Overhead at the ACC Meeting today in Chicago:
There are 174 active cardiology training programs in the United States.
Ten programs do not participate in the National Resident Matching Program (NRMP).
Of the 164 remaining programs, there were about 1200 applicants to fill 699 training positions for Cardiovascular Disease. 6 positions went unfilled.
Approximately 40% of applicants were from non-US medical schools.
Ref: The NRMP's stats - informative, but their stats did not mention the total number of applicants who applied for the 699 positions.
* * *
Although there are about 4000 doctors who call themselves "electrophysiologists" in the US, only about 1700 carry valid board certification from the American Board of Internal Medicine in Cardiac Electrophysiology.
* * *
Just thought you'd like to know...
-Wes
Monday, March 31, 2008
Dr. Wes to Host Grand Rounds
Okay, great and powerful blog-o-sphere, flick those fancy fingers and find your best to fire this way next week as I host the medical blog-o-sphere's Grand Rounds edition Vol 4, No 29 on April 8th, 2008. Let's make this the best one EVER! (This week's April Fool's Grand Rounds it's being hosted over at GruntDoc).
Sensational posts should be the norm, not drab fluff used to fill time voids. Be creative, snarky, insightful, clever, ingenious. Make people laugh, make them cry - it really doesn't matter. Just think, people, THINK!
Being of an eclectic mind, topics can be of your choosing; docs, nurses, administrators, legal beagles, health policy gurus, wonks, wonkettes, and patients are encouraged to submit their best and brightest works relating to medicine and healthcare. (Obviously, the shortest posts or those with lots of pictures or those with accompanying payment to my PayPal account will get highest ranking...)
Seriously, I'm still working on an organizational scheme, but I'm hoping the tapestry develops as the week progresses. So have fun.
Please send posts to wes at medtees dot com and include "Grand Rounds" in the Subject line, blog name, the post URL, and a brief 1-2 sentence description of the work. Do NOT send me the Word document nor send multiple posts (please, one post per person). Posts will be accepted until 8AM Monday, 7 Apr 08 your time. Late posts will be ridiculed mercilessly.
-Wes
Sensational posts should be the norm, not drab fluff used to fill time voids. Be creative, snarky, insightful, clever, ingenious. Make people laugh, make them cry - it really doesn't matter. Just think, people, THINK!
Being of an eclectic mind, topics can be of your choosing; docs, nurses, administrators, legal beagles, health policy gurus, wonks, wonkettes, and patients are encouraged to submit their best and brightest works relating to medicine and healthcare. (Obviously, the shortest posts or those with lots of pictures or those with accompanying payment to my PayPal account will get highest ranking...)
Seriously, I'm still working on an organizational scheme, but I'm hoping the tapestry develops as the week progresses. So have fun.
Please send posts to wes at medtees dot com and include "Grand Rounds" in the Subject line, blog name, the post URL, and a brief 1-2 sentence description of the work. Do NOT send me the Word document nor send multiple posts (please, one post per person). Posts will be accepted until 8AM Monday, 7 Apr 08 your time. Late posts will be ridiculed mercilessly.
-Wes
Sunday, March 30, 2008
Economic Conflict-of-Interest Credentialling
Now here's a new twist to physician credentialling:
Conflicts abound on both sides. I'm not saying I have the answer in this case, but this is certainly new territory for physician credentialling...
-Wes
An “economic conflict-of-interest” policy imposed by Baptist Health has ignited debate that often comes down to this: Are some hospitals and doctors more concerned about their own success than what’s best for patients?Boy, seems the hospital better be careful here. At least one other major medical center has a counter-suit pending by a doctor who exposed conflicts held by others in the hospital's organization. Gosh, and what about the issues of restriction of trade?
The policy, also called “economic credentialing,” denies doctors privileges at Baptist Health hospitals if they own a stake in a competing facility. The Baptist Health system, the largest in Arkansas, includes Baptist Health Medical Center in Little Rock, as well as facilities in North Little Rock, Arkadelphia, Heber Springs and elsewhere.
Conflicts abound on both sides. I'm not saying I have the answer in this case, but this is certainly new territory for physician credentialling...
-Wes
First, Blame the Patient
Here's a prescription for health care reform in case some of us are not aware of the fete accompli that we have reached in the policy world with the upcoming election - here's a quick summary of what's coming:
-Wes
* Of course, do not CALL it "the patient," instead, call it working to "fight chronic disease."
ADDENDUM: Lisa Emrich at Brass and Ivory blog adds her perspective as a patient with chronic disease.
1. First, blame the patient.*We appreciate the detailed spreadsheets of costs provided by the Partnership to Fight Chronic Disease. Given their apparently extensive talent bank and funding for this type of analysis, we look forward to seeing comparable line-item analyses for the costs of ever-burgeoning healthcare bureaucracy.
2. Do not, under any circumstances blame:3. Next, assemble an impressive array of like-minded and highly gifted individuals who sincerely believe the patient is the problem.
- the relentless bureaucracy hell-bent on continued expansion
- the rising cost of technology
- the lack of tort reform
- overtesting occurring because of defensive medicine
- the annually increasing percentage of administrative overhead for healthcare delivery in the US, now approaching 30% of the entire healthcare bill
- direct-to-consumer advertising
- the un-checked hospital construction industry
- the increasing median age of our populace
- the lack of transparency of true costs within the system
- No restriction on healthcare delivery in futile situations
4. Assemble lots and lots of "partners" with financial conflicts in this debate to stand by your side.
5. Build a very fancy website at significant cost.
6. Spend lots and lots of money on "new media consultants" to be sure the blog-o-sphere learns of this website (h/t: Thanks, Chris)
7. Pat yourself on the back for defining "the problem."
-Wes
* Of course, do not CALL it "the patient," instead, call it working to "fight chronic disease."
ADDENDUM: Lisa Emrich at Brass and Ivory blog adds her perspective as a patient with chronic disease.
You Can Never Be Too Careful

I saw this while traveling this weekend.
I wonder if there's a MRSA epidemic being spread at gas pumps...
Anyone know how this foam hand sanitizer works on grease?
-Wes
Thursday, March 27, 2008
Imagine A World Without Medicare
Imagine if Medicare were to become insolvent. What would happen?
Would the sky fall?
Would people stop needing or receiving healthcare?
I don’t think so.
The implications of this are interesting to ponder.
I suspect the majority of us would be fine. Healthcare would be delivered, but the world of healthcare as we know it would rapidly change. Congress would likely attempt to take the path of least resistance to maintain solvency by raising taxes, imposing a healthcare mandate, or delaying the Medicare eligibility age.
But what if all hell broke loose and no Medicare were available. What would our healthcare world look like?
First and foremost, existing entities dependent on Medicare payments would scurry to assure their viability and potential for profitability any way possible. For most, rationing of healthcare benefits would rapidly accelerate. High risk individuals would be denied insurance coverage or face exorbitant premiums. Competition for low-risk patients would accelerate between insurers. The weak insurers would die out or be consolidated and the strong would likely survive. Hospitals would shift billing from their largest insurer to the patients themselves. Patients would have an eye-opening experience when the reality of their price markup reveals the perversity of health care prices. Grass-root advocacy groups would call for immediate change to include price transparency. Hospitals would be forced to compete for high-cost services. Simultaneously, hospitals would recognize the need to greatly restrict new debt obligations (like construction costs) to conserve resources to cover bad debt. The unchecked hospital construction boom would quickly cease. Unnecessary administrative and support personnel would be weaned. Hospitals would put pressure on suppliers to reduce costs: pharmaceutical companies and medical device companies would be forced to cut costs, lest their customers go bankrupt, too. Pharmaceutical companies, eager to cut costs, might remove the excess cost-ballast of direct-to-consumer advertising. CEO’s salaries and severance packages would come into line with reality. No one would be spared cost-cutting measures.
Regrettably, many patients with existing illnesses would likely be forced into bankruptcy as hospitals would increasingly employ legions of collection agents to extract payments from their patients' assets. Some would turn to Medicaid or another government safety net system. These stories would likely make heart-wrenching press stories and more pressure would be placed on the healthcare system to reduce costs or develop cost-effective options for the disenfranchised. Suddenly, patients will ask, “Could this happen to me?”
Doctors would immediately opt out of accepting any Medicare reimbursement due to the unreliability of payment. At least the threat of reimbursement cuts would cease. Especially since the ultimate reimbursement cut had just occurred. Patients would have to negotiate with doctors to provide care. Each test ordered on behalf of their care would be closely scrutinized for necessity. Costs would have to be transparent. Patients would become frugal lest they squander their life savings. Insurers would adapt to providing patients with insurance options to cover their costs. Employers would have the options of purchasing insurance for their employees at varying levels of coverage as a “perk,” provided the costs were not excessive. Since healthcare would no longer an entitlement, people would have to prioritize their savings to adjust for the inevitable need for late life care. Health savings accounts, or their equivalent, would flourish.
Admittedly, there are those less fortunate who cannot afford to contribute meaningfully to their healthcare costs, or there will always be individuals whom have been afflicted with a malady that has left them unable to contribute. For those, a bare-bones government-sponsored health plan would have to be available. To do otherwise would be inhumane. But healthcare, like hotels and restaurants, will gradually be tailored to meet the needs of patients. Those wanting 5-star Hilton-like accommodations and can afford them, will pay for them. Those that can only afford a Motel-6 accommodation will pay less. Nothing will be free any longer. Come to an Emergency Room? Expect a bill. Can’t pay? Apply for government assistance or a low-cost insurance or payment plan. That’s the way it’ll have to be.
Additional pressure would also be applied to limit unnecessary and costly testing in a non-Medicare era. Pressure to establish meaningful nation-wide tort-reform will simultaneously take place. Since medical errors in any healthcare system are inevitable, peer-directed health courts or a no-fault payment policy would have to be implemented. Perhaps then, and only then, patients with legitimate complaints will be heard and compensated, while exorbitant and costly legal posturing and judgments with grossly overpaid expert witnesses and the like, will end.
Without Medicare, for the first time healthcare policy would become a priority, not an afterthought.
Imagine. Real change.
And most for the better.
-Wes
Would the sky fall?
Would people stop needing or receiving healthcare?
I don’t think so.
The implications of this are interesting to ponder.
I suspect the majority of us would be fine. Healthcare would be delivered, but the world of healthcare as we know it would rapidly change. Congress would likely attempt to take the path of least resistance to maintain solvency by raising taxes, imposing a healthcare mandate, or delaying the Medicare eligibility age.
But what if all hell broke loose and no Medicare were available. What would our healthcare world look like?
First and foremost, existing entities dependent on Medicare payments would scurry to assure their viability and potential for profitability any way possible. For most, rationing of healthcare benefits would rapidly accelerate. High risk individuals would be denied insurance coverage or face exorbitant premiums. Competition for low-risk patients would accelerate between insurers. The weak insurers would die out or be consolidated and the strong would likely survive. Hospitals would shift billing from their largest insurer to the patients themselves. Patients would have an eye-opening experience when the reality of their price markup reveals the perversity of health care prices. Grass-root advocacy groups would call for immediate change to include price transparency. Hospitals would be forced to compete for high-cost services. Simultaneously, hospitals would recognize the need to greatly restrict new debt obligations (like construction costs) to conserve resources to cover bad debt. The unchecked hospital construction boom would quickly cease. Unnecessary administrative and support personnel would be weaned. Hospitals would put pressure on suppliers to reduce costs: pharmaceutical companies and medical device companies would be forced to cut costs, lest their customers go bankrupt, too. Pharmaceutical companies, eager to cut costs, might remove the excess cost-ballast of direct-to-consumer advertising. CEO’s salaries and severance packages would come into line with reality. No one would be spared cost-cutting measures.
