Another day, another pacemaker, at least so it seemed at first.
The usual greeting the patient, answering the last questions, consent signing, placement of the IV, EKG leads, prepping of the surgical site and initiation of the pre-operative antibiotics were all recent memories. He laid there, smiling, knowing he'd made the right decision after years of struggling with his arrhythmia in other ways. His heart was showing signs of slight weakening and his arrhythmias remained too fast despite a multitude of therapies, so he had agreed to proceed with placement of a biventricular pacemaker with later ablation of his AV node some weeks later after his surgical wound was well-healed.
The nurses and technicians in the room were wonderful, reassuring the patient as they moved him to the narrow procedural table. More wires were connected to monitors and a blood pressure cuff placed. The instrument table laid ready, and the patient's choice of soft rock could be heard faintly in the background. The pre-sedation note was completed and checklists reviewed.
Meanwhile, I donned by lead, bouffant hair net, headlamp, and face mask, then scrubbed for the procedure. Shortly thereafter I turned to open the procedure room door with my backside and was quickly greeted to a hearty "Time Out!" The patient's identity and procedure confirmed, I could see the patient smiling:
"We lawyers like to hear those things," he said. (Yes, he was a lawyer.*)
"Nurse, make sure you give him a ton of sedation - he'll need it, okay?" I joked. We laughed together at the thought.
"1 of Versed and 25 mcg of Fentanyl," the nurse shouted to the control room.
"1 and 25," the control room answered.
He and I had struggled together with his arrhythmia for years, finally agreeing that this option at this stage in his arrhythmia's progression would be best.
I made my way to his side and once again prepped his chest with chlorhexidine prep sticks, letting each dry before the next was applied. The surgical sight was then drapped to provide an island of an orange plastic film surrounded by a sea of blue paper covering. Other drapes were secured and a pocket for instruments was made. "Everybody have lead?" I asked. The x-ray system was enabled, then the pacemaker system analyzer cable, a SiteRite ultrasound probe and Bovie pen made ready. All was set to begin.
"Mr. Jones (not his real name), I'm going to start to numb your skin with the local anesthestic. This will sting," I said.
"Okay..." as he braced himself for inpact. Then:
"Come-on, doc, you can do better than that!..." as if to mock me, jokingly.
"Yes, I can, " I countered, then proceeded to administer more anesthetic to the area. As the area became more anesthetized, his shoulder seemed to relax. No doubt the Versed helped a bit, too.
I continued, locating the appropriate spot, then performing the incision. He was unaware. The pocket was created first, then I found the vein and placed the first lead without a problem. Badda bing, badda boom. Now for the next…
Then, out of the blue:
"Doc, I heard you're having a knee replacement ... "
"Just a partial, I hope ..."
"Hey, I just want to tell you. It's the best thing I ever did. Listen, it's not as bad as you think, but there's quite a bit you have to be ready for… Don't forget to preload the Miralax - that iron supplement before the procedure to slow you down and then the narcotics afterward to stop you up: it's a Machiavellian ploy by those orthopedic surgeons to assure your discomfort."
I chuckled as I thought about this.
"And whatever you do, take the pain medication before physical therapy. I had a physical therapist threaten to fire me when I failed to take the pain medication 45 minutes before therapy. And get rid of all those rugs. It really helps to plan your trips when you get up. Think about what you need and what you might need to limit your trips. I'm telling you, this saved my life. You know I'm writing a book about stuff like this... I'm waiting on the proof. Don't come back too soon. Have you completed your FMLA forms yet?"
"What?"
"FMLA. Look it up. Loads of fun. Anyhow, be nice to your wife - you're gonna need her. Trust me on this..."
And on and on it went: patient treating doctor, until his pacemaker was done. Then, finally, I had a chance to reciprocate:
"I'm closing."
"Thanks, doc, and good luck. You're going to do fine."
-Wes
* ... yes, he gave me permission to tell this story.
Tuesday, October 28, 2014
Tuesday, October 21, 2014
Reviewing The Regulators
In 1990 the American Board of Medical Specialties (ABMS) and the
American Board of Internal Medicine (ABIM) changed their requirements for
physician board certification from a voluntary life-long designation and
educational process to a time-limited designation lasting 10 years. This
decision to require repeated testing, the public was told, was based
on data from a single
highly flawed retrospective literature review that suggested physician
competence deteriorates over time. Despite this, over the ensuing years hospitals and insurance companies increasingly require physicians to be board certified for credentialing or billing purposes. And as a result of changing the life-long designation of board certification to a temporary one, physicians were left with little choice but to pay for and participate in the ABMS/ABIM MOC program to practice their trade.
