Some people are gifted story tellers. Some people are gifted writers. And yes, some people are gifted doctors.
But rarely do you have the pleasure of reading someone who is all three.
Welcome to StoryTellERdoc.
-Wes
Thursday, April 29, 2010
Lunatics
Lunatics keep re-discovering digoxin:
But lunatics come in all varieties:
... there's a lunatic born every minute.
-Wes
William Withering ... moved in 1762 to Edinburgh, Scotland, to study medicine, and qualified MD in 1766 after submitting a thesis entitled ‘De Angina Gangraenosa’ (Malignant Putrid Sore Throat). Withering moved back to England in 1767, and established a private practice in Stafford, and also worked as a physician at the Stafford Infirmary. Unexpectedly, in 1775, he was invited to go to Birmingham to join the staff of the General Hospital there, where he was to work for the next seventeen years.
During his time at Birmingham Withering published his major work on the foxglove (Digitalis) - "An account of the Foxglove and some of its Medical Uses" (Withering 1785)...
... Withering was encouraged by his membership of the Lunar Society of Birmingham, which met once every month on the Monday nearest to the full moon (hence ‘Lunar’), so that the members would have the benefit of some light on their homeward journeys (in the days of highwaymen and footpads). Withering and his fellow members of the Lunar Society (the ‘lunatics’) epitomized the 18th century learned society in the English Enlightenment, which followed hard on the heels of developments in Scotland (Schofield 1985).
But lunatics come in all varieties:
One evening, in the early summer of 2008, a Colorado sheriff’s deputy named Jonathan Allen came home to find that his wife had made him a “special” dinner. Waiting on the table was his favorite spicy spaghetti dish and a big leafy bowl of salad.So if it's the Monday nearest the full moon remember to check your salad. After all, ...
As he told investigators later, the salad was surprisingly bitter. But his wife told him it was a “spring mix” and he assumed it contained another of those trendy herbs that people use to liven up their greens. At least, he thought that way until he ended up in the hospital suffering from severe stomach cramps and a wildly speeding heart.
After his stomach was pumped and the contents analyzed, that bitter herb turned out to be leaves from a familiar and beautiful ornamental shrub. Allen survived but he did not return to his home in the suburban Denver town of Golden. And just this week, 42-year-old Lisa Leigh Allen, pleaded guilty to felony assault on charges of drugging a victim with what The Denver Post, called a “lethal plant.” ... the plant in this case was the common foxglove which is, indeed, poisonous but also figures as a long time source of some important heart medications.
... there's a lunatic born every minute.
-Wes
Wednesday, April 28, 2010
Finally: Doctors Push Some Lawyers Around
Hard to believe, but true:
On a more serious note, do fund raising, guideline development, lobbying efforts and scientific meeting organization on behalf of our specialty really require that much space?
-Wes
Ogletree Deakins will vacate its current D.C. office at 2400 N St. NW.You've got to love this: our one chance to push around 450 lawyers!
The labor and employment law firm is on the market for a new space because the owner of its building, the American College of Cardiology Foundation, wants to expand into Ogletree’s space. The nonprofit bought the Class A, 177,380-square-foot building in 2005 for $67 million, according to D.C. tax assessment records.
On a more serious note, do fund raising, guideline development, lobbying efforts and scientific meeting organization on behalf of our specialty really require that much space?
-Wes
Tuesday, April 27, 2010
How Many Administrators Does It Take to Run A Hospital?
From KevinMD:
That number should be just about right.
-Wes
... for every one doctor there are 5 more are employed to do administrative tasks.If you want to find out how many administrators it takes to run a hospital, ask yourself how many work on the weekend.
And, frankly, it’s ridiculous. As Dr. Cutler says, “There is a lot of money spent doing things that in no other industry do we tolerate.”
That number should be just about right.
-Wes
Monday, April 26, 2010
Smooth as Silk: Bioabsorbable Electronics
From Technology Review has a roundup of emerging technologies of which this is one:
-Wes
h/t: Instapundit
Implanted electronics could provide a clearer picture of what's going on inside the body to help monitor chronic diseases or progress after surgery, but biocompatibility issues restrict their use. Many materials commonly used in electronics cause immune reactions when implanted. And in most cases today's implantable devices must be surgically replaced or removed at some point, so it's only worth using an implant for critical devices such as pacemakers. Silk, however, is biodegradable and soft; it carries light like optical glass; and while it can't be made into a transistor or an electrical wire, it can serve as a mechanical support for arrays of electrically active devices, allowing them to sit right on top of biological tissues without causing irritation. Depending on how it's processed, silk can be made to break down inside the body almost instantly or to persist for years. And it can be used to store delicate molecules like enzymes for a long time.You've got to love innovation in medicine.
-Wes
h/t: Instapundit
"The RATS Are In the House"
I'm not sure I've heard a term that describes the OIG's audit teams that performs inpatient chart reviews better. The name stems from the Office of Audit Service's software used to determine how many charts to review at each facility:
After all, the cat and "mouse" game of finding evil doctors fraudulently billing by forgetting to note if heart failure is acute or chronic and systolic or diastolic must continue.
-Wes
RAT-STATS is the primary statistical audit tool used by the Office of Audit Services. Developed by the Regional Advanced Techniques Staff (RATS) in San Francisco, it has been used by the Office of Inspector General since the early 1970s. With the arrival of microcomputers, there was opportunity to move the statistical software from the mainframe timeshare systems.And like rats, these chart review teams are replicating like crazy.
