unproven metric.
Not one.
-Wes
Sunday, September 13, 2015
Maintenance of Certification's Real Problem: The Four Deceptions
By now, most specialty boards in medicine appear to have "heard" practicing doctors over their displeasure over the American Board of Medical Specialties' (ABMS) proprietary MOC® program. They understand. They agree with us. They want to play nice. Really. They know how much we really don't like that secure examination every ten years that makes sure about 10-15% of experienced physicians fail because, well, someone has to fail. They understand that the busywork created by the ABMS MOC® program is time-consuming, duplicitous, expensive and meaningless for assuring quality care. A few of them even acknowledged, by golly, that they got it wrong and promise to make things better by setting up new "design principles" for further MOC® development.
But our ABMS Specialty Boards really don't seem to get the big problem: fraud.
Instead, some keep asking doctors to cough up $2100 for "new and improved" exercises that excludes the old MOC® secure examination and replaces them with annual "mini-assessments."
Fortunately, there's a small group of specialty societies that want change, but appear a bit too nervous about ridding themselves of the term "MOC®." They include the American Gastroenterological Association, the American Association of Clinical Endocrinologists, the American College of Rheumatology, and (maybe) the Heart Rhythm Society (although this statement is a greatly toned down version of an earlier one).
But these Specialty Boards and professional organizations are relatively small fry compared to the much larger and richer specialty boards like the American College of Cardiology and the American College of Physicians who remain surprisingly quiet on the controversy.
"It's complicated," I'm told.
No, it's not.
The American Board of Medical Specialties (ABMS) has a problem. A big problem.
Their credibility bloom with practicing physicians is off the rose. Once an icon for assuring ethical, quality specialty medical education, the ABMS and their fellow member boards of the ACGME needed more. Much more. So they over-reached. They paid themselves handsomely despite the origins of the Specialty Boards being frugal. Almost without exception, the leadership of every ABMS specialty board has Presidents and CEOs that make far more income than their contemporary practicing colleagues - way more. They fly first class (or have until 2000), commonly have expensive dinners at the finest five-star hotels, some of which even overlook the Pacific Ocean, travel overseas to spread their regulatory gospel, all because they can. After all, they are special and they are unregulated. Meanwhile, residents and fellows making $50,000 a year are wondering where they'll come up with the $3000 or so it takes to become "certified" by the ABMS in their specialty.
The result? Practicing doctors don't trust our ABMS specialty boards any longer. Worse still, the more recent transgressions have prompted a look back at history, and history has shown the ABMS non-clinical specialty board leadership stumping for corporate interests for personal gain instead of stumping for patients' best interests. Is this what the Boards call "professionalism?" The ABMS member boards also continue to allow their Presidents and CEOs to lead their organizations far past the usual maximum one-, two- or three-year term limits of the original boards, all while these executives earn lavish salaries and benefits as they appoint new "Chairs" and "Directors" to make each organization seem "fresh."
The ABMS's largest member board also happens to be the American Board of Internal Medicine (ABIM).
The ABIM still has the sizable problem of their ABIM Foundation that no one wants to mention: that "secret society" without a credible public mission other than "to support the ABIM" when it was created in 1989. The only logical reason for its creation was to accumulate money from the pockets of practicing physicians to fund an investment portfolio created by the now defunct 1838 Investment Advisors (which were paid handsomely each year to do so). The ABIM leadership did very well using practicing physicians' money for this purpose, accumulating a bankroll of over $59 million without concern of IRS intervention. They also lied about their government lobbying activity that likely helped cement the ABMS MOC® program in the Affordable Care Act. Then, in what can only be considered (at best) an incredible lapse of judgment, they bought their infamous luxury condominium (complete with chauffeur) with some of their colleagues' testing fees they "granted" to the Foundation.
What a deal.
But it's hard to shelter that a profit motive for a non-profit from the IRS unless you have a plan, and who is smarter than the folks and lawyers at the ABIM?
