Just raise the sales tax to 10.75%, the highest in the country.
-Wes
Monday, June 30, 2008
Squelched
I'm not trying to be antisocial, but I've had trouble reaching my blog at this URL recently - seems a new firewall's been installed at work. I have an inquiry in now with our IS department... hopefully things can be reinstated. So while I can still post and respond at home, my ability to respond to comments made during the day has been curtailed, at least for the time being...
Thanks for your understanding.
-Wes
Thanks for your understanding.
-Wes
Sunday, June 29, 2008
Revisiting Cardiac CT Angiograms
The New York Times published an extensive article on the CT angiogram (CTA) for the diagnosis of coronary disease and is a very worthwhile read. In the report, they describe the controversy between cardiologists surrounding these tests. But in their push to provide eye-catching content, they permitted a CT angiogram proponent, Dr. Harvey Hecht of The Lenox Hill Heart and Vascular Institute of New York, to show perfect 3D images of a normal CTA obtained in nice, slow, regular heart rhythm that peels away the rib structures and shows some of the coronary arteries, the inside surface of the heart, and heart valves as he narrates the video. It's like watching something from the "Undersea World of Jacque Cousteau." Yes, they are beautiful pictures and demonstrate the incredible capabilities of this technology. Gosh, who wouldn't want those beautiful pictures of their heart?
Thank you, NYT, for giving Dr. Hecht, and the entire CT proponents all they need to peddle their scans, after all, a picture is worth a thousand words, right?
But if you read the article carefully, those beautiful pictures come at a price: both for the patient and our economically-burdened healthcare system. Not only are they fairly expensive, but the risks of radiation to the patient are real. To the authors' credit, they made this point. But they also failed to explain that for women with generally smaller frames and greater levels of breast tissue, those risks of radiation are amplified. They also didn't show a flawed CTA in their online article sidebar: like one taken in atrial fibrillation (an irregular heart rhythm) or with lots of skipped heart beats - you see, those images aren't quite so clear. Because the heart is a moving organ, collection of the images must be precisely gated to the heart beat. In people with irregular heart rhythms, motion artifact is introduced, degrading the quality of the images obtained.
The authors also failed to show the images of a patient with a heavy coronary calcium score. Those CTA images sometimes don't turn out so well, either. All CT angiograms use iodinated contrast material injected rapidly through an intravenous line placed in the arm. Scanning begins a few seconds later, after the operators think the dye has reached the patient's coronary arteries (the circulation time is estimated). Once the contrast agent reaches the arteries, it causes the blood vessels and chambers of the heart to "stand out" from the surrounding walls of the heart and blood vessels. In the case of someone with too much calcium in the arteries, the native calcium also "stands out" and might shadow the actual ability of the contrast to define the lumen of the blood vessel. Also, things like stents, which are metallic, interfere the same way. Additionally, the contrast agents used might be harmful to a patient if they have compromised kidney function, so most people have a blood test to evaluate their kidney function before the test (yes, more money).
Certainly in complex congenital heart disease, here are few tests better than CTA to define to course of anomalous blood vessels. CTA has also been invaluable to electrophysiologists to image the left atrium and the pulmonary arteries to define the size, number, and orientation of vessels before left atrial catheter ablation procedures. Likewise, there might be a role to perform CTA to exclude coronary artery disease in the chest pain patient who presents to the Emergency Room. But as a screening test for the general population or even our "walking well" in the cardiology clinic, these scans have no role today, despite what others may suggest.
Despite this, the patient testimonial was telling:
Boo rah.
But adding up this patient's cumulative radiation dose (10 mSV for the "Calcium Score" + 27.3 mSv for the thallium study + another 21.4 mSv for the CTA) gives him the equivalent of almost 3000 chest x-rays worth of radiation.
And then his cardiologist (Dr. Hecht) wanted to repeat the test every year "so he could see how quickly the plaque in Mr. Franks’s arteries was thickening" claiming "how do we know that our therapy is effective?"
Boo rah.
For the record, I know of no study demonstrating the safety, cost effectiveness, or the ability of CTA to document CAD progression year to year. Further, Hecht's own paper demonstrated that even with extensive cholesterol lowering, no change to plaque burden was documented. I also have never seen such documentation be able to predict a cardiac event of any type. But Dr. Hecht seems to feel insults to those questioning the utility of CTA are appropriate:
-Wes
References: Nico R. Mollet, Filippo Cademartiri, Carlos A.G. van Mieghem, Giuseppe Runza, Eugène P. McFadden, Timo Baks, Patrick W. Serruys, Gabriel P. Krestin and Pim J. de Feyter. "High-Resolution Spiral Computed Tomography Coronary Arteriography in Patients Referred for Diagnostic Conventional Coronary Angiography." Circulation 2005; 112: 2318-2323.
Abelson R, "Heart Scans Still Covered my Medicare." New York Times 13 March 2008.
Addendum 29Jun2008 @ 1523: - the opposing view over at "The Voice in the Ear".
Thank you, NYT, for giving Dr. Hecht, and the entire CT proponents all they need to peddle their scans, after all, a picture is worth a thousand words, right?
But if you read the article carefully, those beautiful pictures come at a price: both for the patient and our economically-burdened healthcare system. Not only are they fairly expensive, but the risks of radiation to the patient are real. To the authors' credit, they made this point. But they also failed to explain that for women with generally smaller frames and greater levels of breast tissue, those risks of radiation are amplified. They also didn't show a flawed CTA in their online article sidebar: like one taken in atrial fibrillation (an irregular heart rhythm) or with lots of skipped heart beats - you see, those images aren't quite so clear. Because the heart is a moving organ, collection of the images must be precisely gated to the heart beat. In people with irregular heart rhythms, motion artifact is introduced, degrading the quality of the images obtained.
The authors also failed to show the images of a patient with a heavy coronary calcium score. Those CTA images sometimes don't turn out so well, either. All CT angiograms use iodinated contrast material injected rapidly through an intravenous line placed in the arm. Scanning begins a few seconds later, after the operators think the dye has reached the patient's coronary arteries (the circulation time is estimated). Once the contrast agent reaches the arteries, it causes the blood vessels and chambers of the heart to "stand out" from the surrounding walls of the heart and blood vessels. In the case of someone with too much calcium in the arteries, the native calcium also "stands out" and might shadow the actual ability of the contrast to define the lumen of the blood vessel. Also, things like stents, which are metallic, interfere the same way. Additionally, the contrast agents used might be harmful to a patient if they have compromised kidney function, so most people have a blood test to evaluate their kidney function before the test (yes, more money).
Certainly in complex congenital heart disease, here are few tests better than CTA to define to course of anomalous blood vessels. CTA has also been invaluable to electrophysiologists to image the left atrium and the pulmonary arteries to define the size, number, and orientation of vessels before left atrial catheter ablation procedures. Likewise, there might be a role to perform CTA to exclude coronary artery disease in the chest pain patient who presents to the Emergency Room. But as a screening test for the general population or even our "walking well" in the cardiology clinic, these scans have no role today, despite what others may suggest.
Despite this, the patient testimonial was telling:
Nonetheless, in February, Mr. Franks took a test called a calcium score, which measures the amount of calcified plaque in the arteries. The test, a less extensive form of scanning, revealed a moderate buildup of calcium in his arteries, a potential sign of heart disease."If it's free, it's for me," right?
So he decided to have a nuclear stress test. When that test showed no problem, the cardiologist who conducted it said he did not need more testing.
But Mr. Franks was still not satisfied. “I’m someone who wants to know,” he said.
After doing research on the Internet, he found Dr. Hecht, who recommended a CT angiogram. Dr. Hecht acknowledged that Mr. Franks probably did not have severe heart disease. But he said the scan would be valuable anyway because it might reassure him. And his insurance would cover the cost.
Boo rah.
But adding up this patient's cumulative radiation dose (10 mSV for the "Calcium Score" + 27.3 mSv for the thallium study + another 21.4 mSv for the CTA) gives him the equivalent of almost 3000 chest x-rays worth of radiation.
And then his cardiologist (Dr. Hecht) wanted to repeat the test every year "so he could see how quickly the plaque in Mr. Franks’s arteries was thickening" claiming "how do we know that our therapy is effective?"
Boo rah.
For the record, I know of no study demonstrating the safety, cost effectiveness, or the ability of CTA to document CAD progression year to year. Further, Hecht's own paper demonstrated that even with extensive cholesterol lowering, no change to plaque burden was documented. I also have never seen such documentation be able to predict a cardiac event of any type. But Dr. Hecht seems to feel insults to those questioning the utility of CTA are appropriate:
Cardiologists like Dr. Brindis (and Dr. Wes, it seems) hurt their patients by being overly conservative and setting unrealistic standards for the use of new technology, Dr. Hecht said.Hmmm. Dispense with need for evidenced-based medicine? I wonder what Dr. Hecht will say to his patient when the CTA scan shows a tumor mass one year.
“It’s incumbent on the community to dispense with the need for evidence-based medicine,” he said. “Thousands of people are dying unnecessarily.”
-Wes
References: Nico R. Mollet, Filippo Cademartiri, Carlos A.G. van Mieghem, Giuseppe Runza, Eugène P. McFadden, Timo Baks, Patrick W. Serruys, Gabriel P. Krestin and Pim J. de Feyter. "High-Resolution Spiral Computed Tomography Coronary Arteriography in Patients Referred for Diagnostic Conventional Coronary Angiography." Circulation 2005; 112: 2318-2323.
Abelson R, "Heart Scans Still Covered my Medicare." New York Times 13 March 2008.
Addendum 29Jun2008 @ 1523: - the opposing view over at "The Voice in the Ear".
Friday, June 27, 2008
The Ultimate in Woo: The Heart-Bean
You're not going to believe this: presenting... (drum roll, please)... the Heart-Bean:
-Wes
PS: Be sure to see the videos: for guys here and gals here. Have a great weekend!
Emerging from the wildly innovative art school Bezalel in Jerusalem is Heart-Beans, a coffee grinder which when you hold it close to your body, like a baby, grinds coffee based on the rhythm of your heart.Oh, baby! Spin for me!
. . .
It’s pretty cool. It’s pretty smart. Everyone loves coffee - ‘cept for those snooty tea drinkers. And it’s technology with heart as you can see in the video below... It’s the robot that fulfills your innermost desire. In this case, coffee. Deep, rich and dark, from the bottom of your heart (beat). Ground with love - or whatever else you’ve got brewing inside."
-Wes
PS: Be sure to see the videos: for guys here and gals here. Have a great weekend!
Wednesday, June 25, 2008
More Fear-Based Medical Marketing
I'm not sure it gets better than this:
Scanning the heart's arteries for calcium deposits accurately predicts the overall death risk for American adults, a new study suggests.I can hear it now:
"So far, this is the best predictor we have of who will have a problem and who will not," said study co-researcher Dr. Matthew Budoff, associate professor of medicine at the Harbor-UCLA Medical Center.
He and his colleagues reported the finding in the July 1 issue of the Journal of the American College of Cardiology.
A calcium scan looks for calcification, a hardening of the arteries caused by high blood fats and calcium deposits that can eventually block blood vessels, causing heart attacks, strokes and other major problems.