In September 1987, the first microcomputer version of RAT-STATS was developed to run on IBM compatible computers using Microsoft's Disk Operating System (MS-DOS).
After all, the cat and "mouse" game of finding evil doctors fraudulently billing by forgetting to note if heart failure is acute or chronic and systolic or diastolic must continue.
-Wes
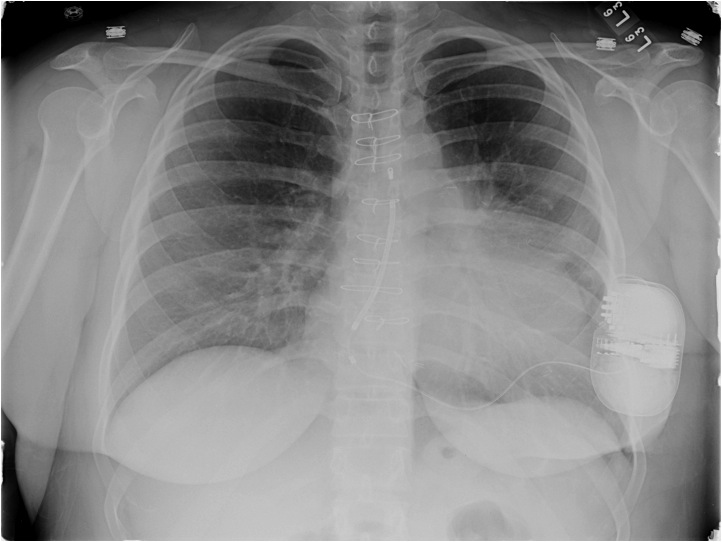
Numbers
Thirteen.
Unlucky?
Ejection fraction.
Three.
Coronaries.
Clean.
One hundred sixty-five.
Milliseconds.
QRS.
Thirty two.
Years.
Defibrillator.
Four hundred ninety.
Pounds.
* Sigh *
One hundred one.
Degrees.
Reprieve.
Thirty.
Days.
Afebrile.
Thirteen.
Thousand platelets.
Later.
Twenty-four.
Respiration.
Recumbent.
One hundred.
Thousand platelets.
Now?
-Wes
Unlucky?
Ejection fraction.
Three.
Coronaries.
Clean.
One hundred sixty-five.
Milliseconds.
QRS.
Thirty two.
Years.
Defibrillator.
Four hundred ninety.
Pounds.
* Sigh *
One hundred one.
Degrees.
Reprieve.
Thirty.
Days.
Afebrile.
Thirteen.
Thousand platelets.
Later.
Twenty-four.
Respiration.
Recumbent.
One hundred.
Thousand platelets.
Now?
-Wes
Sunday, April 25, 2010
The Health Hazards of 3D TV
I can't read for any length of time in a moving vehicle - it makes me nauseous.
This is because in order for the body to determine where it is at all times, the brain combines visual information, touch information, inner ear information, and internal expectations to judge its position in space. Under most circumstances, the senses and expectations agree. When they disagree, there is conflict, and motion sickness can occur. In my case with reading in a car, my eyes that are fixed on the written page tell my brain that I am still. However, as the car goes over bumps and accelerates or decelerates, my inner ear disagrees resulting in my brain activating the nausea center and causing motion sickness.
Well the same thing might happen with 3D TV.
Samsung Australia offers these warnings about the potential effects of 3D TV:
This is not to say there are not web sites out there with plenty of folks who have experienced motion sickness from 3D technology - there are. But we should not forget that there are many, many families outside of Australia who have children with epilepsy or a history of epilepsy and this technology is being actively marketed to children. Granted, photosensitive epilepsy is relatively rare, affecting less than 5% of all people with epilepsy, but as the market reach of this technology expands, manufacturers should make these health issues of their technology known to the public, irrespective of the country in which they reside.
-Wes
This is because in order for the body to determine where it is at all times, the brain combines visual information, touch information, inner ear information, and internal expectations to judge its position in space. Under most circumstances, the senses and expectations agree. When they disagree, there is conflict, and motion sickness can occur. In my case with reading in a car, my eyes that are fixed on the written page tell my brain that I am still. However, as the car goes over bumps and accelerates or decelerates, my inner ear disagrees resulting in my brain activating the nausea center and causing motion sickness.
Well the same thing might happen with 3D TV.
Samsung Australia offers these warnings about the potential effects of 3D TV:
I suppose I should not be surprised, since these issues with 3D TV are very reminiscent of problems experienced with virtual reality display units in the 1980's. But as a recent Samsung TV customer and guy with my particular vestibular predilection, I was surprised to find that these health concerns are not published on Samsung's US website.
- Some viewers may experience an epileptic seizure or stroke when exposed to certain flashing images or lights contained in certain television pictures or video games. If you or any of your family has a history of epilepsy or stroke, please consult with a medical specialist before using the 3D function.
- If you experience any of the following symptoms, immediately stop watching 3D pictures and consult a medical specialist: (1) altered vision; (2) lightheadedness; (3) dizziness; (4) involuntary movements such as eye or muscle twitching; (5) confusion; (6) nausea; (7) loss of awareness; (8) convulsions; (9) cramps; and/or (10) disorientation. Parents should monitor and ask their children about the above symptoms as children and teenagers may be more likely to experience these symptoms than adults.
- Viewing in 3D mode may also cause motion sickness, perceptual after effects, disorientation, eye strain, and decreased postural stability. It is recommended that users take frequent breaks to lessen the likelihood of these effects. If you have any of the above symptoms, immediately discontinue use of this device and do not resume until the symptoms have subsided.
