It figures. I head out of town and the cardiovascular news world erupts:
Dick Cheney gets a heart transplant
This was pretty predictable: after all, he's had every other known cardiovascular therapy known to man and had done remarkably well with all of them. I heard Mr. Cheney speak years ago when he gave the keynote address to the American College of Cardiology when I was indoctrinated as a Fellow in the College. He was a man profoundly affected by the cardiovascular disease, watching his father die at a young age following a massive myocardial infarction treated only with morphine sulfate. He, in contrast, repeatedly benefitted from the phenomenal innovation explosion within our field: he had successful bypass surgery on several occassions, treatment with an implantable cardiac defibrillator, left ventricular assist device - and now - transplant at the age of 71. Old? Certainly. Unheard of? Certainly not. How he'll fare through his last surgical ordeal, one fraught with the added challenges of immunosuppression, remains to be seen.
First-hand Account of the Department of Justice's Investigation on ICD Use Published
I had my say on this and the challenges doctors experience when seeing patients that fall outside of payment criteria for defibrillators but meet professional guideline requirments. (Managed to finalize my edits before boarding my plane!) But with this ongoing paradigm for medical device usage, I continue to wonder what recourse physicians will have when additional inconsistencies are noted between CMS coverage decisions and professional guidelines for all specialties in the years ahead.
Report of Deaths from St. Jude's Riata Lead are Published
I suppose this was really not that surprising, but what was surprising is that St. Jude did not come forth with these findings - only a post hoc analysis of the FDA's MAUDE database by the Robert Hauser, MD and his group from the Minnesota Heart Institute was again necessary. We also see the results of the Vanderbilt groups' fluoroscopic analysis of the Riata leads come to light as well. The implications for managing patients with these leads are significant, especially since the high voltage leads within the Riata lead appear to fail. Most are in agreement that routine extraction of these leads should be avoided. How to handle monitoring of the high voltage portion of these leads remains of concern. While doctors have gotten pretty good at handling these issues, there is no question that the Riata lead fiasco offers new challenges clinically.
So there you have it. My brief summary of the big cardiovascular stories for the past week. While I'm looking forward to re-entering the blog-o-sphere next week, I must say the break from the electronic world with my family has been VERY nice.
-Wes
Friday, March 30, 2012
Monday, March 26, 2012
When the Feds Come Knocking
Slightly over a year ago, the Department of Justice (DOJ) launched an investigation of a large number of institutions regarding concerns that implantable cardiac defibrillator (ICD) procedures were performed for reasons outside of the criteria set forth in Medicare’s National Coverage Decision (NCD). This investigation occurred just after Al-Khatib and others published a report January 4, 2011 in JAMA that suggested as many as 22.5% of implantable defibrillators implanted for primary prevention of sudden death were not evidence-based. While the physician community took issue with the Al-Khatib paper, the media firestorm it generated paired with the announcement to the Heart Rhythm Society physician community that a federal investigation was underway, had a chilling effect on ICD implantation nationwide. Drs. Jonathan S.Steinberg and Suneet Mittal report on their experience with DOJ investigators under this heavy regulatory oversight in today’s Journal of the American College of Cardiology.
Steinberg and Mittal's diplomatic account carefully describes the challenges of retrospective audits performed by lawyers from the Department of Justice and those of their targeted health care facilities. The DOJ identified 229 cases as potentially inappropriate cases based on Medicare code criteria. (This represented 8.7% of the de novo non-resynchronization ICD implants done for primary prevention at their institutions). After determining that some of these targeted cases were actually for secondary prevention or other coding transgressions, the authors could medically justify all but thirty-four (15%) (or a very low 1.5% of all ICD’s implanted for primary prevention of sudden death) at their institution. As has been the case in most reports, the majority of outside NCD-directed ICD implants occurred because of timing violations—too close to the diagnosis of heart failure, heart attack and coronary intervention. These timing constraints constitute the primary issue before implanting doctors: their professional society guidelines do not -- in all cases -- recognize similar timing restrictions.
It is surprising that we are not told what sanctions, if any, were levied against their respective institutions. Perhaps the authors felt this important detail was unimportant to disclose or perhaps they were prohibited from doing so. Perhaps their penalty is still being determined: after all, nothing drives behavior like fear. To this end, we found the authors' compliments of the government's legal team unusual to report in a scientific manuscript, as if the they were suffering from Stockholm Syndrome.
We should acknowledge that the authors have added much needed clarity to the gray area of decision-making surrounding ICD implantation. Their explanations of timing violations highlight problems with coding, confusion around incidental PCI intervention in patients with dilated cardiomyopathy, and demonstrate the overlap decisions that must be made when bradycardia and tachycardia functions might be required for our patients. This kind of clinically-relevant nuance was lacking in the impugnable Al-Khatib JAMA piece.
We can only speculate the large cost of the legal fees and man-hours devoted to this review process. We will never know how many patients died during, or now after, the course of this investigation because they were not offered ICDs because ICDs can only be offered to patients who meet Medicare’s rigid, outdated, and still-to-be-updated National Coverage Decision for implantable defibrillators. But perhaps this is the price of regulation thatAmerica
With this latest report, a new era for medical practice is now upon us – one where priorities of low cost care and high quantity of care determined by non-medical personnel supersede the highest quality of medical care to our patients. For regulators, it is easy to be a Monday-morning armchair quarterback evaluating health care delivery. It is far harder, however, to decide prospectively who is likely to die (or not) when they sit before you with a newly-diagnosed cardiomyopathy and ejection fraction of 12%.
When government and legal officials who carry no responsibility for the long-term well-being of our patients have the authority to retrospectively impugn and penalize doctors (and their health care facilities) based merely on retrospective reviews of billing codes and outdated payment mandates, they risk irrevocable harm to patients who might qualify for devices according to updated professional guidelines. Doctors everywhere should stand up collectively to disown the practice of using NCD mandates, rather than updated professional guidelines, to determine appropriate care for patients.
After all, our patients are depending on us.
Westby G. Fisher, MD
Director, Cardiac Electrophysiology
NorthShore University
Clinical Associate Professor of Medicine
PritzkerSchool Medicine University Chicago
Evanston IL
John Mandrola, MD
Cardiac Electrophysiologist
Baptist Medical Associates
Louisville , KY
Addendum 27 Mar 2012: Link to Steinberg/Mittal article finally added.