In 2005, the ABMS modified their re-certification requirements and created a
program called "Maintenance of Certification" (MOC). This
program required completion of "Practice Improvement Modules" in
addition to the completion of certain knowledge-base testing modules before a
physician could sit for their secure re-certifying examination. This
decision to include "Practice Improvement Modules" was a
unilateral one by the ABMS and its subsidiaries and was never scientifically
challenged or validated by the independent physician community.
This year, the requirements for MOC changed again when allUS
Review of the ABIM’s "research" topics showed they cover a wide range of important clinical care issues including trust, teamwork, ethics, obligations of the Hippocratic Oath, characteristics of internal medicine physicians and their practices, teaching, staffing patterns, electronic health records, clinical skills, and the structure of medical homes. But closer inspection of much of this work shows it was not research, but rather opinion and editorial. Much of the "research" resides behind expensive online paywalls free to the academic community, but expensive for the non-academic physician and public to review. Given these realities, before casting aspersions on physicians' ability to evaluate their own weaknesses, it appears a review of the ABIM's "research" in regard to its clinical legitimacy is in order.
In 2014, the Center for Medicare and Medicaid Services (CMS) published the entire database of $77 billion dollars of payments made to US health care providers in 2012. The data are easily reviewed using a website created by the Wall Street Journal. In an effort to establish the credibility of the ABIM leadership and staff's journal publications as it pertains to the various aspects of medical practice they claim to actively monitor, each author published in the 2014 collection of journal articles published on the ABIM website was cross-referenced with their CMS 2012 Medicare provider payment data.
Methods
The ABIM publishes journal articles authored by ABIM staff and leadership for the years 2000-2014 on its website. The 31 articles published so far in 2014 were randomly selected for review. Each author of each paper was then compared to their 2012 Medicare payment data. If the payment data for a particular author were non-zero, then the total number of inpatient and outpatient new and existing patient encounters were totaled to determine the total 2012 annual Medicare patient care encounters seen by the author. Procedure counts were not added to this total of encounters, since the intent here was to "even the playing field" between "proceduralists" and hospital- or office-based clinicians in terms of the number of patient contact episodes they had each year. In the event more than one physician author's first and last names were identical, the source article was reviewed to assure the proper physician data was obtained based on their city, state, or academic institution.
Authors designated as employees of ABIM, those with acknowledged conflicts of interest or those with non-academic or policy affiliations were also recorded. The average, median and standard deviation of 2012 Medicare payments and patient encounters were then calculated.
As a point of reference, the author of this blog post received a total of $163,184.55 in Medicare payments representing 529 patient encounters (298+75+13 established outpatient visits, 31 outpatient new visits, 82+14 initial hospital/inpatient care and 16 subsequent hospital care visits) according to the 2012 Medicare database. This number of encounters represented 1.5 days of outpatient clinic visits per week in 2012 (personal data) as well as inpatient patient care encounters payments received from Medicare patients. This encounter volume represented 42% of this author’s total number of clinical encounters billed in 2012 (personal data).
Results
Thirty-one articles published by the ABIM staff and leadership in 2014 (so far) represented work by 150 authors. Of the 31 articles published on the ABIM's website to date for 2014, ten of them (33%) were published solely by ABIM employees or leadership. Only 80 of the 150 authors held an MD degree. The authors were a heterogeneous mix of US and non-US physicians, one veterinarian, nurses, students, statisticians, researchers, representatives from National Board of Medical Examiners, Center for Medicare and Medicaid Services, the Urban League, the Foundation for Advancement of International Medical Education and Research, Mathematica Policy Research, Inc., the National Collaborative for Improving Primary Care Through Industrial and Systems Engineering, the VA medical system, staff members of the American Board of Internal Medicine Foundation, and others from Consumer Reports Health.
Clinical Involvement
Of physicians with an MD degree, the average 2012 Medicare payment amount was $18,196.97 ± $68,220.55 (median $0). Only thirty-seven of the 80 physician authors (46%) had Medicare payments paid to them in 2012. Three authors had payments exceeding $100,000 in 2012 while the vast majority (30 of the 37) received under $25,000. This average payment amount corresponded to an average of 131 ± 308 patient encounters (median 0) for the entire year 2012.