"Hey Marge, hey lookie here in the Washington Post! I wanna get one of dem der fancy schmancy CT scanner gizmos to find out if I'm gonna DIE sooner than you are! Let's take $600 bucks for that fancy schmancy thing-a-ma-bob out of our retirement fund. It'd be WORTH IT!"-Wes
Sometime later, in the doctor's office...
Doctor: "Well, Mr. Jones, I see my this fancy schmancy CT scan that you'd got some calcium in your coronaries. Hmmmm. And you calcium score is 210, just like Tim Russert! So, guess what?"
Mr. Jones: "What?"
Doctor: "Well Mr. Jones, you're at increased risk of DYING!"
Mr. Jones: "Uh, what do you mean, Doctor?"
Doctor: "You heard me: you're at increased risk of DYING with all that calcium in those coronaries - you know - BAM! Just like Tim Russert."
Mr. Jones: "Any idea when, Doctor?"(Silence)
Mr Jones: "Doctor, did you hear me? When will I die? I mean, won't we all die sometime?"
Doctor: "Heck, Mr. Jones, I don't know! But I can assure you that based on this fine article here in the prestigious Journal of the American College of Cardiology (you know, the same one that's also promoting their new Cardiovascular Imaging journal) that you're gonna die of SOMETHING sooner than some of the other people who don't have that evil calcium in their arteries."
Mr. Jones: "Gosh. So what should I DO about it, Doctor?"
Doctor: "Well, you know, since we're proposing that it's a RISK FACTOR for DYING, you should do the usual stuff: eat right, take tons of statin drugs, don't smoke, take your aspirin, lose weight, eat a low trans fat, high antioxidant, super-radical-consuming diet, do yoga, take mega vitamins, face East, say a few 'Hail Mary's..."
Mr. Jones: "Uh, but I was already doing that stuff..."
Doctor: "Have you had your CRP level and genes tested yet?"
Mr. Jones: "How would that help?"
Doctor: "Well, Mr. Jones, it might mean your risk of DEATH is EVEN GREATER!"
Mr. Jones: "But what can I do about it if it's positive also?"
Doctor: "Well, you know, the usual stuff... like I said... eat right, take tons of..."
Mr. Jones: "That's okay, Doctor. I've had enough. Thanks for all of your help. Hope that $300 bucks comes in handy. Don't mind me: I'll keep doing what I've been doing and get started preparing my Bucket List. Oh, but one more thing..."
Doctor: "What's that Mr. Jones?"
Mr. Jones: "You wouldn't happen to work with General Electric like those two guys who wrote that article you quoted, would you?"
Tuesday, June 24, 2008
Looking for a Job?
If you're a new doctor in the hunt for a job after training, a new family physician blogger, Jonathan Dee from Clinton, TN, has some suggestions on how to get started.
(I wonder if Dr. Dee knows that he works about 15 miles from Dr. Helen and Instapundit?)
-Wes
(I wonder if Dr. Dee knows that he works about 15 miles from Dr. Helen and Instapundit?)
-Wes
Your Beatin' Heart
Check out this interactive heart animation from Hydrid Medical Illustration. You can use the slider on the video loop to create a "glass heart" through which you can see the heart valves and other structures inside the heart as the heart beats.
Pretty cool.
Hmmmm. I wonder if they could animate atrial fibrillation?
-Wes
PS: You can also check out their blood flow animation, too.
Pretty cool.
Hmmmm. I wonder if they could animate atrial fibrillation?
-Wes
PS: You can also check out their blood flow animation, too.
AED's - The Barriers to Entry
Melinda Beck of the Wall Street Jounal, did a nice piece on the need for automatic external defibrillators (AEDs) in public spaces today and started to address some of the issues of why these amazing gizmo's aren't available more widely:
So why aren't these devices more readily available?
First and foremost: is cost. These devices are still expensive: the cheapest quoted goes for about $1300. But there are other costs not commonly discussed: like the cost of new batteries every 2-7 years (depending on the cost of the model) that can set folks back at least a $100 for each device. And what about those defibrillator patches placed on the chest? They contain a gel that improves the conductivity of the patches on the chest, making the devices more reliable at correcting the normal heart rhythm. That gel degrades and the patches must be replaced every two to seven years, too - to the tune of about $100 a set, too. These are the unspoken issues with AEDs that are never written about and schools and institutions must understand these additional costs and maintenance requirements if they are to assure the proper functioning of these devices.
Next, is the location consideration: where will these devices be used? Will they be in the office setting, car trunk, or placed next to the baseball field? Humidity, motion, and other environmental issues might require a more expensive device to be deployed without the bargain-basement price. Certainly, in the NIH-sponsored trial "Home Automated External Defibrillator Trial (HAT)," home use has not been found to be more effective than a conventional call to 911: in part because of the low incidence of events that occur in the home when a responder is present (58 patients out of 7001 studied, and only 32 had AEDs used and only 4 survived to hospital discharge).
But the cost and efficacy considerations might be offset if more defibrillators were deployed in public spaces where more responders were present and events occurred - thereby driving down the costs. I suppose it would be utopia if these devices could be deployed and maintained within 3 minutes of whereever a person traveled. But the path to implementation, especially with staffing and budget shortfalls, is a lengthy one. As a case in point: many doctors' offices, dialysis centers, and rehab units still do not have these devices and instead rely on calling 911 for a response in emergencies.
Sad, but true.
-Wes
Some states now require AEDs in schools; some require them in health clubs, shopping malls and golf courses. There's little uniformity; despite their foolproof nature, some businesses oppose them out of fear of being sued if something goes awry with an on-site AED. "I predict that 10 years from now, people will say, 'I'm not going to work in a building or stay in a hotel or eat in a restaurant that doesn't have an AED," says San Diego city-council member Jim Madaffer, who helped place nearly 5,000 AEDs in public facilities since 2001. They've saved 49 lives.As electrophysiologists, we often get to see the "saves" made by these devices: the young boy playing baseball, struck in the chest by a fast ball ("commodio cordis") that fibrillates his heart and the police officer who responds with the AED in the trunk of his squad car to save the boy's life; or the father who collapses just outside the fire department and is rescued by their defibrillator. These event happen every day, but unfortunately as experienced in the Tim Russert case, many more are not so fortunate.
Schools have been a tough sell, too, largely because of cost. Some parents are raising money for AEDs themselves, often after a tragedy. Evelyn and Larry Pontbriant have donated 32 AEDs to Norwich, Conn., schools since last summer, when their 15-year-old son, an athlete with no known heart problems, suffered a fatal cardiac arrest during a running event in the local park. An AED arrived on the scene too late. "It's a good investment to have on hand in your school," says Mrs. Pontbriant. "It benefits not just the athletes, but also the teachers, coaches, referees, grandparents and siblings."
So why aren't these devices more readily available?
First and foremost: is cost. These devices are still expensive: the cheapest quoted goes for about $1300. But there are other costs not commonly discussed: like the cost of new batteries every 2-7 years (depending on the cost of the model) that can set folks back at least a $100 for each device. And what about those defibrillator patches placed on the chest? They contain a gel that improves the conductivity of the patches on the chest, making the devices more reliable at correcting the normal heart rhythm. That gel degrades and the patches must be replaced every two to seven years, too - to the tune of about $100 a set, too. These are the unspoken issues with AEDs that are never written about and schools and institutions must understand these additional costs and maintenance requirements if they are to assure the proper functioning of these devices.
Next, is the location consideration: where will these devices be used? Will they be in the office setting, car trunk, or placed next to the baseball field? Humidity, motion, and other environmental issues might require a more expensive device to be deployed without the bargain-basement price. Certainly, in the NIH-sponsored trial "Home Automated External Defibrillator Trial (HAT)," home use has not been found to be more effective than a conventional call to 911: in part because of the low incidence of events that occur in the home when a responder is present (58 patients out of 7001 studied, and only 32 had AEDs used and only 4 survived to hospital discharge).
But the cost and efficacy considerations might be offset if more defibrillators were deployed in public spaces where more responders were present and events occurred - thereby driving down the costs. I suppose it would be utopia if these devices could be deployed and maintained within 3 minutes of whereever a person traveled. But the path to implementation, especially with staffing and budget shortfalls, is a lengthy one. As a case in point: many doctors' offices, dialysis centers, and rehab units still do not have these devices and instead rely on calling 911 for a response in emergencies.
Sad, but true.
-Wes
Monday, June 23, 2008
The Feeding Frenzy Has Begun
... and it's all about the research money:
"An e-mail sent Wednesday to top Feinberg faculty from Rex L. Chisholm, dean of research, included an attachment that lists 29 researchers employed by Evanston Northwestern who draw federal research dollars. Those people will lose their Northwestern faculty positions as the affiliation is unwound over the next year.-Wes
“The dean’s office is interested in hearing from you if you have interest in exploring the possibility of recruiting any of them to NU,” Dr. Chisholm’s message says. He requests “a guesstimate of the resources that might be required to successfully move them to NU.”
About 700 of Northwestern’s 3,000 full- and part-time faculty work at Evanston Northwestern. The three-hospital system has its own research enterprise — it received more than $100 million in external grant money in 2007 — and competes with Northwestern for federal funding."
The Obfuscation of Benefits
"Dr. Wes, I couldn't believe the prices after my wife's surgery and three and a half-day hospital stay."
"Yeah, it's crazy, isn't it? But the prices aren't really the prices, you know - everything's marked up because hospitals know they won't get paid the full amount by the insurers."
"Really?"
"Yeah."
"So why did my remaining deductible that I had to pay go to the hospital so they'd make 100% of their billed amount when the guys doing the surgery only got 29% of what they billed?"
"What do you mean?"
"I got sent this form that said it was my 'Explanation of Benefits' from my insurer..."
"Yeah."