Addendum 14 Sep 2012: Update on the DOJ Decision
References:
Jonathan S. Steinberg and Suneet Mittal. "The Federal Audit of Implantable Cardioverter-Defibrillator Implants: Lessons Learned." J Am Coll Cardiol. April 3, 2012, 59 (14) 1270-4. doi: 10.1016/j.jacc.2011.12.026
Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. J Am Coll Cardiol. May 27, 2008;51(21):e1-62.
Al-Khatib S, Hellkamp A, Curtis J, et al. Non–Evidence-Based ICD Implantations in the United States JAMA. 2011;305(1):43-49. doi: 10.1001/jama.2010.1915
Note: This post also appears on Dr. John Mandrola's blog: http://www.drjohnm.org/
Steinberg and Mittal's diplomatic account carefully describes the challenges of retrospective audits performed by lawyers from the Department of Justice and those of their targeted health care facilities. The DOJ identified 229 cases as potentially inappropriate cases based on Medicare code criteria. (This represented 8.7% of the de novo non-resynchronization ICD implants done for primary prevention at their institutions). After determining that some of these targeted cases were actually for secondary prevention or other coding transgressions, the authors could medically justify all but thirty-four (15%) (or a very low 1.5% of all ICD’s implanted for primary prevention of sudden death) at their institution. As has been the case in most reports, the majority of outside NCD-directed ICD implants occurred because of timing violations—too close to the diagnosis of heart failure, heart attack and coronary intervention. These timing constraints constitute the primary issue before implanting doctors: their professional society guidelines do not -- in all cases -- recognize similar timing restrictions.
It is surprising that we are not told what sanctions, if any, were levied against their respective institutions. Perhaps the authors felt this important detail was unimportant to disclose or perhaps they were prohibited from doing so. Perhaps their penalty is still being determined: after all, nothing drives behavior like fear. To this end, we found the authors' compliments of the government's legal team unusual to report in a scientific manuscript, as if the they were suffering from Stockholm Syndrome.
We should acknowledge that the authors have added much needed clarity to the gray area of decision-making surrounding ICD implantation. Their explanations of timing violations highlight problems with coding, confusion around incidental PCI intervention in patients with dilated cardiomyopathy, and demonstrate the overlap decisions that must be made when bradycardia and tachycardia functions might be required for our patients. This kind of clinically-relevant nuance was lacking in the impugnable Al-Khatib JAMA piece.
We can only speculate the large cost of the legal fees and man-hours devoted to this review process. We will never know how many patients died during, or now after, the course of this investigation because they were not offered ICDs because ICDs can only be offered to patients who meet Medicare’s rigid, outdated, and still-to-be-updated National Coverage Decision for implantable defibrillators. But perhaps this is the price of regulation that
With this latest report, a new era for medical practice is now upon us – one where priorities of low cost care and high quantity of care determined by non-medical personnel supersede the highest quality of medical care to our patients. For regulators, it is easy to be a Monday-morning armchair quarterback evaluating health care delivery. It is far harder, however, to decide prospectively who is likely to die (or not) when they sit before you with a newly-diagnosed cardiomyopathy and ejection fraction of 12%.
When government and legal officials who carry no responsibility for the long-term well-being of our patients have the authority to retrospectively impugn and penalize doctors (and their health care facilities) based merely on retrospective reviews of billing codes and outdated payment mandates, they risk irrevocable harm to patients who might qualify for devices according to updated professional guidelines. Doctors everywhere should stand up collectively to disown the practice of using NCD mandates, rather than updated professional guidelines, to determine appropriate care for patients.
After all, our patients are depending on us.
Westby G. Fisher, MD
Director, Cardiac Electrophysiology
Clinical Associate Professor of Medicine
Pritzker
John Mandrola, MD
Cardiac Electrophysiologist
Baptist Medical Associates
Addendum 27 Mar 2012: Link to Steinberg/Mittal article finally added.
Addendum 14 Sep 2012: Update on the DOJ Decision
References:
Jonathan S. Steinberg and Suneet Mittal. "The Federal Audit of Implantable Cardioverter-Defibrillator Implants: Lessons Learned." J Am Coll Cardiol. April 3, 2012, 59 (14) 1270-4. doi: 10.1016/j.jacc.2011.12.026
Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. J Am Coll Cardiol. May 27, 2008;51(21):e1-62.
Al-Khatib S, Hellkamp A, Curtis J, et al. Non–Evidence-Based ICD Implantations in the United States JAMA. 2011;305(1):43-49. doi: 10.1001/jama.2010.1915
Note: This post also appears on Dr. John Mandrola's blog: http://www.drjohnm.org/
Labels:
CMS,
defibrillator,
DOJ,
guidelines,
ICD,
law,
lawyers,
Medicare
Sunday, March 25, 2012
A Cold Front Descends on ACC12
After a warm week of unusually warm weather in Chicago, a cool front descended on the city this weekend and in many ways, seemed to descend on the American College of Cardiology Scientific Sessions this year as well.
The mood seemed almost somber on Day 1. Perhaps it was the lack of Chicagoans attending the meeting because it was the start of Spring Break for many of the local schools in the area. Perhaps it was the lack of signage outside McCormick place as I drove up to the conference center from Lake Shore Drive (I had a brief moment of concern: "Are they holding the meeting somewhere else?") Strange. Or perhaps it was long walk from the parking lot to the conference center with dark, dank halls where your footsteps echoed off the barren walls and were the only ones heard. And finally, after reaching the registration area, the loss of the festive, colorful ads that used to adorn the skyway over Lakeshore Drive as we walked from the registration area to the main conference area. There were fewer doctors, fewer huddles where people used to welcome each other, fewer smiles. Even the expo hall where the vendors waited in earnest on their plush pile carpet to corner their unwary prey, there seemed to be too many of them and too few of us.
