Increasingly, I find myself receiving direct calls, text messages, and de-identified images from colleages and support staff via cellphone. Really, it won't be long until I say goodbye to a permanent fixture on my belt that I have worn for years:
Good riddance!
-Wes
Wednesday, November 30, 2011
Rationing Health Care For Seniors
A sure-to-be controversial article appears in the Chicago Tribune this morning asking the sensitive question of 'Health care at any age, any cost?:'
It's good we're having this discussion. And yes, since doctors are increasingly employed by hospital systems eager to fund their operations, pressure continues to mount on proceduralists to offer newer and advanced therapies to patients. But it's not all about the money. There really ARE wonderful therapies out there for seniors these days and, thanks to the virtually unlimited marketing of them to elders (especially via direct-to-consumer advertising) seniors will continue to demand them. Adding fuel to the procedural fire, lack of liability protections for health care facilities and doctors who opt not to treat a patient for some very good reasons will further add pressure on doctors and hospitals.
Once again, because of special interest resistance to malpractice reform, centralized government control will become the default option.
And maybe, just maybe, we need to rethink our stand on direct-to-consumer advertising of expensive medications to the populace on the Nightly News.
-Wes
"If you want to save all lives, you're in trouble," said Callahan, co-founder of The Hastings Center, a bioethics research institute in New York, and a faculty member at Harvard Medical School, in an interview. "And if you want to save all lives at any cost, you're really in trouble."The article goes on the make some bold demands of doctors:
Callahan and co-author Nuland, a retired professor of surgery at Yale School of Medicine who wrote the best-selling "How We Die," were both 80 when the article was published.
"We need to stop thinking of medicine as an all-out war against death, because death always wins," said Callahan.
That said, McKoy believes doctors have a responsibility to spend medical resources where they do the greatest good. They must police themselves — otherwise, the government will come in and do it for them, she warns.While I agree that the doctors on the ground should be making these decisions, I, too, have problems with a central regulator imposing a random age limit where all services to functional seniors stop. More importantly, this article ignores another reality for doctors who must make these difficult decisions: the nearly unlimited liability exposure if the family members disagree with all members of the health care team, including hospital ethics panels.
This is not easy, she said, describing the tremendous pressure doctors are under to perform procedures and prescribe medicine that will not help. And, she said, they often give in.
"We get selfish families, and it's often easier for doctors to pull out prescription pads," she said. "Doctors need more often to say no, to say (if a patient is dying): 'We will give you palliative care, but not give you chemotherapy. We will not give you new expensive drugs because it will not make you better.'"
Likewise, medical schools also need to train students to understand the cost-effectiveness of treatments, and to administer them based on medical research into their effectiveness — not just because they are available.
It's good we're having this discussion. And yes, since doctors are increasingly employed by hospital systems eager to fund their operations, pressure continues to mount on proceduralists to offer newer and advanced therapies to patients. But it's not all about the money. There really ARE wonderful therapies out there for seniors these days and, thanks to the virtually unlimited marketing of them to elders (especially via direct-to-consumer advertising) seniors will continue to demand them. Adding fuel to the procedural fire, lack of liability protections for health care facilities and doctors who opt not to treat a patient for some very good reasons will further add pressure on doctors and hospitals.
Once again, because of special interest resistance to malpractice reform, centralized government control will become the default option.
And maybe, just maybe, we need to rethink our stand on direct-to-consumer advertising of expensive medications to the populace on the Nightly News.
-Wes
Tuesday, November 29, 2011
What's the Most Important Question to Ask Before Getting Your Defibrillator?
Answer: How many have you done in the past year?
If the doctor says 37 or more, you should be in very good hands.
-Wes
Reference: Freeman JV, Wang Y, Curtis JP, Heidenreich PA, Hlatky, MA. "Physician Procedure Volume and Complications of Cardioverter-Defibrillator Implantation." Circulation 2011.
If the doctor says 37 or more, you should be in very good hands.
-Wes
Reference: Freeman JV, Wang Y, Curtis JP, Heidenreich PA, Hlatky, MA. "Physician Procedure Volume and Complications of Cardioverter-Defibrillator Implantation." Circulation 2011.
When Lipitor Goes Generic
When the world's leading cholesterol-lowering "statin" drug, Lipitor, goes generic tomorrow, doctors will bear the brunt of the conversion with little information about what the new drug will cost for their patients.
This, of course, is the plan.
Even the Wall Street Journal which has an excellent "user's guide" to making the switch from name-brand to generic Lipitor offers little help as it mentions "co-pays" rather than actual drug cost:
But if we forget the insurers and copays, how much will the generic drug actually cost consumers?
No one will tell you.
That's because everyone else has to make sure they make their cut first. Pharmacy benefit managers, the leeches attached to nearly every prescription written today, have to strong-arm their position in the ever-competitive pharmaceutical profit by "pre-negotiating" prices for consumers wed to even more insurance plans with varying deductibles and co-pays.
Even Pfizer, not wanting to exclude itself from the profits inherent to such a non-transparent system is offering it's own "generic version" through Watson Pharmaceuticals. Theoretically it would be good for the public to have multiple generic manufacturers competing for generic Liptor's market, driving prices down. However, this natural self-regulating market function cannot occur to the benefit of consumers due to the blocking of actual drug price comparison.
Insisting on tranparent retail pricing of the medication's pre-insurance costs would greatly facilitate consumer choice of statin in the doctor's office. Someday, one could imagine a Consumer Reports spreadsheet in the same way they rate appliances and automobiles.
But then again, it seems we can't do that because it would serve the function of weeding out our hidden pharmaceutical middlemen.
-Wes
This, of course, is the plan.
