The following is a case study intended for folks who look at defibrillator recordings. If you find it interesting, great. If you have no clue what is shown here, don't feel bad, just move on to another blog post. I just thought I'd put this up as an unknown for those interested in phenomena encountered in a busy device clinic.
It was a case seen in our clinic: a nice man in his 50's had received a single chamber ICD for recurrent ventricular tachycardia and ventricular fibrillation and called because he had received several shocks from this device. Interrogation of the device showed normal sensing, lead impedance and capture threshold. Interrogation of his device demonstrated multiple VT therapies and untreated events recorded by his device.An example of several of the recorded interval plots (Event 202 and 203) as well has one example of the electrograms (and therapies delivered) recorded during episode 202 are shown below. 56 similar events were recorded since his last device interrogation, all with a similar pattern:
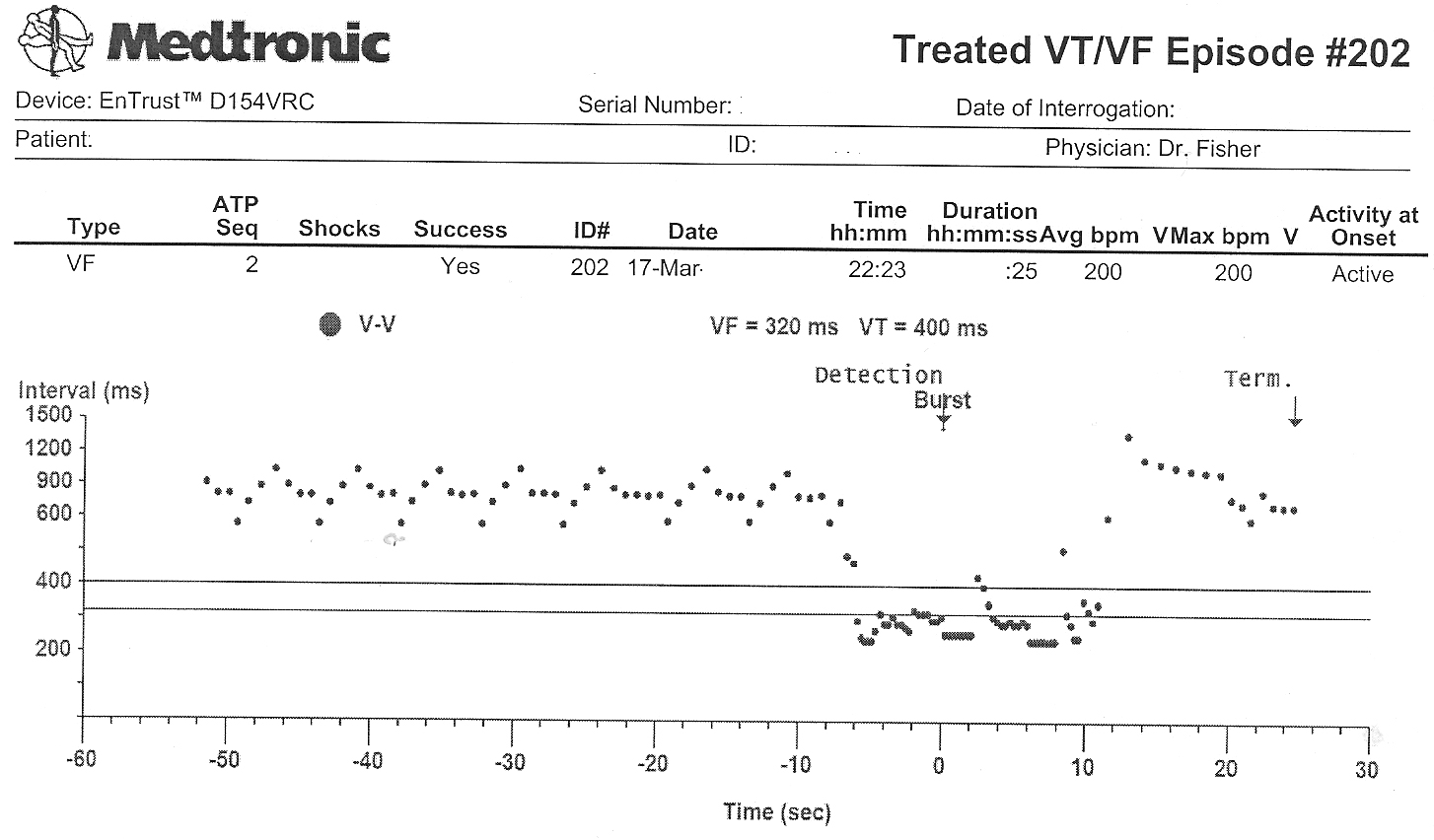 |
| Episode 202 RR Interval Plot (Click to enlarge) |
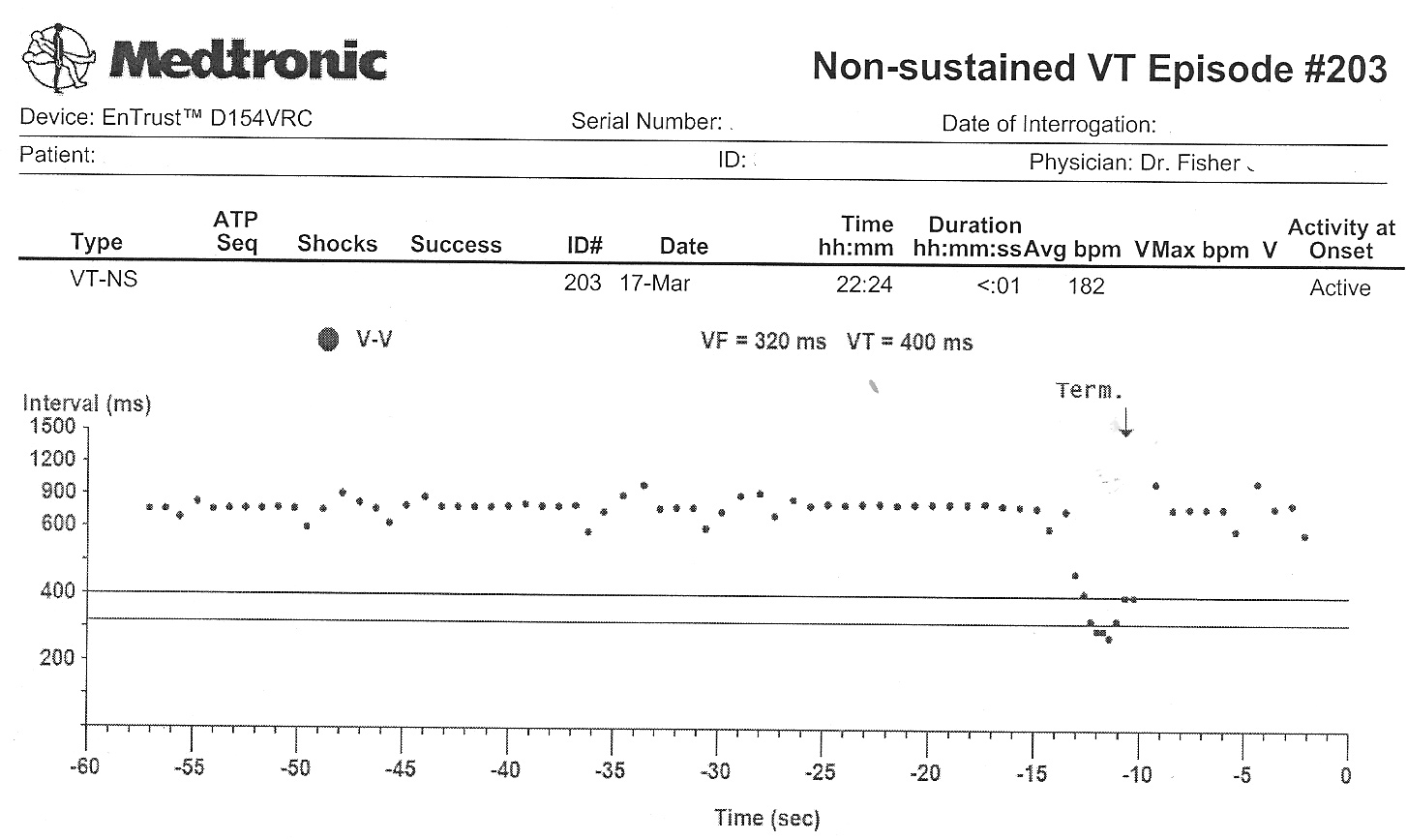 |
| Event 203 RR Interval Plot |
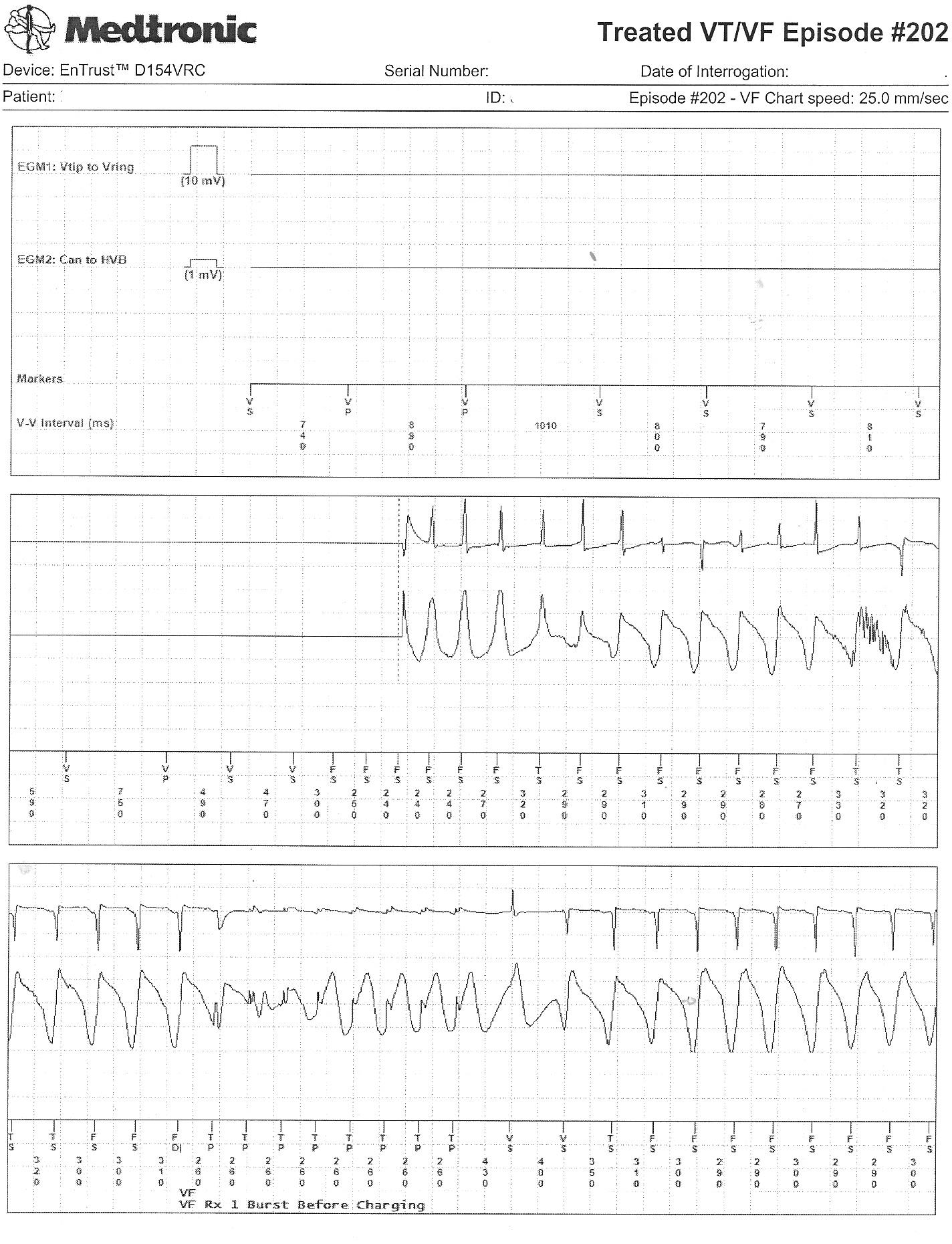 |
| Event 202's Recorded Electrograms and Intervals (Click image to enlarge) |
-Wes
5 comments:
I'm studying it Wes.
There is pacing at 740 msec then on the top strip it goes to 1000 msec
Perhaps the poly VT is somehow related to the rate changes and pacing.