Things are changing at these big Scientific Meetings for doctors now. They used to be fun to attend: now you can see the collective sighs as you spoke with other doctors: the meetings have become more obligatory than anticipated for many. Get your CME's, pay the freight, and head home. Even a fellow from Wayne State's program cornered me at a post-conference event: "What's happening to us? Aren't doctors supposed to be important? I needed a pen, so I asked a vendor if I could have one of theirs that was displayed on their counter. They agreed, but not before scanning my name badge. Depressing."
Perhaps it's the internet, too. People wait online to see the news reports and news coverage. Happy doctors in pretty outfits get videoed and politely displayed online, ever eager to spew forth their opinions about the latest study. No shouting, please, that would be unpleasant. Smile! Then "5, 4, 3...." "That's a take!"
But this is not a reality show. It's real life. It's expensive. It's time-consuming. It's supposed to be a time to meet colleagues and friends and re-charge doctors engines before descending back into the mosh pit of patient care. It unsettling to see these changes compared to an earlier time.
But doctors understand that things are changing. We get that things should change. But it is discouraging to see the blatant focus on us as the bad guy in all that ailes our health care system. We are tracked with RFID tags, monitored for our use of twelve-cent pens, and for the new generation of doctors coming forward, wondering if there will even be a job waiting for us after all their exorbitantly expensive education. (Consolidation and contraction is already upon us in health care).
It's ironic: despite the real need for more doctors to enter health care as a profession, after my first day at the ACC meeting in Chicago, it seems we're doing everything possible to discourage our best and brightest from taking part in what was once considered our noble profession.
-Wes
The mood seemed almost somber on Day 1. Perhaps it was the lack of Chicagoans attending the meeting because it was the start of Spring Break for many of the local schools in the area. Perhaps it was the lack of signage outside McCormick place as I drove up to the conference center from Lake Shore Drive (I had a brief moment of concern: "Are they holding the meeting somewhere else?") Strange. Or perhaps it was long walk from the parking lot to the conference center with dark, dank halls where your footsteps echoed off the barren walls and were the only ones heard. And finally, after reaching the registration area, the loss of the festive, colorful ads that used to adorn the skyway over Lakeshore Drive as we walked from the registration area to the main conference area. There were fewer doctors, fewer huddles where people used to welcome each other, fewer smiles. Even the expo hall where the vendors waited in earnest on their plush pile carpet to corner their unwary prey, there seemed to be too many of them and too few of us.
Things are changing at these big Scientific Meetings for doctors now. They used to be fun to attend: now you can see the collective sighs as you spoke with other doctors: the meetings have become more obligatory than anticipated for many. Get your CME's, pay the freight, and head home. Even a fellow from Wayne State's program cornered me at a post-conference event: "What's happening to us? Aren't doctors supposed to be important? I needed a pen, so I asked a vendor if I could have one of theirs that was displayed on their counter. They agreed, but not before scanning my name badge. Depressing."
Perhaps it's the internet, too. People wait online to see the news reports and news coverage. Happy doctors in pretty outfits get videoed and politely displayed online, ever eager to spew forth their opinions about the latest study. No shouting, please, that would be unpleasant. Smile! Then "5, 4, 3...." "That's a take!"
But this is not a reality show. It's real life. It's expensive. It's time-consuming. It's supposed to be a time to meet colleagues and friends and re-charge doctors engines before descending back into the mosh pit of patient care. It unsettling to see these changes compared to an earlier time.
But doctors understand that things are changing. We get that things should change. But it is discouraging to see the blatant focus on us as the bad guy in all that ailes our health care system. We are tracked with RFID tags, monitored for our use of twelve-cent pens, and for the new generation of doctors coming forward, wondering if there will even be a job waiting for us after all their exorbitantly expensive education. (Consolidation and contraction is already upon us in health care).
It's ironic: despite the real need for more doctors to enter health care as a profession, after my first day at the ACC meeting in Chicago, it seems we're doing everything possible to discourage our best and brightest from taking part in what was once considered our noble profession.
-Wes
Saturday, March 24, 2012
The Risk of Avoiding Social Media: Others Get to Say Who You Are
If you want to let others say who you are, don't dive into social media. If you are too shy about the prospect, then don't complain when surveys like this are published:
Poor neurologists... They get slammed by a WebMD poll that only received a 10% response rate from physicians.
-Wes
PS: For those attending the American College of Cardiology Scientific Sessions in Chicago this weekend, I'll be speaking more about social media's roles for physicians TONIGHT (details here). Please feel free to join me.
Cardiologists, for the most part, drive Japanese cars, believe in a higher power, and are moderately savvy when it comes to social media. Those are just some of the pearls from a lifestyle survey of physicians conducted by Medscape and published online today.
Asked to rank their level of happiness outside of their work on a scale of 1 to 5, the 762 cardiologists who replied to the survey provided an average happiness score of 3.92. That puts them 15th out of the 25 specialties surveyed, where rheumatologists, dermatologists, and urologists were the happiest, with scores of 4.04 to 4.09, and neurologists were, it seems, the glummest about their nonworking lives, with scores of 3.88.
Poor neurologists... They get slammed by a WebMD poll that only received a 10% response rate from physicians.
-Wes
PS: For those attending the American College of Cardiology Scientific Sessions in Chicago this weekend, I'll be speaking more about social media's roles for physicians TONIGHT (details here). Please feel free to join me.
Wednesday, March 21, 2012
The Pavlovian Response to Social Media
My wife, a practicing clinical psychologist, made an interesting observation this morning, comparing me to a pigeon.
I guess I'm trying to reach a higher order of consciousness..
* sigh *
-Wes
"You talk with your wife, and it's not very pleasant. You text your kids and get no response. You even call the kids and still, they don't answer. And yet, you Twitter about the last time you blew your nose and get 10 responses and 4 'likes.'Now, wonder why I haven't been blogging as much lately?
Which behavior will be reinforced? Which behavior will increase in frequency? Everyone is receiving a stream of virtual pellets all day to help them cope with the exigencies of ordinary life. It's a sobering image.
But human beings aren't pigeons, right? Human beings are capable of higher order functioning, provided they are conscious, awake, and aware - and not if their just pecking through the day trying to get some comfort for themselves."
I guess I'm trying to reach a higher order of consciousness..
