The results of the Base-Case Analysis are remarkable: "Internists will incur an average of $23,607 (95% CI, $5,380 to $66,383) in MOC costs over 10 years, ranging from $16,725 for general internists to $40,495 for hematologists-oncologists. Time costs account for 90% of MOC costs. Cumulatively, 2015 MOC will cost $5.7 billion over 10 years, $1.2 billion more than 2013 MOC (emphasis mine). This includes $5.1 billion in time costs (resulting from 32.7 million physician-hours spent on MOC) and $561 million in testing costs."
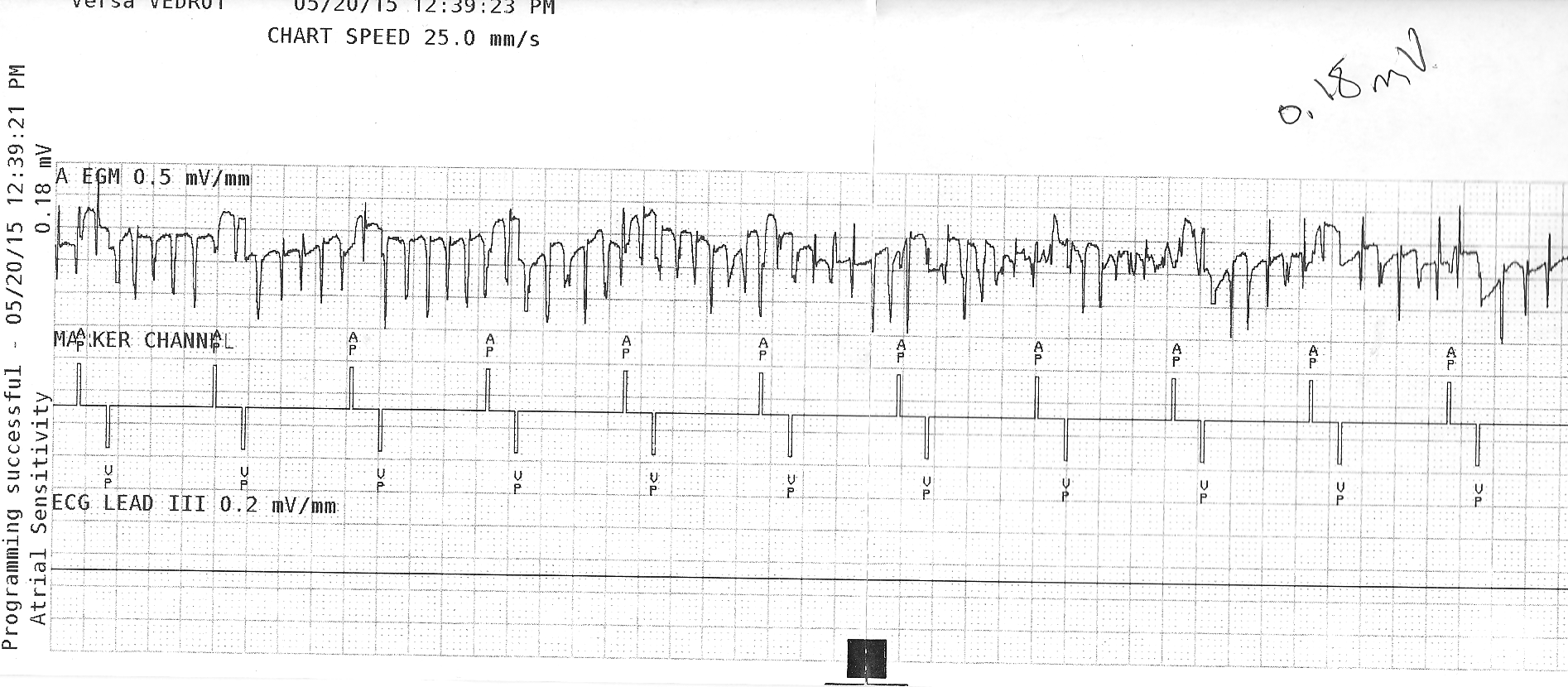