If all of the authors were included in the analysis, the average 2012 Medicare payment was $9705.05 ± $50,502.95. The median Medicare payment to the authors published in 2014 to date was $0. The average number of patient encounters per year in 2014 was 70 ± 234. The median number of patient encounters in 2012 by the authors published to date was 0.
The entire spreadsheet (pdf) of the 2012 Medicare payment and encounter data by each author that published with ABIM leadership and staff in 2014 can be reviewed here.
Discussion
This study is the first to cross-reference a portion of ABIM publishing authors to the 2012 Medicare provider payment database. While Medicare payment data might not represent the full workload of today's clinical physicians, it is the most complete database of US physician clinical work performed on patients in the United States published to date.
The ABMS/ABIM's Maintenance of Certification program has been criticized by many working physicians as onerous, expensive, time-consuming and a poor reflection of physician quality. In his response to physician concerns over the MOC process, the President and CEO of the ABIM stated:
Dramatic changes to the health care landscape have occurred over the past five years. If the mission of the ABIM is to truly certify internists who with “skills and attitudes essential for excellent patient care," we are left to question the legitimacy of recommendations made by physicians who no longer care for patients in today’s health care arena. The ABIM seems content with making recommendations to physicians while being woefully inxperienced about the challenges that face internists today. In fact, the data presented in their work confirms that physician quality is being regulated by an unqualified body.
While some might argue that regimented study and time-consuming non-clinical data acquisitions are required to assure physician quality, it remains quite possible that such a dishonest and lopsided approach will backfire as physicians refuse to participate in this process or retire early from medicine just as more patients are entering our health care system. Burdening clinical physicians with unrealistic and unproven demands for non-clinical tasks detracts from needed patient care. Recall that only three of the physicians included in the author list of ABIM's 2014 publications received over $100,000 of Medicare payments while 30 of 37 physicians in the published articles in 2014 received less than $25,000. Might the recommendations and data that the ABIM is making available to hospital groups and insurance organizations be seriously flawed?
Even a cursory review of the background of the authors of several published works of the ABIM staff and leadership reviewed suggests a troubling narrative. For instance, one article included with the ABIM's 2014 list of journal articles is entitled "Internists' attitudes about assessing and maintaining clinical competence" (J General Int Med 2014; 29(4):608-614). While this title might seem reassuring to the public that the ABIM is serious about their mission, their credibility becomes suspect when closer inspection of the background of the authors revealed only one of the six authors had any clinical encounters in 2012 and another author was a veterinarian. In another article entitled "Time to trust: longitudinal integrated clerkships and entrustable professional activities," (Academic Medicine, 89(2), pp 201-4) none of the authors received payments for patient care in 2012 and the authors acknowledge the ideas presented were provided by two political "think tanks." Should these be the people we entrust to develop clerkship ideals and "entrustable professional activities" (whatever that is) for our future physicians?
We should note that despite fourteen years of articles on the ABIM's website, none of the ABIM’s "research" has ever evaluated any negative consequence of their MOC program. Rather, these ABIM papers "drives and informs" additional unsubstantiated "program development" like a public relations firm. Without independent assessment of their practices, it remains completely possible that the MOC process causes more harm than benefit to actual patient care delivery as a result.
The Medicare payment data of ABIM authors also begs the question, how are the ABIM physicians and legislators spending their time? It is apparent that most physician members of the ABIM are not involved in clinical care. Given the conflicts of interest mentioned in the various citations, physician quality assurance is not the ABIM's priority. Perhaps the physician members of the ABIM would have more credibility advising struggling doctor-employees on beefing up their curriculum vitae, earning consulting fees, perfecting public relations skills, and creating multiple income streams since their annual revenue take with their MOC program implementation went from $46,131,129 in 2010 to $55,625,925 in 2012 (Data from the 2011 and 2013 IRS Form 990 published on guidestar.org/). Given these data, it is appears that the ABIM is more concerned about padding their resume to (1) create and air of legitimacy, (2) serve a political agenda, and (3) to provide a smoke screen for the high salaries of their board members.
Clearly, busy front-line full-time practicing physicians do not have the time for creating publishing mills or for scientifically meaningless survey collection. Patients want capable practicing physician availability, not survey collectors. Assuring physician quality should not be about creating and funding a political action committee subservient to a political agenda, but rather understanding the challenges physicians face in their workplace and knowledge base and working collaboratively to offer continuous professional improvement.