- We do not recommend watching 3D if you are in bad physical condition, need sleep or have been drinking alcohol.
- Watching TV while sitting too close to the screen for an extended period of time may damage your eyesight. The ideal viewing distance should be at least three times the height of the TV screen. It is recommended that the viewer's eyes are level with the screen.
- Watching TV while wearing 3D Active Glasses for an extended period of time may cause headaches or fatigue. If you experience a headache, fatigue or dizziness, stop watching TV and rest.
- Do not use the 3D Active Glasses for any purpose other than viewing 3D television. Wearing the 3D Active Glasses for any other purpose (as general spectacles, sunglasses, protective goggles, etc.) may physically harm you or weaken your eyesight.
- Viewing in 3D mode may cause disorientation for some viewers. DO NOT place your television near open stairwells, cables, balconies or other objects that may cause you to injure yourself.
This is not to say there are not web sites out there with plenty of folks who have experienced motion sickness from 3D technology - there are. But we should not forget that there are many, many families outside of Australia who have children with epilepsy or a history of epilepsy and this technology is being actively marketed to children. Granted, photosensitive epilepsy is relatively rare, affecting less than 5% of all people with epilepsy, but as the market reach of this technology expands, manufacturers should make these health issues of their technology known to the public, irrespective of the country in which they reside.
-Wes
Saturday, April 24, 2010
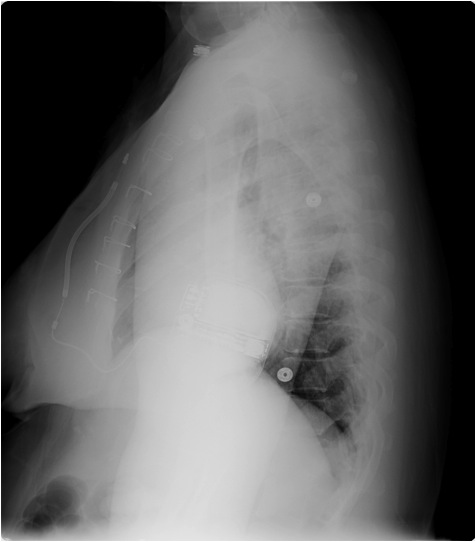
Heart Curves
One very unique, nerdy, and thoughtful tattoo made from a heart-shaped equation.
-Wes
h/t: Dr. Ramona Bates via Twitter.
The Breaking of the Doctor-Patient Relationship
An incredibly important read over at Dr. Rich's place:
-Wes
Until very recently doctors, patients, philosophers and ethicists recognized that, when you are sick, you are no more capable of navigating a complex and hostile healthcare system than are accused felons a complex and hostile legal system, and you are no less in peril if you run afoul of that system. And, just as the felon has a right to a personal advocate, a professional whose job is to protect his individual interests against the conflicting aims of the “system,” so does the patient. That is (quaint conventional wisdom held), when you are sick, you should be entitled to at least the same protections as when you rob a convenience store. And the doctor-patient relationship was supposed to guarantee you that right.Read the whole thing.
This is why, throughout the ages, the basic precepts of medical ethics were aimed at guaranteeing the sanctity of the doctor-patient relationship. Fundamentally, these ethical precepts required the physician to place the needs of his or her individual patient above all other considerations.
It should be clear to everyone that, under either our “old” healthcare system or the one that Obamacare promises us, this formulation of the doctor-patient relationship cannot be allowed to stand. Neither the insurance executives nor government officials can allow spending decisions - that is, decisions on how to spend their money - to be made by individual patients (and their personal advocates). For this reason, the classic doctor-patient relationship had to go.
-Wes
The Costs of a Heart Attack
Quite a bit, according to some:
-Wes
Reference: The WISE Study:
Shaw LJ, Merz CNB, Pepine CJ, et al. The Economic Burden of Angina in Women With Suspected Ischemic Heart Disease: Results From the National Institutes of Health-National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation. Circulation. August 29, 2006 2006;114(9):894-904.
According to an article from the National Business Group on Health, the average total (editor's note: lifetime) cost of a severe heart attack–including direct and indirect costs–is about $1 million. Direct (lifetime) costs include charges for hospitals, doctors and prescription drugs, while the indirect costs include lost productivity and time away from work. The average (lifetime) cost of a less severe heart attack is about $760,000. Amortized over 20 years, that’s $50,000 per year for a severe heart attack and $38,000 per year for a less severe heart attack.I'm all for maintaining a healthy lifestyle, but before we get all hot and bothered about performing more testing to "prevent" a heart attack as a means to save health care costs going forward, remember the lessons we learned from the Tim Russert fallout.
-Wes
Reference: The WISE Study:
Shaw LJ, Merz CNB, Pepine CJ, et al. The Economic Burden of Angina in Women With Suspected Ischemic Heart Disease: Results From the National Institutes of Health-National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation. Circulation. August 29, 2006 2006;114(9):894-904.
Could a Heart Attack During A Trial Help a Defendent in Court?
Perhaps:
Assistant U.S. Attorney Christopher Graveline wrote in a motion that after the judge told the jury about the heart attack “many jurors in their body language and facial expressions, rightly expressed concern for Mr. Cicchetti.” The prosecutor said the government did not object to the judge telling the jury about the heart attack because it assumed that Cicchetti would be prosecuted later before a different jury.-Wes
“It is only natural for the jury to feel sympathy for Mr. Cicchetti’s condition and this sympathy may well play into its consideration of the evidence against Mr. Cicchetti especially in light of his defense that he is a sick harmless older man who is only guilty of loving motorcycles and cocaine.”