Even the Wall Street Journal which has an excellent "user's guide" to making the switch from name-brand to generic Lipitor offers little help as it mentions "co-pays" rather than actual drug cost:
How much cheaper will generic Lipitor be?In addition, Ranbaxy Laboratories Ltd, one of the generic manufacturers of generic Lipitor, won concessions to maintain elevated prices for 180 days from the government (a la our own Food and Drug Administration while the Federal Trade Commission stands idly by complaining how consumers are gouged with this arrangement) to assure prices stay high a bit longer.
Insurance copayments should drop considerably, if patients are getting Lipitor or atorvastatin on the generic tier of their health plans. Currently, Lipitor has been on a higher, branded tier for prescription drugs. Copays for branded drugs average either $29 or $49 depending on the tier, according to Kaiser Family Foundation. Copays for generics average $10.
But if we forget the insurers and copays, how much will the generic drug actually cost consumers?
No one will tell you.
That's because everyone else has to make sure they make their cut first. Pharmacy benefit managers, the leeches attached to nearly every prescription written today, have to strong-arm their position in the ever-competitive pharmaceutical profit by "pre-negotiating" prices for consumers wed to even more insurance plans with varying deductibles and co-pays.
Even Pfizer, not wanting to exclude itself from the profits inherent to such a non-transparent system is offering it's own "generic version" through Watson Pharmaceuticals. Theoretically it would be good for the public to have multiple generic manufacturers competing for generic Liptor's market, driving prices down. However, this natural self-regulating market function cannot occur to the benefit of consumers due to the blocking of actual drug price comparison.
Insisting on tranparent retail pricing of the medication's pre-insurance costs would greatly facilitate consumer choice of statin in the doctor's office. Someday, one could imagine a Consumer Reports spreadsheet in the same way they rate appliances and automobiles.
But then again, it seems we can't do that because it would serve the function of weeding out our hidden pharmaceutical middlemen.
-Wes
Monday, November 28, 2011
When a HIPAA Security Breech Occurs
It wasn't the fact that pop-star Lindsey Lohan's father, Michael Lohan, was hospitalized that caught my eye, nor was it the splashy headline: Michael Lohan Struggling to Speak, Breathe. What caught my eye was the picture that accompanies the article that reportedly shows Mr. Lohan asleep in his hospital bed.
Is this picture of a man who is "short of breath" authentic? Since there is no oxygen tubing and no pulse oximeter applied to the pictured patient's finger, we are left to wonder.
But what if the picture IS authentic? What will happen as a result?
Will this photograph be ignored? For hospital administration and government regulators, this would pose an enormous problem.
If not ignored, will the perpetrators be brought to justice? What financial "lesson" will be levied against them?
It is frightening to consider how an investigation of such an obvious lapse in patient privacy might be conducted thanks to the implications to health care facilities imposed by HIPAA. Will all the nurses on the unit be placed on administrative leave until someone squeals? Or maybe the cleaning staff? Maybe the family themselves? Perhaps the whole hospital will have to attend HIPAA refresher courses. Perhaps the ward should be closed until the problem identified. And what about the hospital administration who have permitted such an egregious lapse in governmental policy? What fines will be levied against them as a result? Will hospital costs for future patients be adversely affected as a result of these fines?
What is clear is that the ability to maintain patient privacy is quickly becoming impossible to manage, thanks to the explosion of hand-held cell phones and miniature cameras, not to mention the requirement for electronic medical records for those receiving government-funded health care.
Real patient privacy remains a local challenge, not a universal, governmental one. Sadly, in our attempt to provide global governmental privacy protections, we forgot to protect those that are most affected when breeches occur: the innocent workers and patients themselves.
-Wes
Is this picture of a man who is "short of breath" authentic? Since there is no oxygen tubing and no pulse oximeter applied to the pictured patient's finger, we are left to wonder.
But what if the picture IS authentic? What will happen as a result?
Will this photograph be ignored? For hospital administration and government regulators, this would pose an enormous problem.
If not ignored, will the perpetrators be brought to justice? What financial "lesson" will be levied against them?
It is frightening to consider how an investigation of such an obvious lapse in patient privacy might be conducted thanks to the implications to health care facilities imposed by HIPAA. Will all the nurses on the unit be placed on administrative leave until someone squeals? Or maybe the cleaning staff? Maybe the family themselves? Perhaps the whole hospital will have to attend HIPAA refresher courses. Perhaps the ward should be closed until the problem identified. And what about the hospital administration who have permitted such an egregious lapse in governmental policy? What fines will be levied against them as a result? Will hospital costs for future patients be adversely affected as a result of these fines?
What is clear is that the ability to maintain patient privacy is quickly becoming impossible to manage, thanks to the explosion of hand-held cell phones and miniature cameras, not to mention the requirement for electronic medical records for those receiving government-funded health care.
Real patient privacy remains a local challenge, not a universal, governmental one. Sadly, in our attempt to provide global governmental privacy protections, we forgot to protect those that are most affected when breeches occur: the innocent workers and patients themselves.
-Wes
Tuesday, November 22, 2011
Grand Rounds: The Medical Blog-o-Sphere Gives Thanks
... over at the Diabetes Mine blog. Yes, I'm thankful I don't have to use this old medical kit either (but the pics are cool).
-Wes
-Wes
Sunday, November 20, 2011
Something to Be Thankful For
I was sent an e-mail from Amy Tenderich of the well-respected Diabetes Mine blog asking for contributions for this Thanksgiving’s edition of Grand Rounds. I sat with this a while and really struggled to find a topic. “It would be nice to creative writing,” I thought.
So I sat and stared at the computer.
Nothing.
I sat some more.
Still nothing.