Regrettably, many patients with existing illnesses would likely be forced into bankruptcy as hospitals would increasingly employ legions of collection agents to extract payments from their patients' assets. Some would turn to Medicaid or another government safety net system. These stories would likely make heart-wrenching press stories and more pressure would be placed on the healthcare system to reduce costs or develop cost-effective options for the disenfranchised. Suddenly, patients will ask, “Could this happen to me?”
Doctors would immediately opt out of accepting any Medicare reimbursement due to the unreliability of payment. At least the threat of reimbursement cuts would cease. Especially since the ultimate reimbursement cut had just occurred. Patients would have to negotiate with doctors to provide care. Each test ordered on behalf of their care would be closely scrutinized for necessity. Costs would have to be transparent. Patients would become frugal lest they squander their life savings. Insurers would adapt to providing patients with insurance options to cover their costs. Employers would have the options of purchasing insurance for their employees at varying levels of coverage as a “perk,” provided the costs were not excessive. Since healthcare would no longer an entitlement, people would have to prioritize their savings to adjust for the inevitable need for late life care. Health savings accounts, or their equivalent, would flourish.
Admittedly, there are those less fortunate who cannot afford to contribute meaningfully to their healthcare costs, or there will always be individuals whom have been afflicted with a malady that has left them unable to contribute. For those, a bare-bones government-sponsored health plan would have to be available. To do otherwise would be inhumane. But healthcare, like hotels and restaurants, will gradually be tailored to meet the needs of patients. Those wanting 5-star Hilton-like accommodations and can afford them, will pay for them. Those that can only afford a Motel-6 accommodation will pay less. Nothing will be free any longer. Come to an Emergency Room? Expect a bill. Can’t pay? Apply for government assistance or a low-cost insurance or payment plan. That’s the way it’ll have to be.
Additional pressure would also be applied to limit unnecessary and costly testing in a non-Medicare era. Pressure to establish meaningful nation-wide tort-reform will simultaneously take place. Since medical errors in any healthcare system are inevitable, peer-directed health courts or a no-fault payment policy would have to be implemented. Perhaps then, and only then, patients with legitimate complaints will be heard and compensated, while exorbitant and costly legal posturing and judgments with grossly overpaid expert witnesses and the like, will end.
Without Medicare, for the first time healthcare policy would become a priority, not an afterthought.
Imagine. Real change.
And most for the better.
-Wes
Wednesday, March 26, 2008
Eleven Years and Counting
How old will I be in 11 years when Medicare’s Trust Fund goes bankrupt?
I’ll be sixty.
Five years before I’m eligible for the program.
I mean, I’m entitled to healthcare! Just like everybody else. Free is for me! Doesn’t anybody care about this?
So, how old will you be when Medicare goes belly-up?
And who will take care of all of us 60-year olds when we start really needing healthcare because we have been unable to “prevent” ailments or impose cost controls because we have to insure the ubiquitous “47 million ” as we accelerate the pace to assure that hundreds of millions more of us will join these ranks in just eleven years?
Probably doctors.
But not just any doctors. There will be doctors who are risk-averse and will stay with the system, and entrepreneurial doctors who have opted out of the rat race: a two-tiered system.
Oh, sure, there’ll be “universal (‘free’) healthcare” for all - after all that sounds so politically-correct. But the system we rely on today is dying a rapid death.
One way or another, look for Americans to shoulder more and more of the healthcare costs through taxes, or mandates, or higher deductibles or more and more rationing as government invades physicians’ space.
Just to support the ridiculous bureaucratic machine that is healthcare today.
But we as patients could make a difference if we just took an interest in our own well-being.
Maybe there’s a better way...
Perhaps we should just declare Medicare dead now and wake up to the reality so we can finally start working on a healthcare reform package that will be sustainable rather than perpetuating this ruse through empty promises.
-Wes
I’ll be sixty.
Five years before I’m eligible for the program.
I mean, I’m entitled to healthcare! Just like everybody else. Free is for me! Doesn’t anybody care about this?
So, how old will you be when Medicare goes belly-up?
And who will take care of all of us 60-year olds when we start really needing healthcare because we have been unable to “prevent” ailments or impose cost controls because we have to insure the ubiquitous “47 million ” as we accelerate the pace to assure that hundreds of millions more of us will join these ranks in just eleven years?
Probably doctors.
But not just any doctors. There will be doctors who are risk-averse and will stay with the system, and entrepreneurial doctors who have opted out of the rat race: a two-tiered system.
Oh, sure, there’ll be “universal (‘free’) healthcare” for all - after all that sounds so politically-correct. But the system we rely on today is dying a rapid death.
One way or another, look for Americans to shoulder more and more of the healthcare costs through taxes, or mandates, or higher deductibles or more and more rationing as government invades physicians’ space.
Just to support the ridiculous bureaucratic machine that is healthcare today.
But we as patients could make a difference if we just took an interest in our own well-being.
Maybe there’s a better way...
Perhaps we should just declare Medicare dead now and wake up to the reality so we can finally start working on a healthcare reform package that will be sustainable rather than perpetuating this ruse through empty promises.
-Wes
Tuesday, March 25, 2008
Monday, March 24, 2008
Hypoperformance Anxiety Syndrome
My suggestion for a new diagnosis for the upcoming American Psychiatric Associations' Medicare coding criteria, DSM-V:
Yes, I know, I'm leaving out Axis II...
-Wes
Hypoperformance Anxiety Syndrome (HPAS)
Definition:
Axis I: An acute state of unrest, sleeplessness, and agitation caused by Pay for Performance measures which are no longer measuring productivity while on vacation.
Yes, I know, I'm leaving out Axis II...
-Wes
Saturday, March 22, 2008
Meet My Blog Parents
Yesterday on our way South we had a chance to meet some mega-bloggers: Dr. Helen Smith (Dr. Helen) and Glenn Reynolds of Instapundit.com fame. Helen and Glenn were the people who were instrumntal at introducing me to the blog-o-sphere.
It was funny how I learned of this strange world: Glenn posted a picture of Helen wearing one our t-shirts from MedTees.com on Instapundit, sending such a flood of traffic that I wondered if I was having a denial-of-service attack.
So Glenn and Helen, here's to you! I hope my three readers flood your sites with some blog love, too!
-Wes
It was funny how I learned of this strange world: Glenn posted a picture of Helen wearing one our t-shirts from MedTees.com on Instapundit, sending such a flood of traffic that I wondered if I was having a denial-of-service attack.
So Glenn and Helen, here's to you! I hope my three readers flood your sites with some blog love, too!
-Wes
Friday, March 21, 2008
Spring Break!
Thursday, March 20, 2008
How to Piss Off An Attending
Noon conference, for those unfamiliar, is an educational endeavor where an attending physician gets to spoon-feed medical residents factoids and pearls about various medical conditions or treatments critical for their training. Usually it consists of "core" educational topics felt by their peers to be those topics necessary to prepare them for passing their National Board Examination. For attendings, these aren't the most exciting lectures to give, but they certainly serve an important purpose. For the residents, it's a chance to hear from experienced attending physicians from various departments throughout the hospital who have spent considerable time, energy and effort to organize the critical themes central to their education. The residents get to sit back, interact, and learn.
And sometimes in the dark, warm, post-prandial post-call setting, residents drift off to sleep. I'm okay with that.
But being at noontime, residents often eat lunch since their many responsibilities preclude much time to stop by the cafeteria. Not uncommonly, nice, attractive drug reps bring tantalizingly scrumptious cuisine upon which they can munch during the lecture. They, too, want to make that the budding doctors-to-be know how to give the latest dose of Drug X or Drug Y, and "here's-a-corparately-sponsored-study-we-thought-you'd-like-to-see."
So let me be perfectly blunt.
The minute residents start prioritizing their interactions with the industry drug rep over the attending's lecture, I'd suggest they consider another field...
... like marketing.
-Wes
And sometimes in the dark, warm, post-prandial post-call setting, residents drift off to sleep. I'm okay with that.
But being at noontime, residents often eat lunch since their many responsibilities preclude much time to stop by the cafeteria. Not uncommonly, nice, attractive drug reps bring tantalizingly scrumptious cuisine upon which they can munch during the lecture. They, too, want to make that the budding doctors-to-be know how to give the latest dose of Drug X or Drug Y, and "here's-a-corparately-sponsored-study-we-thought-you'd-like-to-see."
So let me be perfectly blunt.
The minute residents start prioritizing their interactions with the industry drug rep over the attending's lecture, I'd suggest they consider another field...
... like marketing.
-Wes
Resident vs. Hospital Cafeteria
Kudos to Dr. Rob Stevenson:
-Wes
The irony is that the hospital, which helped develop the nutritious menu at the new school, is now being used to circumvent its own efforts.Well done, my man. Well done.
And that irony is not lost on a group of cardiology doctors and nurses, who last month protested their own hospital’s lax nutrition standards by staging an eat-in at the high school.
Dissatisfied with Capital Health’s tepid response, cardiology resident Rob Stevenson penned an opinion piece, published in this paper on Wednesday, in which he urged the hospital to deep-six the deep fryers.
-Wes
My Job is Secure
Pretty optimistic forecast for my field from these guys:
We still need a multi-center, prospective, randomized mortality trial to determine the long-term safety and efficacy of primary therapy of atrial fibrillation ablation compared to medical therapy. Until this occurs, only symptomatic patients refractory to medical therapy should be considered for referral for this procedure.
-Wes
According to Millennium Research Group's Global Markets for Atrial Fibrillation (AF) Treatment Devices 2008 report, over 32,000 electrophysiology (EP) procedures were performed for the treatment of AF in the US in 2007. AF EP procedure volumes will increase at a compound annual growth rate of over 25% from 2008 to 2012.While "increasing physician acceptance" helps to drive this market, regrettably, so does economics - catheter ablation still pays better than most procedures electrophysiologists perform.
Growth in procedure volumes will be driven by the increasing physician acceptance of EP ablation as a viable and effective treatment for AF. Over the next several years, these procedures will be used more often over medical therapy than in the past. The introduction of new technology will also support greater procedure volumes through 2012; these new devices will enable physicians to increase the safety, efficiency, and efficacy of EP ablation catheter procedures. By 2012, over 109,000 EP procedures will be performed to treat AF in the US.
We still need a multi-center, prospective, randomized mortality trial to determine the long-term safety and efficacy of primary therapy of atrial fibrillation ablation compared to medical therapy. Until this occurs, only symptomatic patients refractory to medical therapy should be considered for referral for this procedure.
-Wes
Tuesday, March 18, 2008
Single or Multiple-Use Medical Instruments?
Today's Wall Streeet Journal rejuvenates a long-standing debate in hospitals: that of re-cycling equipment that is labeled "single use" to save on costs. Re-sterilization of instruments has become a multi-million dollar industry. Why? Because what hospitals care about most these days is saving money on consumables, and what better way to save than to recycle an instrument for a small fee and charge the patient for a new single-use instrument.
In effect, this is done every day in hospitals that reprocess instruments.