“The government believes that allowing Mr. Cicchetti to continue in absentia would prejudice its ability to have a fair hearing and that there would be a high probability that an extrinsic factor, i.e. the defendant’s health, could affect the jury’s decision rather than the evidence presented in court.”
One Man's Mission
Mr. Ron Murray, a tranplant heart recipient, tells his story:
From the video:
-Wes
From the video:
"… if the transplant issue ever comes up for anyone listening, that’s almost the first thing they would think, too. If I had time to think about it over that year, I would have realized, oh my God, I would have apprehension all built up about how I would react to...I mean is it going to change my way of thinking? Is it going to alter my own thoughts? None of that holds up, ultimately.Remarkable guy. May his message reach millions.
When I realized that there was going to be, forever, an emotional component, and maybe a spiritual component to this thing that I hadn’t thought about, is when I became – God, I don’t even know if I can tell you about it – that I began to grieve for the donor, that brought be to tears several of those nights.
But they weren’t bad tears, they were were just, like tears you feel when you go to a funeral – someone you know – and I didn’t know Kevin but I did now, is the way I looked at it. And so, the rest of my time in the hospital was an alternating time between listening to music in my head and writing it and making it up, and thinking about Kevin and his family and what all of this really means to my future life.
So, I formulated a plan to try to reach a lot of people for the specific reason that I passed up so many deserving people on the Austin transplant waiting list. There were 12 people ahead of me who had been waiting for a heart, sometimes up to a year, and I had only been on the list three weeks and here I am jumping ahead to get the heart. (By the way, he saved four or five people that night – he was a donor of everything).
So I figured the reason that I jumped ahead of so many people was because there was such a severe shortage of donors, and ultimately that proved to be true. So anyway, my effort now is to reach as many people as possible, and this is part of that effort…”
-Wes
Thursday, April 22, 2010
Bad Looks, Good Concept: A Bluetooth Heart Rate Monitor for the iPhone
Someone has to talk to this company about ergonomic engineering:
-Wes
What looks like a bulky female hygiene product is actually a health monitor that hooks up to an iPhone via Bluetooth, sending bodily information such as heart rates to the compatible app.To their engineers: Any color but white or light blue, okay?
It's not on sale yet, with Proteus' Raisin sensor only just being passed through the FDA, but it's another step for the iPhone into the operating room, after Apple showed off the Lifescan app by Johnson & Johnson at last year's WWDC, which works alongside a wireless glucose meter. Diabetes can analyze the glucose levels in their blood, with the information being sent to the iPhone app over Bluetooth.
-Wes
What a Welfare State Looks Like
Only in Illinois: where teachers and union members rallied to raise more taxes yesterday.
And this is before the tax bill for health care comes due.
But there is a better option for our beleaguered state and it was offered by a member of the Democratic House in Illinois, Jack D. Franks.
We need to pressure our Illinois legislative leaders to support his legislation.
-Wes
Addendum: Thanks to Glenn Reynolds for the Instalanche.
And this is before the tax bill for health care comes due.
But there is a better option for our beleaguered state and it was offered by a member of the Democratic House in Illinois, Jack D. Franks.
We need to pressure our Illinois legislative leaders to support his legislation.
-Wes
Addendum: Thanks to Glenn Reynolds for the Instalanche.
Wednesday, April 21, 2010
Will iPhone Apps Have to be FDA-Approved as Medical Devices?
... if you're a radiologist, it seems some do:
-Wes
Now, the next blockbuster: the FDA-approval iPhone app!
“We did a stroke trial ... and compared performance of radiologists reading on the iPhone to the standard clinical reading work station and the performance was identical,” said Mitchell. “They performed just as well in this tough diagnostic task.
“That’s a really good indicator that this could be quite useful for diagnosing all sorts of things that aren’t as tough,” he added.
Mitchell said it’s currently being tested on the new iPad, which has a larger screen to view the images.
The application for iPhone and other mobile devices has been licensed as a medical device in Canada, said Philippe Laroche, a spokesman for Health Canada.
It’s still awaiting approval from the US Food and Drug Administration and CE Mark in Europe.
-Wes
Tuesday, April 20, 2010
When Doctors Decide Damages
In an interesting twist to the ongoing saga of device recalls, the Minneapolis Startribune reported that the two doctors, Robert Hauser, MD and Barry Maron, MD who first brought the Prism II ICD device malfunction to public attention by releasing their story to the New York Times in 2005, wrote a letter to the judge reviewing the plea bargain agreement and told him:
While these doctors have every right to express their opinions on the case (and certainly the actions of the company were egregious), their letter opens an interesting precedent for physicians advocating on behalf of their patients: deciding what is "just" concerning damage awards in legal matters on their behalf.
Should this be the purview of physicians?
I wonder.
What I do know is an incredible amount of good has come to the medical device industry since this story broke. Companies do a much better job of reporting problems with their devices now as evidenced by excellent product performance reports. Companies also raise flags regarding their devices MUCH earlier, perhaps even notifying patients of every advisory condition imaginable (like cosmic radiation could interact with their device memory chips) - suddenly nothing was too small to report. We have also seen the profession have a greater understanding of the need to quantify the incidence of device problems by returning all devices - normally functioning or not - to companies for ongoing quantification of device reliability to better appreciate the level of device performance we should accept as "standard." Device registries now are used routinely to track and better understand the myriad of variables that influence device performance in the real world.