Limitations
There are several limitations to this study. First, because the CMS Medicare payment database does not capture work performed on patients under the age of 65, the database does not accurately reflect the total clinical work load a physician performs each year. Physicians who do not accept Medicare for payment would not appear on this database. However, since older patients commonly access our health care system more frequently as they age, it would be expected that internists writing policy for health care delivery would participate in the Medicare government program. Second, the 2012 Medicare payment data reviewed does not correlate to the year the articles were published in the literature. However, one would expect that experienced physicians who changed the testing requirements for MOC in 2014 would have recent direct patient care experience to appreciate the many factors that impact physicians today. Finally, reviewing only one year's literature published on the ABIM's website might have introduced sampling bias. Still, the sampling of the most recent year offers the advantage of reviewing articles that might affect upcoming policy decisions.
Conclusions
Physicians are not above proving their competence and establishing quality standards, especially if those standards are scientifically sound and transparent. The legitimacy of the MOC process to assure physician quality should be called into question based on a careful literature review of the many conflicts exposed by this review and the limited recent clinical experience of those that contribute to their evidence base. Citing numerous publications to legitimize the MOC program creates the illusion that this process of insuring quality care and has been vetted by actual scientific data. Nothing could be further from the truth.
-Wes
This year, the requirements for MOC changed again when all
"There is a good deal of research demonstrating the
value of MOC: from the validity of the examination, to the importance of
independent assessments – clinicians are not good at evaluating their own
weaknesses. All of this research drives and informs our program requirements
and product development."
Review of the ABIM’s "research" topics showed they cover a wide range of important clinical care issues including trust, teamwork, ethics, obligations of the Hippocratic Oath, characteristics of internal medicine physicians and their practices, teaching, staffing patterns, electronic health records, clinical skills, and the structure of medical homes. But closer inspection of much of this work shows it was not research, but rather opinion and editorial. Much of the "research" resides behind expensive online paywalls free to the academic community, but expensive for the non-academic physician and public to review. Given these realities, before casting aspersions on physicians' ability to evaluate their own weaknesses, it appears a review of the ABIM's "research" in regard to its clinical legitimacy is in order.
In 2014, the Center for Medicare and Medicaid Services (CMS) published the entire database of $77 billion dollars of payments made to US health care providers in 2012. The data are easily reviewed using a website created by the Wall Street Journal. In an effort to establish the credibility of the ABIM leadership and staff's journal publications as it pertains to the various aspects of medical practice they claim to actively monitor, each author published in the 2014 collection of journal articles published on the ABIM website was cross-referenced with their CMS 2012 Medicare provider payment data.
Methods
The ABIM publishes journal articles authored by ABIM staff and leadership for the years 2000-2014 on its website. The 31 articles published so far in 2014 were randomly selected for review. Each author of each paper was then compared to their 2012 Medicare payment data. If the payment data for a particular author were non-zero, then the total number of inpatient and outpatient new and existing patient encounters were totaled to determine the total 2012 annual Medicare patient care encounters seen by the author. Procedure counts were not added to this total of encounters, since the intent here was to "even the playing field" between "proceduralists" and hospital- or office-based clinicians in terms of the number of patient contact episodes they had each year. In the event more than one physician author's first and last names were identical, the source article was reviewed to assure the proper physician data was obtained based on their city, state, or academic institution.
Authors designated as employees of ABIM, those with acknowledged conflicts of interest or those with non-academic or policy affiliations were also recorded. The average, median and standard deviation of 2012 Medicare payments and patient encounters were then calculated.
As a point of reference, the author of this blog post received a total of $163,184.55 in Medicare payments representing 529 patient encounters (298+75+13 established outpatient visits, 31 outpatient new visits, 82+14 initial hospital/inpatient care and 16 subsequent hospital care visits) according to the 2012 Medicare database. This number of encounters represented 1.5 days of outpatient clinic visits per week in 2012 (personal data) as well as inpatient patient care encounters payments received from Medicare patients. This encounter volume represented 42% of this author’s total number of clinical encounters billed in 2012 (personal data).