* sigh *
-Wes
Sunday, March 18, 2012
Friday, March 16, 2012
Upcoming Engagements at the ACC Meeting
Yours truly will be participating in the following events during the upcoming American College of Cardiology meeting in Chicago:
I look forward to seeing everyone in Chicago next Saturday!
-Wes
- I'll take part in an editorial and unsupported videotaped discussion Saturday afternoon on the impact and role of social media in cardiology practice with Shelley Wood, managing editor of theheart.org, and fellow blogger who covers private practice issues for theheart.org, Dr Seth Bilazarian. (Air time TBD).
- Now, for those looking for something a bit different at the ACC, come join me for a talk and "Tweet-up" at PUBLIC Chicago (pssst, click the link to see the hip place I'll be talking), 1301 North State Parkway, Chicago, IL Saturday 24 Mar 2012 at 6:30 pm for a talk on "The Power of Social Media to Impact Health Care Policy and Delivery." (Kindly sponsored by Zoll Medical - invite here as pdf). I hope all three of my local Twitter followers will attend.
For those unable to attend in person, we'll be using the hashtag #zollacc12 on Twitter for the event. (You can follow along in realtime using Tweetchat or Twitterfall - I am not responsible for the content there). While the event is considered officially as a "New and Recent Fellows Reception," others are welcome. Message me at @doctorwes on Twitter if you have no clue how to use Google maps and need directions. (I hear taxis will be available for those unable to drive after the event.)
I look forward to seeing everyone in Chicago next Saturday!
-Wes
The Red Light
He was an older man, lying head-up in the Intensive Care Unit attached to telemetry and pulse oximetry monitors. A small plastic cannula irritated the columella of his nose. He lifted his hand to scratch the area, but the IV tubing in his hand did the work for him sooner than he expected. He looked at the wall behind him.
"So far so good," he thought.
A soft knock was heard on the wall outside his room.
"Come in," he uttered.
A bright young woman in a neatly-pressed pant suit entered, carrying a clip board.
"Hello, Mr. Smith, my name is Sally. I'm from the Office of Patient Advocacy. I was wondering if I could ask you a few questions about your stay here in the ICU."
"I don't see why not," he said, straining his head to see the wall behind him once more. He looked back at her. "Go ahead."
"How have the staff been here? Any problems?"
"No! They've been wonderful. Really. Can't say enough about them except 'Fantastic.'"
He quickly looked at the wall again, then tuned back.
"Have the staff been responsive to you when you needed something?" the advocate asked.
"I'll say! Couldn't be nicer, but the food still needs some work."
She jotted something on her clipboard then looked up and saw the man glancing at the wall behind him again.
"I'm sorry, Mr. Smith, is there something that's concerning you?"
He turned back to her and waved to her to come closer, looking concerned.
"You see that light back there, the yellow one?"
"Yes," she said.
"Well I don't know what it's for, but last night, the guy's next to me turned red and twenty people rushed into his room and beat the poor guy to death."
-Wes
"So far so good," he thought.
A soft knock was heard on the wall outside his room.
"Come in," he uttered.
A bright young woman in a neatly-pressed pant suit entered, carrying a clip board.
"Hello, Mr. Smith, my name is Sally. I'm from the Office of Patient Advocacy. I was wondering if I could ask you a few questions about your stay here in the ICU."
"I don't see why not," he said, straining his head to see the wall behind him once more. He looked back at her. "Go ahead."
"How have the staff been here? Any problems?"
"No! They've been wonderful. Really. Can't say enough about them except 'Fantastic.'"
He quickly looked at the wall again, then tuned back.
"Have the staff been responsive to you when you needed something?" the advocate asked.
"I'll say! Couldn't be nicer, but the food still needs some work."
She jotted something on her clipboard then looked up and saw the man glancing at the wall behind him again.
"I'm sorry, Mr. Smith, is there something that's concerning you?"
He turned back to her and waved to her to come closer, looking concerned.
"You see that light back there, the yellow one?"
"Yes," she said.
"Well I don't know what it's for, but last night, the guy's next to me turned red and twenty people rushed into his room and beat the poor guy to death."
-Wes
When Programmers Outnumber Doctors
Patience. You have have to have patience.
“It’s got to be me,” I tell myself. "I'm a computer guy. Surely there must be something I’m missing." "Why would they take away that functionality that we had before?" "Why so many buttons and choices?" "Seriously?"
Everyone wants something different from our electronic medical records these days. Administrators want numbers, doctors want pictures and meaningful narrative, nurses want every pill given and bed-rail elevated documented and every check-list completed. The geeks want it mobile. Our government, administrators, physician leaders and legal system say they need this piece of data or that piece of data and then, please people, give us some more data, will you?
So everything we think, eat, and breathe is entered on a computer. Right now, it's all about the computer. After all, we’re told the Electronic Medical Record sees everything and will be our salvation.
But now I’m seeing something new.
There’s so much data that we risk doctors becoming lost in it. It is entirely possible that we are in danger of not being able to find our most important clinical signals amongst the noise and clutter of all the data. Worse: time with patients is disappearing.
Our health care information gold rush has acquired teams of programmers to feverishly implement a myriad of bureaucratic information system requirements in just a few short years. To this end, these programmers have been extremely effective. But almost as incredibly, these same programmers have little perspective of what physicians do or how we interact with patients and THIER data. As a result, doctors are not only confronted by all of this this information placed before them, but waste preceious time sifting amongst the data and continue to be the fall-guy for data entry. Codes, quality measures, documentation requirements and, oh, yeah, the progress and operative notes, are all being entered by doctors. In return, our screens have become crowded intersections of buttons, flags, options, icons, colors, warning alerts and (if we're lucky) text. Oh yeah, and a new "upgrade's" coming next week.
Typing, clicking, choosing, clicking. That one? No? Maybe this one? Yeah. But wait, now what?
Entire industries have sprouted to address this problem and provide doctors scribes to enter all this data. But are there cost savings this way? With such a model, aren't we just changing our doctors from data entry to quality assurance personnel? (“Is this what you said?” “Which code should we use, doctor?”)
Few seemed concerned about the data flood and screen crowding that's upon us. In fact, most don’t acknowledge such a problem even exists.