Litigation is always expensive and time-consuming. I am left to wonder if ongoing court litigation versus a hefty out-of-court settlement will really provide additional benefit to to the loved ones who lost their children or, as these doctors suggest in their letter, future patients. I worry that ongoing litigation might just drag this process on for years so that future patients will have to bear the costs in the form of even higher device prices.
I admit that I do not know how much money the plaintiffs would receive with the anticipated settlement and whether that will be enough compensation for all that has happened, but irrespective of the judge's decision in this matter, I hope we can continue to move past this unfortunate incident and continue working with industry and regulators to make sure this never happens again.
-Wes
We are physicians who cared for Joshua Okrup (eds note: should be "Oukrop"), a 21 year-old college student, who died when his Guidant Prizm 2 implantable cardioverter-defibrillator (ICD) short-circuited and failed to deliver a life-saving shock. His unnecessary death was caused by a product defect that Guidant Inc. had known about for years and failed to inform patients, physicians, and the U.S. Food and Drug Administration. Accordingly, we are extremely dismayed by the U.S. Attorney General’s decision to enter into a plea agreement with Guidant LLC, rather than prosecute the company and the individuals responsible for this egregious act. On behalf of the patients who died or suffered pain and mental anguish as the direct result of Guidant’s illegal and unethical behavior, we urge you not to accept the plea agreement.An out-of-court $296 million plea agreement is not enough it seems.
While these doctors have every right to express their opinions on the case (and certainly the actions of the company were egregious), their letter opens an interesting precedent for physicians advocating on behalf of their patients: deciding what is "just" concerning damage awards in legal matters on their behalf.
Should this be the purview of physicians?
I wonder.
What I do know is an incredible amount of good has come to the medical device industry since this story broke. Companies do a much better job of reporting problems with their devices now as evidenced by excellent product performance reports. Companies also raise flags regarding their devices MUCH earlier, perhaps even notifying patients of every advisory condition imaginable (like cosmic radiation could interact with their device memory chips) - suddenly nothing was too small to report. We have also seen the profession have a greater understanding of the need to quantify the incidence of device problems by returning all devices - normally functioning or not - to companies for ongoing quantification of device reliability to better appreciate the level of device performance we should accept as "standard." Device registries now are used routinely to track and better understand the myriad of variables that influence device performance in the real world.
Litigation is always expensive and time-consuming. I am left to wonder if ongoing court litigation versus a hefty out-of-court settlement will really provide additional benefit to to the loved ones who lost their children or, as these doctors suggest in their letter, future patients. I worry that ongoing litigation might just drag this process on for years so that future patients will have to bear the costs in the form of even higher device prices.
I admit that I do not know how much money the plaintiffs would receive with the anticipated settlement and whether that will be enough compensation for all that has happened, but irrespective of the judge's decision in this matter, I hope we can continue to move past this unfortunate incident and continue working with industry and regulators to make sure this never happens again.
-Wes
Monday, April 19, 2010
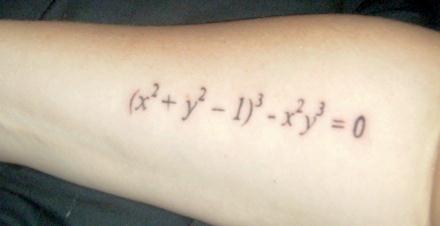
Art From the Heart
2010 Cardiology Calendars
Marketing efforts abound in health care and cardiology in particular, but promoting your office staff on a 2010 calendar?
I guess if it sells sports magazines, it might just work for some private cardiologists.
-Wes
Click to enlarge (if you must)
I guess if it sells sports magazines, it might just work for some private cardiologists.
-Wes
Proof That Cutting Costs Might Affect Quality of Care
... when the new, cheaper answering service answers the phone after hours:
(At least it was worth a chuckle.)
-Wes
"Cardiac Electro-psychology. How may I help you?"Sad, but true.
(At least it was worth a chuckle.)
-Wes
The Loss of Physician-Owned Hospitals Solves Nothing
With the new health care reform bill signed in to law, the fate of physician-owned hospitals was sealed:
So with the downturn in heart attacks that we are now seeing thanks to public health initiatives like anti-smoking campaigns, how is Sanford going to fund their shiny new facility?
Why prevention, of course!
But then, our Congressmen understood all this, right?
-Wes
The bill Congress passed in March includes a ban on new physician-owned hospitals and freezes those already in business at their present size. Doctors hold a one-third interest in Avera Heart, which opened in 2001, so the bill President Obama signed would prevent that facility from ever growing.While it is easy to point to the potential conflict of interest inherent to physician-owned medical facilities, it is not so easy to demonstrate that non-physician-owned hospitals don't have similar conflicts with generating profits. After all, continuing to build large $78 million-dollar expansions requires hospitals of any kind to achieve a return on their investment in order to continue operations.
The law change, in effect, leaves expansion of treatment of cardiovascular disease open for Sanford to dominate locally in coming years - if in fact that field of medicine grows. Avera Heart says such growth is not a given, because people are living healthier and have less need for emergency care.
So with the downturn in heart attacks that we are now seeing thanks to public health initiatives like anti-smoking campaigns, how is Sanford going to fund their shiny new facility?
Why prevention, of course!