"... and the hospital's portion of the bill was $53,619.70 and they got paid 100% of what they billed from my insurer provided, of course, you include my co-pay. You want to see? Here's what they sent me for the hospital charges:"
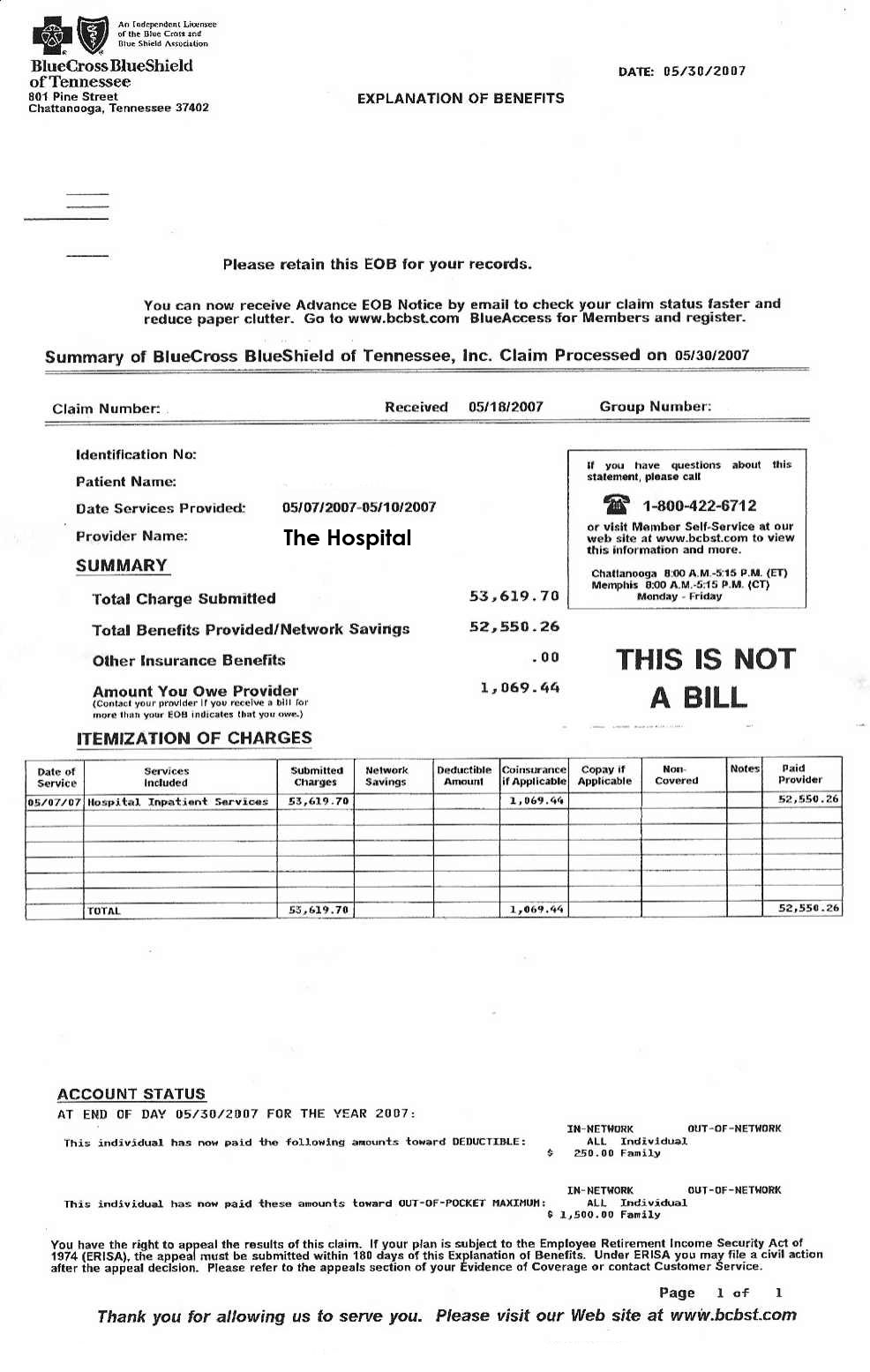
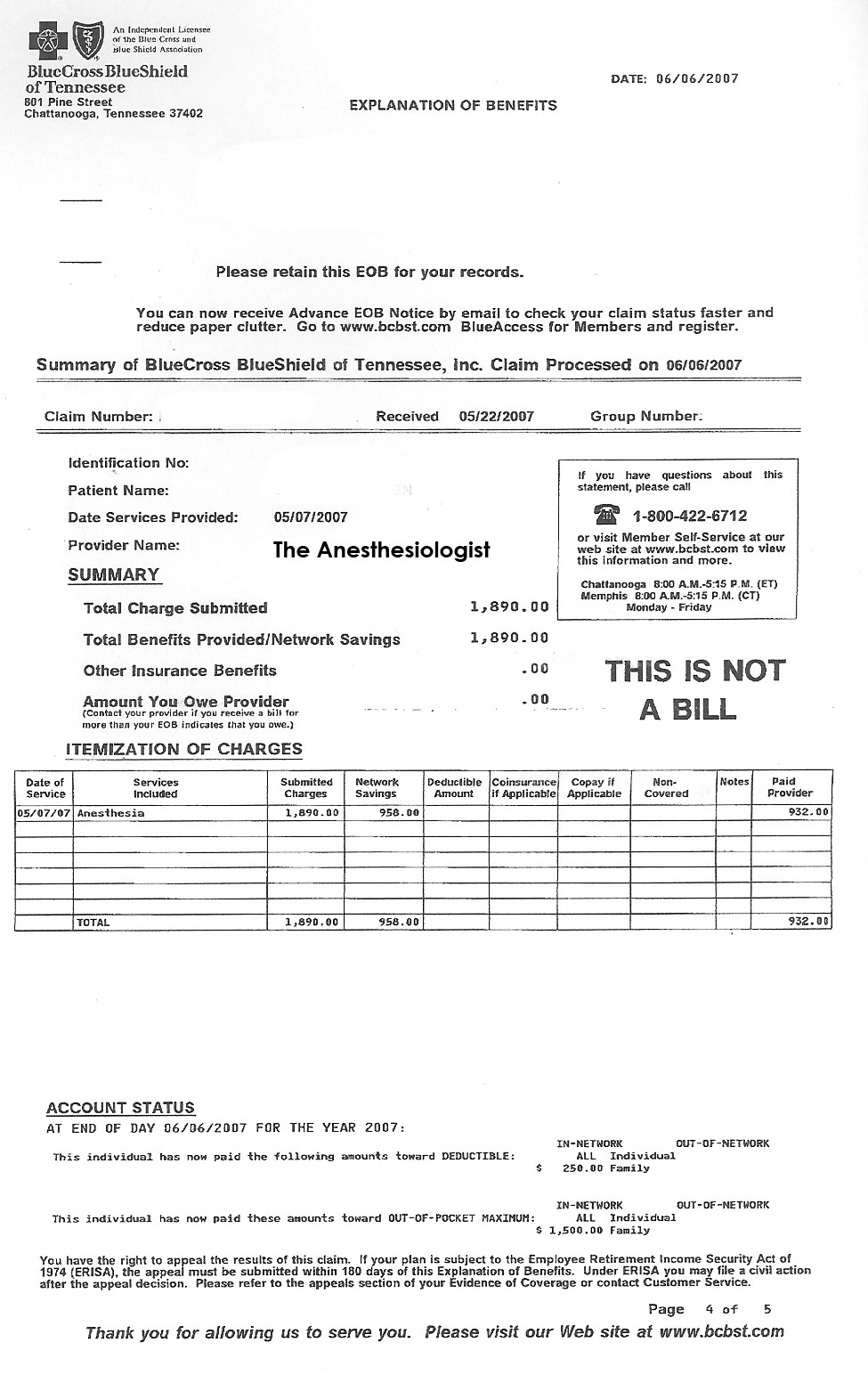
"See? I had to pay my co-pay so the hospital made 100% of what they billed... and yet the surgeon who did the surgery only made 29% of what he billed. Here's two 'Explanation of Benefit' forms of what they paid my surgeon....:"
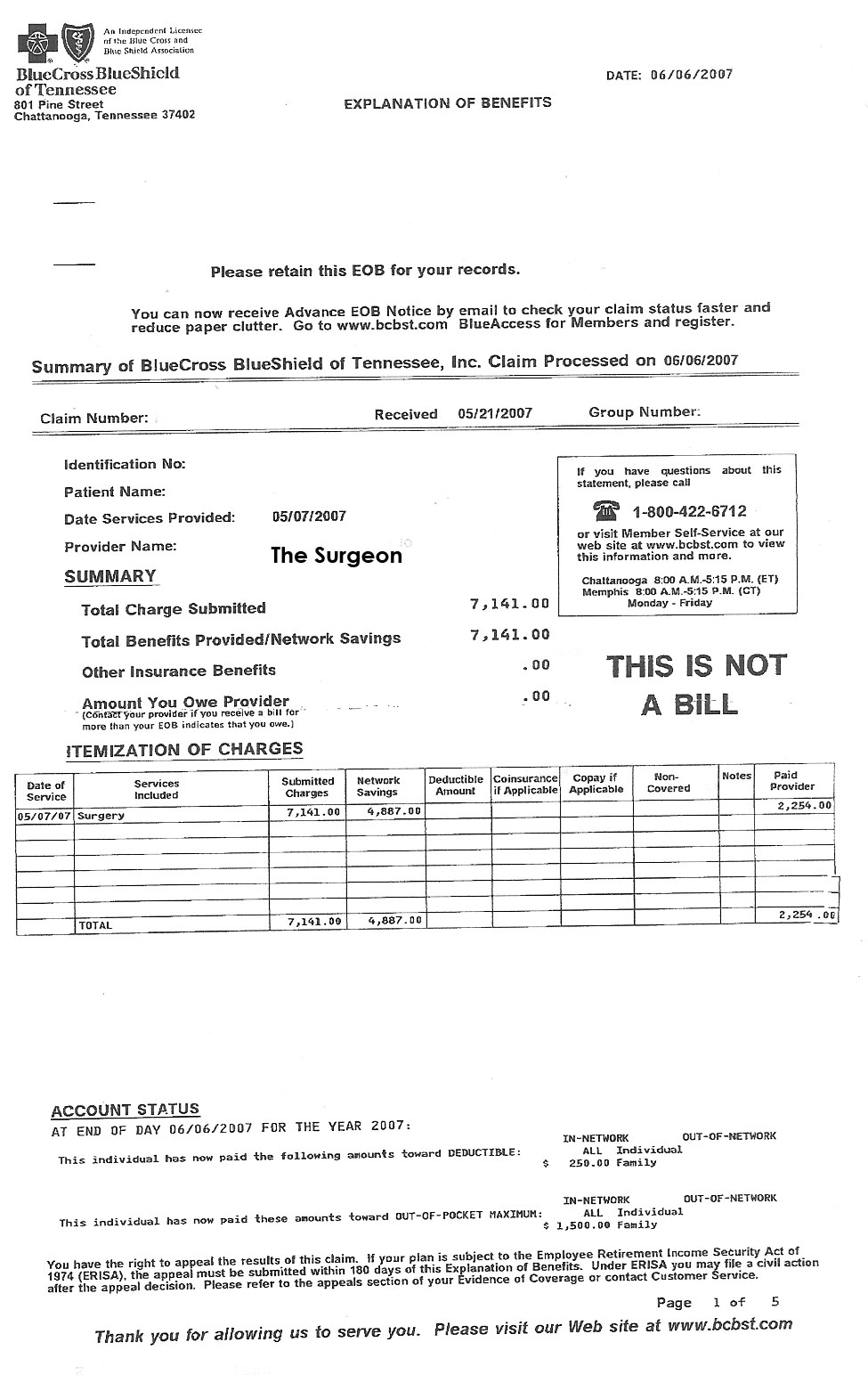

"... I mean, why two payments to my surgeon? And why didn't he get paid the full amount he billed? He was the one doing the surgery, right? I would have rather my co-payment go to the guy doing the surgery rather than the hospital..."
"I'm sorry, I can't answer your questions."