Now to be fair, what really happens from the hospitals' perspective is they get a lump sum reimbursement payment for a procedure and must use that amount to pay for all of the procedural consumables, including instruments. That lump sum payment amount is negotiated with the insurer well before any talk of re-using instruments occurs. It is usually negotiated assuming new "single-use" instruments are used. Further, because reprocessing has been "approved" by the FDA for some instruments under careful regulation, it's legit and hospitals can save a bundle.
Although rare, legal precedent has been established where re-used catheters were found dangerous. Was this a frivolous case or were there circumstances that were less than ideal? At least one jury thought their might have been a problem.
Cases like this sent shock waves around local hospitals - at least for a time.
But money is a strong motivator. Equipment and staff aren't getting cheaper. So to reassure hospitals, the re-sterilization industry began offering liability coverage as a form of indemnity against potential legal challenges regarding the safety of their service. Also, they point to the FDA which has sanctioned their process as "safe."
So naturally, many hospitals have entered back into the fold of re-use.
The instrument manufacturing industry is now understandably incensed and outraged at these reprocessors because the practice of instrument re-use substantially cuts into their bottom line profits. In my estimation, manufacturers sell about one tenth of their usual instruments to hospitals, since it is not uncommon for a "single-use" non-metallic instruments to be reprocessed 8 to 10 times before being discarded. Some metallic instruments may be used far longer.
Meanwhile, patients do not see the savings - the hospitals pass this on to cover other expenses. C'est la vie.
But the manufacturers have one thing on their side: the patient safety argument. You can never be too safe these days.
The manufacturers can point to ethylene oxide (used to sterilize instruments that cannot withstand heat) that can be harmful to humans, and there have been instances where excessive levels were detected on re-processed electrophysiology catheters when screened. For the clinician, there's no readily-apparent way to detect for residual ethylene oxide contaminants before procedures at the patient's bedside, so we take it in trust that levels are satisfactorily low. Were the instruments allowed to "air" for 14 days? Impossible to tell - we have to rely on those handy-dandy FDA inspections to assure compliance. Or alternatively, there have been small studies that found proteinacious material on catheters after re-sterilization. Eeeewwww.
So to combat the large preprocessing industry, device manufacturers wanted patient's to consent to the use of re-sterilized and re-used equipment during their surgeries. Seems reasonable, right?
But this hasn't happened.
Imagine.
Now to be fair, I have been on both sides of this debate - I have worked at institutions that have re-sterilized instruments and I have worked at institutions that are single-use. I found that doctors are shoved into this debate unwittingly: we need the hospital to do our procedures and provide the instruments, but may not like having to use re-processed instruments on our patients. In the case of electrophysiology catheters - they just don't handle the same. Further, the thought that a patient is unaware of this practice is unsettling. Because of the nature of medicine these days, we assume the responsibility for the patient's well-being in tandem with the hospital. Yet often, we are not part of the discussion regarding the use of preprocessed instruments. If we are, then the whole murky area of what it took for doctors to agree to using these re-used catheters begins to raise its ugly head.
So while economic arguments exist on both sides of the device re-reprocessing fence, we must not lose sight that it's the patient that matters here. Certainly, if re-used instruments are being used in a laboratory, I believe that patients should be made aware and have this included in their informed consent, with any potential risks spelled out. Further, if a patient knew they could apply some of the cost savings of re-processing toward their procedure costs, then perhaps they'd be more willing to agree to the practice.
But the subterranean way things happen now is not acceptable.
Given the current satate of affairs, here's the ultimate litmus test on this issue in my book:
If you were having a procedure, which instrument(s) would you want used on yourself: re-processed or single-use?
-Wes
In effect, this is done every day in hospitals that reprocess instruments.
Now to be fair, what really happens from the hospitals' perspective is they get a lump sum reimbursement payment for a procedure and must use that amount to pay for all of the procedural consumables, including instruments. That lump sum payment amount is negotiated with the insurer well before any talk of re-using instruments occurs. It is usually negotiated assuming new "single-use" instruments are used. Further, because reprocessing has been "approved" by the FDA for some instruments under careful regulation, it's legit and hospitals can save a bundle.
Although rare, legal precedent has been established where re-used catheters were found dangerous. Was this a frivolous case or were there circumstances that were less than ideal? At least one jury thought their might have been a problem.
Cases like this sent shock waves around local hospitals - at least for a time.
But money is a strong motivator. Equipment and staff aren't getting cheaper. So to reassure hospitals, the re-sterilization industry began offering liability coverage as a form of indemnity against potential legal challenges regarding the safety of their service. Also, they point to the FDA which has sanctioned their process as "safe."
So naturally, many hospitals have entered back into the fold of re-use.
The instrument manufacturing industry is now understandably incensed and outraged at these reprocessors because the practice of instrument re-use substantially cuts into their bottom line profits. In my estimation, manufacturers sell about one tenth of their usual instruments to hospitals, since it is not uncommon for a "single-use" non-metallic instruments to be reprocessed 8 to 10 times before being discarded. Some metallic instruments may be used far longer.
Meanwhile, patients do not see the savings - the hospitals pass this on to cover other expenses. C'est la vie.
But the manufacturers have one thing on their side: the patient safety argument. You can never be too safe these days.
The manufacturers can point to ethylene oxide (used to sterilize instruments that cannot withstand heat) that can be harmful to humans, and there have been instances where excessive levels were detected on re-processed electrophysiology catheters when screened. For the clinician, there's no readily-apparent way to detect for residual ethylene oxide contaminants before procedures at the patient's bedside, so we take it in trust that levels are satisfactorily low. Were the instruments allowed to "air" for 14 days? Impossible to tell - we have to rely on those handy-dandy FDA inspections to assure compliance. Or alternatively, there have been small studies that found proteinacious material on catheters after re-sterilization. Eeeewwww.
So to combat the large preprocessing industry, device manufacturers wanted patient's to consent to the use of re-sterilized and re-used equipment during their surgeries. Seems reasonable, right?
But this hasn't happened.
Imagine.
Now to be fair, I have been on both sides of this debate - I have worked at institutions that have re-sterilized instruments and I have worked at institutions that are single-use. I found that doctors are shoved into this debate unwittingly: we need the hospital to do our procedures and provide the instruments, but may not like having to use re-processed instruments on our patients. In the case of electrophysiology catheters - they just don't handle the same. Further, the thought that a patient is unaware of this practice is unsettling. Because of the nature of medicine these days, we assume the responsibility for the patient's well-being in tandem with the hospital. Yet often, we are not part of the discussion regarding the use of preprocessed instruments. If we are, then the whole murky area of what it took for doctors to agree to using these re-used catheters begins to raise its ugly head.
So while economic arguments exist on both sides of the device re-reprocessing fence, we must not lose sight that it's the patient that matters here. Certainly, if re-used instruments are being used in a laboratory, I believe that patients should be made aware and have this included in their informed consent, with any potential risks spelled out. Further, if a patient knew they could apply some of the cost savings of re-processing toward their procedure costs, then perhaps they'd be more willing to agree to the practice.
But the subterranean way things happen now is not acceptable.
Given the current satate of affairs, here's the ultimate litmus test on this issue in my book:
If you were having a procedure, which instrument(s) would you want used on yourself: re-processed or single-use?
-Wes
EKG Du Jour #3
It seems it's a slow news day in the field of Cardiology, so continuing the "EKG Hall of Fame" series, here comes the toughest diagnosis yet...
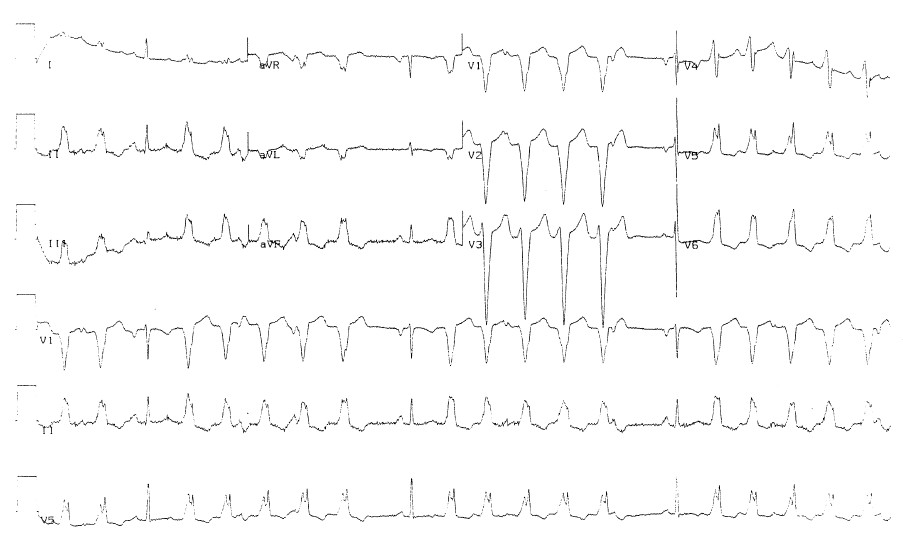
A 17 year old high school senior presents to the Emergency Room with intermittent shortness of breath and lightheadedness unrelated to exertion. He has never lost conciousness. He is otherwise "healthy" and is new to the health care system. He denies any recent illness, fever, cough, or history of lung disease. He has no family history of heart disease or unexpected death. His physical examination is completely normal and are the usual cauldron of ER blood tests. An EKG is obtained and you are called to review the EKG because the ER staff is "concerned." The EKG is shown below:

So, what's the diagnosis? If you're unsure, what other history, exam findings, test(s) would you order?
Finally, would you send him home or admit him?
-Wes
A 17 year old high school senior presents to the Emergency Room with intermittent shortness of breath and lightheadedness unrelated to exertion. He has never lost conciousness. He is otherwise "healthy" and is new to the health care system. He denies any recent illness, fever, cough, or history of lung disease. He has no family history of heart disease or unexpected death. His physical examination is completely normal and are the usual cauldron of ER blood tests. An EKG is obtained and you are called to review the EKG because the ER staff is "concerned." The EKG is shown below:

Click to Enlarge
So, what's the diagnosis? If you're unsure, what other history, exam findings, test(s) would you order?
Finally, would you send him home or admit him?
-Wes
Monday, March 17, 2008
They Missed Something
By causing the blood vessels that supply the heart to abruptly occlude, cocaine can also cause your heart to fibrillate (stop) resulting in
... and can happen before you ever get to an Emergency Room.
Any questions?
-Wes
| sudden | ||
| cardiac | ||
| death |
... and can happen before you ever get to an Emergency Room.
Any questions?
-Wes
Sunday, March 16, 2008
With Whom Will I Hang?
Yesterday's Chicago Tribune laid bare a troubling reality: Evanston Northwestern Healthcare (my institution) is in a spat with Northwestern University's Feinberg School of Medicine over some form of interesting affiliation fee. I had no idea there were such fees, but hey, I'm just a doctor. Guess you gotta pay to play.
I had never heard of Rosalind Franklin University of Medicine and Science until I read the article. It seems that's the new name they gave the old Chicago Medical School. I'm embarrassed to say that I had to use Google Maps to know where they were located. (I guess I don't get out very much. Yikes, it's smack dab in the Great Lakes Naval Training Center and the North Chicago VA - geez, guys, I just retired!)
Can't wait to catch the buzz tomorrow morning. I wonder if it has anything to do with this? Rumor has it that Northwestern University Medical Center downtown was interested in the Rush North Shore Medical Center acquisition, too.