It was complete and utter writers’ block. Then I remembered a similar time many, many years ago:
Happy Thanksgiving, Mom. (And sorry about all my typos.)
-Wes
So I sat and stared at the computer.
Nothing.
I sat some more.
Still nothing.
It was complete and utter writers’ block. Then I remembered a similar time many, many years ago:
"... but I don’t know what to write.”And before you know it, you’re not just a doctor, you’re a writer, too.
“What is it you’re trying to say?”
“That I want to get into medical school. That I like biomedical engineering. That I like people and kids and migrating monarch butterflies and music and art and all kinds of stuff! How the heck am I supposed to write something that makes sense of all this? How does one write something that will get you into medical school, for goodness sakes! This stinks!”
“Just write. It’ll come together,” she said as she returned to the afternoon’s dishes.
After I calmed down, I took out a fresh piece of paper and wrote. I wrote mountains of disjointed sentences without a central core. A stared at the page, dissatisfied. I wrote some more. Somewhere in the back of my might hid a thought, an overarching theme that failed to materialize despite my best attempts. I kept writing and writing as if somehow, some way, I’d force it out of me. Finally, out of frustration, I brought my work back to her.
“Here’s what I’ve got so far.”
“Wonderful!”
She sat and read what I had written. Occasional smiles would appear from her lips, then a look of confusion. I knew it wasn’t great since science and math were my thing at the time, not writing. She read the entire mess, start to finish, then stared up from the page, looked upward and contemplated her next move. Her radiant eyes turned toward me and pierced my stubborn façade. “You’ve got good stuff here, but I don’t get how it makes you feel. It’s too disjointed. Don’t you mean to say…?”
And we were off. I watched a master at work. She had a remarkable knack for diction and the written word. She reveled at the chance to add a verb, an adjective, a noun that changed the ordinary into the extraordinary. She’d stop and ask, “So then what?” and I’d explain. Red arrows would link concepts and ideas; a roadmap to clarity formed before my eyes. “You need to expand on this,” she’d say. Then I would return to my thoughts, frustrated at how hard this was to complete. Would it ever make any sense? But as I sat and thought some more I realized that she was right, not so much about the topic, but about the process.
Think. Write.
Don’t think. Write.
Then write some more. Be willing to toss aside the perfect stand-alone nuggets of writing that make things too verbose and distract from your message. Keep those that clarify and sharpen it. Then process the thoughts and re-work them until the final composition develops to something larger than what you had anticipated.
Like an acceptance letter to medical school.
Happy Thanksgiving, Mom. (And sorry about all my typos.)
-Wes
Saturday, November 19, 2011
HIPAA, Case Reports, and the "Small Cell" Problem
It was an interesting tweet that referenced a soon-to-be-published case report from the Annals of Emergency Medicine (via @EmergencyDocs) that piqued my interest:
Is this unique case report HIPAA compliant?
I would say, according to our current definition of HIPAA's "personal health information," such a case report is not HIPAA compliant. Nor could such a case be mentioned on a blog, for that matter, even though it presents important information for people dealing with these patients.
There is an important quality-of-care role in telling these clinical stories. In fact, HIPAA states there are just "18 little rules" that doctors are supposed to follow when they report important clinical cases. But details about cases may need to be very specific. Specific case reports can bring important specific clinical details to the attention of the medical community. For instance, if doctors had not been willing to describe several cases of pulmonary vein stenosis or two cases of esophageal perforation in a major medical journal years ago, how many more people might have been injured as a result?
But there's problem giving such details about clinical details about patient cases: "the small cell problem:"
But doctors should not be afraid of publishing case reports especially since there are good reasons for them clinically. Further, when doctors make good faith efforts to conceal patient's personal information in those reports, they should not be subject to threats of HIPAA's "small cell" problem. Simply put: the "small cell" problem is HIPAA's, not the doctors'. Extending the definition of personal health information as defined by HIPAA to include "any other unique identifying characteristic" about a patient's case limits doctors' ability to improve care to our patients while greatly increasing our legal culpability for that effort.
-Wes
Thrilling case study: emergency doc cracked chest to save 42 y/o woman in cardiac tamponade after ablation therapy. http://bit.ly/umnydcDetails about the case are quite specific and the case reports heralds from a town in Minnesota. It describes, in very specific detail, the management of a patient who presented to the emergency room in shock from cardiac tamponade after a catheter ablation procedure for right ventricular outflow tract tachycardia.
Is this unique case report HIPAA compliant?
I would say, according to our current definition of HIPAA's "personal health information," such a case report is not HIPAA compliant. Nor could such a case be mentioned on a blog, for that matter, even though it presents important information for people dealing with these patients.
There is an important quality-of-care role in telling these clinical stories. In fact, HIPAA states there are just "18 little rules" that doctors are supposed to follow when they report important clinical cases. But details about cases may need to be very specific. Specific case reports can bring important specific clinical details to the attention of the medical community. For instance, if doctors had not been willing to describe several cases of pulmonary vein stenosis or two cases of esophageal perforation in a major medical journal years ago, how many more people might have been injured as a result?
But there's problem giving such details about clinical details about patient cases: "the small cell problem:"
Clinicians should be sensitive to the "small cell problem": the existence of individuals with such unique or unusual diagnoses or illnesses, that it might be possible for others (or patients and families themselves) to identify the individuals in case reports or medical text books based upon limited information, such as state or city of residence, age and diagnosis.The "small cell" problem violates HIPAA and HIPAA means business: millions of dollars of business that gets released in press releases from the Department of Health and Human Services when they catch their prey.