Results
Thirty-one articles published by the ABIM staff and leadership in 2014 (so far) represented work by 150 authors. Of the 31 articles published on the ABIM's website to date for 2014, ten of them (33%) were published solely by ABIM employees or leadership. Only 80 of the 150 authors held an MD degree. The authors were a heterogeneous mix of US and non-US physicians, one veterinarian, nurses, students, statisticians, researchers, representatives from National Board of Medical Examiners, Center for Medicare and Medicaid Services, the Urban League, the Foundation for Advancement of International Medical Education and Research, Mathematica Policy Research, Inc., the National Collaborative for Improving Primary Care Through Industrial and Systems Engineering, the VA medical system, staff members of the American Board of Internal Medicine Foundation, and others from Consumer Reports Health.
Clinical Involvement
Of physicians with an MD degree, the average 2012 Medicare payment amount was $18,196.97 ± $68,220.55 (median $0). Only thirty-seven of the 80 physician authors (46%) had Medicare payments paid to them in 2012. Three authors had payments exceeding $100,000 in 2012 while the vast majority (30 of the 37) received under $25,000. This average payment amount corresponded to an average of 131 ± 308 patient encounters (median 0) for the entire year 2012.
If all of the authors were included in the analysis, the average 2012 Medicare payment was $9705.05 ± $50,502.95. The median Medicare payment to the authors published in 2014 to date was $0. The average number of patient encounters per year in 2014 was 70 ± 234. The median number of patient encounters in 2012 by the authors published to date was 0.
The entire spreadsheet (pdf) of the 2012 Medicare payment and encounter data by each author that published with ABIM leadership and staff in 2014 can be reviewed here.
Discussion
This study is the first to cross-reference a portion of ABIM publishing authors to the 2012 Medicare provider payment database. While Medicare payment data might not represent the full workload of today's clinical physicians, it is the most complete database of US physician clinical work performed on patients in the United States published to date.
The ABMS/ABIM's Maintenance of Certification program has been criticized by many working physicians as onerous, expensive, time-consuming and a poor reflection of physician quality. In his response to physician concerns over the MOC process, the President and CEO of the ABIM stated:
"ABIM's mission is to enhance the quality
of health care by certifying internists and subspecialists who demonstrate the
knowledge, skills and attitudes essential for excellent patient care."
Dramatic changes to the health care landscape have occurred over the past five years. If the mission of the ABIM is to truly certify internists who with “skills and attitudes essential for excellent patient care," we are left to question the legitimacy of recommendations made by physicians who no longer care for patients in today’s health care arena. The ABIM seems content with making recommendations to physicians while being woefully inxperienced about the challenges that face internists today. In fact, the data presented in their work confirms that physician quality is being regulated by an unqualified body.
While some might argue that regimented study and time-consuming non-clinical data acquisitions are required to assure physician quality, it remains quite possible that such a dishonest and lopsided approach will backfire as physicians refuse to participate in this process or retire early from medicine just as more patients are entering our health care system. Burdening clinical physicians with unrealistic and unproven demands for non-clinical tasks detracts from needed patient care. Recall that only three of the physicians included in the author list of ABIM's 2014 publications received over $100,000 of Medicare payments while 30 of 37 physicians in the published articles in 2014 received less than $25,000. Might the recommendations and data that the ABIM is making available to hospital groups and insurance organizations be seriously flawed?
Even a cursory review of the background of the authors of several published works of the ABIM staff and leadership reviewed suggests a troubling narrative. For instance, one article included with the ABIM's 2014 list of journal articles is entitled "Internists' attitudes about assessing and maintaining clinical competence" (J General Int Med 2014; 29(4):608-614). While this title might seem reassuring to the public that the ABIM is serious about their mission, their credibility becomes suspect when closer inspection of the background of the authors revealed only one of the six authors had any clinical encounters in 2012 and another author was a veterinarian. In another article entitled "Time to trust: longitudinal integrated clerkships and entrustable professional activities," (Academic Medicine, 89(2), pp 201-4) none of the authors received payments for patient care in 2012 and the authors acknowledge the ideas presented were provided by two political "think tanks." Should these be the people we entrust to develop clerkship ideals and "entrustable professional activities" (whatever that is) for our future physicians?
We should note that despite fourteen years of articles on the ABIM's website, none of the ABIM’s "research" has ever evaluated any negative consequence of their MOC program. Rather, these ABIM papers "drives and informs" additional unsubstantiated "program development" like a public relations firm. Without independent assessment of their practices, it remains completely possible that the MOC process causes more harm than benefit to actual patient care delivery as a result.