First, for Deception #1, you have to file a request for tax-exempt status for your newly-created "American Board of Internal Medicine Foundation" with the IRS. Note that this was a very different name from the "ABIM Foundation" that was filed with the state of Pennsylvania in 1989. That way, the "American Board of Internal Medicine Foundation" never had too many dollars in its coffers to be tracked by the Internal Revenue Service (IRS).
Next, to avoid the tax consequences of accumulating a lot of money in a non-profit, you have to deflect. Unfortunately for the ABIM, changes in the IRS Form 990 made in 2008 required them to start reporting a "state of domicile." Deception #2: tell the IRS and the public (repeatedly until this year) on their Form 990 that the ABIM Foundation was domiciled in Iowa where no financial audit is required.
Then, when you realize your Foundation (that's supposed to be supporting the ABIM) has made a lot of cash covertly from the wallets of ABIM diplomats and investments, you magically perform Deception #3: ask the IRS to change the name of your "American Board of Internal Medicine Foundation" to the "ABIM Foundation" yet keep it 'domiciled' in Iowa. Oh, and be sure the "computer-generated notices" are "changed" and a new non-profit determination letter is re-issued in the new name because, gosh, they got it wrong when they first applied.
And guess what happens? The new ABIM Foundation magically has a boat-load of physician-supplied cash to give back to the ABIM (or their many cash-hungry friends who promise to spread the gospel of "Choose Wisely®") without an easily traceable trail because (as the ABIM Foundation website and their tax forms claimed) the ABIM Foundation really didn't exist (in the public or the IRS's eyes) before 1999!
Finally, it is very important to perform Deception #4: Make up a reason the ABIM Foundation was "created" in 1999 and delete the web page the stated the ABIM Foundation was "restructured" in 1999 as an operating Foundation to 'complement' the ABIM." Then be sure the reason for the "new" Foundation sounds really sincere - like "to advance the core values of medical professionalism to promote excellence in health care." (Forget to mention you created your own definition of "medical professionalism") Who could argue with such a "mission?" Also, make sure to create a Physician Charter of all your best bureaucratic and academic friends so they can join you at really nice venues to talk about things. Then make sure doctors "Choose Wisely®" treatments that they must forego in the name of "social justice." Once you've done all of these things, no one will ever know (or have time to suspect) where all that ABIM Foundation money came from.
It's a clever way to hide the money trail to the ABIM, it's officers and membership fees paid by the ABIM to the ABMS, don't you think?
(No wonder "it's complicated.")
Now, let's end the ABMS MOC® program entirely - every last bit of it - shall we?
That would be the truly professional thing to do and every ABMS specialty board today knows it.
-Wes
But our ABMS Specialty Boards really don't seem to get the big problem: fraud.
Instead, some keep asking doctors to cough up $2100 for "new and improved" exercises that excludes the old MOC® secure examination and replaces them with annual "mini-assessments."
Fortunately, there's a small group of specialty societies that want change, but appear a bit too nervous about ridding themselves of the term "MOC®." They include the American Gastroenterological Association, the American Association of Clinical Endocrinologists, the American College of Rheumatology, and (maybe) the Heart Rhythm Society (although this statement is a greatly toned down version of an earlier one).
But these Specialty Boards and professional organizations are relatively small fry compared to the much larger and richer specialty boards like the American College of Cardiology and the American College of Physicians who remain surprisingly quiet on the controversy.
"It's complicated," I'm told.
No, it's not.
***
The American Board of Medical Specialties (ABMS) has a problem. A big problem.
Their credibility bloom with practicing physicians is off the rose. Once an icon for assuring ethical, quality specialty medical education, the ABMS and their fellow member boards of the ACGME needed more. Much more. So they over-reached. They paid themselves handsomely despite the origins of the Specialty Boards being frugal. Almost without exception, the leadership of every ABMS specialty board has Presidents and CEOs that make far more income than their contemporary practicing colleagues - way more. They fly first class (or have until 2000), commonly have expensive dinners at the finest five-star hotels, some of which even overlook the Pacific Ocean, travel overseas to spread their regulatory gospel, all because they can. After all, they are special and they are unregulated. Meanwhile, residents and fellows making $50,000 a year are wondering where they'll come up with the $3000 or so it takes to become "certified" by the ABMS in their specialty.