If you're skeptical, just ask a doctor if he spends more time with his computer or his patients now.
Doctors need better information before us, not more of it. We don't need to know what "type" of order we entered, for instance. We need more time with our patients and less time with data entry. We need white space on our screens. Deciding what information goes and what stays for all caregivers should be a priority we consider going forward.
But we can never have enough data these days, can we? Like Play-doh, we play with it, we compile it, we shape it and twist it, then bounce it around.
But someewhere in there, we also make critical medical decisions with it.
So if Google can understand the value of white space on their front page, why can't we?
-Wes
“It’s got to be me,” I tell myself. "I'm a computer guy. Surely there must be something I’m missing." "Why would they take away that functionality that we had before?" "Why so many buttons and choices?" "Seriously?"
Everyone wants something different from our electronic medical records these days. Administrators want numbers, doctors want pictures and meaningful narrative, nurses want every pill given and bed-rail elevated documented and every check-list completed. The geeks want it mobile. Our government, administrators, physician leaders and legal system say they need this piece of data or that piece of data and then, please people, give us some more data, will you?
So everything we think, eat, and breathe is entered on a computer. Right now, it's all about the computer. After all, we’re told the Electronic Medical Record sees everything and will be our salvation.
But now I’m seeing something new.
There’s so much data that we risk doctors becoming lost in it. It is entirely possible that we are in danger of not being able to find our most important clinical signals amongst the noise and clutter of all the data. Worse: time with patients is disappearing.
Our health care information gold rush has acquired teams of programmers to feverishly implement a myriad of bureaucratic information system requirements in just a few short years. To this end, these programmers have been extremely effective. But almost as incredibly, these same programmers have little perspective of what physicians do or how we interact with patients and THIER data. As a result, doctors are not only confronted by all of this this information placed before them, but waste preceious time sifting amongst the data and continue to be the fall-guy for data entry. Codes, quality measures, documentation requirements and, oh, yeah, the progress and operative notes, are all being entered by doctors. In return, our screens have become crowded intersections of buttons, flags, options, icons, colors, warning alerts and (if we're lucky) text. Oh yeah, and a new "upgrade's" coming next week.
Typing, clicking, choosing, clicking. That one? No? Maybe this one? Yeah. But wait, now what?
Entire industries have sprouted to address this problem and provide doctors scribes to enter all this data. But are there cost savings this way? With such a model, aren't we just changing our doctors from data entry to quality assurance personnel? (“Is this what you said?” “Which code should we use, doctor?”)
Few seemed concerned about the data flood and screen crowding that's upon us. In fact, most don’t acknowledge such a problem even exists.
If you're skeptical, just ask a doctor if he spends more time with his computer or his patients now.
Doctors need better information before us, not more of it. We don't need to know what "type" of order we entered, for instance. We need more time with our patients and less time with data entry. We need white space on our screens. Deciding what information goes and what stays for all caregivers should be a priority we consider going forward.
But we can never have enough data these days, can we? Like Play-doh, we play with it, we compile it, we shape it and twist it, then bounce it around.
But someewhere in there, we also make critical medical decisions with it.
So if Google can understand the value of white space on their front page, why can't we?
-Wes
Thursday, March 15, 2012
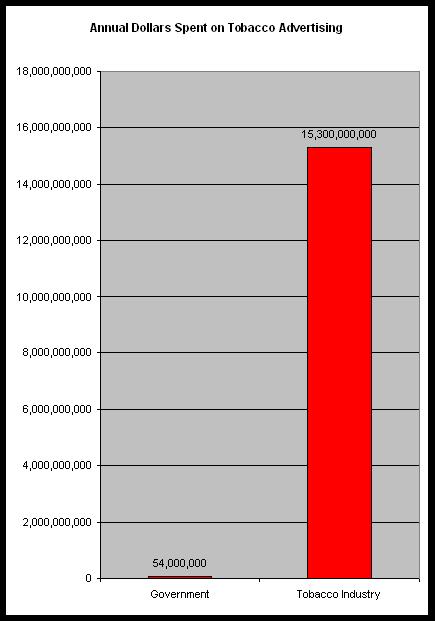
The Anti-smoking Advertising Challenge
With the government's new, graphic $54 million dollar anti-smoking advertising campaign announced today by the Centers for Disease Control, we should remember that the annual advertising budget for the tobacco industry is about $15.3 billion dollars in the U.S. alone:
-Wes
Click image to enlarge
-Wes
Tuesday, March 13, 2012
Crowdsourcing a Fellow's Social Media Talk
Pretend for a moment that you are an actively-engaged physician blogger on the internet. You are approached to give a talk at a national meeting on social media's importance to young, fledgling doctors entering their chosen field in medicine. You want to be relevant and truthful. You do NOT want to be boring. You have a pretty open forum to say anything you like.
If you only had forty minutes to convey your message, what would you say?
How would you present these ideas?
What would YOU want to hear (or see) at such a talk if you were in the audience?
Go ahead. Think about it a bit. Be creative. Help me construct my talk at the upcoming ACC meeting in Chicago on the 24th of March so it's one you'd want to attend.
Then let it rip in the comments section.
(Thanks in advance.)
-Wes
If you only had forty minutes to convey your message, what would you say?
How would you present these ideas?
What would YOU want to hear (or see) at such a talk if you were in the audience?
Go ahead. Think about it a bit. Be creative. Help me construct my talk at the upcoming ACC meeting in Chicago on the 24th of March so it's one you'd want to attend.
Then let it rip in the comments section.
(Thanks in advance.)
-Wes
Medicine 2018
It was Spring, 2018. She sat writhing in bed, complaining of nausea, feeling bloated and distended. The health care consultants who had gathered in the hall outside her room peeked in. Concerned, they began wringing their hands.
“Maybe if we tweet the symptoms, our health care social media friends can help us!”
So they did. The internet responded: “WTF?” and “How long has this been going on?” and “Maybe it’s acute appendicitis” and “F.O.S.?”
The consultants looked at each other, puzzled. “F.O.S.?”
Then it hit them: maybe she’s constipated!
So they electronically ordered a flat plat abdominal x-ray from their iPad 12 to be performed “as soon as possible.”