But doctors should not be afraid of publishing case reports especially since there are good reasons for them clinically. Further, when doctors make good faith efforts to conceal patient's personal information in those reports, they should not be subject to threats of HIPAA's "small cell" problem. Simply put: the "small cell" problem is HIPAA's, not the doctors'. Extending the definition of personal health information as defined by HIPAA to include "any other unique identifying characteristic" about a patient's case limits doctors' ability to improve care to our patients while greatly increasing our legal culpability for that effort.
-Wes
Friday, November 18, 2011
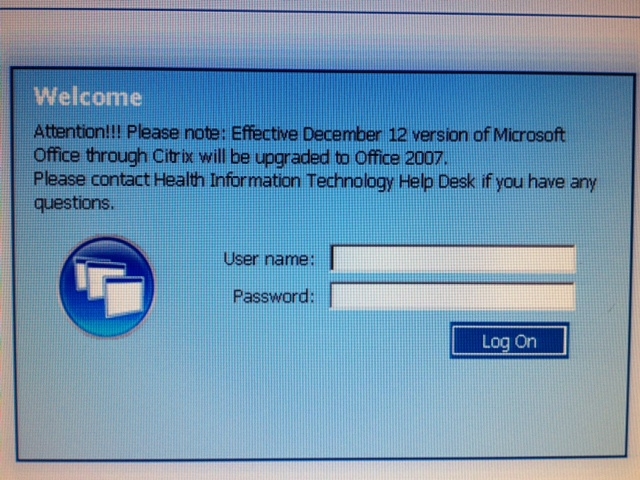
UpToDate for EMRs
It's Friday. I sat down to work, saw this, and it made me smile:
It's not easy keeping up with technology when things move so fast.
-Wes
It's not easy keeping up with technology when things move so fast.
-Wes
Thursday, November 17, 2011
Doctors Passing Fake Sick Notes Get Reprimand
From the Wisconsin Journal Sentinel:
Pity.
-Wes
h/t: Instapundit
The Medical Examining Board reached stipulations with seven doctors Wednesday in which they were formally reprimanded for failing to make adequate records on the patients they saw during the protests. The stipulations also required the doctors to pay $225 to $350 each for costs and take four hours of continuing education courses within 90 days on medical record keeping.A mere hand slap.
The reprimands will stay on the doctors' records permanently and will show up in a national database of physicians, Murray said. The doctors' reprimands would be a factor in determining discipline in future cases if any of the doctors come before the board again, he said.
Pity.
-Wes
h/t: Instapundit
Wednesday, November 16, 2011
Pacing Without Wires
From Medgadget via The Medical Quack:
But to suggest that a left heart catheterization to place their little device in the endocardium of the left ventricle "removes the need for complex surgery" is a stretch. Embolic complications, valvular complications and the potential for stroke complications (with the need for at least some anticoagulation) will quickly temper their enthusiastic press release. And what happens when a patient needs an ultrasound of their heart or has a capsule endoscopy? Could there be significant electromagnetic interference?
But we should not rain on these companies' parade too quickly, even if they are a bit late to the party. The implications of this technology as we move forward with more sophisticated pacing therapies are profound. One only needs to consider complex congenital heart cases with anomalous venous return, epicardial delivery of this technology, or its capability to paired with drug delivery systems in the future to see where things might go with such a novel means of pacing.
-Wes
EBR Systems, a start-up out of Sunnyvale California, and Cambridge Consultants, the technology design and development firm, have developed a leadless pacemaker system for patients with advanced heart failure. The Wireless Cardiac Stimulation System (WiCS) comprises two units, an implantable electrode and an external control unit. The electrode incorporates an ultrasonic, wireless receiver and delivers an electrical stimulus to the heart based on triggering signals from the external control unit.Nice.
In its current iteration the WiCS system is designed to work with conventional pacemakers/defibrillators pacing the right ventricle of patients requiring biventricular pacing. The WiCS external control unit senses the pacing stimulus delivered to the right ventricle and initiates a burst of stimulus from the electrode implanted in the left ventricle. According to the company, the wireless left ventricular pacing approach removes the need for complex surgery and the complications often associated with the coronary sinus leads used to pace the left ventricle.
But to suggest that a left heart catheterization to place their little device in the endocardium of the left ventricle "removes the need for complex surgery" is a stretch. Embolic complications, valvular complications and the potential for stroke complications (with the need for at least some anticoagulation) will quickly temper their enthusiastic press release. And what happens when a patient needs an ultrasound of their heart or has a capsule endoscopy? Could there be significant electromagnetic interference?
But we should not rain on these companies' parade too quickly, even if they are a bit late to the party. The implications of this technology as we move forward with more sophisticated pacing therapies are profound. One only needs to consider complex congenital heart cases with anomalous venous return, epicardial delivery of this technology, or its capability to paired with drug delivery systems in the future to see where things might go with such a novel means of pacing.
-Wes
Tuesday, November 15, 2011
Welcome to My Office
It sure beats the heck out of a desk, chair and desk phone:
At the start of each case, I still have to pinch myself when I contemplate the wonder of it all.
-Wes
At the start of each case, I still have to pinch myself when I contemplate the wonder of it all.
-Wes
Monday, November 14, 2011
From the AHA: You Are Here
Thanks to Larry Husten over at Cardiobrief for posting this great picture from the American Heart Association meeting going on now in Orlando, FL. It's a helpful sign if there ever was one:
With all the mobile devices and internet connectivity available to doctors attending these meetings now, perhaps a more relevant sign should have read: "Be Here Now."
-Wes
With all the mobile devices and internet connectivity available to doctors attending these meetings now, perhaps a more relevant sign should have read: "Be Here Now."