The result? Practicing doctors don't trust our ABMS specialty boards any longer. Worse still, the more recent transgressions have prompted a look back at history, and history has shown the ABMS non-clinical specialty board leadership stumping for corporate interests for personal gain instead of stumping for patients' best interests. Is this what the Boards call "professionalism?" The ABMS member boards also continue to allow their Presidents and CEOs to lead their organizations far past the usual maximum one-, two- or three-year term limits of the original boards, all while these executives earn lavish salaries and benefits as they appoint new "Chairs" and "Directors" to make each organization seem "fresh."
The ABMS's largest member board also happens to be the American Board of Internal Medicine (ABIM).
The ABIM still has the sizable problem of their ABIM Foundation that no one wants to mention: that "secret society" without a credible public mission other than "to support the ABIM" when it was created in 1989. The only logical reason for its creation was to accumulate money from the pockets of practicing physicians to fund an investment portfolio created by the now defunct 1838 Investment Advisors (which were paid handsomely each year to do so). The ABIM leadership did very well using practicing physicians' money for this purpose, accumulating a bankroll of over $59 million without concern of IRS intervention. They also lied about their government lobbying activity that likely helped cement the ABMS MOC® program in the Affordable Care Act. Then, in what can only be considered (at best) an incredible lapse of judgment, they bought their infamous luxury condominium (complete with chauffeur) with some of their colleagues' testing fees they "granted" to the Foundation.
What a deal.
But it's hard to shelter that a profit motive for a non-profit from the IRS unless you have a plan, and who is smarter than the folks and lawyers at the ABIM?
First, for Deception #1, you have to file a request for tax-exempt status for your newly-created "American Board of Internal Medicine Foundation" with the IRS. Note that this was a very different name from the "ABIM Foundation" that was filed with the state of Pennsylvania in 1989. That way, the "American Board of Internal Medicine Foundation" never had too many dollars in its coffers to be tracked by the Internal Revenue Service (IRS).
Next, to avoid the tax consequences of accumulating a lot of money in a non-profit, you have to deflect. Unfortunately for the ABIM, changes in the IRS Form 990 made in 2008 required them to start reporting a "state of domicile." Deception #2: tell the IRS and the public (repeatedly until this year) on their Form 990 that the ABIM Foundation was domiciled in Iowa where no financial audit is required.
Then, when you realize your Foundation (that's supposed to be supporting the ABIM) has made a lot of cash covertly from the wallets of ABIM diplomats and investments, you magically perform Deception #3: ask the IRS to change the name of your "American Board of Internal Medicine Foundation" to the "ABIM Foundation" yet keep it 'domiciled' in Iowa. Oh, and be sure the "computer-generated notices" are "changed" and a new non-profit determination letter is re-issued in the new name because, gosh, they got it wrong when they first applied.
And guess what happens? The new ABIM Foundation magically has a boat-load of physician-supplied cash to give back to the ABIM (or their many cash-hungry friends who promise to spread the gospel of "Choose Wisely®") without an easily traceable trail because (as the ABIM Foundation website and their tax forms claimed) the ABIM Foundation really didn't exist (in the public or the IRS's eyes) before 1999!
Finally, it is very important to perform Deception #4: Make up a reason the ABIM Foundation was "created" in 1999 and delete the web page the stated the ABIM Foundation was "restructured" in 1999 as an operating Foundation to 'complement' the ABIM." Then be sure the reason for the "new" Foundation sounds really sincere - like "to advance the core values of medical professionalism to promote excellence in health care." (Forget to mention you created your own definition of "medical professionalism") Who could argue with such a "mission?" Also, make sure to create a Physician Charter of all your best bureaucratic and academic friends so they can join you at really nice venues to talk about things. Then make sure doctors "Choose Wisely®" treatments that they must forego in the name of "social justice." Once you've done all of these things, no one will ever know (or have time to suspect) where all that ABIM Foundation money came from.
It's a clever way to hide the money trail to the ABIM, it's officers and membership fees paid by the ABIM to the ABMS, don't you think?