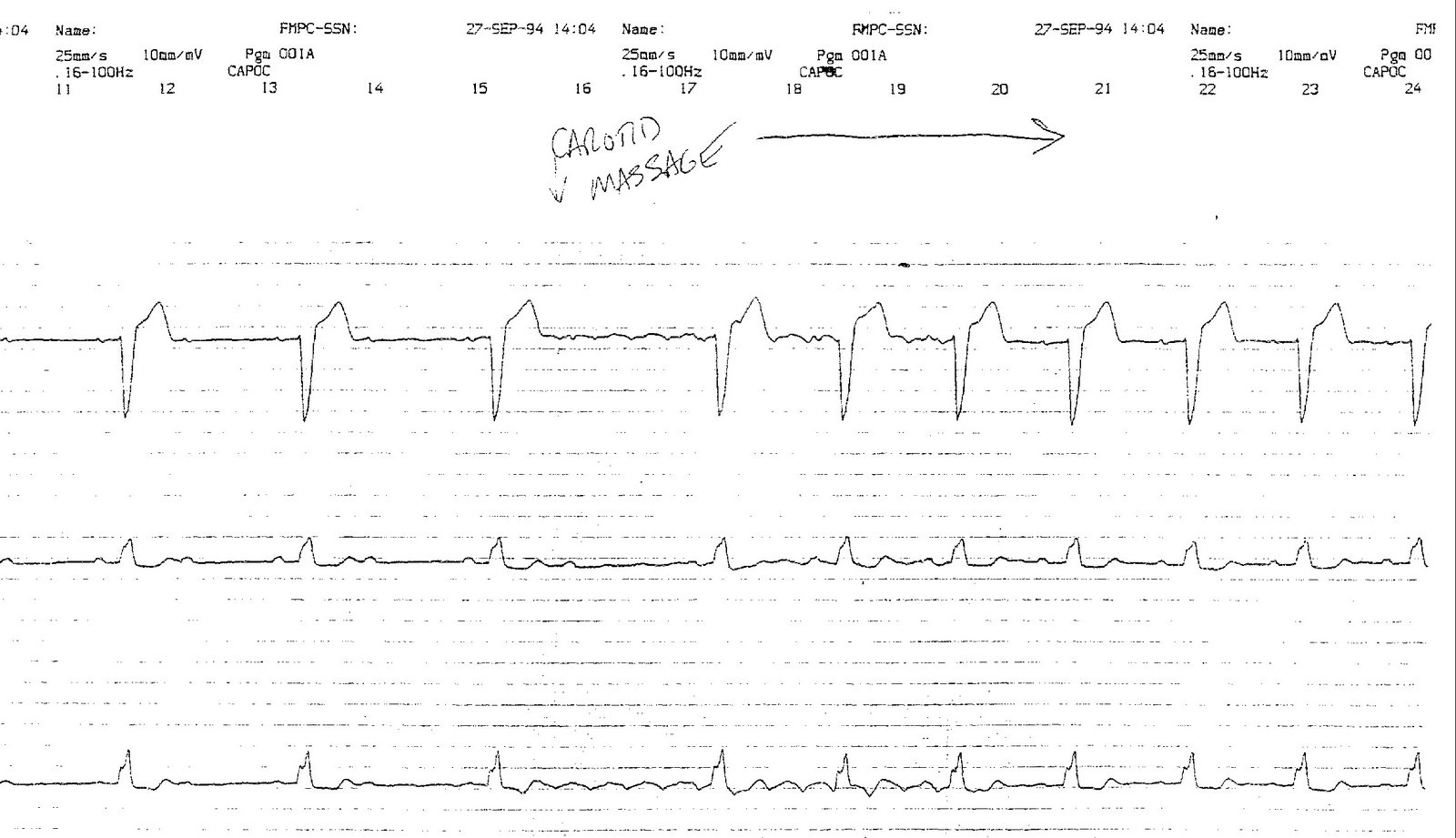
"I mean, even the anesthesiologist got paid only 51% of what he billed, but the hospital got 100%! Look:"
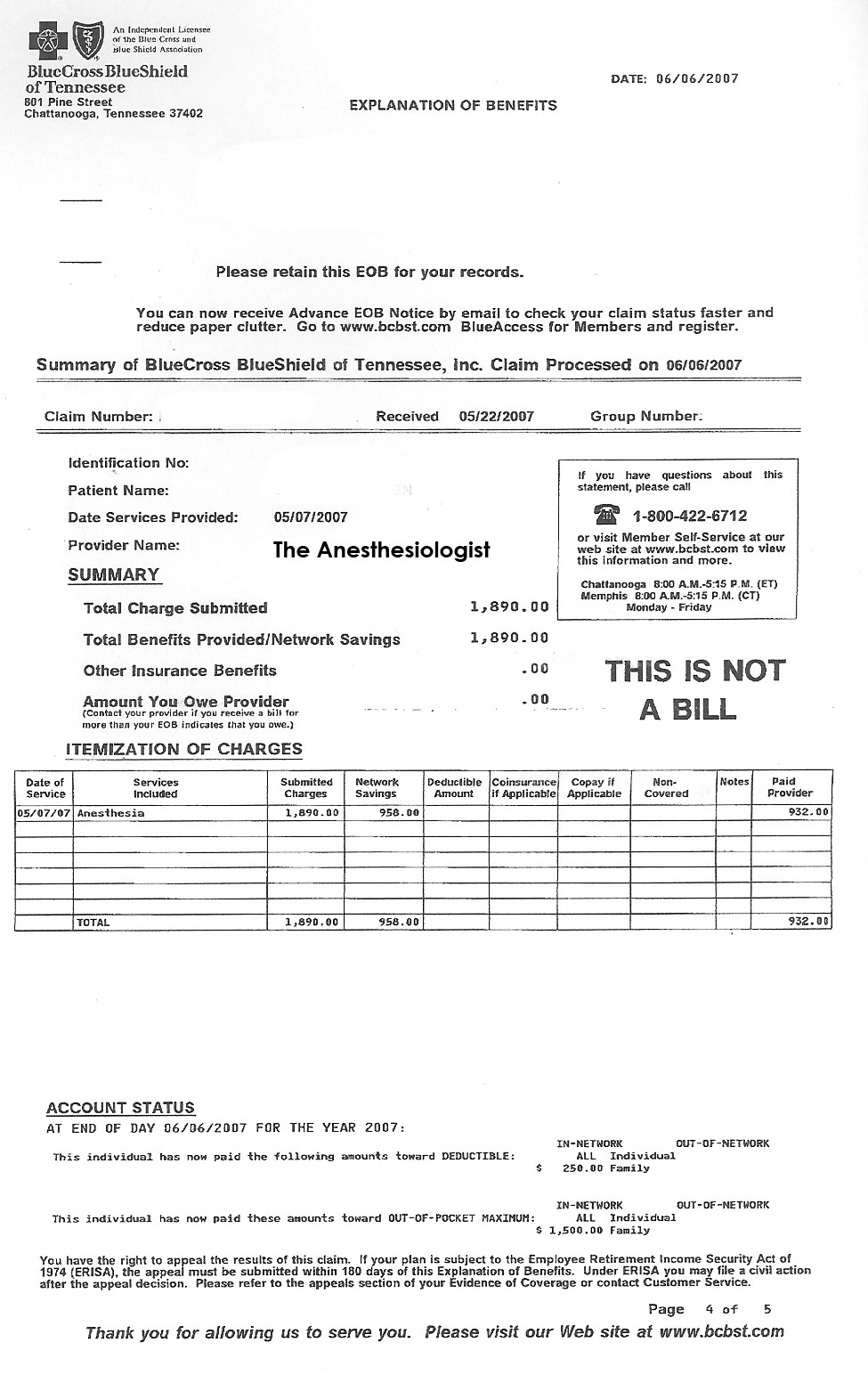
"...I mean, wasn't the anesthesia guy pretty important to my wife when her surgery was going on? Why should the hospital get 100% and he make only a portion of what he billed?"
"That's the way it works, I'm afraid."
"You know what doc?"
"What?"
"That sucks. And you know what else?"
"What?"
"How the hell am I supposed to figure this out with such crappy itemization on these so-called 'Explanation of Benefits' forms? They should really be called 'Obfuscation of Benefits' forms; at least that name would lend them a modicum of credibility."
-Wes
"Yeah, it's crazy, isn't it? But the prices aren't really the prices, you know - everything's marked up because hospitals know they won't get paid the full amount by the insurers."
"Really?"
"Yeah."
"So why did my remaining deductible that I had to pay go to the hospital so they'd make 100% of their billed amount when the guys doing the surgery only got 29% of what they billed?"
"What do you mean?"
"I got sent this form that said it was my 'Explanation of Benefits' from my insurer..."
"Yeah."
"... and the hospital's portion of the bill was $53,619.70 and they got paid 100% of what they billed from my insurer provided, of course, you include my co-pay. You want to see? Here's what they sent me for the hospital charges:"
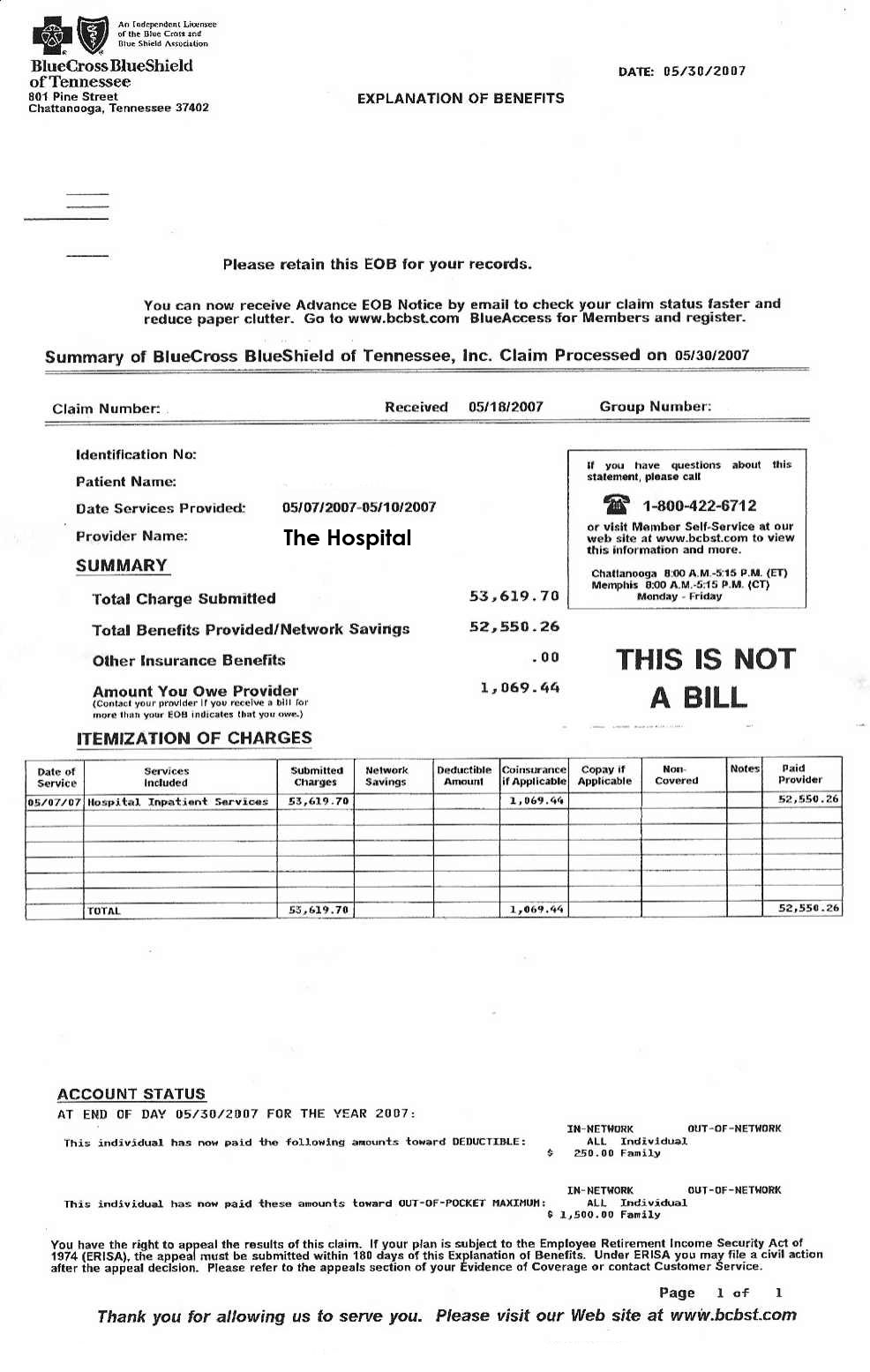
Click image to enlarge.