Within twenty minutes, a tired x-ray tech grabbed a blue gown outside, slathered his hands in antibacterial goo, donned plastic gloves and then entered the room. He followed the carefully outlined lines on the floor, placed there to minimize infection based on the laminar airflow characteristics of the room. He positioned the hard film plate behind the woman's belly, shot the picture of her abdomen, and shipped it off electronically to an eager radiologist in Dubai.
Within minutes the results returned. The ordering consultant's iDroid-10 was alerted. The results were shared with the other consultants. While impatient with the slow response time, they nonetheless peered at the results:
They paused and then looked at each other, confident they could affect a cure.
Reaching for their iDroid-10s in unison, each clicked through their multiple apps. They scrolled forward, past the ones for drug dosing, clinical formulas, Grand Rounds chats, differential diagnostic analyzer, EKG, pulse oximetry, World of Warcraft Residency Training tool, and even a retina reader…
Wait!
Maybe we have a Facebook friend that can help us!
They clicked on the iDroid-10 Facebook app and updated their status:
“Need digital dis-impaction at our local facility. Anybody game?”
Within seconds, they got 20 “Likes” but no takers.
“Damn it,” they thought.
“Looks like we’ll have to hire a doctor.”
-Wes
“Maybe if we tweet the symptoms, our health care social media friends can help us!”
So they did. The internet responded: “WTF?” and “How long has this been going on?” and “Maybe it’s acute appendicitis” and “F.O.S.?”
The consultants looked at each other, puzzled. “F.O.S.?”
Then it hit them: maybe she’s constipated!
So they electronically ordered a flat plat abdominal x-ray from their iPad 12 to be performed “as soon as possible.”
Within twenty minutes, a tired x-ray tech grabbed a blue gown outside, slathered his hands in antibacterial goo, donned plastic gloves and then entered the room. He followed the carefully outlined lines on the floor, placed there to minimize infection based on the laminar airflow characteristics of the room. He positioned the hard film plate behind the woman's belly, shot the picture of her abdomen, and shipped it off electronically to an eager radiologist in Dubai.
Within minutes the results returned. The ordering consultant's iDroid-10 was alerted. The results were shared with the other consultants. While impatient with the slow response time, they nonetheless peered at the results:
They paused and then looked at each other, confident they could affect a cure.
“Evidence of stool fills the entire ascending, transverse, descending colon and rectum. No free air. No evidence of obstruction.”
Reaching for their iDroid-10s in unison, each clicked through their multiple apps. They scrolled forward, past the ones for drug dosing, clinical formulas, Grand Rounds chats, differential diagnostic analyzer, EKG, pulse oximetry, World of Warcraft Residency Training tool, and even a retina reader…
Wait!
Maybe we have a Facebook friend that can help us!
They clicked on the iDroid-10 Facebook app and updated their status:
“Need digital dis-impaction at our local facility. Anybody game?”
Within seconds, they got 20 “Likes” but no takers.
“Damn it,” they thought.
“Looks like we’ll have to hire a doctor.”
-Wes
In the Mail: Zoll Medical to acquired by Asahi Kasei
Imagine: a wearable defibrillator company valued at a cool $2.2 billion. Not bad. (Amazing what happens when you survive a FDA "reconsideration" of your technology.
But who's Ahashi Kasei?
-Wes
But who's Ahashi Kasei?
-Wes
Monday, March 12, 2012
I Am So Screwed
I thought I'd start the week off right, get up early, have a cup of coffee, and get prepared for the week ahead, Little did I know what was in store for me when I checked my e-mail.
Margaret Polaneczky, MD (aka, @tbtam the incredibly bright OB-GYN of The Blog That Ate Manhatan fame) had left a comment on my last post suggesting I check out my profile on the CMS's Physician Compare website.
What I found was so discouraging, so demoralizing, so indicative of what we can expect from our newly-contructed computer databases compiled by a Central Authority without its own quality assurance checks, that every US doctor and patient should demand an immediate halt to what we're creating until the developers of this mess can prove they can get it right.
You see, according to the government's database, I'm not a cardiac electrophysiologist.
That's right. I do not practice cardiac electrophysiology and never have. Instead, I am just a general cardiologist. Never mind that I have searchable credentials and billings to prove it.
And if that's not enough, according to the same database, I have offices in 254 locations (I'm not kidding). Something as simple as my vocation and office locations are already completely screwed up.
And that is not even the half of it.
Mark Hamer, MD, whom I replaced at our facility in 2001 and has practices in Rochester, NY since then, is still listed as working here in Chicago. John Alexander, MD, a prominent cardiothoracic surgeon at our facility? He's retired now and no longer sees patients. Yet there they are: fully credentialled and, according to our government's CMS physician finder database, working from the same 254 offices that I work in.
According to Dr. Polaneczky, I can expect it will take at least a 6-months to correct these errors on the CMS database. (And, if you'd like some ocean-front property in Arizona, I can sell you that, too.)
I am so screwed.
But as bad as it is for me, I'm not the only one who's screwed, am I? You see, if this is as good as the government can get at culling their vast repository of information collected by hoards of coders, billers, and legions of other non-medical folk upon whom they entrust to get the data right, we are in trouble in many more ways than this. One only has to imagine the issues that arise when our government regulators turn to similarly-contructed databases to make life-and-death payment decisions. We ALL had better reconsider the wisdom of our complete reliance on such unverified databases going forward.
One thing is now perfectly clear: just because our government health care regulators have all this quality assurance and billing data at their disposal, they have no earthly idea how to use it correctly.
-Wes
Margaret Polaneczky, MD (aka, @tbtam the incredibly bright OB-GYN of The Blog That Ate Manhatan fame) had left a comment on my last post suggesting I check out my profile on the CMS's Physician Compare website.
What I found was so discouraging, so demoralizing, so indicative of what we can expect from our newly-contructed computer databases compiled by a Central Authority without its own quality assurance checks, that every US doctor and patient should demand an immediate halt to what we're creating until the developers of this mess can prove they can get it right.
You see, according to the government's database, I'm not a cardiac electrophysiologist.
That's right. I do not practice cardiac electrophysiology and never have. Instead, I am just a general cardiologist. Never mind that I have searchable credentials and billings to prove it.