(No wonder "it's complicated.")
Now, let's end the ABMS MOC® program entirely - every last bit of it - shall we?
That would be the truly professional thing to do and every ABMS specialty board today knows it.
-Wes
Wednesday, September 09, 2015
The ABIM and Big Tobacco - A Love Story
Some of us were shooting spitballs in class in 1963, more interested in the political machinations of the playground than we were with those affecting our future professions. But for those of us trying to understand now how the American Board of Internal Medicine (ABIM) and the American Board of Medical Specialties (ABMS) have run so far afield of representing the average working physician in America today, that is the time in history we have to return to.
It turns out ABIM colluded with Big Tobacco in 1963. Before then, its aims were more educational and helped to serve the public interest, that is until it climbed into bed with the likes of RJ Reynolds and Phillip Morris.
This morning, I woke to an anonymous blog contributor who offered the story of Dr. Thomas Brem, former Chair of the ABIM and President of the "Advisory Board of Medical Specialties" (our current ABMS) stumping for Big Tobacco. Included in the link is Dr. Brem's curriculum vitae. Turns out, Dr. Brem heard the siren song of stumping for profit-making companies on the basis that the "rate of increase" of cancer incidence that declined year after year despite mounds of evidence that the total incidence of lung cancer was increasing annually since the introduction of cigarette smoking.
So when it seems shocking that the ABIM got this far purchasing condos, lobbying Congress and filing false tax forms while hiding tax dollars, we should realize that the corruption in ABIM and the ABMS has been more than 50 years in the making.
But it's not how specialty boards started.
And it certainly is not how we have to continue.
-Wes
It turns out ABIM colluded with Big Tobacco in 1963. Before then, its aims were more educational and helped to serve the public interest, that is until it climbed into bed with the likes of RJ Reynolds and Phillip Morris.
This morning, I woke to an anonymous blog contributor who offered the story of Dr. Thomas Brem, former Chair of the ABIM and President of the "Advisory Board of Medical Specialties" (our current ABMS) stumping for Big Tobacco. Included in the link is Dr. Brem's curriculum vitae. Turns out, Dr. Brem heard the siren song of stumping for profit-making companies on the basis that the "rate of increase" of cancer incidence that declined year after year despite mounds of evidence that the total incidence of lung cancer was increasing annually since the introduction of cigarette smoking.
So when it seems shocking that the ABIM got this far purchasing condos, lobbying Congress and filing false tax forms while hiding tax dollars, we should realize that the corruption in ABIM and the ABMS has been more than 50 years in the making.
But it's not how specialty boards started.
And it certainly is not how we have to continue.
-Wes
Tuesday, September 08, 2015
Why the History of the Specialty Boards Is Important
According the American Board of Medical Specialties' website, the creation of the first medical specialty board was widely attributed to the ophthalmologist Derrick M. Vail, Sr., MD because of remarks he made in his presidential address to the American Academy of Ophthalmology and Otolaryngology (AAOO) in 1908. In 2012 while researching the origins of modern-day specialty boards, Denis O'Day and Mary Ladden from Vanderbilt in Nashville, TN performed a historical literary criticism of the ABMS's assertion that the ophthalmologist Derrick M. Vail, Sr., MD conceived of the specialty board system. By O'Day and Ladden's careful research, the true origin of specialty boards was likely created over a 12-year period by much of the work of ophthalmologist Edward M. Jackson, MD whose "Education for Ophthalmologic Practice" presidential address four years earlier at the AAOO meeting in 1904 sewed the seeds for board certification education system as we know it.