O'Brien acknowledges the down trend in heart attacks but said other needs are increasing. Sanford performed 20,000 heart screenings the past two years, and about 1,000 led to follow-up such as a stent procedure to clear a passageway for blood flow. In the past, many such problems would show up later as a heart attack.On the surface, prevention sounds sexy as a cure-all for our current health care cost conundrum. What's not to like with preventing disease before it happens? But to think the hospital administrators have patients best interests at heart by using prevention as their excuse to "screen" for more heart disease, we should ask ourselves if the non-physician hospitals are any more altruistic than partially physician-owned facilities:
"We see fewer heart attacks than we did in previous years, but more can be done without resorting to surgery," he said. "Across the country surgery numbers are down, and angioplasty and stent numbers are up." (Editor's note: So much for having the COURAGE to say "no," eh? Let's not forget the conflicts inherent to physicians being employees of hospitals who increasingly tie physician compensation to their productivity)
"You don't build cath labs and surgical suites if you're going to do preventive medicine."Amen.
But then, our Congressmen understood all this, right?
-Wes
Sunday, April 18, 2010
When All the Cardiologists Merge with a Single Hospital
Is competition or consolidation is the best way to deliver care and contain costs in the post-reform business of health care?
In Maine, the state Legislature has maintained that competition should prevail:
Somehow, I don't think the Maine legislature really believes their theory that competition is the best way to control costs in health care. Rather, what this anti-trust argument really boils down to is the legislature does not want to lose two other hospitals (and the taxes and jobs they represent) to market consolidation.
-Wes
In Maine, the state Legislature has maintained that competition should prevail:
Under the plan, MaineHealth, owner of Maine Medical Center, would hire the 40 cardiologists now with Maine Cardiology Associates, which is based in South Portland, and Cardiovascular Consultants of Maine, based in Scarborough. The doctors would continue to see patients at their existing offices with the same medical and support staffs, although MaineHealth would buy the offices and equipment.While the theory of competition to control costs works in free markets, health care is anything but a free market. As proof of this, competition between hospitals has failed to lower costs in most other health care markets nationwide.
MaineHealth and the physician groups asked for a change in state law that would protect the deal from antitrust challenges if they can show it is in the public interest – for example, that it preserves access to high-quality heart care.
That effort failed in the closing days of the legislative session, however, and it’s unclear whether MaineHealth and the cardiologists will move ahead and risk legal challenges, or wait and try again when the Legislature reconvenes next winter.
“We’re assessing our different opportunities to move forward. We’re still fully committed to our integration,” said Mark Harris, spokesman for MaineHealth, a nonprofit that owns seven Maine hospitals and several other health care organizations. “It would be in our best interest and in the best interest of the state, as well.”
Mercy Hospital in Portland and Central Maine Medical Center in Lewiston have objected to the change in state law. Officials with those hospitals also say the merger would effectively give Maine Medical Center a monopoly in cardiac medicine that could harm competitors and patients.
Both the Federal Trade Commission and the Maine Attorney General’s Office have been monitoring the plan because competition – at least in theory – leads to better services and lower prices, and the deal could threaten that.
Somehow, I don't think the Maine legislature really believes their theory that competition is the best way to control costs in health care. Rather, what this anti-trust argument really boils down to is the legislature does not want to lose two other hospitals (and the taxes and jobs they represent) to market consolidation.
-Wes
Saturday, April 17, 2010
Heart Strings
Thanks to the wonders of magnetic resonance imaging (MRI), amazing images of the muscle fiber orientation of the left ventricle have been obtained:

-Wes

The image was produced using a branch of magnetic resonance imaging (MRI) called diffusion tensor imaging (DTI). The technique tracks the diffusion of water throughout the myocardium (the heart’s muscular wall comprising interconnected sheets of muscle cells called myocytes). Due to the way the myocytes are organized, the movement of water is restricted, so tracking the location of water molecules can reveal valuable information about the structure of the heart in a non-invasive way.Nice.
-Wes
Thursday, April 15, 2010
When States Tie Conditions of Licensure to Insurance Payments
A bill currently under review by the state Senate in Massachusetts will make participation in the state and federal Medicare/Medicaid programs a condition of medical licensure, effectively making physicians employees of the state:
Unbelievable.
My prediction: look for many doctors to move elsewhere.
-Wes
Every health care provider licensed in the commonwealth which provides covered services to a person covered under "Affordable Health Plans" must provide such service to any such person, as a condition of their licensure, and must accept payment at the lowest of the statutory reimbursement rate, an amount equal to the actuarial equivalent of the statutory reimbursement rate, or the applicable contract rate with the carrier for the carrier’s product offering with the lowest level benefit plan available to the general public within the Connector, other than the young adult plan, and may not balance bill such person for any amount in excess of the amount paid by the carrier pursuant to this section, other than applicable co-payments, co-insurance and deductibles.So what this means is that in order for doctors to become licensed in Massachusetts, they will have to agree to accepting the payment rates imposed by the government, even though those payments may not cover their actual expenses for the care rendered.
Unbelievable.
My prediction: look for many doctors to move elsewhere.
-Wes
Wednesday, April 14, 2010
The First Health Care Information Technology Help Desk
For anyone who has or will be implementing an Electronic Medical Record, here's the very first successful implementation of the information technology help desk:
Look familiar?
-Wes
Look familiar?
-Wes
Tuesday, April 13, 2010
Extramarital Affairs and the Heart
As I tweeted before from the recent ACC meeting, physical exertion during extramarital affairs is over twice as strenuous on the heart for men. But what happens to women if they have an extramarital affair?
Well, Mind Hacks points us to a case report of a woman who died while having an extramarital affair with her lover:
Oh, and if you think you still might be tempted to proceed despite these facts and are in the market for a new car, consider buying big for your own safety.