-Wes
I had never heard of Rosalind Franklin University of Medicine and Science until I read the article. It seems that's the new name they gave the old Chicago Medical School. I'm embarrassed to say that I had to use Google Maps to know where they were located. (I guess I don't get out very much. Yikes, it's smack dab in the Great Lakes Naval Training Center and the North Chicago VA - geez, guys, I just retired!)
Can't wait to catch the buzz tomorrow morning. I wonder if it has anything to do with this? Rumor has it that Northwestern University Medical Center downtown was interested in the Rush North Shore Medical Center acquisition, too.
-Wes
A Call for Equipoise
My head is still reeling after the reports of doctors hacking into the wireless transmissions of an automatic defibrillator.
Oh, it’s not so much the fact that it was done. Really, that was something. It certainly took our best and brightest a remarkable amount of scientific expertise to reverse-engineer the protocol for communication with Medtronic’s defibrillator device. The resources they used and all – what was it? $30,000 or so? And how many hours did it take for those engineers and computer scientists to crack the code? Certainly many. I suppose we should congratulate them for their ingenuity and fortitude. I feel safer now.
But that’s not what I see as disturbing.
It’s the bigger picture that bothers me.
You see, I’m worried about what it means to our profession as doctors.
Doctors must continually strive for equipoise in medicine. While it is a noble cause to want to always cure disease, strive for perfect patient safety in all arenas, and help mankind progress to the ultimate prize of immortality, we realize that each of these goals, taken to their extreme, is an impossibility. We have to balance the inevitability and cruelty of disease, the social and political climates in which we work, and even the sometimes atrocious things that one human being does to another, to help the unfortunate patient, victims and family members cope with the reality of their medical predicaments.
To me, it seems that since the Institute of Medicine’s report on medical errors was published admonishing the safety record of medicine as a whole, we’ve begun tipping to one side of the scale of medical reality. We strive for perfect safety records and implement protocols analogous to airline checklists to become robotic and perfect in our actions. Mountains of paperwork and regulation requirements are completed by teams of well-meaning individuals each day. Countless hours are devoted to record-keeping to prove that we’ve been keeping our records. Electronic medical records spew forth past medical histories, medication lists, family histories, social histories time and time again not because it helps the patient, but because we don’t want to “miss anything” that might be perceived as “inadequate” documentation for the patient. (In reality, we just have to do that stupid requirement just to get paid adequately – but that’s a discussion for another essay.)
Now I have nothing against improving our health care delivery system, and Lord knows there are areas where the Institute of Medicine’s wakeup call has helped patients. But politically, we’ve already seen how neat and tidy the patient safety argument becomes. I mean, what compassionate physician in their right mind could ever not argue for patient safety? It would be professional suicide.
But exactly how safe is safe enough?
Should all surgeons, in their quest to minimize infection, scrub for 3 minutes, 5 minutes, 10 minutes, 30 minutes, or become obsessive hand washers in the interest of minimizing the possible spread of that last remaining bacterium from their hand before entering the operating room? When do we stop?
Or maybe, since defibrillator wireless transmissions can be tapped now, we should encrypt other wireless transmission devices, like entire telemetry units or hospital administrators’ cell phone conversations? Better yet, barricades should be erected around hospitals just in case a doctor goes ballistic and decides to crash an ambulance into the main building. And why aren’t there metal detectors and people checking shoes at all of the hospital entrances – aren’t we missing another potential patient safety opportunity?
Sure, these examples are extreme, but they illustrate my point.
We have so many incredibly difficult challenges ahead in medicine: funding of healthcare, the loss of primary care doctors, the social problems in our inner cities, the overcrowding of our emergency rooms – the list goes on and on. Be it cardiology, medicine, obstetrics, or neurology, or general surgery, etc. – each branch of our profession has a million more important clinical and non-clinical problems to tackle right now. But when we start looking for problems in areas that do not represent active problems, thereby creating a new problem where none existed previously, we begin to tip the balance of equipoise in medicine to the penurious. And when this scale is tipped too far toward one side, we completely miss the boat as a profession as what it will take to maintain our clear perspective in our upcoming challenges.
Our resources are finite. When we spend so much money on safety trivialities in our most esteemed medical education establishments relative to the Big Picture of healthcare today, all of us who proclaim to be purveyors of our patients’ best interests have completely dropped the ball.
-Wes
16 March 2008 19:00 CST Addendum: Roy Poses over at Health Care Renewal doesn't agree with me, but it's good to get both sides of the argument. What do you think?
Oh, it’s not so much the fact that it was done. Really, that was something. It certainly took our best and brightest a remarkable amount of scientific expertise to reverse-engineer the protocol for communication with Medtronic’s defibrillator device. The resources they used and all – what was it? $30,000 or so? And how many hours did it take for those engineers and computer scientists to crack the code? Certainly many. I suppose we should congratulate them for their ingenuity and fortitude. I feel safer now.
But that’s not what I see as disturbing.
It’s the bigger picture that bothers me.
You see, I’m worried about what it means to our profession as doctors.
Doctors must continually strive for equipoise in medicine. While it is a noble cause to want to always cure disease, strive for perfect patient safety in all arenas, and help mankind progress to the ultimate prize of immortality, we realize that each of these goals, taken to their extreme, is an impossibility. We have to balance the inevitability and cruelty of disease, the social and political climates in which we work, and even the sometimes atrocious things that one human being does to another, to help the unfortunate patient, victims and family members cope with the reality of their medical predicaments.
To me, it seems that since the Institute of Medicine’s report on medical errors was published admonishing the safety record of medicine as a whole, we’ve begun tipping to one side of the scale of medical reality. We strive for perfect safety records and implement protocols analogous to airline checklists to become robotic and perfect in our actions. Mountains of paperwork and regulation requirements are completed by teams of well-meaning individuals each day. Countless hours are devoted to record-keeping to prove that we’ve been keeping our records. Electronic medical records spew forth past medical histories, medication lists, family histories, social histories time and time again not because it helps the patient, but because we don’t want to “miss anything” that might be perceived as “inadequate” documentation for the patient. (In reality, we just have to do that stupid requirement just to get paid adequately – but that’s a discussion for another essay.)
Now I have nothing against improving our health care delivery system, and Lord knows there are areas where the Institute of Medicine’s wakeup call has helped patients. But politically, we’ve already seen how neat and tidy the patient safety argument becomes. I mean, what compassionate physician in their right mind could ever not argue for patient safety? It would be professional suicide.
But exactly how safe is safe enough?
Should all surgeons, in their quest to minimize infection, scrub for 3 minutes, 5 minutes, 10 minutes, 30 minutes, or become obsessive hand washers in the interest of minimizing the possible spread of that last remaining bacterium from their hand before entering the operating room? When do we stop?
Or maybe, since defibrillator wireless transmissions can be tapped now, we should encrypt other wireless transmission devices, like entire telemetry units or hospital administrators’ cell phone conversations? Better yet, barricades should be erected around hospitals just in case a doctor goes ballistic and decides to crash an ambulance into the main building. And why aren’t there metal detectors and people checking shoes at all of the hospital entrances – aren’t we missing another potential patient safety opportunity?
Sure, these examples are extreme, but they illustrate my point.
We have so many incredibly difficult challenges ahead in medicine: funding of healthcare, the loss of primary care doctors, the social problems in our inner cities, the overcrowding of our emergency rooms – the list goes on and on. Be it cardiology, medicine, obstetrics, or neurology, or general surgery, etc. – each branch of our profession has a million more important clinical and non-clinical problems to tackle right now. But when we start looking for problems in areas that do not represent active problems, thereby creating a new problem where none existed previously, we begin to tip the balance of equipoise in medicine to the penurious. And when this scale is tipped too far toward one side, we completely miss the boat as a profession as what it will take to maintain our clear perspective in our upcoming challenges.
Our resources are finite. When we spend so much money on safety trivialities in our most esteemed medical education establishments relative to the Big Picture of healthcare today, all of us who proclaim to be purveyors of our patients’ best interests have completely dropped the ball.
-Wes
16 March 2008 19:00 CST Addendum: Roy Poses over at Health Care Renewal doesn't agree with me, but it's good to get both sides of the argument. What do you think?
Saturday, March 15, 2008
Insurers and Doctors' Identity Theft
Dr. Val had a recent post describing "Medical Identity Theft." This is where a non-insured individual acquires the insurance information of another patient and uses this to rack up all kinds of health care bills while rendering the victimized patient virtually uninsurable later.
What she didn't tell us, though, was that some doctors have already been having a different form of identify theft: from their friendly, neighborhood managed care company.
What's that you say, Dr. Wes?
Well, remember those voluminous forms with all that personal insformation that you had to fill out to obtain insurance reimbursements? It took FOREVER to complete those forms. Entering your name, address, social security number, date of birth, Medicare UPIN number, DEA number, your state's controlled substance number, mother's maiden name (well, not really that one) on all of those forms sure was arduous, wasn't it?
But you complied and dutifully entered all of that information because you wanted to get paid by our omnipotent healthcare insurance system. In return, you were afforded the utmost confidence that your data (like that of your patients) would be held in strict confidence, remember?
Well, it seems there might have been a little problem.
It seems at least one managed care company who handles the military's health care program, HealthNet Federal Services, LLC, had a little security breach.
From their "Dear Doctor" letter:
But its okay. They'll offer you a free complimentary credit monitoring service absolutely free for 12 months and give you some online resources and phone numbers where you can get a free credit report!
Wow, what a deal!
Come on, doctors, what are you waiting for? Sign up NOW! You won't want to miss out on this exciting offer...
-Wes
What she didn't tell us, though, was that some doctors have already been having a different form of identify theft: from their friendly, neighborhood managed care company.
What's that you say, Dr. Wes?
Well, remember those voluminous forms with all that personal insformation that you had to fill out to obtain insurance reimbursements? It took FOREVER to complete those forms. Entering your name, address, social security number, date of birth, Medicare UPIN number, DEA number, your state's controlled substance number, mother's maiden name (well, not really that one) on all of those forms sure was arduous, wasn't it?
But you complied and dutifully entered all of that information because you wanted to get paid by our omnipotent healthcare insurance system. In return, you were afforded the utmost confidence that your data (like that of your patients) would be held in strict confidence, remember?
Well, it seems there might have been a little problem.
It seems at least one managed care company who handles the military's health care program, HealthNet Federal Services, LLC, had a little security breach.
From their "Dear Doctor" letter:
In late December 2007, Health Net was informed that this web file was accessed and may have included your name, provider address, and social security number. The specific information accessed includes providers' information that show dates of service between October 2005 through September 2006 with a TRICARE claim paid on or prior to October 2006.Oops.
But its okay. They'll offer you a free complimentary credit monitoring service absolutely free for 12 months and give you some online resources and phone numbers where you can get a free credit report!
Wow, what a deal!
Come on, doctors, what are you waiting for? Sign up NOW! You won't want to miss out on this exciting offer...
-Wes
Friday, March 14, 2008
Tabled
With no love lost between the two Democratic presidential candidates about health care mandates and such, so much for making patient safety the centerpiece of medical liability reform, huh?
Seems this "critical legislation" hasn't gone anywhere since 9/28/2005.
I guess this NEJM piece was nice window dressing - especially when we review the legal professions' contributions to the democratic candidates...
Sorry. It's just NOT about the patients, is it?
-Wes
Seems this "critical legislation" hasn't gone anywhere since 9/28/2005.
I guess this NEJM piece was nice window dressing - especially when we review the legal professions' contributions to the democratic candidates...
Sorry. It's just NOT about the patients, is it?