"See? I had to pay my co-pay so the hospital made 100% of what they billed... and yet the surgeon who did the surgery only made 29% of what he billed. Here's two 'Explanation of Benefit' forms of what they paid my surgeon....:"
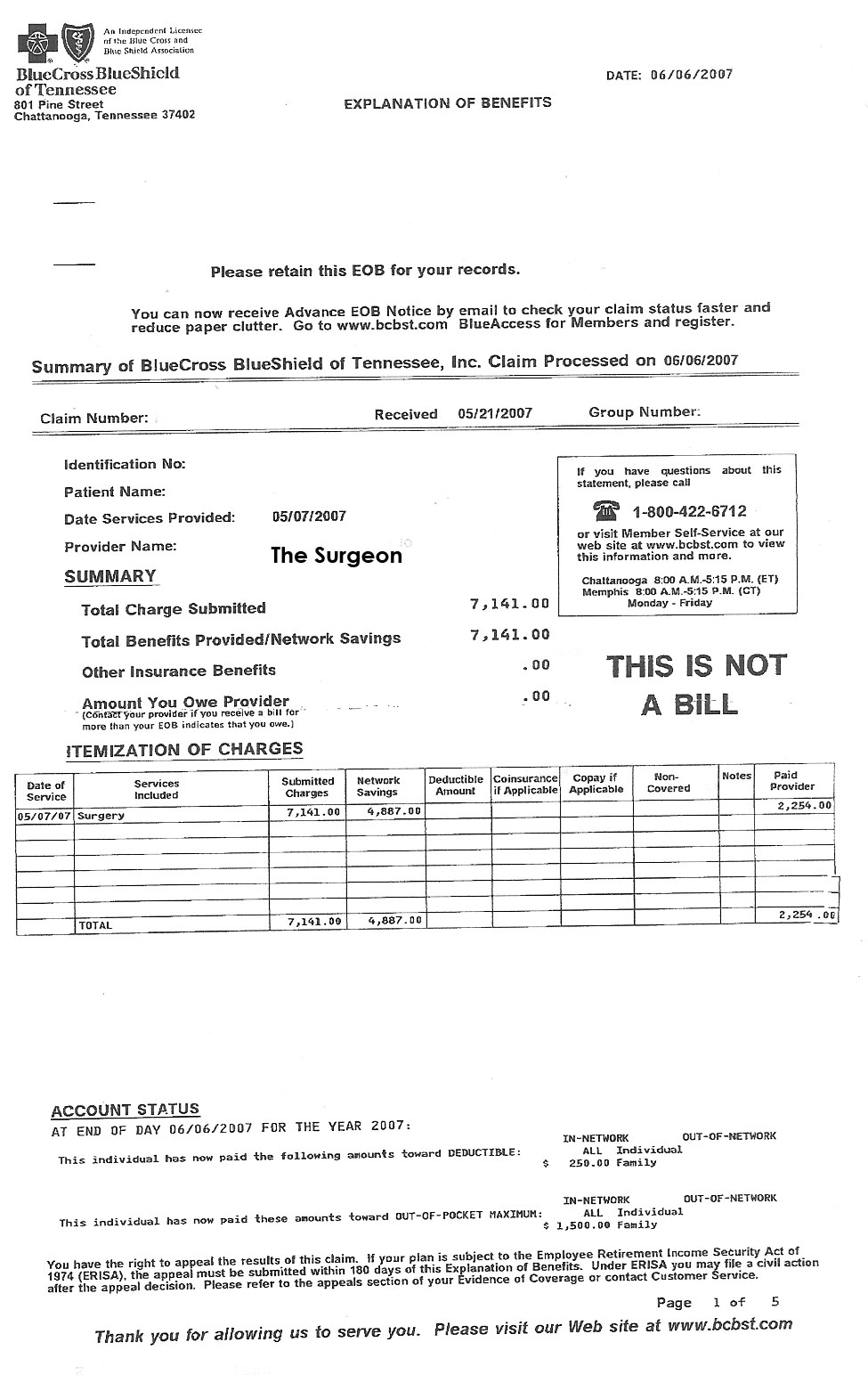
Click image to enlarge.

Click image to enlarge.
"... I mean, why two payments to my surgeon? And why didn't he get paid the full amount he billed? He was the one doing the surgery, right? I would have rather my co-payment go to the guy doing the surgery rather than the hospital..."
"I'm sorry, I can't answer your questions."
"I mean, even the anesthesiologist got paid only 51% of what he billed, but the hospital got 100%! Look:"
Click image to enlarge.
"...I mean, wasn't the anesthesia guy pretty important to my wife when her surgery was going on? Why should the hospital get 100% and he make only a portion of what he billed?"
"That's the way it works, I'm afraid."
"You know what doc?"
"What?"
"That sucks. And you know what else?"
"What?"
"How the hell am I supposed to figure this out with such crappy itemization on these so-called 'Explanation of Benefits' forms? They should really be called 'Obfuscation of Benefits' forms; at least that name would lend them a modicum of credibility."
-Wes
Thursday, June 19, 2008
Taking a Break
Dr. Wes will be taking a blog break far from internet access with family 'til Monday. See you then.
-Wes
-Wes
Wednesday, June 18, 2008
A Pacemaker for the Diaphragm
Getting patients off a ventillator with diaphragmatic pacing: a simple idea whose time has come. Manufactured by Synapse Biomedical, Inc., this pacing system allows people to get off the ventillator for as long as four hours a day.
Remarkable.
-Wes
Remarkable.
-Wes
Tuesday, June 17, 2008
The Tim Russert Fallout
It’s hard for me not to sit amazed at the job medicine has done convincing people we can control heart attacks. One only needs to review the many news stories regarding news journalist Tim Russert's untimely death to see the public fallout of our efforts to "educate" the populace about "screening tests" used to "prevent" the likelihood of having a heart attack. You see, with Mr. Russert's death, those tests have suffered a huge public relations nightmare.
Cholesterol screening and statins: dead in the water.
CT scanning for detection of plague to prevent heart attack: harpooned.
Stress testing to assure you're protected against the Big One: pulverized.
Not one damn thing predicted (or prevented) Mr. Russert's death.
Oh sure, there's plenty of others who want to jump right in to promote the next great lifestyle modification, rather than those damn cholesterol drugs as a way to save your life, provided of course, you buy their book. Or those who promise reduced mortality if everyone just got an ultrasound of their carotid arteries, even though this test still can't predict acute plaque rupture and the onset of a heart attack like Mr. Russert's.
You see, the entire industrial complex of healthcare technology and innovation was shaken, not because Mr. Russert was a nice guy and great journalist, but rather because they will have to explain why their technology isn't worth a damn at predicting heart attacks.
Welcome, my friends, to the world of real-life medicine rather than marketing.
-Wes
Cholesterol screening and statins: dead in the water.
CT scanning for detection of plague to prevent heart attack: harpooned.
Stress testing to assure you're protected against the Big One: pulverized.
Not one damn thing predicted (or prevented) Mr. Russert's death.
Oh sure, there's plenty of others who want to jump right in to promote the next great lifestyle modification, rather than those damn cholesterol drugs as a way to save your life, provided of course, you buy their book. Or those who promise reduced mortality if everyone just got an ultrasound of their carotid arteries, even though this test still can't predict acute plaque rupture and the onset of a heart attack like Mr. Russert's.
You see, the entire industrial complex of healthcare technology and innovation was shaken, not because Mr. Russert was a nice guy and great journalist, but rather because they will have to explain why their technology isn't worth a damn at predicting heart attacks.
Welcome, my friends, to the world of real-life medicine rather than marketing.
-Wes
Monday, June 16, 2008
Ending an Era
It's official: ENH and Northwestern are parting. It's a sad day, really. The relationship, while strained, was a good one in many ways for both parties. But business is business, and the complexities of the ever-changing Chicago healthcare market have strained the marriage to its breaking point.
Now ENH must choose a new name, change its stationary, find a new academic partner, re-establish some 180 academic appointments, re-certify its training programs, and work toward re-branding itself.
It'll be interesting, to say the least. I'll be interested to see what the community thinks...
-Wes
Addendum: More from the Chicago Tribune.
Now ENH must choose a new name, change its stationary, find a new academic partner, re-establish some 180 academic appointments, re-certify its training programs, and work toward re-branding itself.
It'll be interesting, to say the least. I'll be interested to see what the community thinks...
-Wes
Addendum: More from the Chicago Tribune.
Why People Can't Afford Insurance
Maybe this little tidbit will bring some clarity to the issue:
-Wes
"Almost every CEO of a publicly traded health insurance company made more than the median salary for a top executive in the S&P 500 in 2007.When the heck will this trend cease?
...
In its analysis of S&P 500 companies, Equilar found median total compensation for the CEOs was $8.8 million. The six publicly traded health plans that are a part of the S&P 500 index all paid their CEOs more than that median: from $9.1 million for WellPoint's Angela Braly to $25.8 million for Cigna's H. Edward Hanway."
-Wes
Predicting the Future
In 2005, the Physician Quality Reporting Initiative, an effort by the Center for Medicare and Medicaid Services (CMS) to assure quality healthcare was tied to physician reimbursement, began with a mere 36 measures. This initiative has grown steadily, such that now 138 measures (with 16 new ones just last week!) have been defined.
I wondered if there was a growth trend that could be predicted as to how many quality measures for physicians will exist by 2019, when the Medicare Trust Fund is predicted to be bankrupt.
What was striking, was the remarkably linear relationship of growth of these measures. If one applies a least squares method to determine the annual rate of growth of measures so far, the number of measures is defined by the equation:
Here's how the graph looks:

So if this formula holds true, by 2019 physicians should expect 386 measures to track!
Wow. Let's look at that. If we have an 8 hour work day, and there are 60 minutes in an hour, then there are 480 minutes to the average work day. If each of these measures take, say, one minute to collect and record, then 94 minutes will be left over to see patients.
Now, if we leave 15 minutes for a potty break and maybe a very quick bite to eat, then we've whittled it down to 79 minutes left for patient care. If the average doctor expects to see 20 patients a day, then 3.95 minutes will be devoted to each patient.
All in the name of healthcare rationing.
Keep up the good work, CMS!
-Wes
I wondered if there was a growth trend that could be predicted as to how many quality measures for physicians will exist by 2019, when the Medicare Trust Fund is predicted to be bankrupt.