-Wes
Sunday, November 13, 2011
When Screening Teenage Athletes for Sudden Cardiac Arrest Risk, History Matters
Before reaching for tests like EKGs to screen teen athletes, we should first ask ourselves if we've taken a careful history:
The new study consisted of Madsen and his fellow researchers sending out surveys to every pediatrician and family practice doctor in Washington State. They received a good response–surveys were returned by 72 percent of pediatricians and 56 percent of family practitioners.-Wes
The results were disheartening:
Dr. Gaurav Arora, associate director of electrophysiology at the Children’s Hospital of Pittsburgh and an assistant professor of pediatrics at the University of Pittsburgh, was surprised to see the number of physicians in the new study who said they didn’t ask every teen athlete about fainting or chest pain. He said, “Those are red flags in young athletes.”
- 28 percent of doctors surveyed failed to always ask if a teen experienced chest pain during exercise.
- 22 percent of doctors surveyed failed to always ask if the teen ever fainted without a known cause or explanation.
- 26 percent of doctors surveyed failed to always ask about early deaths in their family history.
- 67 percent failed to always ask about heart disease in their family history.
Friday, November 11, 2011
Miss Manners Goes to the ACCF
Dear Ms. Manners:
I am a fellow of the American College of Cardiology and I just learned that the American College of Cardiology Foundation (ACCF), the same foundation that publishes most of our patient care and treatment guidelines, is providing training to medical device and pharmaceutical personnel so our interactions with them become “effective and efficient.”
How nice.
Is this how Multaq (er, dronedarone) got such an early mention in our latest atrial fibrillation treatment guidelines? I've always wondered, especially after we later learned that there might be a few unsavory issues with this drug.
Still, I have no doubt the need is there. Glad to see that my annual membership fees are being put to such good use. After all, up until now, it really HAS been hard interacting with industry reps when they brought lunch. Don’t get me wrong, it wasn’t their professional demeanor or their knowledge of their device or drug. No, that wasn’t it. It was just so hard to explain to them why I had to dine and dash.
Now, thanks to you, I won't have to. I'll just spend more of my limited time getting down with industry personnel so we can share. Imagine: having smart people we can talk to about our latest, coolest case so they can record how much money they spend on our get-togethers. That's efficiency exemplified.
I'm especially impressed that the ACCF training of industry personnel will occur every two years. I was worried about quality of our industry reps' knowledge base, so I'm glad you've made this effort a full-time job. (By the way, I had NO IDEA the ACCF now has a vivarium for all this training - when did you guys spring for that?) Impressive. Rest assured that I'll be SURE to check for your ACCF Training Logo on their business cards before I help myself to a gyro.
But do me a favor, will you? Would you mind passing on some of those fees you receive for that industry training to those of us helping ourselves to lunch? After all, those membership fees we're paying to the ACC are getting a bit stiff. (*wink wink*)
Just kidding.
I'm sure you're really collecting those fees to help lower the cost of my patients' medical devices and drugs in an effort to support their "positive health outcomes." After all, it's this cost thing that's reaking havoc on our health care system, right? (I wish I had thought of such a clever way to address this problem).
Ms. Manners?
Ms. Manners?
Right?
-Wes
h/t: Larry Husten over at Cardiobrief.
I am a fellow of the American College of Cardiology and I just learned that the American College of Cardiology Foundation (ACCF), the same foundation that publishes most of our patient care and treatment guidelines, is providing training to medical device and pharmaceutical personnel so our interactions with them become “effective and efficient.”
How nice.
Is this how Multaq (er, dronedarone) got such an early mention in our latest atrial fibrillation treatment guidelines? I've always wondered, especially after we later learned that there might be a few unsavory issues with this drug.
Still, I have no doubt the need is there. Glad to see that my annual membership fees are being put to such good use. After all, up until now, it really HAS been hard interacting with industry reps when they brought lunch. Don’t get me wrong, it wasn’t their professional demeanor or their knowledge of their device or drug. No, that wasn’t it. It was just so hard to explain to them why I had to dine and dash.
Now, thanks to you, I won't have to. I'll just spend more of my limited time getting down with industry personnel so we can share. Imagine: having smart people we can talk to about our latest, coolest case so they can record how much money they spend on our get-togethers. That's efficiency exemplified.
I'm especially impressed that the ACCF training of industry personnel will occur every two years. I was worried about quality of our industry reps' knowledge base, so I'm glad you've made this effort a full-time job. (By the way, I had NO IDEA the ACCF now has a vivarium for all this training - when did you guys spring for that?) Impressive. Rest assured that I'll be SURE to check for your ACCF Training Logo on their business cards before I help myself to a gyro.
But do me a favor, will you? Would you mind passing on some of those fees you receive for that industry training to those of us helping ourselves to lunch? After all, those membership fees we're paying to the ACC are getting a bit stiff. (*wink wink*)
Just kidding.
I'm sure you're really collecting those fees to help lower the cost of my patients' medical devices and drugs in an effort to support their "positive health outcomes." After all, it's this cost thing that's reaking havoc on our health care system, right? (I wish I had thought of such a clever way to address this problem).
Ms. Manners?
Ms. Manners?
Right?
-Wes
h/t: Larry Husten over at Cardiobrief.
