Laura Landro in today's issue from the
Wall Street Journal describes an initiative hospitals are taking to collect better medication information on their patient's in a rather feeble attempt to prevent medical errors. This is in response to a national patient safety standard that went into effect in January called "medication reconciliation." This means hospitals must have in place means for collecting complete drug and allergy histories and comparing them with new medications that their doctors order.
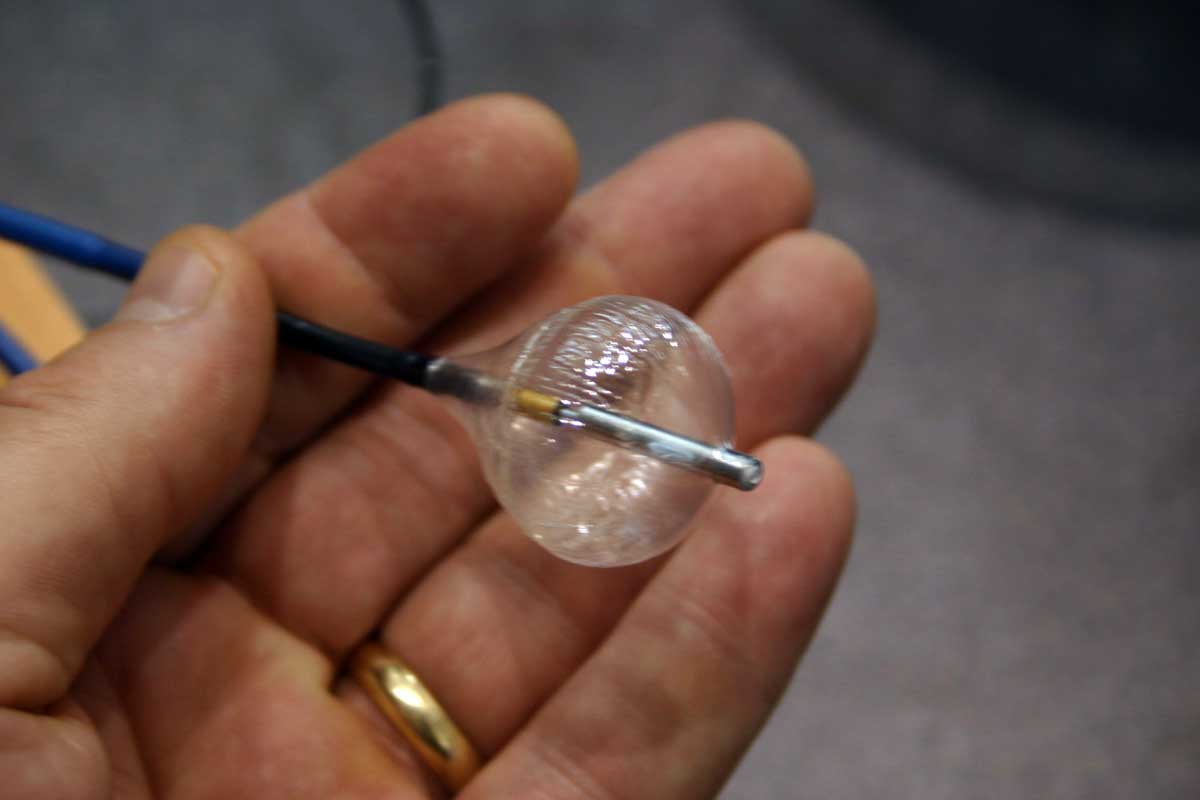
Stanford Hospital has initiated a
"Vial of Life" program with local EMS services where the patient's medication lists are printed on paper and placed in an old medication vial and stored in that highly accessible and often visited location: the refrigerator. Huh? Have you ever heard the adage, "Out of sight, out of mind?" This seems like an unlikely place to keep medication changes up-to-date and current. People I know don't carry a refrigerator. Perhaps most important, the reliance on patients to become "more proactive" in knowing their medications is sure to fail. When I see patients in clinic, most don't know the names of medications, but might know they're on a "water pill" at best, and more often have NO idea the purpose of each medicationn, let alone their names. On top of this, to expect them to know the milligram
dosage of each drug is unrealistic. And that dosage, which has been stored in the refrigerator vial for 6 months, is not likely to be updated. Sincerety and spin don't save lives.
I am fortunate to work in one of the
"100 most wired" hospital systems in the country. Yet even our system is insufficient. We use the
EPIC medical system, touted to be the next frontier of health care, that is integrated between the outpatient physicians' offices and the hospital. Medications entered by the patient's outpatient physician alters the same medical record that providers within the hospital see. This adds incredible continuity of care on many fronts. But I am frustrated at the incredibly complex screen that is displayed when I reorder a myriad of medications and have to "reconcile" their complex and innumerable interactions. More challenging is that if my patient travels to a physician's office outside our network, no information can flow easily with them. Suffice it to say, this system goes well beyond "the paper in a vial" approach.
It was with awe that I had the chance to meet with
Ross Fletcher, MD, Chief of Staff, from the
VA Medical Center from Washington DC last week. Ross has been instrumental in developing and promoting the
VA's Vista Electronic Medical Record (EMR) used by the VA Medical system, and a model for the EMR industry. Best of all, its free. It's power is demonstrated in its ability to incorporate geographically disparate graphical and data-driven information and display it for the physician in a organized, easy-to-comprehend fashion on any commercially-available computer screen. And this data is culled from every VA medical center across the United States, in seconds. Information from a VA in California, Utah, and Washington can be viewed side-by-side in chronological order.
While sitting with Ross at dinner, his pager went off. He looked down, smiled, and delighted in the fact that a seasonal variation in effectiveness of therapy was suggested by analyzing over 1
billion vital signs on veterans collected over the preceeding five years across the U.S. using multivariate analysis. The sleepy old VA?
And you can bet their medication lists are up to date.
--Wes
 (But I do like the database of phone numbers it contains to call for help...)
(But I do like the database of phone numbers it contains to call for help...)  (But I do like the database of phone numbers it contains to call for help...)
(But I do like the database of phone numbers it contains to call for help...)