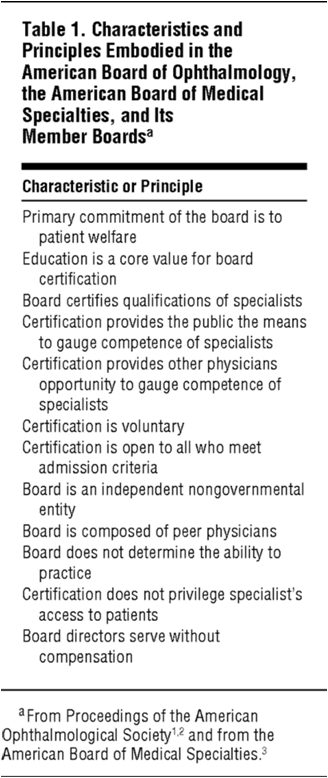
In their paper, O'Day and Ladden published the sentinel characteristics and principles embodied in the American Board of Ophthalmology (the "first" specialty board), the American Board of Medical Specialties, and its Member Boards:
Today, many of these founding characteristics and principles have been cast aside long ago, specifically, (1) the "Board does not determine the ability to practice" and (2) "Board directors serve without compensation", and (3) "Certification is voluntary."
For instance, with Maintenance of Certification (MOC), a trademarked product created by the ABMS, the program goes much further and is increasingly tied to hospital credentials and is now thoroughly incorporated into the new Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) ensconcing the program with the US government and will impact how physicians are paid after the law takes effect in 2019. So much for the ABMS principle of "not determining the (physician's) ability to practice" or keeping the ABMS "a non-governmental entity."
Also, the entire 24-member specialty board system of the ABMS is mired in large conflicts of interest created by their physician officers earning millions of dollars in compensation on the backs of working physicians. Only the National Board of Physicians and Surgeons (NBPAS.org) has unpaid board members for its recertification program created to compete with the AMBS MOC program, yet is still at its infancy of being accepted by hospitals in the United States.
Clearly, the original creators of specialty boards recognized the potential for conflicts of interest to arise when non-clinical physicians earned handsome incomes regulating their peers and worked to limit such conflicts. This is clearly not the case with the ABMS today.
As history reminds us, board certification was once performed to assure the proper education of specialty physicians, not to assure a money stream to the boards. "Re-certification," it seems, is little more than a means to subsidize the overpaid leadership of the ABMS and its member boards.
-Wes
P.S. Be sure to listen to Paul Tierstein, MD's NPR interview that aired yesterday for more on the origins of the NBPAS.
References:
History of the ABMS. ABMS.org website. Archived Jan 31, 1998. Available at: https://web.archive.org/web/19980131095657/http://www.abms.org/history.html
O’Day DM and Ladden MR. The Influence of Derrick T Vail Sr, MD, and Edward M. Jackson, MD, on the Creation of the American Board of Ophthalmology and the Specialist Board System in the United States. JAMA Ophthalmology Feb 2012 130(2): 224-232.
In their paper, O'Day and Ladden published the sentinel characteristics and principles embodied in the American Board of Ophthalmology (the "first" specialty board), the American Board of Medical Specialties, and its Member Boards:
 |
| (Click to enlarge) |
Today, many of these founding characteristics and principles have been cast aside long ago, specifically, (1) the "Board does not determine the ability to practice" and (2) "Board directors serve without compensation", and (3) "Certification is voluntary."
Clearly, the original creators of specialty boards recognized the potential for conflicts of interest to arise when non-clinical physicians earned handsome incomes regulating their peers and worked to limit such conflicts. This is clearly not the case with the ABMS today.
As history reminds us, board certification was once performed to assure the proper education of specialty physicians, not to assure a money stream to the boards. "Re-certification," it seems, is little more than a means to subsidize the overpaid leadership of the ABMS and its member boards.
-Wes
P.S. Be sure to listen to Paul Tierstein, MD's NPR interview that aired yesterday for more on the origins of the NBPAS.
References:
History of the ABMS. ABMS.org website. Archived Jan 31, 1998. Available at: https://web.archive.org/web/19980131095657/http://www.abms.org/history.html
Friday, September 04, 2015
The Unintended Consequences of Performance Measurement
When it rains, it pours.
So it is with the unintended consequences of performance measurement.
Performance measurement is an important part if our new health care law. The problem is, most of the people who wrote the law have no idea how to define "proper" performance or "quality" care. And when these bureaucrats and political minds attempt to apply individual health care principles to the arena of public health, they simply cannot perceive all of the unintended consequences their policies unleash in turn, especially when payments to physicians are tied to them.