Thursday, November 10, 2011
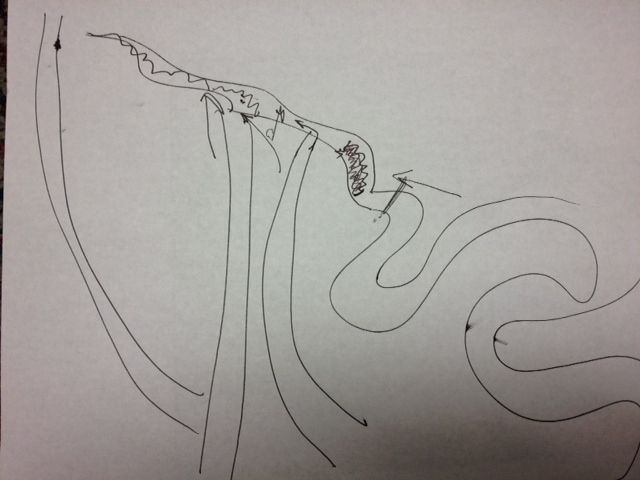
Planning
Years of college, medical school, residency, cardiology fellowship, and interventional fellowship training all comes down to this:
-Wes
Click image to enlarge
-Wes
Wednesday, November 09, 2011
Just Five Little Minutes
"I estimate these changes to your charting work flow will take only five minutes."
Five minutes is fine if it happens for only one patient. But when it is multiplied by as many as forty patients in a day, the multiples get impressive. Five minutes x forty patients = 200 minutes (more than 1.5 hours a day).
Minor five-minute changes to administrative charting requirements aren't so minor, especially when you add more time for quality assurance reporting or pay-for-performance initiatives. Suddenly huge swaths of time from a doctor's opportunity to take care of their patients. We need more care time and less data entry time. Doctors must insist that we not become data entry clerks.
Increasingly, I see the data entry burdens of regulatory health care documentation requirements falling on doctors. On first blush, this seems logical because only doctors (or very capable, highly trained surrogates) understand the nuances required to make potentially life-altering adjustments to the electronic medical record. But when new administrative documentation requirements are added to doctors and other care providers, it compromises our time with patients where we explain the mechanisms of their disease and its management nuances. Discussions of medications, therapies, and required follow-up get get short shrift to mandated governmental documentation burdens. If we want to maintain patient volumes to improve access for new patients, we must get creative. After all, time is not expandable.
And there could be a better way.
I believe we need to get patients more involved in their own care before they see their doctor. Imagine a patient entering proposed changes to their list of health problems, surgeries performed, medications and doses being taken and allergies before they are seen on their cell phone or local waiting-room computer terminal or iPad. These proposed changes could then be reviewed, validated, a approved (or not) by their doctor leaving the majority of the patient visit for what matters: actual patient care.
Then maybe, just maybe, I could salvage four of those five precious minutes for both of us.
-Wes
Five minutes is fine if it happens for only one patient. But when it is multiplied by as many as forty patients in a day, the multiples get impressive. Five minutes x forty patients = 200 minutes (more than 1.5 hours a day).
Minor five-minute changes to administrative charting requirements aren't so minor, especially when you add more time for quality assurance reporting or pay-for-performance initiatives. Suddenly huge swaths of time from a doctor's opportunity to take care of their patients. We need more care time and less data entry time. Doctors must insist that we not become data entry clerks.
Increasingly, I see the data entry burdens of regulatory health care documentation requirements falling on doctors. On first blush, this seems logical because only doctors (or very capable, highly trained surrogates) understand the nuances required to make potentially life-altering adjustments to the electronic medical record. But when new administrative documentation requirements are added to doctors and other care providers, it compromises our time with patients where we explain the mechanisms of their disease and its management nuances. Discussions of medications, therapies, and required follow-up get get short shrift to mandated governmental documentation burdens. If we want to maintain patient volumes to improve access for new patients, we must get creative. After all, time is not expandable.
And there could be a better way.
I believe we need to get patients more involved in their own care before they see their doctor. Imagine a patient entering proposed changes to their list of health problems, surgeries performed, medications and doses being taken and allergies before they are seen on their cell phone or local waiting-room computer terminal or iPad. These proposed changes could then be reviewed, validated, a approved (or not) by their doctor leaving the majority of the patient visit for what matters: actual patient care.
Then maybe, just maybe, I could salvage four of those five precious minutes for both of us.
-Wes
Monday, November 07, 2011
AMA Medical News: Social Media's Public Health Implications and Limitations
From a mention in today's AMA Medical News:
Many health professionals do not see social media-based research replacing more traditional study methods, because not everyone uses the Internet or social networking. But they expect data gathered from social media to play an increasingly larger role in addressing public health issues.-Wes
"Social media has huge potential for public health," Dr. Fisher said. "I don't think that people have even begun to realize that potential yet."
Saturday, November 05, 2011
Smile! You're on Candid Camera!
They sat anxiously waiting for their loved one to enter the holding area after the procedure, one nervously clutching her purse, another today's paper, and a third, her cellphone. The air was tense as they awaited the news of how the procedure went. All the preparation, the concern, and the questioning come down to this moment when they learn if they made the right decision to go forward with the procedure. Will there be elation or despair?
So of course they want to videotape the moment.
The door opened, there was their loved one, looking no worse for wear, followed by the doctor. As he came forth to tell them the good news, the cellphone video recorder captured the discussion, the elation, the "thank you's," and the specifics about the case. It was done discretely and not noticed until the end of the conversation with the group. The doctor was caught completely off-guard.
In this case, the news was happy. All went well. But what should happen if the news weren't so good or even devastating?
I wonder.
We have entered an era where instantly-available photographs and video loops are becoming a way of life for many. YouTube, Facebook, and Twitter are everyday household words. More and more people own cellphones capable of uploading photographs and video content in seconds to the internet. And people bring these marvels of technology into hospitals and clinics every day. What this will mean to patient privacy, HIPAA compliance, and the sanctity of the doctor-patient relationship remains to be seen. But one thing's for certain, surveillance cameras are showing up everywhere and not likely to go away.
-Wes
So of course they want to videotape the moment.