-Wes
Thursday, March 13, 2008
EKG Du Jour - #2
Over the years, there have been memorable cases that go into my teaching file - I call it my "EP Hall of Fame" file. One such case was presented earlier on this blog. These serve as a rich source of instructional material for my students, residents, fellows, and cardiology colleagues, so I thought I'd share a case with the blog-o-sphere. These are not particularly tough for most electrophysiologists, but I find its helpful to review these cases once in a while to remind our colleagues to be on the lookout for these not-so-uncommon arrhythmias.
She was a 42-year old mother of three children who presented with a chief complaint of exertional shortness of breath and progressive swelling of her lower extremities for the past two months. She could not lie flat at night and required three pillows to sleep comfortably. She never had syncope or near syncope, but did note lightheadedness if standing quickly from a sitting position. She had no family history of heart disease or sudden death. She was on no medications, did not drink alcohol, smoke, or use illicit substances.
Her physical examination showed a rapid, irregular pulse of about 120 b/min and a blood pressure of 94/62, jugulovenous distention to the angle of her jaw at 30 degrees, and bilateral rales half-way up both lung fields. She had moderate lower extremity edema. Here's her EKG:
She was admitted and placed on telemetry, a 60-minute strip from which is shown here:
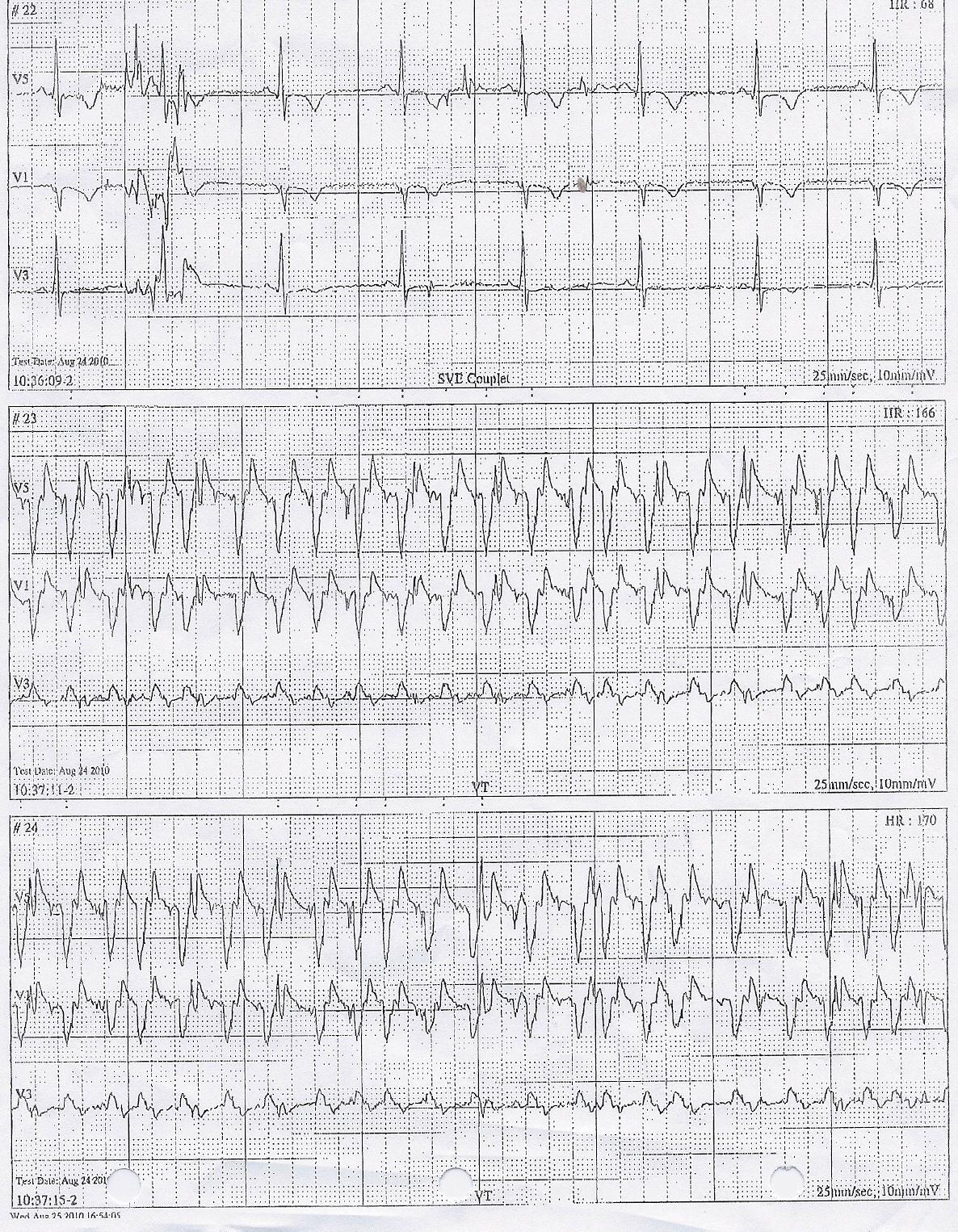
Her echo demonstrated a markedly dilated right and left ventricle with moderate-to-severe mitral regurgitation and left atrial enlargement. Her estimated ejection fraction was 22%.
Sooooo. What is this and what therapy (therapies) would you recommend?
-Wes
She was a 42-year old mother of three children who presented with a chief complaint of exertional shortness of breath and progressive swelling of her lower extremities for the past two months. She could not lie flat at night and required three pillows to sleep comfortably. She never had syncope or near syncope, but did note lightheadedness if standing quickly from a sitting position. She had no family history of heart disease or sudden death. She was on no medications, did not drink alcohol, smoke, or use illicit substances.
Her physical examination showed a rapid, irregular pulse of about 120 b/min and a blood pressure of 94/62, jugulovenous distention to the angle of her jaw at 30 degrees, and bilateral rales half-way up both lung fields. She had moderate lower extremity edema. Here's her EKG:
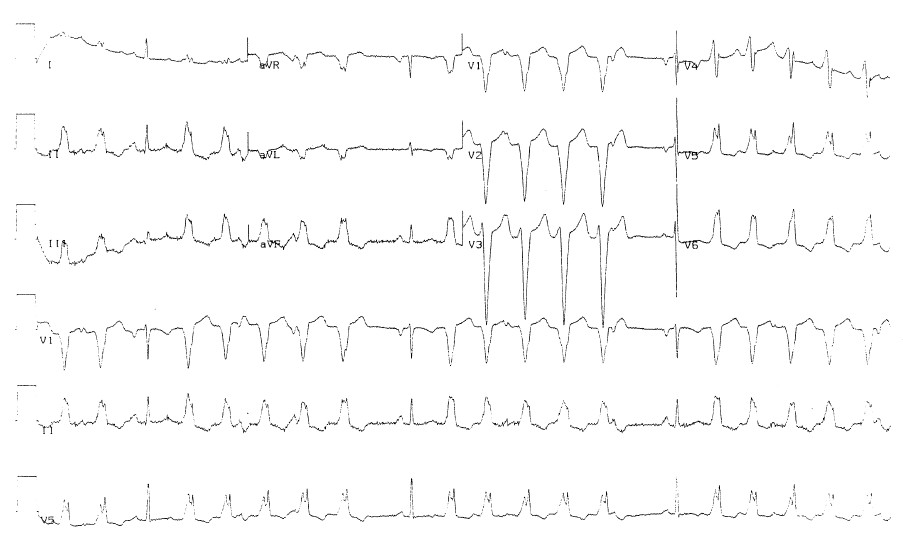
Click to Enlarge
She was admitted and placed on telemetry, a 60-minute strip from which is shown here:
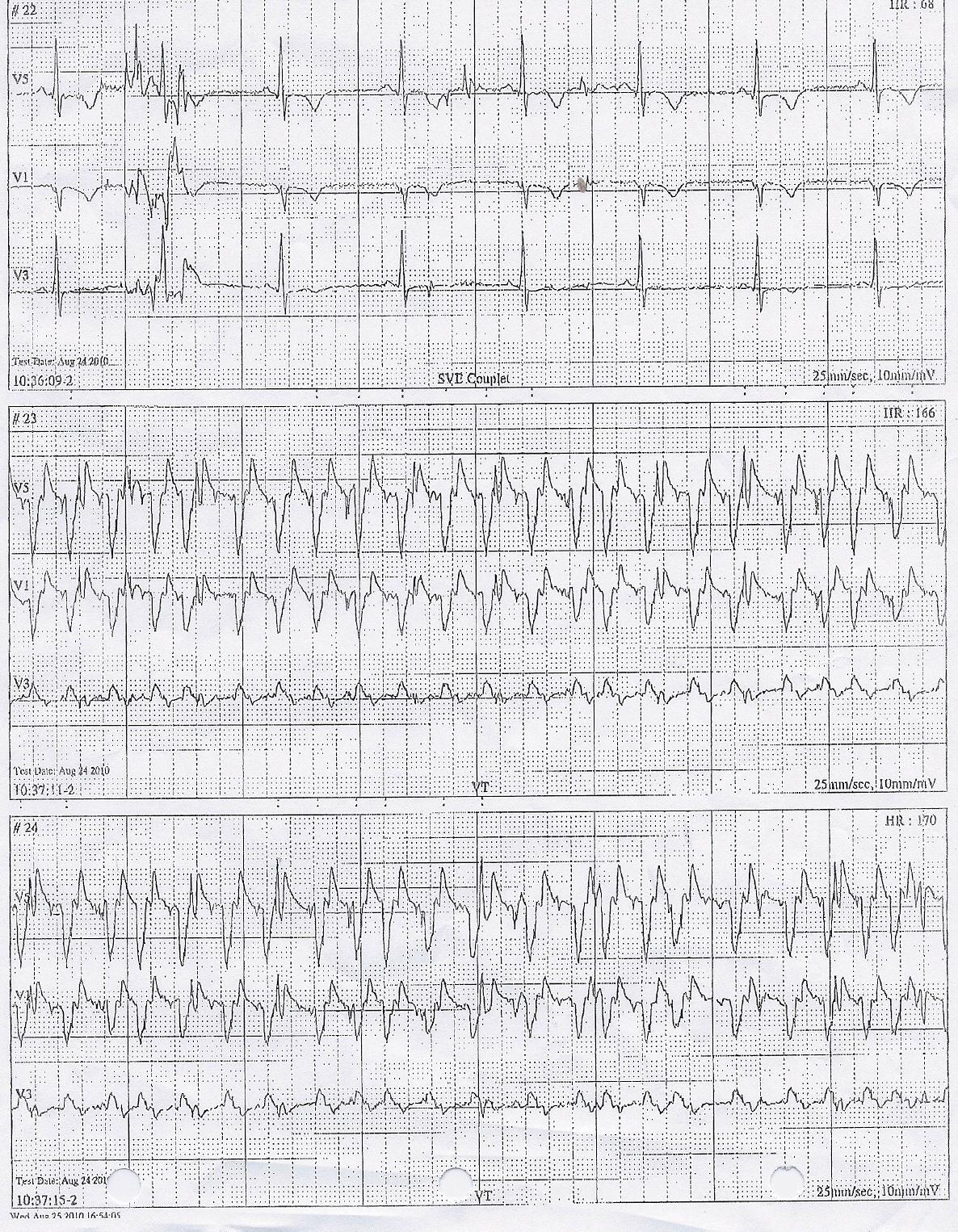
Click to Enlarge
Her echo demonstrated a markedly dilated right and left ventricle with moderate-to-severe mitral regurgitation and left atrial enlargement. Her estimated ejection fraction was 22%.