What was striking, was the remarkably linear relationship of growth of these measures. If one applies a least squares method to determine the annual rate of growth of measures so far, the number of measures is defined by the equation:
y = mx + b, where:
y = number of measures
m = 25
b = 11
Here's how the graph looks:

So if this formula holds true, by 2019 physicians should expect 386 measures to track!
Wow. Let's look at that. If we have an 8 hour work day, and there are 60 minutes in an hour, then there are 480 minutes to the average work day. If each of these measures take, say, one minute to collect and record, then 94 minutes will be left over to see patients.
Now, if we leave 15 minutes for a potty break and maybe a very quick bite to eat, then we've whittled it down to 79 minutes left for patient care. If the average doctor expects to see 20 patients a day, then 3.95 minutes will be devoted to each patient.
All in the name of healthcare rationing.
Keep up the good work, CMS!
-Wes
Sunday, June 15, 2008
I Envision a New Medical World Order
Well, I don't, but Happy does:
-Wes
If anyone in Washington believes PQRI or any other of an assortment of quality systems will put the brakes on health care inflation, they are fools. If you believe they are doing it for quality over money, you are a fool. It's not a quality issue. It's a money issue. And the money train is delivered by volume. We do too much. Way too much. And we do it because we get paid to do it. We do it because we get sued if we don't do it. We do it because the gravy train has a spigot that has no off position. We do it because patients have become doctors. We do it because drug companies have brainwashed the public. We do it because the lobbyists in Washington pay hundreds of millions of dollars in bribe money to keep their piece of the gravy train flowing. I see it every day. I get 10 pieces of junk mail a day telling me what I need to prescribe, what I need to order, what procedures I need to learn.Read it. It's worth it.
-Wes
Friday, June 13, 2008
Russert Dead of Apparent Heart Attack
 Bummer.
Bummer.Exchanges like these will be sorely missed:
Russert: The night you took the country to war, March 17th, you said this: "Intelligence gathered by this and other governments leaves no doubt that the Iraq regime continues to possess and conceal some of the most lethal weapons ever devised."Tim, you'll be sorely missed.
President Bush: Right.
Russert: That apparently is not the case.
President Bush: Correct.
Russert: How do you respond to critics who say that you brought the nation to war under false pretenses?
President Bush: Yes. First of all, I expected to find the weapons. Sitting behind this desk making a very difficult decision of war and peace, and I based my decision on the best intelligence possible, intelligence that had been gathered over the years, intelligence that not only our analysts thought was valid but analysts from other countries thought were valid.
And I made a decision based upon that intelligence in the context of the war against terror. In other words, we were attacked, and therefore every threat had to be reanalyzed. Every threat had to be looked at. Every potential harm to America had to be judged in the context of this war on terror.
And I made the decision, obviously, to take our case to the international community in the hopes that we could do this — achieve a disarmament of Saddam Hussein peacefully. In other words, we looked at the intelligence. And we remembered the fact that he had used weapons, which meant he had had weapons. We knew the fact that he was paying for suicide bombers. We knew the fact he was funding terrorist groups. In other words, he was a dangerous man. And that was the intelligence I was using prior to the run up to this war.
Now, let me — which is — this is a vital question —
Russert: Nothing more important.
President Bush: Vital question.
And so we — I expected there to be stockpiles of weapons. But David Kay has found the capacity to produce weapons. Now, when David Kay goes in and says we haven't found stockpiles yet, and there's theories as to where the weapons went. They could have been destroyed during the war. Saddam and his henchmen could have destroyed them as we entered into Iraq. They could be hidden. They could have been transported to another country, and we’ll find out. That's what the Iraqi Survey Group — let me — let me finish here.
But David Kay did report to the American people that Saddam had the capacity to make weapons. Saddam Hussein was dangerous with weapons. Saddam Hussein was dangerous with the ability to make weapons. He was a dangerous man in the dangerous part of the world.
And I made the decision to go to the United Nations.
By the way, quoting a lot of their data — in other words, this is unaccounted for stockpiles that you thought he had because I don't think America can stand by and hope for the best from a madman, and I believe it is essential — I believe it is essential — that when we see a threat, we deal with those threats before they become imminent. It's too late if they become imminent. It's too late in this new kind of war, and so that's why I made the decision I made.
Russert: Mr. President, the Director of the CIA said that his briefings had qualifiers and caveats, but when you spoke to the country, you said "there is no doubt." When Vice President Cheney spoke to the country, he said "there is no doubt." Secretary Powell, "no doubt." Secretary Rumsfeld, "no doubt, we know where the weapons are." You said, quote, "The Iraqi regime is a threat of unique urgency.” “Saddam Hussein is a threat that we must deal with as quickly as possible."
You gave the clear sense that this was an immediate threat that must be dealt with.
President Bush: I think, if I might remind you that in my language I called it a grave and gathering threat, but I don't want to get into word contests.
-Wes
Thursday, June 12, 2008
Guys' Health Issues Kick Off ENH Radio
Wow, we've entered Web 2.0 at our institution as we delve into weekly podcasts. Feel free to check it out: the first two shows are for guys.
I've been asked to do one for atrial fibrillation sometime in late July or early August...
-Wes
I've been asked to do one for atrial fibrillation sometime in late July or early August...
-Wes
EKG Du Jour - #9
Another from the EKG Hall of Fame:
-Wes
PS: (EP's: please refrain for about 12 hours or so to let others have some fun... thanks!)
An elderly man presents to the ER for a laceration of his hand and was noted to be bradycardic. An rhythm strip was performed and documented a wide complex, bradycardic rhythm. You are asked to see him.
He was completely asymptomatic, but the ER doctors were concerned and thought he might need a pacemaker. You decide to perform carotid massage, with the results shown:
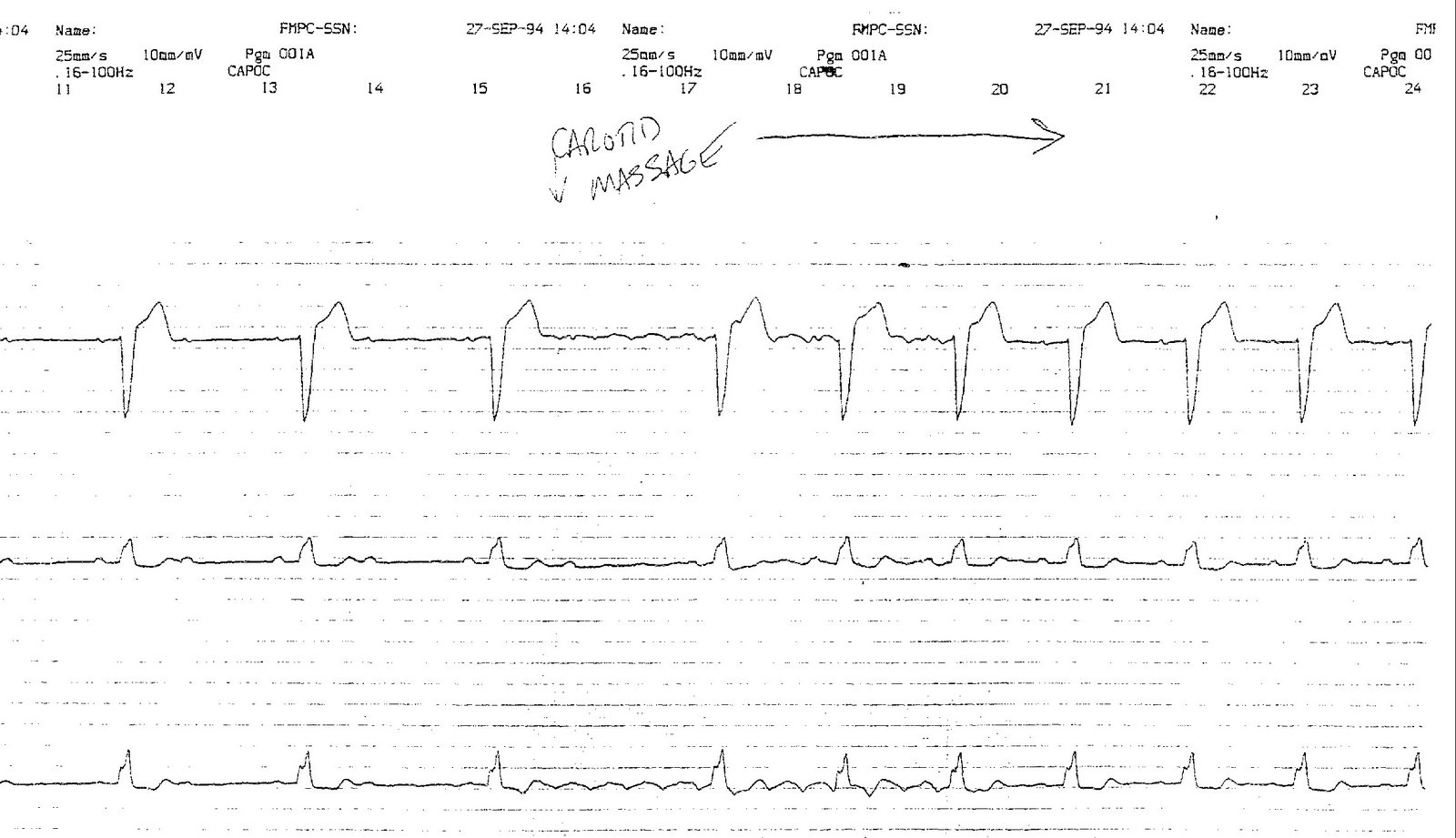
Click image to enlarge
-Wes
PS: (EP's: please refrain for about 12 hours or so to let others have some fun... thanks!)
The Diabetic Concept Car

... it's only the beginning. With this functionality, there will be no more need to worry when you ate your last cracker. Instead, if the device detects your blood sugar's so low that you might lose conciousness, it'll deploy the airbag just in time to wake your ass up!
But that's not all. Just think of the other possibilities we'll soon have with the advent of medical devices interacting with everyday objects.
 Now when you're in the throes of passion with your loved one, she'll soon be able to hear you revved up heart beat as your defibrillator reaches its tachycardia detect zone and puts on a full blown light show with our new Bluetooth-enabled Lightning Alarm Clock!
Now when you're in the throes of passion with your loved one, she'll soon be able to hear you revved up heart beat as your defibrillator reaches its tachycardia detect zone and puts on a full blown light show with our new Bluetooth-enabled Lightning Alarm Clock! Or use your supraventricular tachycardia to power your blender as you make those early morning smoothies for the family with the 5-speed polycarbonate VitaMix Super 5200 blender!
Or use your supraventricular tachycardia to power your blender as you make those early morning smoothies for the family with the 5-speed polycarbonate VitaMix Super 5200 blender!And now that the really cool G3-enabled iPhone here, you can be the first to upload your favorite heart-rate stimulating selections with the new iPod accessories promised soon! (Just be sure not to upload "Stairway to Heaven.")
Dang. I gotta get working on those patent applications...
-Wes
Wednesday, June 11, 2008
What's Hot on the Web? Health and Politics
Even though Walt Disney Co.'s ABC News is close to scrapping the current format of its daily "World News" Webcast, there are two sections they won't chuck:
-Wes
Inside ABC's Web division, the mantra is: "Hard news is a hard sell." Of last Monday's 7.8 million clicks, three million were to photo slideshows, including one of celebrities at the beach and another of the "pregnant man." Some hard-news categories have done well: Page views for the health and politics sections of the site have increased around threefold since last year, with 14.9 million page views for the health section in May and 19.4 million for politics. Mr. Westin says ABC plans to build these niche focuses.I mean, with such authoritative stories like this, I learn a lot, don't you?