-Wes
References:
[1] Lee S, Chae J, Cho Y. Causes of sudden death related to sexual activity: results of a medicolegal postmortem study from 2001 to 2005. J Korean Med Sci 2006;21:995–9.
[2] Parzeller M, Raschka C, Bratzke C. Sudden cardiovascular death in correlation with sexual activity — results of a medicolegal postmortem study from 1972–1998. Eur Heart J 2001;22:610–1.
[3] Gips H, Zaitsev K, Hiss J. "Sudden cardiac death of a woman during extramarital sex: A case report and review of the literature." Journal of Forensic and Legal Medicine 2010; 17: 186–187.
Well, Mind Hacks points us to a case report of a woman who died while having an extramarital affair with her lover:
The presented case is unique in that the deceased was a femaleA review of the literature in the discussion section of the article sheds more light on the subject:
affected by chronic hypertensive cardiovascular disease, engaged in a long standing extramarital romantic relationship.
Case report
A 46-year old woman, married and mother of two, has been meeting with her 52-years old married lover twice a month for several years. These sexual encounters were conducted in the male partner’s class B car, typically lasting less than an hour. The last tryst took place on a hot summer afternoon, in a car exposed to direct sunlight. Reportedly, the male companion urged her to rush their activities as he was supposed to pick up his wife later on. During foreplay, the woman became dyspneic, and was unable to drink the water offered by her companion. He rushed her to a nearby medical center and immediately drove off. She was pronounced dead on arrival. Rectal temperature was not measured. The lover was later apprehended by local police and released after questioning.
Autopsy revealed an obese female (BMI = 32), with enlarged heart of 560 g, with thickening of the anterior left ventricular wall and interventricular septum, atherosclerotic narrowing of three major coronary vessels of up to 60–70% of the lumen, and severe pulmonary edema and congestion. Microscopic examination of the heart did not disclose acute myocardial infarction, but rather myocardial hypertrophy along with interstitial fibrosis. Severe fatty change of the liver and hepatomegaly (2360 g) were noted. Other organs, along with her brain, showed acute congestion. Toxicological screening revealed no alcohol, drugs or any other chemical substance in her body.
In a study conducted in Korea[1] on causes of sudden death related to sexual activity, out of the 14 reported fatalities, only five women were described, aged 43–50 years, three of which died from subarachnoid hemorrhage (SAH), while two suffered from complications of CAD, which falls within the gender differences in cause of death in the general population (CAD in men vs. SAH in women). Sudden death following sexual activity is mainly caused by re-infarction or acute myocardial infarction (AMI) in males, while in females most commonly by intracranial hemorrhage or cardiovascular disease.But the authors of the current case report wonder if the size of the car might have contributed to this outcome of this case:
These findings are supported by Parzeller et al.,[2] who report that the main cause of death following sexual activity in Germany was re-infarction or AMI (55%), followed by coronary artery disease (29%) or, less commonly, left ventricular hypertrophy (9%). Two instances of intracerebral hemorrhage and one myocarditis were listed in this study, all three of which in women between the ages of 43 and 49 years.
Although it was impossible to obtain sufficient information as to the deceased position in the car during their foreplay, the authors estimate that the relatively small size of the car required some physical effort for achieving any desirable position to reach sexual gratification.So ladies, although it happens rarely, consider yourself warned.
Oh, and if you think you still might be tempted to proceed despite these facts and are in the market for a new car, consider buying big for your own safety.
-Wes
References:
[1] Lee S, Chae J, Cho Y. Causes of sudden death related to sexual activity: results of a medicolegal postmortem study from 2001 to 2005. J Korean Med Sci 2006;21:995–9.
[2] Parzeller M, Raschka C, Bratzke C. Sudden cardiovascular death in correlation with sexual activity — results of a medicolegal postmortem study from 1972–1998. Eur Heart J 2001;22:610–1.
[3] Gips H, Zaitsev K, Hiss J. "Sudden cardiac death of a woman during extramarital sex: A case report and review of the literature." Journal of Forensic and Legal Medicine 2010; 17: 186–187.
It's Official: It's Not Okay to Die in a Hospital
Dear Mr or Ms. Patient,
We are writing to inform you that if you die in a hospital, your hospital will be blacklisted in the name of published "quality" data:
Thank you for your understanding.
-The Administration
We are writing to inform you that if you die in a hospital, your hospital will be blacklisted in the name of published "quality" data:
Patients die of common medical conditions more often at some of the area's best-known hospitals than at other institutions with less sterling reputations, according to a new state report published Monday.So please think twice about coming to a hospital for care when you're really sick, okay? Just be nice and die at home. That way, your local hospital will be able to save costs and look like it provides the finest of care.
Thank you for your understanding.
-The Administration
Electronically Tailoring Consents
What would you rather know when undergoing a surgical procedure, what are your most likely complications during the proposed surgery based on your own personal characteristics, or all of the potential complications that could arise with your upcoming surgical procedure?
Several major medical centers are betting you'd like to know your tailored personal risks:
After all, if you have a stroke during the procedure (no matter how low the pre-operative risk assessment was), your risk suddenly becomes 100%.
-Wes
Several major medical centers are betting you'd like to know your tailored personal risks:
Integris Heart Hospital doctors are testing a high-tech consent form for patients considering angioplasty. A computer program draws from a database of 600,000 patients around the country to better predict individual risks and benefits of the procedure.While it is impossible to know all of the risks that can occur during a surgical procedure, there may be some value prioritizing risks for a patient based on their renal or hepatic function, for instance. Still, I wonder if we risk sugar-coating invasive procedures (like a coronary angiogram) by suggesting to patients that their risk of stroke was virtually zero.