Sooooo. What is this and what therapy (therapies) would you recommend?
-Wes
Getting A Blog Off the Ground
Thinking about starting a blog? Here are some brief thoughts of mine published in the February issue of EP Lab Digest.
-Wes
-Wes
Wednesday, March 12, 2008
Medical Terrorism
Maybe the New York Times Sunday crossword puzzle got too easy for Dr. William Maisel.
Fishing about for another amusement, Dr. Maisel from Harvard Medical School, stumbled upon another corporate vulnerability and decided to hire some engineers to hack defibrillator wireless transmissions.
I mean fun is fun, right?
Just think of the buzz sitting before all of those AP press interviews. I wonder if he fancies himself the David taking on the Goliaths. And what better way, than to terrorize the general population who have already had the misfortune of having an implantable cardiac defibrillator installed:
Amazing. A computer scientist who’s never been asked to confront his mortality or and heart-related issue becomes the latest spokesperson for our next cardiovascular public safety nightmare. Lets leave medical terrorism to the nightly news and the tabloids. But I guess it's too much to ask the Wall Street Journal to exercise some restraint.
Oh, my God! PACEMAKERS AND DEFIBRILLATORS ARE LETHAL, PEOPLE! RUN FOR YOUR LIVES!
But then again, safety Nazis aren’t on the front line of patient care, are they?
Why doesn’t the press interview a few people who’s lives have been saved, time and time again, by these devices? Why don’t we hear about the constant monitoring these wireless transmissions permit to ASSURE the patient’s safety and well-being as impedance monitoring is performed automatically each night?
No, we’ll never hear about this. We’ll only hear about death, destruction, and chaos.
After all, medical terrorism sells.
-Wes
12 Mar 2008 1310 PM CST Addendum: The link to the paper as reported by the now widely publicized, self-aggrandizing "Medical Device Security Center."
Fishing about for another amusement, Dr. Maisel from Harvard Medical School, stumbled upon another corporate vulnerability and decided to hire some engineers to hack defibrillator wireless transmissions.
I mean fun is fun, right?
Just think of the buzz sitting before all of those AP press interviews. I wonder if he fancies himself the David taking on the Goliaths. And what better way, than to terrorize the general population who have already had the misfortune of having an implantable cardiac defibrillator installed:
Dr. Maisel and his collaborators -- Kevin Fu of the University of Massachusetts, and Tadayoshi Kohno of the University of Washington, both computer-science professors (editor's note: and co-authors) -- emphasized that the findings are as yet limited to one model of defibrillator made by Medtronic. They informed the Food and Drug Administration last month, they said.And then the press, in their ever sensationalist effort to find the next health care safety crisis, lept to interview computer scientists who proclaimed, “I find it absolutely terrifying, the idea of having a computer-controlled devices implanted in us.”
Amazing. A computer scientist who’s never been asked to confront his mortality or and heart-related issue becomes the latest spokesperson for our next cardiovascular public safety nightmare. Lets leave medical terrorism to the nightly news and the tabloids. But I guess it's too much to ask the Wall Street Journal to exercise some restraint.
Oh, my God! PACEMAKERS AND DEFIBRILLATORS ARE LETHAL, PEOPLE! RUN FOR YOUR LIVES!
But then again, safety Nazis aren’t on the front line of patient care, are they?
Why doesn’t the press interview a few people who’s lives have been saved, time and time again, by these devices? Why don’t we hear about the constant monitoring these wireless transmissions permit to ASSURE the patient’s safety and well-being as impedance monitoring is performed automatically each night?
No, we’ll never hear about this. We’ll only hear about death, destruction, and chaos.
After all, medical terrorism sells.
-Wes
12 Mar 2008 1310 PM CST Addendum: The link to the paper as reported by the now widely publicized, self-aggrandizing "Medical Device Security Center."
Tuesday, March 11, 2008
Taken Too Early
Tonight the room is filled with your friends and colleagues, relatives and husband. Words seemed so trite.
We looked at pictures and saw a young girl at her birthdays with glorious eyes that beamed as a piece of cake clutched tightly squirts icing through her tender fingers. Or others of a young girl wrapped in her father’s arms with a can of mosquito spray – was it her first campout? Or sitting with those jeans on a fence outside a barn, or smiling with a graduation cap beside a school, a mother by her side. More birthdays. Graduations. A wedding album. A kiss. Happy times with a smile - always a smile – radiant, stunning. “She was beautiful inside and out,” I kept hearing.
Yes, you were.
I learned tonight that the diagnosis came in 1996. You were only 28. Your nursing colleagues were not sure what to say. But there in the scrapbook of pictures from earlier days was a picture of a pair of gauze panties from the OB ward stretched between IV poles for a game of volleyball on the ward during the late shift anyway. Was that your idea?
Two years later: more bad news – your spine. Why? No matter, it seemed. You became an Advanced Practice Nurse anyway. It was all you wanted to do. Help others, stay productive, touch people.
I met you in 2001, completely unaware. That’s how you were. Gracious, compassionate, professional, caring. I know why now. I was so naïve. Your perspective was crystal clear and level-headed; mine, rose-colored. It was not until you lost your hair that I learned of your struggle. But your smile persisted; you came to work every chance you could, made rounds, returned phone calls, kept going until you just got too tired. Your husband told me tonight that that was the part that hurt you the most – when you couldn’t work anymore – damn.
Beneath the flowers, there you were tonight, kind of. I was glad I could say goodbye. It was a lovely dress, but the torn jeans pocket laid on your dress with a note to “Teresa” said it all. Damn, you were special!
So carry on, dear friend. Make sure those wards up there are humming. Keep 'em laughing and smiling, just as you did down here. And as we say in the Navy:
Fair winds, following seas, and may the peace of the Lord always be with you.
-Wes
We looked at pictures and saw a young girl at her birthdays with glorious eyes that beamed as a piece of cake clutched tightly squirts icing through her tender fingers. Or others of a young girl wrapped in her father’s arms with a can of mosquito spray – was it her first campout? Or sitting with those jeans on a fence outside a barn, or smiling with a graduation cap beside a school, a mother by her side. More birthdays. Graduations. A wedding album. A kiss. Happy times with a smile - always a smile – radiant, stunning. “She was beautiful inside and out,” I kept hearing.
Yes, you were.
I learned tonight that the diagnosis came in 1996. You were only 28. Your nursing colleagues were not sure what to say. But there in the scrapbook of pictures from earlier days was a picture of a pair of gauze panties from the OB ward stretched between IV poles for a game of volleyball on the ward during the late shift anyway. Was that your idea?
Two years later: more bad news – your spine. Why? No matter, it seemed. You became an Advanced Practice Nurse anyway. It was all you wanted to do. Help others, stay productive, touch people.
I met you in 2001, completely unaware. That’s how you were. Gracious, compassionate, professional, caring. I know why now. I was so naïve. Your perspective was crystal clear and level-headed; mine, rose-colored. It was not until you lost your hair that I learned of your struggle. But your smile persisted; you came to work every chance you could, made rounds, returned phone calls, kept going until you just got too tired. Your husband told me tonight that that was the part that hurt you the most – when you couldn’t work anymore – damn.
Beneath the flowers, there you were tonight, kind of. I was glad I could say goodbye. It was a lovely dress, but the torn jeans pocket laid on your dress with a note to “Teresa” said it all. Damn, you were special!
So carry on, dear friend. Make sure those wards up there are humming. Keep 'em laughing and smiling, just as you did down here. And as we say in the Navy:
Fair winds, following seas, and may the peace of the Lord always be with you.
-Wes
Lotteries to Ration Healthcare
Seems Oregon is on to something: if it's free it's for me!
98% get stiffed.
Sad, but true.
But at least overt rationing by way of a lottery vividly highlights the magnitude of our current healthcare cost crisis. Imagine when the remaining 98% are picked up by good 'ol Uncle Sam.
If Oregon can't afford it, how will we?
-Wes
Officials began drawing names last week for a chance at some rare openings in the state's healthcare plan.Now, let's say that "a few thousand people" really means about 2,000 people. If so, Oregon can provide only a little over 2% of the outstanding healthcare needs via their state's healthcare plan.
Announced in February, the lottery drew 91,675 hopefuls in 30 days. The winners will receive a postcard notifying them that they can apply for the Oregon Health Plan.
Like millions of people across the country, cash-strapped Oregonians bypass doctors, forgo prescription drugs and neglect basic healthcare when they can't afford health insurance. The state's Department of Human Services says at least 600,000 Oregonians live day to day without health insurance.
For some, life or death could hinge on the outcome of the unique insurance lottery.
Budget limitations capped the Oregon Health Plan standard benefit package in mid-2004. Now the plan has room for a few thousand people. The lottery winners will be the first new applicants since the cap was imposed.
Oregon's standard plan covers physician services, prescription drugs, mental health and chemical dependency services, emergency medical services, and limited dental, hospital and vision benefits. Premiums range from zero to $20.
98% get stiffed.
Sad, but true.
But at least overt rationing by way of a lottery vividly highlights the magnitude of our current healthcare cost crisis. Imagine when the remaining 98% are picked up by good 'ol Uncle Sam.
If Oregon can't afford it, how will we?
-Wes
RA Drugs for the Heart?
Although rheumatoid arthritis drugs (including glucocorticoids, conventional disease-modifying antirheumatic drugs (DMARDs), and biologic agents) were associated with significant 8% to 58% reductions in the risk of the developing heart attacks, strokes, and cardiovascular disease in one poorly-controlled international study, there might be other side effects that preclude their widespread use.
Here's just one reason I'd never consider using this therapy to prevent heart disease or stroke.
If that doesn't make your stomach turn, I'd don't know what will...
-Wes
Here's just one reason I'd never consider using this therapy to prevent heart disease or stroke.
If that doesn't make your stomach turn, I'd don't know what will...
-Wes
Monday, March 10, 2008
A New Blog
A future new medical student at Northwestern medical school, Matthew E. Nolan, enters the blog-o-sphere with "The Natural Condition."
Well written, interesting stuff.
Stop by and say "hi" and "congrats!"
-Wes
Well written, interesting stuff.
Stop by and say "hi" and "congrats!"
-Wes
Oops, We Did It Again
Free care might not always lead to more care, for one simple reason: cost.
Government-run healthcare ...
... be careful what you ask for.
Instead of asking where the other $0.66 went, these clever doctors, always interested in maintaining their livelihood (who can blaim them?) and understanding the system, do what any well-meaning group in this system would do: ask the government for more money!
Oops, we're doin' it again!
-Wes
Addendum 09:45AM CST: One more thought: Hey, if we don't care about costs, it's almost funny that the state can find a billion dollars for a single new children's hospital, but can't find $75 million to supplement doctors' fees.
At issue is the amount of reimbursement pediatric specialists get from state and federal funds after treating a child insured under Medicaid or the All Kids program, which uses Medicaid funds. Currently, Illinois specialists said, they are repaid just 33 cents for every dollar they spend on such patients, one of the lowest reimbursement rates in the country.Now I really don't want to attract more specialists to our state (so that argument falls flat with me), but the mass exodus of doctors to other states is a consistent finding in states where doctors cannot economically maintain practices. After all, how long would any business last that received $0.33 for every $1 it spends providing their service?