The door opened, there was their loved one, looking no worse for wear, followed by the doctor. As he came forth to tell them the good news, the cellphone video recorder captured the discussion, the elation, the "thank you's," and the specifics about the case. It was done discretely and not noticed until the end of the conversation with the group. The doctor was caught completely off-guard.
In this case, the news was happy. All went well. But what should happen if the news weren't so good or even devastating?
I wonder.
We have entered an era where instantly-available photographs and video loops are becoming a way of life for many. YouTube, Facebook, and Twitter are everyday household words. More and more people own cellphones capable of uploading photographs and video content in seconds to the internet. And people bring these marvels of technology into hospitals and clinics every day. What this will mean to patient privacy, HIPAA compliance, and the sanctity of the doctor-patient relationship remains to be seen. But one thing's for certain, surveillance cameras are showing up everywhere and not likely to go away.
-Wes
Friday, November 04, 2011
Forced Productivity: Our New Sweatshop
We have to ask ourselves how are we going to take care of 32 million more patients in 2014 with a limited number of physicians to care for them. Better yet, how are we going to do this and save money doing it.
Thanks to our central regulators, they have already figured out how to do this: forced productivity. The term itself brings to mind images of outer Siberia or Chinese sweat shops. Lower costs and expect the workers to do more to make the same income. Perhaps you haven't heard this term in our President's health care reform speeches.
But it's out there as a lynchpin in the brave New World of medicine. I heard this term listening to a recent lecture by banker Steven Lipstein, the new Vice Chair of the Board of the Patient Centered Outcomes Research Institute (PCORI) established under the Patient Protection and Affordable Care Act during a recent lecture at our institution. He is also President and CEO of BJC HealthCare in St. Louis, MO who also serves as Chairman of the Board of Directors of the St. Louis Federal Reserve Bank.
But as I listened to Mr. Lipstein I wondered, how and when will forced productivity end?
How much forced productivity can doctors tolerate before they snap. How many hours can they endure when no workday or geographic restrictions are in place for them while residents and medical students saunter home after an eight-hour work day? How much forced productivity can they endure to repay their huge medical school loans?
Most importantly, what debts are incurred by "forced productivity gains" to patients? If patients think their doctors are busy now as they stuggle to get an appointment or feel rushed when the do get an appointment, just wait.
Mr. Lipstein understood the principles of the new health care climate well when he explained how we got to where we are today. What he doesn't understand at all, however, is the unintended consequences that are likely to occur as a result of these changes.
You see, doctors don't keep bankers' hours.
-Wes
Thanks to our central regulators, they have already figured out how to do this: forced productivity. The term itself brings to mind images of outer Siberia or Chinese sweat shops. Lower costs and expect the workers to do more to make the same income. Perhaps you haven't heard this term in our President's health care reform speeches.
But it's out there as a lynchpin in the brave New World of medicine. I heard this term listening to a recent lecture by banker Steven Lipstein, the new Vice Chair of the Board of the Patient Centered Outcomes Research Institute (PCORI) established under the Patient Protection and Affordable Care Act during a recent lecture at our institution. He is also President and CEO of BJC HealthCare in St. Louis, MO who also serves as Chairman of the Board of Directors of the St. Louis Federal Reserve Bank.
But as I listened to Mr. Lipstein I wondered, how and when will forced productivity end?
How much forced productivity can doctors tolerate before they snap. How many hours can they endure when no workday or geographic restrictions are in place for them while residents and medical students saunter home after an eight-hour work day? How much forced productivity can they endure to repay their huge medical school loans?
Most importantly, what debts are incurred by "forced productivity gains" to patients? If patients think their doctors are busy now as they stuggle to get an appointment or feel rushed when the do get an appointment, just wait.
Mr. Lipstein understood the principles of the new health care climate well when he explained how we got to where we are today. What he doesn't understand at all, however, is the unintended consequences that are likely to occur as a result of these changes.
You see, doctors don't keep bankers' hours.
-Wes
Thursday, November 03, 2011
Hybrid Operating Rooms
Yesterday, the FDA approved Edward Lifescience's percutaneous transvalvular aortic valve replacement catheter for human use. Despite this, it appears unlikely that implants of these valves will progress in short order due to concerns of demand for the expensive technology in the era of increased scrutiny of device utilization by payers, especially CMS. Which constraints will be placed on cardiologists and which institutions will be approved for this technology are issues still being considered. At the current rate, it appears unlikely at this time that this technology will be deployed before the end of the year.
One new trend in cardiovascular circles (and a trend that is very politically-correct in our new "Accountable Care Organization" era of medicine that also plays well with health care marketing teams) has been the installation of new, very expensive 'hybrid' catheterization laboratory/operating rooms capable of transitioning from a conventional operating room to a catheterization laboratory (or back again) in larger hospitals. It is clear that patient selection for percutaneous valve procedures will likely require collaboration between cardiothoracic surgeons and cardiologists and some valvular procedures may require both specialists in complicated cases.
Here's a time-lapse video of the conversion of a hybrid operating room from the University of California, San Diego where a patient first had a DaVinci robot-assisted single-vessel off-pump coronary bypass operation followed by placement of an intracoronary stent in another coronary artery by cardiologists. (Not sure why it was done this way, but I don't know specifics about the case.)
While staged DaVinci robot procedures with angioplasty probably won't be common, these fancy "hybrid" operating rooms (OR's) are much more likely to be used for percutaneous valve implantations or even atrial fibrillation ablations using simultaenous epicardial and endocardial approaches.
Fun times.