Like a "V-8 head-slapping moment," two important articles have appeared this week, one by Lisa Rosenbaum, MD in the New England Journal of Medicine, and the other on Robert Centor, MD's blog. Each discusses the unintended consequence of performance measurement tied to medical payments: risk aversion.
Rosenbaum's article chronicles how New York's cardiothoracic surgical services are cherry-picking less complicated patients and pairing them with less experienced surgeons in the name of assuring better Medicare payments, and Centor's blog discusses his recent epiphany of the lack of proof of the benefits of performance measures but lots of examples of their unintended consequences.
Yet medicine is inherently risky, especially when caring for the complicated, critically ill, indigent, poor, and uneducated.
This same problem exists with the American Board of Medical Specialties' (ABMS) Utopian vision of improving physician performance by requiring them to perform their highly lucrative Maintenance of Certification re-examinations every six to ten years without EVER understanding the negative consequences of this mandate. No where has any member board of the ABMS ever studied the repercussions of their mandate upon practicing physicians and the patients they care for. Rather than acknowledging the reality that their MOC program is expensive and increasingly tied to physician's hospital credentials and can directly affect their employment, their member boards deflect and create new "design principles" that promise "shared purpose and impact first," to make patients "the North Star," "simplicity and relevancy," to "think internal and external," to "always include the WHY, HOW, and WHO," "to balance the community centered-design with ABIM's expertise and research," to promise "participation and not just communication," and transparent decisions."
I'm not sure I've ever heard such doublespeak to justify the unintended consequences of an unproven and potentially dangerous exercise that could do more harm than good to patient care.
Perhaps as these unintended consequences of performance measurement gain an understanding with patients and legislators, we'll see a change in our health care law that could really help reduce costs and help patient care:
... the dissolution of these needless, unproven, and expensive exercises in futility.
-Wes
So it is with the unintended consequences of performance measurement.
Performance measurement is an important part if our new health care law. The problem is, most of the people who wrote the law have no idea how to define "proper" performance or "quality" care. And when these bureaucrats and political minds attempt to apply individual health care principles to the arena of public health, they simply cannot perceive all of the unintended consequences their policies unleash in turn, especially when payments to physicians are tied to them.
Like a "V-8 head-slapping moment," two important articles have appeared this week, one by Lisa Rosenbaum, MD in the New England Journal of Medicine, and the other on Robert Centor, MD's blog. Each discusses the unintended consequence of performance measurement tied to medical payments: risk aversion.
Rosenbaum's article chronicles how New York's cardiothoracic surgical services are cherry-picking less complicated patients and pairing them with less experienced surgeons in the name of assuring better Medicare payments, and Centor's blog discusses his recent epiphany of the lack of proof of the benefits of performance measures but lots of examples of their unintended consequences.
Yet medicine is inherently risky, especially when caring for the complicated, critically ill, indigent, poor, and uneducated.
This same problem exists with the American Board of Medical Specialties' (ABMS) Utopian vision of improving physician performance by requiring them to perform their highly lucrative Maintenance of Certification re-examinations every six to ten years without EVER understanding the negative consequences of this mandate. No where has any member board of the ABMS ever studied the repercussions of their mandate upon practicing physicians and the patients they care for. Rather than acknowledging the reality that their MOC program is expensive and increasingly tied to physician's hospital credentials and can directly affect their employment, their member boards deflect and create new "design principles" that promise "shared purpose and impact first," to make patients "the North Star," "simplicity and relevancy," to "think internal and external," to "always include the WHY, HOW, and WHO," "to balance the community centered-design with ABIM's expertise and research," to promise "participation and not just communication," and transparent decisions."
I'm not sure I've ever heard such doublespeak to justify the unintended consequences of an unproven and potentially dangerous exercise that could do more harm than good to patient care.
Perhaps as these unintended consequences of performance measurement gain an understanding with patients and legislators, we'll see a change in our health care law that could really help reduce costs and help patient care:
... the dissolution of these needless, unproven, and expensive exercises in futility.
-Wes
Subscribe to:
Comments (Atom)