Physicians worry the increasing gap between medical costs and Medicaid reimbursement rates will make it more difficult to attract new pediatric specialists to the state. Many also worry specialists will leave Illinois or stop accepting children who are covered by Medicaid or All Kids.
Government-run healthcare ...
... be careful what you ask for.
Instead of asking where the other $0.66 went, these clever doctors, always interested in maintaining their livelihood (who can blaim them?) and understanding the system, do what any well-meaning group in this system would do: ask the government for more money!
Physicians hope legislation submitted to the Illinois General Assembly will help bring reimbursements closer to costs, allowing pediatric specialists, among other practices, to continue seeing All Kids and Medicaid patients.Who do you think will pay the bill?
But adjustments for pediatric specialists alone could cost the state $75 million, said George Hovanec, former state Medicaid director who is a consultant for Children's Memorial Hospital.
Oops, we're doin' it again!
-Wes
Addendum 09:45AM CST: One more thought: Hey, if we don't care about costs, it's almost funny that the state can find a billion dollars for a single new children's hospital, but can't find $75 million to supplement doctors' fees.
Friday, March 07, 2008
A Conversation I Never Want to Have
Mr. Smith, welcome back to the real world!
Did you know that your heart stopped earlier today, but thanks to your friendly neighborhood paramedic and a handy-dandy AED, we got it going again?
Amazing, huh?
We've done an extensive evaluation of your medical condition, Mr. Smith, and we think you need to have and ICD implanted.
What's that? Oh, an "ICD" is short for a implantable cardioverter defibrillator. It's a little device we implant under your skin that is attached to special wires we place in your heart that monitors your heart rhythm, so that should this happen again, the device can automatically detect, charge, and shock your heart back to normal rhythm lickety split.
Sound good? Great!
Now, a few things I need to ask you: we have three main manufacturers that make these devices here in the US: Medtronic, Boston Scientific, and St. Jude Medical. If those don't sound good, you can alternatively have us special-order you a device from Germany called a Biotronik device. It might cost you a bit more and I'm not sure there will always be a rep available to help check the device, but hey, we want to keep you well informed about ALL possibilities. Any preference?
What's that you say, you're not sure? Well, here's some more information:
The safety record for each of these manufacturers has been pretty good, but once in a while there have been some problems with recalls of leads and batteries of these devices. When this happens, believe it or not these suckers can explode inside your chest with lots of great big shocks and maybe even kill you. I'm not kidding. Really. Now admittedly this happens infrequently, but hey, I just want you to know about this. We want you informed. There's even legal action pending against all of the manufacturers. Did you know this? Now the FDA has all kinds of requirements that they make these device companies jump through, but you know, they've been a bit short-staffed lately. But they're getting stricker now. I mean they check everything now - heck new products? Well, they're still checking out the old ones. Oh, and those overseas plants that make parts? Well the FDA has to keep checking those too.
How often are there problems? Well, I'm so glad you asked!
Here's the manufacturers' published safety statistics for Boston Scientific, Medtronic, St. Jude. Study this information carefully. I really don't want you making the wrong decision! What's that you say? You're not sure if you should have one? But the data are so CLEAR!
Oh well, that's your decision, Mr. Smith. Never mind that you saw God earlier today.
Hey, at least I feel good you're now COMPLETELY informed!
* * *
It's easy to criticize our current system of checks and balances for medical device safety, as William H. Maisel, MD, MPH does so well in the New England Journal of Medicine this week. And while he makes some good points about the need for consideration of better overview of pre-release testing of new devices to the market, can we really expect that patients can understand all of the implications of ICD type, safety information, and implications for their care just after they've suffered an episode of aborted sudden death?
With remarkable failure to acknowledge efforts by the FDA, Heart Rhythm Society, and manufacturers already underway to improve post-market performance evaluations, he writes:
Certainly, we should always strive for improved patient safety. But to suggest that efforts are not underway to assure timely reporting of post-market performance analysis flies in the face of the many countless individuals who have devoted huge personal effort and resources to continually improve this endeavor.
Maybe, just maybe, we should empower the doctors to present the data to the patient, rather than impose more governmental regulation.
No. I forgot.
In the medicine of today, bureaucracy always wins.
-Wes
Did you know that your heart stopped earlier today, but thanks to your friendly neighborhood paramedic and a handy-dandy AED, we got it going again?
Amazing, huh?
We've done an extensive evaluation of your medical condition, Mr. Smith, and we think you need to have and ICD implanted.
What's that? Oh, an "ICD" is short for a implantable cardioverter defibrillator. It's a little device we implant under your skin that is attached to special wires we place in your heart that monitors your heart rhythm, so that should this happen again, the device can automatically detect, charge, and shock your heart back to normal rhythm lickety split.
Sound good? Great!
Now, a few things I need to ask you: we have three main manufacturers that make these devices here in the US: Medtronic, Boston Scientific, and St. Jude Medical. If those don't sound good, you can alternatively have us special-order you a device from Germany called a Biotronik device. It might cost you a bit more and I'm not sure there will always be a rep available to help check the device, but hey, we want to keep you well informed about ALL possibilities. Any preference?
What's that you say, you're not sure? Well, here's some more information:
The safety record for each of these manufacturers has been pretty good, but once in a while there have been some problems with recalls of leads and batteries of these devices. When this happens, believe it or not these suckers can explode inside your chest with lots of great big shocks and maybe even kill you. I'm not kidding. Really. Now admittedly this happens infrequently, but hey, I just want you to know about this. We want you informed. There's even legal action pending against all of the manufacturers. Did you know this? Now the FDA has all kinds of requirements that they make these device companies jump through, but you know, they've been a bit short-staffed lately. But they're getting stricker now. I mean they check everything now - heck new products? Well, they're still checking out the old ones. Oh, and those overseas plants that make parts? Well the FDA has to keep checking those too.
How often are there problems? Well, I'm so glad you asked!
Here's the manufacturers' published safety statistics for Boston Scientific, Medtronic, St. Jude. Study this information carefully. I really don't want you making the wrong decision! What's that you say? You're not sure if you should have one? But the data are so CLEAR!
Oh well, that's your decision, Mr. Smith. Never mind that you saw God earlier today.
Hey, at least I feel good you're now COMPLETELY informed!
It's easy to criticize our current system of checks and balances for medical device safety, as William H. Maisel, MD, MPH does so well in the New England Journal of Medicine this week. And while he makes some good points about the need for consideration of better overview of pre-release testing of new devices to the market, can we really expect that patients can understand all of the implications of ICD type, safety information, and implications for their care just after they've suffered an episode of aborted sudden death?
With remarkable failure to acknowledge efforts by the FDA, Heart Rhythm Society, and manufacturers already underway to improve post-market performance evaluations, he writes:
According to its mission statement, the FDA is "responsible for protecting the public health" and for "helping the public get the accurate, science-based information they need." Unfortunately, the agency is failing to fulfill that mission. In 1998, the Advisory Commission on Consumer Protection and Quality in the Health Care Industry adopted a Patients' Bill of Rights whose primary tenet is that patients have "the right to receive accurate, easily understood information to assist them in making informed decisions." Regrettably, patients considering implantation of medical devices often fail to receive critical information on device safety.Should patients be faced with all available safety information when they present as the fictional patient above does? And what about the product performance report references that are already published, updated quarterly, and available on the web? Should they be given the opportunity to scour these data before signing their surgical consents? Should the data be updated weekly? Will patients be able to understand these data and the nuances of the recalls underway? How much more "safety data" will patient's need to absorb to meet Dr. Maisel's expectations for full "disclosure?"
Certainly, we should always strive for improved patient safety. But to suggest that efforts are not underway to assure timely reporting of post-market performance analysis flies in the face of the many countless individuals who have devoted huge personal effort and resources to continually improve this endeavor.
Maybe, just maybe, we should empower the doctors to present the data to the patient, rather than impose more governmental regulation.
No. I forgot.
In the medicine of today, bureaucracy always wins.
-Wes
Thursday, March 06, 2008
PFO Closure and Migraines
There has been a remarkable amount of excitement about closing patent foramen ovales (PFO's) or larger atrial septal defects (ASDs) to cure intractable migrane headaches based on observational studies, and many, many companies have rushed to develop devices for this indication.
This week's Circulation (on-line version) released the much anticipated MIST trial (Migraine Intervention With STARFlex Technology) results which randomized 147 patients with a moderate to large PFOs between implantation of a STARFlex PFO closure device and a sham (or placebo) procedure.
The study's primary efficacy end point was migraine headache cessation during the analysis phase. It was derived from diary data.
Secondary efficacy comparisons were incidence of migraine during the healing phase; change in the severity of migraine attacks based on MIDAS (over a 3-month retrospective period) and headache impact test (HIT-6) (over a 1-month retrospective period) scores; change in the frequency of migraine attacks other than elimination of attacks; change in the characteristics of migraine (with or without aura and change thereof); change in the severity, frequency, and character of migraine relative to effective closure rate or presence of residual leak; and change in quality of life based on the SF-36v2 questionnaire (over a 1-month retrospective period).
The bottom line? The authors concluded that "no significant effect was found for primary or secondary end points."
Ouch.
To be fair, this was a tough group to fix: all had lots and lots of migraine headaches that were refractory to multiple medical therapies. The authors also note that the study was "underpowered" to show such a difference (do I sense backpedaling??) and the there was a trend toward fewer hours of headache experienced in the treatment group. The investigators want us to wait for the longer-term MIST-III trial results.
But the scuttlebutt doesn't stop there with this trial. Oh, no.
It is interesting that the study's prior "co-principle investigator's" name does not appear on the author list for this manuscript. Wow.
Last year at TCT 2007, Peter Wilmshurst,MD claimed there was data mismanagement over this trial and that perhaps the reason the study was negative was because of the poor performance of the device:
Clearly, the definitive jury about migraines and PFO closure is still out, but there are still many other trials (including MIST-III, PREMIUM and ESCAPE) pending with other companies devices, so hopefully more data will be forthcoming soon.
One thing's for sure, though, the MIST-I results will be a headache for gaining FDA approval of future devices without a clear headache improvement and more comprehensive residual interatrial shunt data to back up the observations.
-Wes
Image reference.
12 Mar 08 Addendum: More analysis on the MIST trial is available from theHeart.org (registration required).
This week's Circulation (on-line version) released the much anticipated MIST trial (Migraine Intervention With STARFlex Technology) results which randomized 147 patients with a moderate to large PFOs between implantation of a STARFlex PFO closure device and a sham (or placebo) procedure.
The study's primary efficacy end point was migraine headache cessation during the analysis phase. It was derived from diary data.
Secondary efficacy comparisons were incidence of migraine during the healing phase; change in the severity of migraine attacks based on MIDAS (over a 3-month retrospective period) and headache impact test (HIT-6) (over a 1-month retrospective period) scores; change in the frequency of migraine attacks other than elimination of attacks; change in the characteristics of migraine (with or without aura and change thereof); change in the severity, frequency, and character of migraine relative to effective closure rate or presence of residual leak; and change in quality of life based on the SF-36v2 questionnaire (over a 1-month retrospective period).

The bottom line? The authors concluded that "no significant effect was found for primary or secondary end points."
Ouch.
To be fair, this was a tough group to fix: all had lots and lots of migraine headaches that were refractory to multiple medical therapies. The authors also note that the study was "underpowered" to show such a difference (do I sense backpedaling??) and the there was a trend toward fewer hours of headache experienced in the treatment group. The investigators want us to wait for the longer-term MIST-III trial results.
But the scuttlebutt doesn't stop there with this trial. Oh, no.