And if that's not enough, according to the same database, I have offices in 254 locations (I'm not kidding). Something as simple as my vocation and office locations are already completely screwed up.
And that is not even the half of it.
Mark Hamer, MD, whom I replaced at our facility in 2001 and has practices in Rochester, NY since then, is still listed as working here in Chicago. John Alexander, MD, a prominent cardiothoracic surgeon at our facility? He's retired now and no longer sees patients. Yet there they are: fully credentialled and, according to our government's CMS physician finder database, working from the same 254 offices that I work in.
According to Dr. Polaneczky, I can expect it will take at least a 6-months to correct these errors on the CMS database. (And, if you'd like some ocean-front property in Arizona, I can sell you that, too.)
I am so screwed.
But as bad as it is for me, I'm not the only one who's screwed, am I? You see, if this is as good as the government can get at culling their vast repository of information collected by hoards of coders, billers, and legions of other non-medical folk upon whom they entrust to get the data right, we are in trouble in many more ways than this. One only has to imagine the issues that arise when our government regulators turn to similarly-contructed databases to make life-and-death payment decisions. We ALL had better reconsider the wisdom of our complete reliance on such unverified databases going forward.
One thing is now perfectly clear: just because our government health care regulators have all this quality assurance and billing data at their disposal, they have no earthly idea how to use it correctly.
-Wes
Sunday, March 11, 2012
Let's Make a Deal
It's a beautiful Sunday morning and I'm sitting in front of a computer, partly because I feel rejuvenated after slowing my blog-pace a bit, and partly out of a sense of obligation to post something on this blog.
In blogging, if you don't write, you die. It's a simple as that.
Not that you have to post much, but if it doesn't have relevance, you'll die, too. So here I am, trying to find something relevant, when I stumble upon an article from earlier this week from AMA Medical News entitled: "HHS seeks physician comments on meaningful use rules."
* sigh *
In the article, a member of the Department of Health and Human Services (HHS) likens the rules for Meaningful Use, Part 2 (MU-II) to a game show:
The reality for doctors is this: we see that hospitals have hired legions of personnel, practice managers, IT specialists, and consultants to creatively implement the law - a law written on losely-outlined imperatives which are all closely tied to the threat of withholding payments from the government should anyone dare to do anything different. We are promised "efficiencies." We are promised the value for care that the software patch will provide. But we soon see that entire workflows are being reconstructed by computer programmers with absolutely no appreciation for what WE feel and do that is important to patient care. Rather, it's all about what documentation will be required to meet the demands of MU-II to earn governmental monetary Brownie points.
Ask any doctor today what most of their group meeting are spent discussing and I would venture to say most would say that much of their meetings are spent discussing the new software upgrade coming around the corner that will lay the groundwork for qualifying for juicy government handouts for implementing MU-II. Most of MU-II is about constructing a way to handle bundled payments. As if doctors care about bundles. We care about the details, the history, we care about communication with our patients rather than a screen. We care about outcomes and costs, none of which we're allowed to see. These are the things that affect our patients, not meaningful use rules.
So it is no wonder Mr. Posnack likens the rule making process and importance of comments to the TV show "American Idol." After all, he's required by law to make us play his game. It's supposed to be fun!
But as doctors see these increasingly complex computer games consume more and more of their precious time with patients and see their compensation tied to chart completion rather than patient care, the game has already lost its luster.
Yeah, time to get outside.
-Wes
In blogging, if you don't write, you die. It's a simple as that.
Not that you have to post much, but if it doesn't have relevance, you'll die, too. So here I am, trying to find something relevant, when I stumble upon an article from earlier this week from AMA Medical News entitled: "HHS seeks physician comments on meaningful use rules."
* sigh *
In the article, a member of the Department of Health and Human Services (HHS) likens the rules for Meaningful Use, Part 2 (MU-II) to a game show:
Steven Posnack likens the rule-making process and importance of public comments to the TV show "American Idol." "Every once in a while, the fan favorite is voted off because everyone thought they were safe and so they don't vote for them," said Posnack, director of federal policy for the Office of the National Coordinator for Health Information Technology. In the rule-making world, he said, good policy can be eliminated because people don't express their satisfaction with what they like. This is why the Dept. of Health and Human Services' Centers for Medicare & Medicaid Services and the ONC hope people in the health information technology world -- including physicians -- will take the time to read the proposed stage 2 meaningful use rules and express their opinions, both good and bad.Like doctors have any say in this, really. It's the law now. We weren't asked to be involved (really) with this to computer thing to begin with, so to come to us this late in the process seems like an afterthought. We should comment now? (Like they'll reprogram things based on what we say? I'm not seeing it.)
The reality for doctors is this: we see that hospitals have hired legions of personnel, practice managers, IT specialists, and consultants to creatively implement the law - a law written on losely-outlined imperatives which are all closely tied to the threat of withholding payments from the government should anyone dare to do anything different. We are promised "efficiencies." We are promised the value for care that the software patch will provide. But we soon see that entire workflows are being reconstructed by computer programmers with absolutely no appreciation for what WE feel and do that is important to patient care. Rather, it's all about what documentation will be required to meet the demands of MU-II to earn governmental monetary Brownie points.
Ask any doctor today what most of their group meeting are spent discussing and I would venture to say most would say that much of their meetings are spent discussing the new software upgrade coming around the corner that will lay the groundwork for qualifying for juicy government handouts for implementing MU-II. Most of MU-II is about constructing a way to handle bundled payments. As if doctors care about bundles. We care about the details, the history, we care about communication with our patients rather than a screen. We care about outcomes and costs, none of which we're allowed to see. These are the things that affect our patients, not meaningful use rules.
So it is no wonder Mr. Posnack likens the rule making process and importance of comments to the TV show "American Idol." After all, he's required by law to make us play his game. It's supposed to be fun!
But as doctors see these increasingly complex computer games consume more and more of their precious time with patients and see their compensation tied to chart completion rather than patient care, the game has already lost its luster.
Yeah, time to get outside.