The Medicare payment data of ABIM authors also begs the question, how are the ABIM physicians and legislators spending their time? It is apparent that most physician members of the ABIM are not involved in clinical care. Given the conflicts of interest mentioned in the various citations, physician quality assurance is not the ABIM's priority. Perhaps the physician members of the ABIM would have more credibility advising struggling doctor-employees on beefing up their curriculum vitae, earning consulting fees, perfecting public relations skills, and creating multiple income streams since their annual revenue take with their MOC program implementation went from $46,131,129 in 2010 to $55,625,925 in 2012 (Data from the 2011 and 2013 IRS Form 990 published on guidestar.org/). Given these data, it is appears that the ABIM is more concerned about padding their resume to (1) create and air of legitimacy, (2) serve a political agenda, and (3) to provide a smoke screen for the high salaries of their board members.
Clearly, busy front-line full-time practicing physicians do not have the time for creating publishing mills or for scientifically meaningless survey collection. Patients want capable practicing physician availability, not survey collectors. Assuring physician quality should not be about creating and funding a political action committee subservient to a political agenda, but rather understanding the challenges physicians face in their workplace and knowledge base and working collaboratively to offer continuous professional improvement.
Limitations
There are several limitations to this study. First, because the CMS Medicare payment database does not capture work performed on patients under the age of 65, the database does not accurately reflect the total clinical work load a physician performs each year. Physicians who do not accept Medicare for payment would not appear on this database. However, since older patients commonly access our health care system more frequently as they age, it would be expected that internists writing policy for health care delivery would participate in the Medicare government program. Second, the 2012 Medicare payment data reviewed does not correlate to the year the articles were published in the literature. However, one would expect that experienced physicians who changed the testing requirements for MOC in 2014 would have recent direct patient care experience to appreciate the many factors that impact physicians today. Finally, reviewing only one year's literature published on the ABIM's website might have introduced sampling bias. Still, the sampling of the most recent year offers the advantage of reviewing articles that might affect upcoming policy decisions.
Conclusions
Physicians are not above proving their competence and establishing quality standards, especially if those standards are scientifically sound and transparent. The legitimacy of the MOC process to assure physician quality should be called into question based on a careful literature review of the many conflicts exposed by this review and the limited recent clinical experience of those that contribute to their evidence base. Citing numerous publications to legitimize the MOC program creates the illusion that this process of insuring quality care and has been vetted by actual scientific data. Nothing could be further from the truth.
-Wes
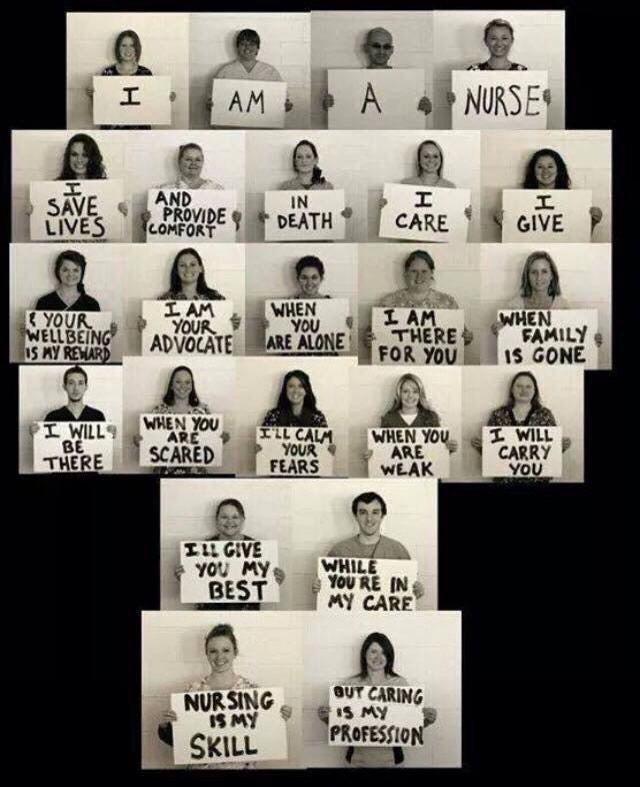
What Signs Would Bureaucrats and Regulators Hold Up?
Nice to see front-line health care workers finding their voice.
I wonder what signs our health care bureaucrats and regulators would hold up?
-Wes
Subscribe to:
Comments (Atom)