-Wes
One new trend in cardiovascular circles (and a trend that is very politically-correct in our new "Accountable Care Organization" era of medicine that also plays well with health care marketing teams) has been the installation of new, very expensive 'hybrid' catheterization laboratory/operating rooms capable of transitioning from a conventional operating room to a catheterization laboratory (or back again) in larger hospitals. It is clear that patient selection for percutaneous valve procedures will likely require collaboration between cardiothoracic surgeons and cardiologists and some valvular procedures may require both specialists in complicated cases.
Here's a time-lapse video of the conversion of a hybrid operating room from the University of California, San Diego where a patient first had a DaVinci robot-assisted single-vessel off-pump coronary bypass operation followed by placement of an intracoronary stent in another coronary artery by cardiologists. (Not sure why it was done this way, but I don't know specifics about the case.)
While staged DaVinci robot procedures with angioplasty probably won't be common, these fancy "hybrid" operating rooms (OR's) are much more likely to be used for percutaneous valve implantations or even atrial fibrillation ablations using simultaenous epicardial and endocardial approaches.
Fun times.
-Wes
Wednesday, November 02, 2011
Alan Simpson: On Starting to Cut Health Care Costs
Former Senator Alan Simpson blasts John Kerry at the "Super Committee" (aka, the Joint Deficit Reduction Committe) hearing yesterday regarding health care costs:
Be sure to see former Clinton White House chief of staff Erskine Bowles add his two cents, too.
You have to wonder: is anybody listening?
-Wes
h/t: Kaiser Health News
"We just knew that whatever you call it, if you want to use the negatives and call it Obamacare or any kind of care you want to, it won't work. It can't work because all you have to do is use common sense. You have this emplosion of people, you have diabetes, you have one person in America that weighs more than the other two, you got guys who choose tobacco, choose booze, choose to use designer drugs, and all of them will be taken care of. You've got pre-existing conditions in three year-olds - what happens throught their sixty, or fifty, years of life? All you have to do is forget the charts and know that if you torture statistics long enough they will eventually confess and know that this country cannot exist on any kind of situation where a guy who could buy this buidling gets a $150,000 heart operation and doesn't even get a bill. Now that's nuts and that's where we are in America. No affluence testing. You gotta raise co-pays, you gotta knock down providers, you gotta deal with physicians, you gotta have hospitals keep one set of books instead of two - that will be a start."Here's the video:
Be sure to see former Clinton White House chief of staff Erskine Bowles add his two cents, too.
You have to wonder: is anybody listening?
-Wes
h/t: Kaiser Health News
Tuesday, November 01, 2011
Meaningful Ruse Rap
At first I thought this video on "meaningful use" of the electronic medical record (EMR) was clever. But as I watched it, I realized it was too clever and too professionally produced. Then, what was first supposed to be funny, actually exposes the ridiculous complexity of the "meaningful use" requirements for Electronic Medical Records. (Independent doctors, take note!)
But, hey, it's your tax dollars at work, so for your entertainment, I bring you our government's way of explaining what it will take to acquire the $44,000 promised to doctors for installing an EMR through rap:
-Wes
h/t: My office manager (yes, they've all seen it).
But, hey, it's your tax dollars at work, so for your entertainment, I bring you our government's way of explaining what it will take to acquire the $44,000 promised to doctors for installing an EMR through rap:
-Wes
h/t: My office manager (yes, they've all seen it).
Can I Watch?
It's one of the more common questions I hear from family members before I take their loved one into a procedure: "Can I watch?"
For me, the answer is simple: no.
Fortunately, when I explain my rationale, most people come to understand why this isn't such a good idea:
For me, the answer is simple: no.
Fortunately, when I explain my rationale, most people come to understand why this isn't such a good idea:
- First, the doctor performing the procedure has enough to think about without having to be a tour guide to a family member. Even something as simple as a pacemaker battery change can go very wrong if an operator is distracted long enough to accidentally reverse the atrial and ventricular leads when they are reattached to the new pacemaker pulse generator.
- Second, if something should occur that is unexpected during a procedure, a doctor needs to focus on the problem at hand without having to deal with the physical and psychological well-being of a family member also.
- Third, the operating room has all kinds of unusual sights, sounds, and (often unexpectedly) smells to which many people are not accustomed. If a family member becomes lightheaded, nauseous, or hits the deck as a result of these powerful stimuli, it can make for a very long (and embarassing) day indeed.
Warning: Self-Removal of a Pacemaker Can Be Deadly
A bizarre story from the Chicago Tribune today:
-Wes
h/t: Ves Dimov, MD via Twitter.
A 47-year-old man living in a group home in Chicago's Uptown neighborhood died Monday night after he tried to remove his heart pacemaker from his chest, officials said.Pacemakers and their leads become densely encapsulated with fibrous tissue within weeks of their implant. As such, their removal is not as easy as it may seem to the casual observer. I know this sounds obvious to most, but if you're having chest pains, please seek medical advice and do NOT attempt to remove your permanent pacemaker.
The man, who lived in the 4700 block of North Winthrop Avenue, was pronounced dead at 11:33 p.m. at Advocate Illinois Masonic Hospital, according to the Cook County medical examiner's office.
Chicago Fire Department paramedics were called after the man told a worker in the home that he was experiencing chest pains and asked them to call an ambulance.
The man returned to his room, where he remained until paramedics arrived, police said. When they did, he complained to them about chest pains and was taken to the ambulance where he fell unconscious, police said.
As paramedics were trying to revive him, they discovered a puncture wound on the upper left side of his chest, police said. At some point, police were called when it became apparent that the man had been stabbed, police said.
After the man was taken to the hospital, a doctor told police that the man had apparently tried to remove his pacemaker himself, police said. It was not known what the man used in that attempt.
-Wes
h/t: Ves Dimov, MD via Twitter.
Subscribe to:
Comments (Atom)