-Wes
Thursday, March 08, 2012
On Medtronic's Most Recent Medical Device "Correction"
Yesterday, Medtronic, Inc, the world's largest medical device manufacturer, notified me in clinic about another problem with one of their lines of defibrillators via a Dear Doctor letter (1 Mbyte) headed by the line "URGENT: MEDICAL DEVICE CORRECTION."
It seems this term is now commonly seen on other Medtronic device advisories as well.
I wondered how the marketing and legal folks at Medtronic could use that term on the top of such a letter. After all, there is no "correction" that I can see in their "Dear Doctor" letter given to me.
By way of background, the letter explained there is a problem with a very small subset of Medtronic's Entrust (US market) and Escudo (overseas market) line of defibrillators which began to be used in 2005. After 30 months of implant, a drop from 3.0V to 2.61V (ERI) can occur in 1 week to six months in rare cases. It is estimated that there are approximately 39,000 patients with these devices still implanted worldwide with 21,600 of the remaining devices in U.S. patients. The root cause of the defect described in the letter is thought to be a battery short that develops as the battery in consumed. Consequently, the battery may not last the expected three months after the device reaches its initial elective replacement indicator and doctors are advised to replace the generator immediately once the device reaches this indicator. Importantly, no deaths have occurred as a result of this defect but there is a theoretic potential that a device might not reach an effective discharge voltage after the battery depletion occurs. For doctors and patients, this alert ranks pretty low on the concern scale, provided patients are monitored closely and have their battery-reaching-ERI alerts programmed "ON." (Please see the above linked letter for full details)
This issue of what to call these device alerts is not a small issue. In early 2005 when a rash of serious ICD problems began to surface, they were uniformly called "device recalls." But the Heart Rhythm Society recognized the problems with this nomenclature:
As a result, the terms "advisory alert" or "safety alert" were proposed to describe less serious communications with doctors and patients regarding important device communications.
So why now "important device corrections?" In cases like this, I feel it would be best that device manufacturers stick with terms that industry and physician groups have agreed so that the appropriate level of concern is conveyed to doctors and patients alike without sugar-coating the defects. That way when these letters are issued, we're all on the same page.
-Wes
It seems this term is now commonly seen on other Medtronic device advisories as well.
I wondered how the marketing and legal folks at Medtronic could use that term on the top of such a letter. After all, there is no "correction" that I can see in their "Dear Doctor" letter given to me.
By way of background, the letter explained there is a problem with a very small subset of Medtronic's Entrust (US market) and Escudo (overseas market) line of defibrillators which began to be used in 2005. After 30 months of implant, a drop from 3.0V to 2.61V (ERI) can occur in 1 week to six months in rare cases. It is estimated that there are approximately 39,000 patients with these devices still implanted worldwide with 21,600 of the remaining devices in U.S. patients. The root cause of the defect described in the letter is thought to be a battery short that develops as the battery in consumed. Consequently, the battery may not last the expected three months after the device reaches its initial elective replacement indicator and doctors are advised to replace the generator immediately once the device reaches this indicator. Importantly, no deaths have occurred as a result of this defect but there is a theoretic potential that a device might not reach an effective discharge voltage after the battery depletion occurs. For doctors and patients, this alert ranks pretty low on the concern scale, provided patients are monitored closely and have their battery-reaching-ERI alerts programmed "ON." (Please see the above linked letter for full details)
This issue of what to call these device alerts is not a small issue. In early 2005 when a rash of serious ICD problems began to surface, they were uniformly called "device recalls." But the Heart Rhythm Society recognized the problems with this nomenclature:
Terminology should be commensurate with risk. HRS has previously recommended that the term “recall” not be used in reference to devices that do not require removal or explant, as it may foster miscommunication and lead to unnecessary and potentially harmful interventions. Research supports the concept that the specific wording chosen to warn patients has critical implications and that some words (urgent, danger, FDA) and some phrases (FDA Public Safety Warning, Product Danger Alert, Public Safety Warning) are perceived as being just as important as phrases that include the word “recall.” The term “recall” has regulatory and legal implications that extend beyond cardiac rhythm management devices and substantial hurdles must be overcome to change the terminology. Nevertheless, the FDA is encouraged to explore the legal and regulatory alternatives to facilitate the establishment of a simple and intuitive nomenclature to publicly communicate important information out implanted medical device performance.
As a result, the terms "advisory alert" or "safety alert" were proposed to describe less serious communications with doctors and patients regarding important device communications.
So why now "important device corrections?" In cases like this, I feel it would be best that device manufacturers stick with terms that industry and physician groups have agreed so that the appropriate level of concern is conveyed to doctors and patients alike without sugar-coating the defects. That way when these letters are issued, we're all on the same page.
-Wes
Tuesday, March 06, 2012
Developing a Hybrid Pacemaker
Much like a hybrid car recaptures energy lost with braking, so too are technologies being developed to recapture the heart's motion to power a pacemaker using piezoelectric crystals and magnets:
The researchers haven’t built a prototype yet, but they’ve made detailed blueprints and run simulations demonstrating that the concept would work. As reported in the journal Applied Physics Letters, a hundredth-of-an-inch thin slice of a special “piezoelectric” ceramic material would essentially catch heartbeat vibrations and briefly expand in response. Piezoelectric materials’ claim to fame is that they can convert mechanical stress (which causes them to expand) into an electric voltage.-Wes
Karami and his colleague Daniel Inman, chair of aerospace engineering at U-M, have precisely engineered the ceramic layer to a shape that can harvest vibrations across a broad range of frequencies. They also incorporated magnets, whose additional force field can drastically boost the electric signal that results from the vibrations.
The new device could generate 10 microwatts of power, which is about eight times the amount a pacemaker needs to operate, Karami says. It always generates more energy than the pacemaker requires, and it performs at heart rates from 7 to 700 beats per minute. That’s well below and above the normal range.
Monday, March 05, 2012
Sexism in Government Heart Health Programs
I saw this ad campaign sprinkled around O'hare airport last evening:
While understand the importance of increasing awareness of heart disease in women, let's not forget the issue of heart disease is just as important (if not more so) for men.
-Wes
Click image to enlarge
While understand the importance of increasing awareness of heart disease in women, let's not forget the issue of heart disease is just as important (if not more so) for men.
-Wes
Subscribe to:
Comments (Atom)