-Wes
Kids Say the Darndest Things
One of our staff cardiologists is due to deliver in August, and her 3-year old son was overheard speaking to friends about the pregnancy:
-Wes
"My mommy is getting bigger and bigger. I think she's going to have a boy or a puppy."Heh. I guess he's not sure which one he wants...
-Wes
Tuesday, June 10, 2008
The Bits and Bytes of Pathology
Imagine: digital image processing and informatics complementing pathology - well, it's here, and Dr. Keith Kaplan, a former pathologist from our institution who has relocated to Mayo Clinic to pursue this area has a cool blog over at Digital Pathology Blog. As he says:
There's a lot more over there - he's been at it for a year: check it out and say "hi."
-Wes
The intent of this blog is to cover issues relevant to imaging and image analysis in pathology.I particularly liked his post with the video on "Combating Cervical Cancer With Cameraphones" which highlights how cameraphones are being used to deliver routine gynecologic care to rural Africa.
There's a lot more over there - he's been at it for a year: check it out and say "hi."
-Wes
Monday, June 09, 2008
More Rain on the "Report Card" Parade
It seems hospital "report cards" documenting "quality measures" fail to predict "preventable" deaths after bypass surgery.
Maybe the idea of Medicare reimbursing for "pay-for-performance" measures really misses the point: they should pay for outcomes, not for the performance of mere documentation. It's like asking a student to grade their own class performance: funny how almost all of them get A's that way.
For instance, here's the "quality data" of three different hospitals in our area:
Now, which of these three hospitals will give you the lowest bypass mortality?
Stumped? Gosh, how can you be? I mean the data are so, well, CLEAR!
Just think: how many chart-reviewers were required to review these charts and gather these data? How many hours? How much money do we spend annually to assure these "quality" data are posted to make the governmental "grade?" Most importantly, with hospital reimbursements tied to such worthless performance measures, how are our patient "consumers" ever going to use this data when the variance between centers is so slight and skewed consistently toward perfection?
You get what you pay for, alright. Pay for "good" data and you'll get "good" data. After all, it's the "Skinner Box" effect: if hospitals push the right levers, they get their "conditional reward" of slightly higher Medicare reimbursements.
Even if these measures don't mean dog-doo-doo.
-Wes
Maybe the idea of Medicare reimbursing for "pay-for-performance" measures really misses the point: they should pay for outcomes, not for the performance of mere documentation. It's like asking a student to grade their own class performance: funny how almost all of them get A's that way.
For instance, here's the "quality data" of three different hospitals in our area:
| Percent of Surgery Patients Who Received Preventative Antibiotic(s) One Hour Before Incision | 92% of 885 patients | 95% of 435 patients | 94% of 357 patients |
| Percent of Surgery Patients Who Received the Appropriate Preventative Antibiotic(s) for Their Surgery | 98% of 909 patients | 97% of 448 patients | 97% of 362 patients |
| Percent of Surgery Patients Whose Preventative Antibiotic(s) are Stopped Within 24 hours After Surgery | 90% of 856 patients | 90% of 417 patients | 87% of 339 patients |
| Percent of Surgery Patients Whose Doctors Ordered Treatments to Prevent Blood Clots (Venous Thromboembolism) For Certain Types of Surgeries | 92% of 182 patients | 92% of 150 patients | 95% of 178 patients |
| Percent of Surgery Patients Who Received Treatment To Prevent Blood Clots Within 24 Hours Before or After Selected Surgeries to Prevent Blood Clots | 92% of 182 patients | 92% of 150 patients | 88% of 178 patients |
Now, which of these three hospitals will give you the lowest bypass mortality?
Stumped? Gosh, how can you be? I mean the data are so, well, CLEAR!
Just think: how many chart-reviewers were required to review these charts and gather these data? How many hours? How much money do we spend annually to assure these "quality" data are posted to make the governmental "grade?" Most importantly, with hospital reimbursements tied to such worthless performance measures, how are our patient "consumers" ever going to use this data when the variance between centers is so slight and skewed consistently toward perfection?
You get what you pay for, alright. Pay for "good" data and you'll get "good" data. After all, it's the "Skinner Box" effect: if hospitals push the right levers, they get their "conditional reward" of slightly higher Medicare reimbursements.
Even if these measures don't mean dog-doo-doo.
-Wes
Sunday, June 08, 2008
Polypharmacy Gone Wild
If you've ever wondered why doctors gone insane managing patients, take a look at this inpatient drug treatment list on a single patient. It came to my attention on call this weekend that many of the drugs that seem repetitious are actually computer-generated by the electronic medical record "management:"
Does this save lives? Or does this cost patients for four different medications perhaps never needed? What is the cost of such automaticity when orders appear to manage patients without physician involvement? (That "little" order for glucagon, costs $104.82 retail at CostCo pharmacy. How much is it marked up for the hospital?)
Also, how many errors occur on the basis of misinterpretations of these automatic orders ("Oops, I forgot to ask if she was pregnant.")? Where are the evidence-based studies demonstrating the utility of this automated approach to patient care? Could this be why EMR's have not been found to save money to our health care system? Are we losing cost savings to our system by removing physician judgement?
In this era of cost overruns and exhorbitant Medicare expenditures, should we not be asking these tough questions?
No. That would be too difficult. Rather, it's far easier to cover your butt with automatically-generated orders that the patient has to pay for in the interest of assuring their own "safety."
-Wes
Furosemide SOLN 40 mg (LASIX)Note the last several highlighted formulations of glucose and glucagon. If the patient has diabetes, a "hypoglycemic protocol" order set is automatically generated by the pharmacy. (No doctor order is required, but the treating physician's name is attached automatically to the orders, and these orders are typically reviewed by hospital physician "experts" endocrinologists before being deployed). It seems there are glucose blood sugar cut-offs that mandate a different form of glucose to be administered to the patient. Here's our example of cook-book medicine:
Enoxaparin SOLN 135 mg
Carvedilol TABS 6.25 mg (COREG)
Furosemide TABS 20 mg
Valsartan TABS 80 mg (DIOVAN)
LevoFLOXacin SOLN 750 mg (Levaquin)
Polyethylene Glycol PACK 1 Each (MIRALAX)
Ferrous sulfate TABS 300 mg (FEOSOL)
Pantoprazole TBEC 40 mg (PROTONIX)
Docusate CAPS 200 mg (COLACE)
Hydrocodone-Acetaminophen 10-325 MG TABS 1-2 Tab (NORCO)
Ezetimibe TABS 10 mg (ZETIA)
FLAVOCOXID CAPS 250 mg
Ranolazine TB12 1,000 mg (RANEXA)
Clopidogrel TABS 75 mg (PLAVIX)
GlyBURIDE TABS 5 mg (MICRONASE)
Pioglitazone TABS 15 mg (ACTOS)
ROSUVASTATIN CALCIUM TABS 40 mg (CRESTOR)
Acetaminophen TABS 325-650 mg (TYLENOL)
Aspirin Enteric-Coated TBEC 325 mg (ASPIRIN)
ALBUTEROL-IPRATROPIUM 2.5-0.5 MG/3ML SOLN 3 mL (DUONEB)
Insulin (Aspart) Correction Table INJ (Novolog)
Bisacodyl SUPP 10 mg (DULCOLAX)
Milk of Magnesia SUSP 30 mL (MOM)
ProCHLORperazine SOLN 10 mg
Nitroglycerin SUBL 0.4 mg (NITROSTAT)
Glucose CHEW 16 g
Dextrose Gel GEL 15 g (GLUCOSE GEL)
Dextrose SOLN 12.5-25 g (DEXTROSE)
Glucagon SOLR 1 mg (GLUCAGEN)
If Blood Glucose is <70mg/d (less than 60mg/d in the pregnant patient): 1. Give 15g of simple sugars: 4 Glucose Tablets (if unable to chew, give 4 oz of juice) 2 Recheck Blood Glucose in 15 minutes 3 Repeat 15g of Simple Sugars if glucose is not above 70mg/dl 4 Recheck Blood Glucose 5 Repeat 15g of Simple Sugars if glucose is not above 70mg/dl and notify physicianImagine: these four orders for every patient admitted to the hospital with diabetes.
If patients' blood Glucose is <70mg/d (less than 60mg/d in the pregnant patient) and is conscious but NPO: - Dextrose 50% Half Amp IV - Recheck Blood Glucose in 15 minutes - Repeat Dextrose 50% if blood glucose is not >70mg/dl
If patient's Blood Glucose is <70mg/d (less than 60mg/d in the pregnant patient) and is unconscious: -1. Dextrose 50% 1 Amp IV and notify physician.- -2. If unable to administer D50 wihtin 5 minutes, give glucagon 1 mg IM and contact physicican. Monitor for nausea and vomiting.- - Recheck Blood Glucose in 15 minutes - Notify Physician, if blood glucose is not >70mg/dl
Does this save lives? Or does this cost patients for four different medications perhaps never needed? What is the cost of such automaticity when orders appear to manage patients without physician involvement? (That "little" order for glucagon, costs $104.82 retail at CostCo pharmacy. How much is it marked up for the hospital?)
Also, how many errors occur on the basis of misinterpretations of these automatic orders ("Oops, I forgot to ask if she was pregnant.")? Where are the evidence-based studies demonstrating the utility of this automated approach to patient care? Could this be why EMR's have not been found to save money to our health care system? Are we losing cost savings to our system by removing physician judgement?
In this era of cost overruns and exhorbitant Medicare expenditures, should we not be asking these tough questions?
No. That would be too difficult. Rather, it's far easier to cover your butt with automatically-generated orders that the patient has to pay for in the interest of assuring their own "safety."
-Wes
Saturday, June 07, 2008
Gone Golfing
Friday, June 06, 2008
Where I Draw the Line
 Okay, I'm alright with measuring blood pressures, and pulses, and counselling people to stop smoking and discussing family hisories of heart disease and a million other things....
Okay, I'm alright with measuring blood pressures, and pulses, and counselling people to stop smoking and discussing family hisories of heart disease and a million other things....... but toenail clippings?
Come on now! I have to draw the line somewhere...
-Wes
English As A Second Language
An interesting issue came up today as I sat before our Investigational Review Board (IRB) on behalf of a colleague who was trying to get a multi-center, prospective, randomized NIH-sponsored trial approved. The trial uses a medical device in one arm (the subject of randomization). The issue at hand involved the insistence (by trial design) that the patient participants should be fluent in English.
Immediately, the reviewers of the protocol were concerned that excluding patients based on their language of origin might suggest enrollees were discriminated upon based on their ability to speak English. This was, after all, an NIH-sponsored trial. It is true that, historically, women and minorities have been underrepresented in national trial designs – the desire to adequately represent these groups seems appropriate. But I found it difficult not to require enrollees to be fluent in English for such a complicated trial involving over 2 years of follow-up – it is, after all, our national language. More importantly, I argued, the very reason we were sitting before the IRB was because the investigation was felt to pose “less than minimal risk” for our patients. If a problem arose during the course of the trial, and a non-English-speaking patient calls our center, would they be able to communicate their concerns? More importantly, would we have the capabilities to communicate with them? Would this potentially increase the risk to the patient if communication were compromised? In to how many languages should our consents be translated? Spanish? Hindi? Urdu? Mandarin? Russian? Polish? The list seems endless.