It is interesting that the study's prior "co-principle investigator's" name does not appear on the author list for this manuscript. Wow.
Last year at TCT 2007, Peter Wilmshurst,MD claimed there was data mismanagement over this trial and that perhaps the reason the study was negative was because of the poor performance of the device:
At the TCT 2007 meeting last week, Dowson reported that the closure success rate was 94%, according to the implanting physician--in other words, a residual shunt rate of just 6% for the trial. Wilmshurst's review of the echocardiograms, however, suggested that the residual shunt rate was far higher--approximately one-third of the echocardiograms--a number he says was rejected by NMT, which then had the echocardiograms reviewed again, by the data monitor, Dr Luke Missault (St Jan Hospital, Brugges, Belgium). That second review, says Wilmshurst, who also sits on the steering committee for MIST, was statistically consistent with his own review. Wilmshurst states that all communications with NMT ground to a halt after he told the company the results of his review of the residual shunts. Ironically, while a higher rate of residual shunts would help explain the negative outcome in MIST, it has much larger implications for a device already marketed in Europe for the treatment of cryptogenic stroke.The author's and manufacturer's decision not to report the effectiveness of residual interatrial shunt data following ASD closure is troubling, given the controversy.
Clearly, the definitive jury about migraines and PFO closure is still out, but there are still many other trials (including MIST-III, PREMIUM and ESCAPE) pending with other companies devices, so hopefully more data will be forthcoming soon.
One thing's for sure, though, the MIST-I results will be a headache for gaining FDA approval of future devices without a clear headache improvement and more comprehensive residual interatrial shunt data to back up the observations.
-Wes
Image reference.
12 Mar 08 Addendum: More analysis on the MIST trial is available from theHeart.org (registration required).
The Baxter Heparin Recall
Thanks to the previous post's commenter who asked for a brief note regarding the recent Baxter pharmaceutical heparin recall. Today's Chicago Tribune front page story suggested that an unknown contaminant was possibly added to the heparin. While this makes for all kinds of intrigue, it seems to me that the authors forgot one important issue: what hospitals are doing with heparin availability in the meantime.
First, it is important to note that the recalled heparin is only in the higher dose concentrations. Importantly, other heparin is available from other manufacturers, though it might be less abundant. So I called our pharmacists, and they were nice enough to send on these steps we're implementing:
-Wes
First, it is important to note that the recalled heparin is only in the higher dose concentrations. Importantly, other heparin is available from other manufacturers, though it might be less abundant. So I called our pharmacists, and they were nice enough to send on these steps we're implementing:
"Because of this recall we anticipate at least several weeks of short supply as other manufacturers work to get more product to the market. This will impact Evanston Northwestern Healthcare in the following ways:Glad to see my atrial fibrillation ablation procedures can continue...
- Patients on a heparin nomogram with boluses: If a bolus dose of heparin is needed based on the aPTT result, the nurse must contact pharmacy to dispense the bolus. Pharmacy will be drawing up patient specific bolus doses to conserve available stock. Vials of heparin have been removed from general nursing unit Pyxis machines.
- Use of standard heparin for VTE prophylaxis. This strength will be in particularly short supply. Pharmacists will be working with physicians to try to convert as many patients as possible to other prophylaxis measures, e.g., Lovenox (enoxaparin). In addition, the pharmacy will be dispensing the standard heparin prophylaxis doses from the central pharmacy as syringes after our vial stock runs out.
- Several treatment areas that require heparin urgently will continue to have stock in Pyxis or floorstock as usual, however please be aware that it may look different than you may be used to. As always, please be sure to read medication labels carefully. The pharmacy department will be communicating with these areas as we become aware of any changes to products stocked."
-Wes
Wednesday, March 05, 2008
Speed Record
Clocked at 352 beats per minute (at it's fastest), this is a recording from a event recorder I saw today (used with permission). Note the small inverted triangle is a marker denoting when the patient pushed the button on the event recorder. The patient was a "little lightheaded" when this occurred:



So, what is this?
-Wes



Click to enlarge
So, what is this?
-Wes
Tuesday, March 04, 2008
HIPAA's Worthless and Here's Why
Do you have disability insurance? Do you want to utilize it? Well, my friend, if you want to tap into the disability coffers, plan on surrendering your privacy and sign this "Medical Disclosure Authorization." It gives our special "Medical Disability Advisor" the right to transmit to the world your persoanl and medical history (including HIV status), HIPAA free!
Welcome to the world of "Insurance Catch-22."
So why the heck do we even have HIPAA when insurers can play this game with our most private healthcare information?
-Wes
I understand that any health information disclosed pursuant to this authorization will no longer be protected by the HIPAA Privacy Rule when received by Reed Group.I received this request to complete an "Attending Physician's Statement" for a patient to receive their disability insurance. It had this form attached (not yet signed by the patient). As we can clearly see, this patient's healthcare record will be "free and clear" from a HIPAA perspective if this patient signs this "Medical Disclosure Authorization." Everything and anything about their health is fair game... forever. Both this patient's employer and future insurers can use this information against this patient for any future claims (even if their health problem is resolved). Yet if this patient does not sign this form, then this patient will not likely receive the benefits for which this patient has paid for through deductions from their salary.
When relevant to my claim, Reed Group may re-disclose(without further authorization) this information to any of the following, (a)Any person or facility that attends, treats or examines me; (b) Any person or facility that impacts the determination of my claim or that coordinates my benefits, including without limitation the employer to the extent permitted by state or federal law; or (c) The Social Security Administration or a social security or vocational rehabilitation vendor. Reed Group and DePaul University may use information obtained pursuant to this authorization in any other claim matter they handle related to me. I understand that this authorization is necessary for the processing of my claim or reguest for medical restrictions and that failure to sign this authorization may impair or impede the processing of my claim or request for medical restrictions.
I understand my treatment provider will not base treatment, payment enrollment or eligibitity on the refusal to sign this authorization. However, I understand that such refusal may affect my eligibility for benefits under my employers disability policy.
Welcome to the world of "Insurance Catch-22."
So why the heck do we even have HIPAA when insurers can play this game with our most private healthcare information?
-Wes
Monday, March 03, 2008
The Medical Record Emergency
File this under, "You get more with honey than with vinegar" or "Former-Chicago alderman goes wild:"
-Wes
The fracas unfolded in the emergency room's waiting area.Ms. Tillman learned an important lesson: never, ever mess with a nursing supervisor.
Tillman had taken her aunt, Mabel Barker, to the emergency room the previous evening. Frustrated by an overnight stay that she said yielded little treatment, Tillman requested the medical records when hospital officials discharged Barker.
She said she hoped to take her aunt to another hospital for treatment. Tillman said she was told the records were not immediately available. Barker received the same reply when she asked, Tillman said.
Jackson Hospital policy requires that requests for medical records be made in writing, spokesman Peter Frohmader said.
Unfazed, Tillman said she continued to request the records. A nursing supervisor alerted hospital security. They in turn notified police officers when they could not subdue Tillman, according to police and hospital officials.
"She was very disorderly with hospital security, and they asked her several times to leave the building," Cook said.
Tillman disputed such characterizations, saying she was mindful of not upsetting her aunt.
"I don't think I was screaming. I didn't go like crazy, crazy," Tillman said. "My only concern was to get some treatment for my aunt."
Tillman said she was arrested and put in "leg chains and shackles."
"It was really something," Tillman said. "They did the real police thing."
-Wes
Aim High
Aim So High You'll Never Be Bored...
The
greatest waste
of our
natural resources
is the
number of
people
who never
achieve their
potential.
Get out
of that
slow lane.
Shift
into that
fast lane.
If you think
you can't,
you won't.
If you think
you can,
there's a
good chance
you will.
Even making
the effort
will make
you feel
like a new
person.
Reputations
are made
by searching
for things that
can 't be done
and doing them.
Aim low:
boring.
Aim high:
soaring.
Best of luck on your last audition for college today, buddy.
-Wes
The
greatest waste
of our
natural resources
is the
number of
people
who never
achieve their
potential.
Get out
of that
slow lane.
Shift
into that
fast lane.
If you think
you can't,
you won't.
If you think
you can,
there's a
good chance
you will.
Even making
the effort
will make
you feel
like a new
person.
Reputations
are made
by searching
for things that
can 't be done
and doing them.
Aim low:
boring.
Aim high:
soaring.
Best of luck on your last audition for college today, buddy.
-Wes
As published in the Wall Street Journal January 15, 1996. The clipping hung behind my father's desk for years.
Sunday, March 02, 2008
The Look of Things to Come?
There's no such thing as a free lunch:
This "fix" has happened locally here in Chicago and is now law. Could this outcome foreshadow the impact of some of the currently proposed national healthcare reform strategies?
You betcha.
-Wes
Only a year ago, County Board President Todd Stroger was lopping bodies from the county payroll and closing health clinics as a way to heal a gaping budget deficit.Making a lean, mean functional machine seems impossible for politicians and bureaucrats. When you're in the government, making more government is much more palitable to your colleagues, but it means more taxes to the common man with even more bureaucracy. 1000 "new jobs" are now on their way with all of the overhead inherent to new hires, re-training of personnel, and "streamlining processes."
. . .
The new tax increase, which confers the dubious honor on Chicago of having the highest sales tax -- 10.25 percent -- of any major U.S. city, will add about $426 million annually to the county's coffers.
But Stroger's victory was not complete.
Stroger settled for a smaller sales-tax increase than he originally sought. He also agreed to place the Health Services Bureau under some form of outside control for three years. Critics also say in the process, which was often marred by bitter personal attacks, that Stroger lost some of his credibility as a manager by raising taxes rather than instituting reforms.
"As a result of a lack of a reasonable financial plan we're going to raise taxes and jeopardize the economic vitality of the Chicago region," said Laurence Msall, president of the Civic Federation, a fiscal watchdog group.
Msall said the county's increase is four times greater than the sales-tax increase granted to the CTA, which agreed to a series of "comprehensive and historic" reforms.
"There is no reform tied to this," said Msall. "There is nothing here the taxpayers can look forward to. ... Nothing in this budget that gives the Civic Federation confidence that the millions collected [under the tax increases] are going to be spent any differently than the other $3 billion in the budget."
Jerry Roper, president and chief executive officer of the Chicagoland Chamber of Commerce, said the sales-tax increase "impacts our jobs climate and makes our region more expensive and less competitive as our country lies on the brink of recession."
This "fix" has happened locally here in Chicago and is now law. Could this outcome foreshadow the impact of some of the currently proposed national healthcare reform strategies?
You betcha.
-Wes
Saturday, March 01, 2008
Cool?
Driving alone, lightheaded, really lightheaded, loses consciousness, regains consciousness, wakes to find the car's still on the road with others honking, remarkably manages to drive to ER. "...otherwise I might have died." BP low, EKG done:

Meds given. Patient and doctors' pulses improve. EKG repeated:

Feelin' cool, until:
"Why, doctor, why?"
Tests done.
Lots of 'em.
Back to back.
Including MRI:

"Therapy" given. Patient does well, until:
"What do you mean I can't drive? I have to work!"
How do I explain when I can't explain why? Logic, science, and genetics seem so cold right now. The family must know. More lives upended. "What do you mean?" Explanations. Questions. More explanations. Mother: "It was probably me."
Shock.
Denial.
Guilt.
Quiet tears.
Anything, anything...
... but cool.
-Wes
Subscribe to:
Comments (Atom)