Could we have some other clues, like whether he has some of the wonky proprietary algorithms turned on. Does he have a long QT, low Potassium.
Pacing proarrhythmia?
John -
As requested, a bit more information:
The patient's potassium was normal. His EKG showed a prolonged QT interval, but this was thought secondary to Amiodarone which had been started because of recurrent ICD shocks. Mexilentine was also added when Amiodarone failed to be effective at reducing the patient's shock frequency. His ejection fraction was checked by echo and found to be 52%.
Review of his device interrogation disclosed a wonky pacing algorithm buried deep in the programming was on.
Ideas?
-Wes
Wes,
I think...I hope...
This is MDT's version of rate smoothing. They call it rate stabilization.
These sorts of extraneous algorithms illustrate my thesis that less is more, even in electrophysiology/pacing.
I'm infamous around here for being a non-believer in 'extra' proprietary stuff on cardiac devices. "Turn that $%^& off."
Thanks for posting this. It's a humbling example of how we should all strive for minimally-disruptive electrophysiology.
JMM
John -
Good work. This is a rarely described example of ventricular proarrhythmia induced by Medtronic's ventricular rate stabilization algorithm.
A few notes about the case. Interval plots like those shown can be helpful to identify the possible mechanism of arrhythmia induction, especially if there is always a pattern of RR intervals that repeats and that preceeds arrhythmia onset. Of interest, an RR interval that was exactly 150 msec longer than a preceeding premature beat occassionally induced this patient's ventricular arrhythmia. His ventricular rate increment was programmed to 150 msec. Noted that after a PVC, the device gradually increases the RR interval 150 msec with each beat until sinus rhythm returns. But every single episode of arrhythmia induction recorded by the patient's device showed the first ventricular beat that was paced 150 longer than the preceeding RR interval induced his arrhythmia, confirming proarrhythmia from the pacing.
The challenge with this patient, however, was the fact that this algorithm was programmed on because spontaneous long-short intervals often induced ventricular fibrillation (eg, the intervals seen on patient's EGM strips that prompted this feature to be programmed on were 640, 469, 560, 1320, 570, 1270, 380 ->VF.
It was elected to increase the increment to 300 msec intially, and his VT/VF episodes resolved since pacing occurred later in the patient's vulnerable period. Only more recently have shocks returned, and I suspect it's because of the prolongation of his QT interval with continued Amiodarone. Stopping Amiodarone and adding of an atrial lead to avoid RV pacing altogether might be our next best option.
Hopefully, this case might help others identify this phenomena when managing similar complicated arrhythmia patients.
Interesting case. thanks for sharing.
Post a Comment