Are we discriminating against a sect of the population that is non-English-speaking by not offering them these trials or just playing it safe by excluding those not fluent in our language?
The answer seems obvious to me, but then, I speak English. Any one else have thoughts on this? Suggestions?
Immediately, the reviewers of the protocol were concerned that excluding patients based on their language of origin might suggest enrollees were discriminated upon based on their ability to speak English. This was, after all, an NIH-sponsored trial. It is true that, historically, women and minorities have been underrepresented in national trial designs – the desire to adequately represent these groups seems appropriate. But I found it difficult not to require enrollees to be fluent in English for such a complicated trial involving over 2 years of follow-up – it is, after all, our national language. More importantly, I argued, the very reason we were sitting before the IRB was because the investigation was felt to pose “less than minimal risk” for our patients. If a problem arose during the course of the trial, and a non-English-speaking patient calls our center, would they be able to communicate their concerns? More importantly, would we have the capabilities to communicate with them? Would this potentially increase the risk to the patient if communication were compromised? In to how many languages should our consents be translated? Spanish? Hindi? Urdu? Mandarin? Russian? Polish? The list seems endless.
Are we discriminating against a sect of the population that is non-English-speaking by not offering them these trials or just playing it safe by excluding those not fluent in our language?
The answer seems obvious to me, but then, I speak English. Any one else have thoughts on this? Suggestions?
Wednesday, June 04, 2008
When Airlines Affect Clinic Schedules
It can be tough on your Monday clinic patients:
-Wes
A Perth cardiologist has lashed out at national airline Qantas, saying regular flight delays were potentially putting country patients at risk.Talk about office overhead. I wonder how he covers the expense of airfare?
Western Cardiology consultant Johan Janssen has flown to Kalgoorlie every Monday for the past five years. This year, only about four of 20 flights have been on time, with some experiencing delays of up to four hours.
Dr Janssen said even one-hour delays on May 19 and 26, both due to mechanical problems, could have had a devastating effect on his patients.
“I’m so busy I’m booked three months in advance, so if I’m an hour late between five and 10 patients can’t see me,” Dr Janssen said.
“Some are really upset because they don’t feel well and if they’re elderly they can’t travel to Perth,” he said.
-Wes
Tuesday, June 03, 2008
Chicago: A Case Study in Healthcare Market Consolidation
It was quite a morning for Evanston Northwestern Healthcare physicians as we heard from Mark Neaman, our President and CEO, about the rapidly-evolving healthcare market in Chicago. In his presentation, he chronicled the series of events that have lead to the changes seen so far in Chicago, and opened a glimpse of what’s to come.
Most of the news was old news:
Much of this healthcare system consolidation has been enabled by the emergence of the Electronic Medical Record that permits geographically disparate “virtual offices” to exist within a single healthcare system: it’s no longer which hospital or clinic you receive your healthcare from, but rather which “system.” The Mayo Clinic, with its satellite centers in Scottsdale, Arizona and Jacksonville, FL, has known this for years.
This has lead Evanston Northwestern Healthcare (ENH) to rethink their name and academic affiliation, since their tenuously amicable academic affiliation with Northwestern University has become seemingly irrevocably strained, limiting ENH’s ability to differentiate itself from its staunchest competitors (especially since its name contains "Northwestern"). For many reasons, it seems, the earlier 1994 academic affiliation agreement between Northwestern’s Feinberg School of Medicine is not likely to last much longer. While there were initial reports of an academic affiliation with Rosalind Franklin medical school, it was revealed today that ENH has recently entered into a 60-day agreement to evaluate a possible academic affiliation with the University of Chicago. This would be a represent a more formidable competitor to stem Northwestern's north suburban expansion.
Yes folks, our purple logo may soon change to maroon and the ENH 'brand' will likely cease to exist in the not-so-distant future.
All's fair in love and war when it comes to hospital systems, it seems.
It is important to note that these discussions are still ongoing, but public enough for them to have been announced to a significant portion of the ENH physicians today. Therefore, I suspect they are serious. Many questions remain unanswered. What this means to academic affiliations for ENH’s “affiliate” physicians, physician academic benefits, and the like, are uncertain. Clearly, ENH has a vested interest in maintaining its hard-earned physician affiliations and will be working to resolve these issues once the air clears a bit about our future.
While change is difficult, it seems necessary if ENH is going to continue its own growth strategy while the market forces evolve in Chicagoland. One thing is certain, though, the competitive climate between centers is more feverish than ever and change, it seems, is inevitable.
Perhaps on a broader note, other cities across America are likely to see the same forces toward consolidation, especially as the electronic medical record facilitates geographic spread of hospital system brand identity. It is clear that many doctors will increasingly become reliant on large healthcare systems to weather the economic impact of the threatened 10.1% Medicare physician pay cut in July, the ongoing unrealistic bureaucratic requirements for pay for performance measure documentation, the ongoing lack of tort reform, and increased work requirements by staff physicians to offset the upcoming resident work hour reductions from 80 to 56 hours per week.
-Wes
Most of the news was old news:
- He reviewed the financial struggles of Condell Medical Center in Libertyville from “contractual discounts” resulting in its suit with Blue Cross and subsequent countersuit of Blue Cross against Condell with the eventual withdrawal of Blue Cross patients from the Condell system. Condell bled so much red ink they were soon seeking a buyer as the economic impact of the situation became clear. (ENH looked at the opportunity, but Advocate was favored by Condell as their suitor),
- The financial struggles and huge debt load of Rush North Shore, coupled with Rush Medical Center (downtown)’s desire to make a $1 billion dollar mega-expansion and ENH’s need for local geography, prompting ENH to bid for Rush North Shore, and
- the newer alliance between Northwestern Memorial Hospital and its Northwestern Medical Faculty Foundation, making it a formidable competitor to the our financially separate ENH system as they also compete for market share in the desirable Northern and Western suburbs of Chicago – especially since they just bought 10 acres of prime real estate near I-294 and Willow roads, only 1 mile from ENH’s Glenbrook Hospital.
Much of this healthcare system consolidation has been enabled by the emergence of the Electronic Medical Record that permits geographically disparate “virtual offices” to exist within a single healthcare system: it’s no longer which hospital or clinic you receive your healthcare from, but rather which “system.” The Mayo Clinic, with its satellite centers in Scottsdale, Arizona and Jacksonville, FL, has known this for years.
This has lead Evanston Northwestern Healthcare (ENH) to rethink their name and academic affiliation, since their tenuously amicable academic affiliation with Northwestern University has become seemingly irrevocably strained, limiting ENH’s ability to differentiate itself from its staunchest competitors (especially since its name contains "Northwestern"). For many reasons, it seems, the earlier 1994 academic affiliation agreement between Northwestern’s Feinberg School of Medicine is not likely to last much longer. While there were initial reports of an academic affiliation with Rosalind Franklin medical school, it was revealed today that ENH has recently entered into a 60-day agreement to evaluate a possible academic affiliation with the University of Chicago. This would be a represent a more formidable competitor to stem Northwestern's north suburban expansion.
Yes folks, our purple logo may soon change to maroon and the ENH 'brand' will likely cease to exist in the not-so-distant future.
All's fair in love and war when it comes to hospital systems, it seems.
It is important to note that these discussions are still ongoing, but public enough for them to have been announced to a significant portion of the ENH physicians today. Therefore, I suspect they are serious. Many questions remain unanswered. What this means to academic affiliations for ENH’s “affiliate” physicians, physician academic benefits, and the like, are uncertain. Clearly, ENH has a vested interest in maintaining its hard-earned physician affiliations and will be working to resolve these issues once the air clears a bit about our future.
While change is difficult, it seems necessary if ENH is going to continue its own growth strategy while the market forces evolve in Chicagoland. One thing is certain, though, the competitive climate between centers is more feverish than ever and change, it seems, is inevitable.
Perhaps on a broader note, other cities across America are likely to see the same forces toward consolidation, especially as the electronic medical record facilitates geographic spread of hospital system brand identity. It is clear that many doctors will increasingly become reliant on large healthcare systems to weather the economic impact of the threatened 10.1% Medicare physician pay cut in July, the ongoing unrealistic bureaucratic requirements for pay for performance measure documentation, the ongoing lack of tort reform, and increased work requirements by staff physicians to offset the upcoming resident work hour reductions from 80 to 56 hours per week.
-Wes
Grand Rounds: All Roads Lead to Happy
Happy Hospitalist hosts this week's best of the medical blog-o-sphere with all bloggers leading to Happy in six degrees of separation or less...
-Wes
-Wes
You'll Be Disabled No More

... with this flame-throwing wheelchair:
According to Lance Greathouse, "It was made for the disabled person looking for something a little different, why drive something that looks like a medical device when you can drive something lethal?"-Wes
h/t: Instapundit.
More photos.
Monday, June 02, 2008
The Microeconomics of Medical Practice
“Microeconomics is a branch of economics that studies how individuals, households and firms make decisions to allocate limited resources, typically in markets where goods or services are being bought and sold. Microeconomics examines how these decisions and behaviors affect the supply and demand for goods and services, which determines prices; and how prices, in turn, determine the supply and demand of goods and services.”
- Wikipedia
It’s been a nice weekend: gorgeous weather, enjoying “connect time” with the family, and attending a mammoth high school graduation with all of the family activities that that entails. Needless to say, I failed to sit before a keyboard this weekend and reveled in the lack of computer-screen fluorescence.
But earlier this month, the Mrs (or should it be 'Drs?') has been working to shore up the coffers before the personal economic onslaught of two simultaneous college tuitions takes hold. As such, she has slowly been growing her clinical psychology practice: office space, rent, business cards, website, phone, etc. For months she has been working outside The System on a fee-for-service basis: she bills patients directly for services rendered. Accounting is simple and unencumbered: she pays her expenses from the revenues generated, and if at the end of the month she discovers her bank account is positive, she stays open for business. If not, she shudders the practice. Call it “Shoebox Economics:” put all your bills in a shoebox, then pay them off each month and see what’s left over.
Then she decided to “expand” her practice and become a Medicare provider in hopes of securing a larger patient pool.
First, she was unsure how to apply for a Medicare provider number, so being the ever-resourceful person that she is, she hired a billing professional friend who understood the system to help her with the paperwork. “Problem solved,” she thought, and continued seeing patients peacefully. At least until the Medicare provider number arrived, which it did, Friday. Suddenly and graphically, she met The Beast and reached an epiphany:
“Group number? Why do I need a ‘group number?’ Where’s my individual provider number?”This morning, I saw the first flecks of dust beginning to accumulate on her Medicare provider number letter… It’ll be interesting to see where this goes.
“What do you mean I must bill electronically?”
“What do you mean I can’t just complete a simple form and be reimbursed for my professional services?”
“What do you mean I have to hire a ‘billing specialist’ to do my billing?”
“There’ll be no money left over to apply to tuition!”
* blink * (Light turns on above her head.)
-Wes
Subscribe to:
Comments (Atom)