How much does it cost by specialty over 10 years? Here's a copy of one of the tables from the article included for your review:
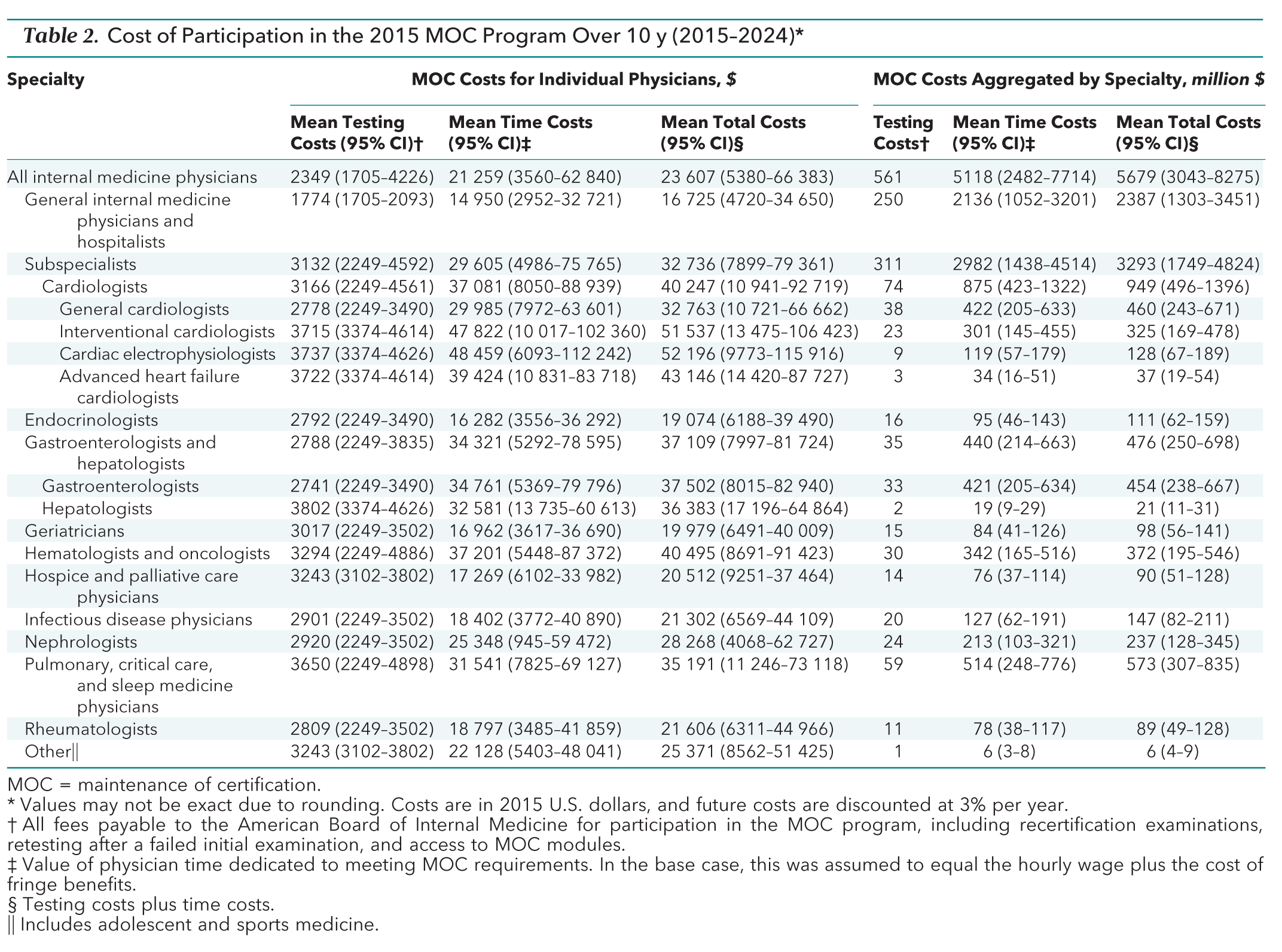 |
| Cost to Participate in MOC by Subspecialty (Click to enlarge) |
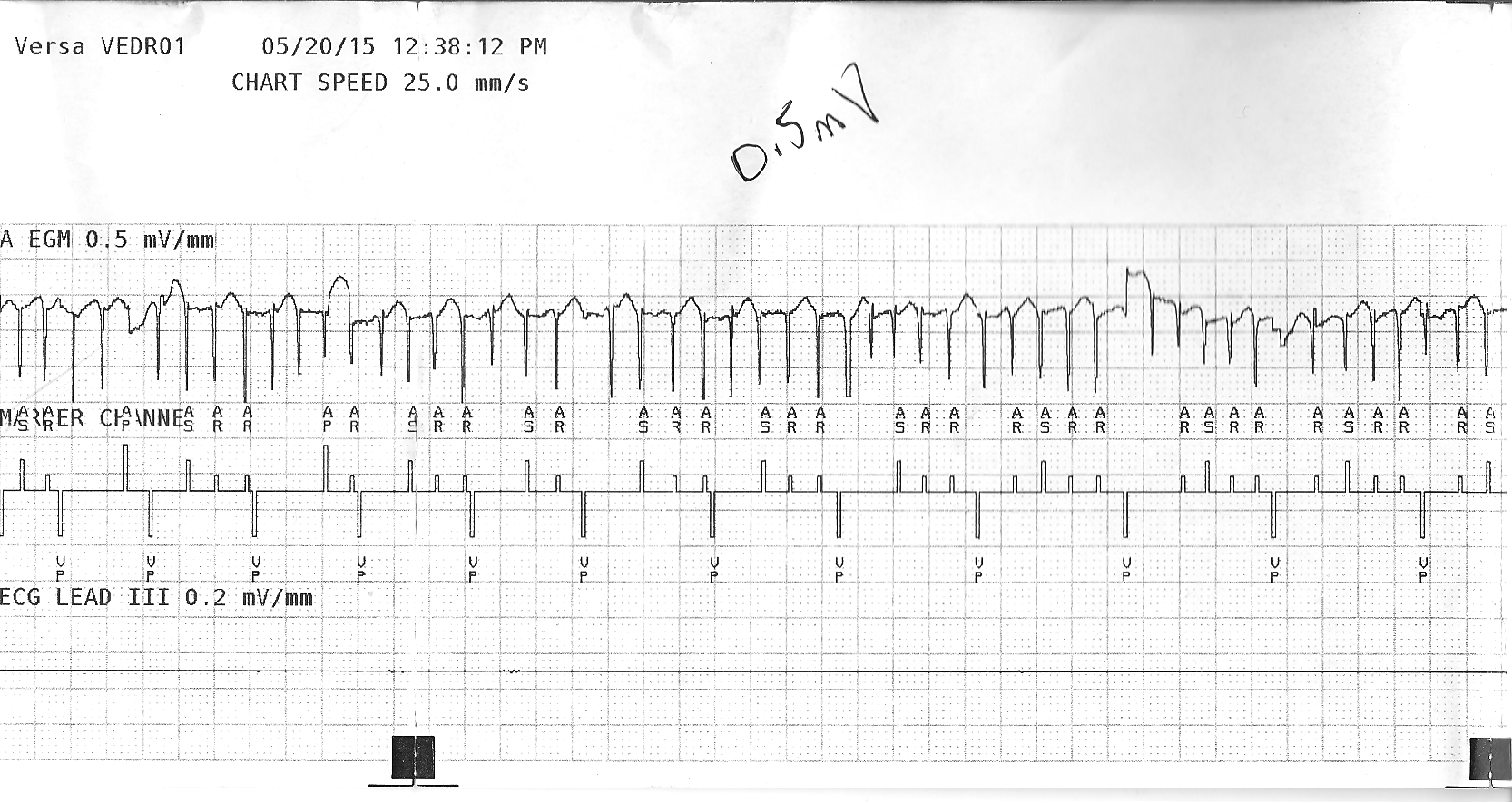
Here's a breakdown of MOC costs for individual physicians from the article based on the number of certificates they maintain with confidence intervals displayed:
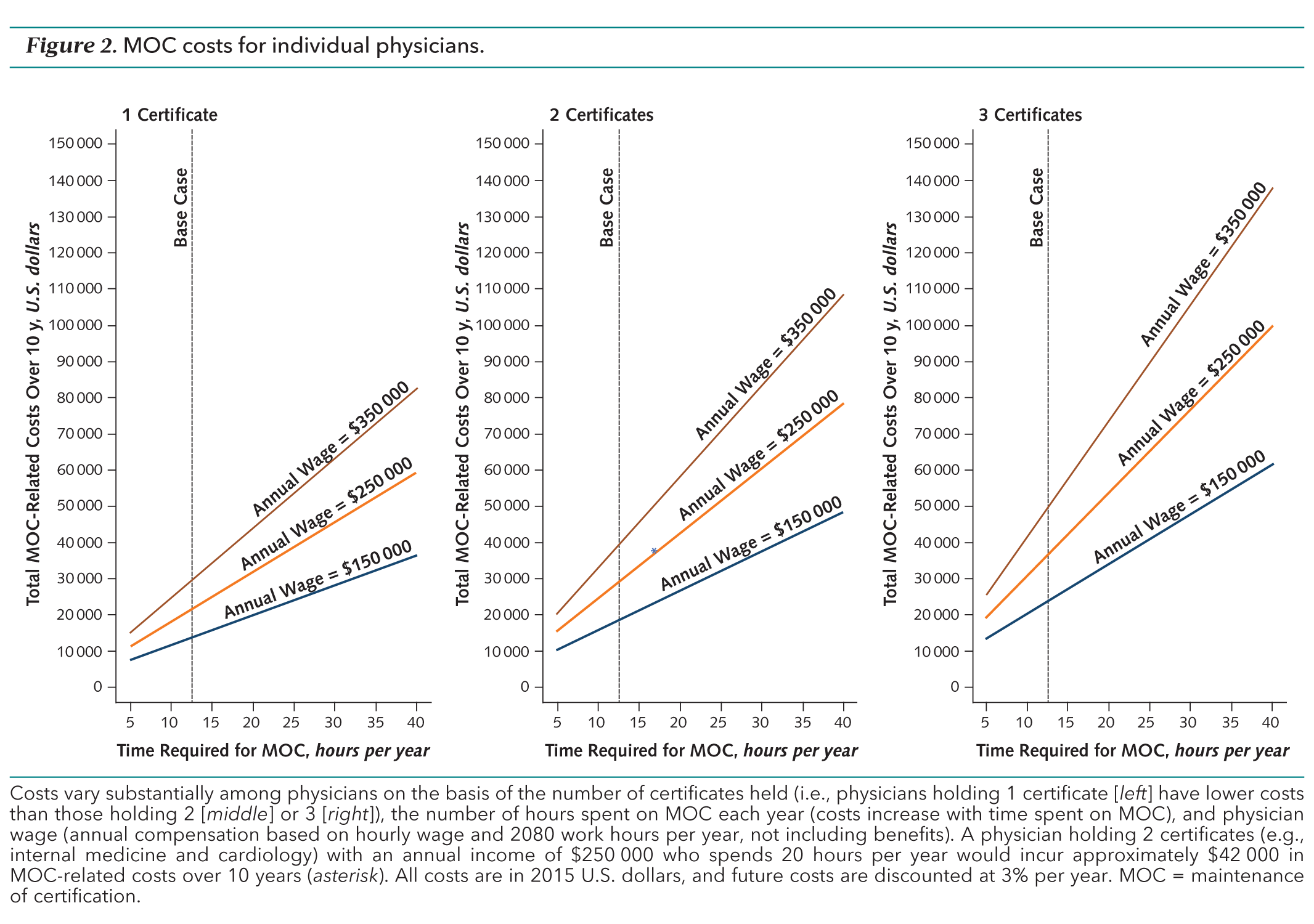 |
| MOC Costs for Individual Physicians - (Click to enlarge) |
MOC is not an educational program based on evidence of improved patient outcomes or care quality. Rather, it is an educational program that was created by fear - fear of loss of credentials and fear of loss of insurance panel participation and payments. As such, it is inherently coercive.
If there ever was a time to stop the wasting of physicians resources and time that has yet to demonstrate any evidence that the program improves patient outcomes or care quality, the time is now.
-Wes
Reference:
Alexander T Sandhu , R. Adams Dudley, Dhruv S. Kazi. "Cost Analysis of the ABIM Maintenance of Certification Program" Ann Intern Med 28 July 2015,(), doi: 10:7326/M15-1011.
Addendum 29 Jul 2015 @ 12:41PM CST:
Dr. Richard Baron responds to this Cost Analysis on the ABIM blog as "The Cost of Keeping Up." No public comments are taken on the blog any longer, but the ABIM is accepting e-mails. Baron's response fails to acknowledge that the authors projected ABIM will make more than half a billion dollars in ten years and that this cost estimate is ten times higher than Dr. Baron has mentioned on numerous occassions (see here and here), irrespective of the time required by physicians "to keep up."