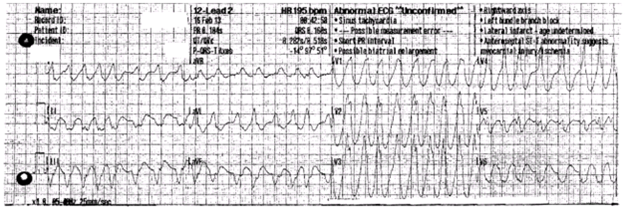
Several minutes later, the paramedics arrived and found that his pants were a bit wet (he never understood why he urinated on himself), but he was awake and coversant to the ambulance attendants. They connected him to a limited lead II tracing and weren't sure what they were seeing (the report said "SVT vs VT?"), so he was administered 6 mg adenosine in the field. The patient noted the paramedics looked concerned after administering the medication. An ECG strip was recorded, seen below:
 | ||
| Strip recorded after adenosine 6.0 mg administered - (click to enlarge). |
 | ||
| 12-lead EKG of his presenting rhythm - note similarity of lead II to rhythm strip and the "excellence" of the computer interpretation - (click to enlarge). |
He was urgently transferred to the closest Emergency Room. Interestingly, upon arriving there, he felt much better. Here's his initial EKG on presentation:
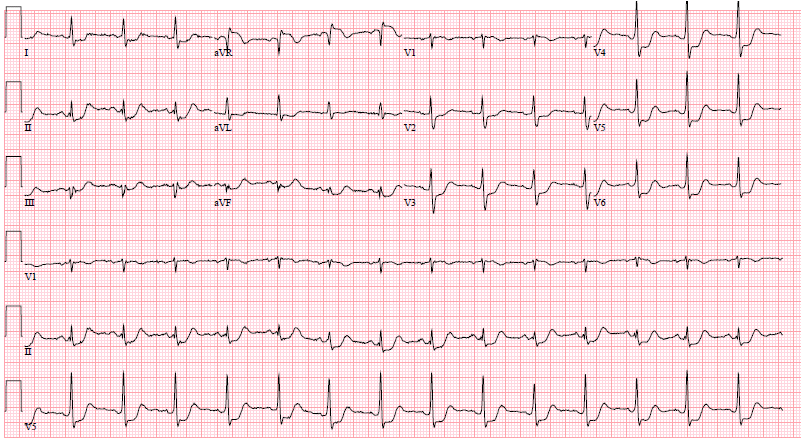 | ||
| 12-lead EKG of his presenting ER rhythm - (click to enlarge). |
-Wes
P.S.: Another EKG tracing from the following morning, in case you're wondering, can be found here.
4 comments:
Pre-excited AFib, adenosine was not ideal (to use an euphemism), they were lucky it didn't degenerate in VFIB. I'd proceed with AP ablation, it looks septal (antero- or mid-), so it can be tricky. A Na+ channel blocker could be an alternative, but he could have CAD given the post-cardioversion EKG (even though, I think my EKG would look the same after those sustained heart rates), so I would want to exclude that somehow. Amiodarone, especially during the loading phase, would be my last choice.
mcg -
Of the first two tracings shown, you are correct that these represent pre-excited atrial fibrillation. The story, however, was a bit more complicated.
It seems the patient may have been in a narrow complex SVT at the outset when the paramedics arrived (but unfortunately no tracing was recorded). The patient was administered adenosine 6 mg IVP and developed atrial fibrillation. Adenosine can induce atrial fibrillation by the shortening of atrial action potential duration while it is used for terminating atrioventricular re-entrant tachycardia. The resultant rhythm strip (lead II) and EKG were then recorded. The patient was then administered and Amiodarone (150 mg) bolus en route to the Emergency Room and converted to sinus rhythm just before arrival there.
The initial ER EKG showed normal sinus rhythm with diffuse ST segment depression suggestive of ischemia. These ST segment changes resolved completely by the following morning. No clear evidence of preexcitation is seen on any of the sinus rhythm EKGs.
The patient underwent an echocardiogram which showed normal LV function, but his intial troponins were elevated at 0.7. He underwent a left heart catheterization which documented normal coronary anatomy.
The patient underwent EP study the following day and had easily inducible orthodromic AVRT induced with either atrial or ventricular extrastimulus testing. Atrial fibrillation was not induced at the time of EP study intentionally. The patient had a very short AH interval (50 msec) and normal HV interval, but a single PVC demonstrated VA conduction via a left lateral accessory pathway. The patient underwent transseptal catheterization and successful ablation of a single left anterolateral accessory pathway with a single 30-second application of radiofrequency energy. No further SVT could be induced and complete retrograde dissociation via the AV node was documented post-ablation.
In summary, then, the patient experienced pre-excited atrial fibrillation via a "concealed" left anterolateral accessory pathway after administration of adenosine in the field. Because of the patient's rapid AV nodal conduction properties and far left-lateral location of the accessory pathway, manifest pre-excitation was never clearly seen on any of the patient's sinus rhythm EKGs.
As Paul Harvey used to say: "Now you know the rest of the story."
There is something a little unusual about this case (apart from the obvious).
How does a preexcited AF through a left anterolateral AP result in a deeply negative lead III, or even positive aVL and lead I?
Do you think this is lead reversal (?LA, LL would make most sense).
Great case - although (at least to the eye of a pediatric cardiologist) there is clear absence of the physiologic q in V6 on both of the sinus rhythm ECGs, suspicious for latent preexcitation.
Post a Comment