The new process replaces one-size-fits-all forms that were used primarily as a legal formality. The high-tech version uses simple language and illustrations to explain procedures, while mathematically predicting the risk of complications based on individual characteristics.
After all, if you have a stroke during the procedure (no matter how low the pre-operative risk assessment was), your risk suddenly becomes 100%.
-Wes
Monday, April 12, 2010
Running on Empty
"In sixty-nine I was twenty-one and I called the road my own
I don't know when that road turned onto the road I'm on.
Running on, running on empty
Running on, running blind
Running on, running into the sun
But I'm running behind."
-Jackson Browne
"We're stretched so thin, right now. No new hires in sight. Look at this list of patients: twenty-two of 'em, all over 70, eight "new's" among them, every one with tons of medical issues. Didn't get out of here until 10:30 last night. Then back at it at 8 (am) this morning. I'm telling you, I hate it. Hate it. There just doesn't ever seem to be an end in sight. We're just a bunch of "f**in' employees, and no one gives a damn."
I sat stunned. I knew him from before. His job had taken it's toll. This wasn't the guy I knew earlier. I really didn't know how to respond, but did suggest that maybe hospitalist medicine wasn't for him.
I had been there once. Like a fly buzzing against a pane of glass, persistently buzzing, buzzing, unable to escape, able to see the sun on the other side of the window, but no matter how hard I buzzed against that window, I could never make it outside. The forces against me were just too great. But it's right there! Can't you see it? If I just work a little harder. Hey, others can do this job, so I must just be doing something that I can fix. What can be so hard about this? Hell, I've got a medical degree! I'm smart enough to figure this out!
But only after the fly stopped buzzing against the window to noted that there was an open door right next to him, was he ever able to reach the great outdoors.
But woe to the fly that doesn't make the change...
... for if he keeps buzzing against the window, he'll die.
-Wes
Friday, April 09, 2010
Massachusett's: Foreshadowing Our Nation's Health Care System?
Paul Levy, President and CEO of Beth Israel Deaconess Medical Center in Boston, MA, today suggests we watch Massachusetts for what might be coming with health care reform:
*Sigh*
-Wes
Things are playing out just as one might predict in the Massachusetts small business and individual insurance market. The Insurance Commissioner turned down proposed rate increases, the state's insurers appealed to the courts, and now they can't write policies.Perhaps more concerning is what Dennis Byron, a commenter on Mr. Levy's blog says about insurance exchanges:
I care because I am one of those that has been cancelled by my insurer (Fallon) solely I believe because I am an individual, have been told to go to the exchange, but the exchange does not work. This is a perfect example of why you don't want the guys that run the Registry running your health care.If nothing else, this exposes the risks inherent to mandating unproven policy initiatives on a national scale that have yet to be even worked out in a single state.
*Sigh*
-Wes
Thursday, April 08, 2010
Using "Treatment Standardization" To Bar Cardiologists From Hospitals
Is the need for cookbook medicine is being used as a ploy to bar cardiologists from practicing at competing hospital systems in Colorado?
-Wes
Banner Health, the owner of McKee Medical Center in Loveland and the operator of North Colorado Medical Center in Greeley, soon will bar cardiologists who are not on the Banner payroll from practicing at the Greeley hospital. The denial of hospital privileges to cardiologists outside the Phoenix-based Banner system is the latest step in carving up the heart of the Northern Colorado health care market, where two dominant hospital groups — Banner and Poudre Valley Health System — vie for shares.I wonder who will stand up for patients if hospital-directed "standardized treatment procedures" are antiquated or just not right?
PVHS chief executive Rulon Stacey said the decision to block non-Banner cardiologists was an unprecedented step in Colorado’s health care industry.
“I personally have never seen, and don’t believe there is anywhere in Colorado, a policy of exclusivity that applies to cardiologists,” Stacey said Tuesday. “We have no plans to restrict access to any of our hospitals, and have never even discussed the topic.”
But Rick Sutton, former chief executive at McKee and now in his second year in the same position at NCMC, said the move was not about competition but about patient interests.
Sutton said the new policy, spelled out in a March 17 memo to his medical staff and taking effect April 19, was designed to standardize treatment procedures and reduce variation. He said Stacey’s criticism has no bearing on the goals of the new policy.
“That may be his experience and his opinion, but that doesn’t mean this is something we can’t do,” Sutton said.
-Wes
Wednesday, April 07, 2010
BoxTop Board Certification
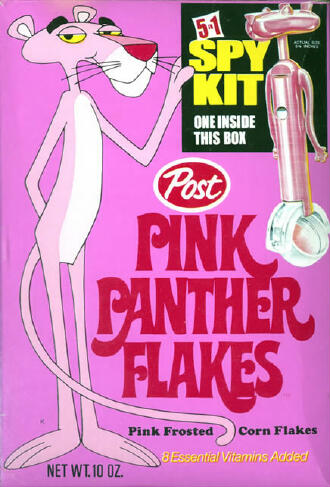 Remember when you were a child and an offer to be a member of a special spy club appeared on your morning cereal box? You knew, yes knew that the offer was the real deal. All you had to do is send in three cereal box tops and you'd be sent all the prerequisite items. Of course, when the plastic trinkets arrived weeks later, there always seemed to be the air of buzzkill when the reality of what you received for your efforts was revealed.
Remember when you were a child and an offer to be a member of a special spy club appeared on your morning cereal box? You knew, yes knew that the offer was the real deal. All you had to do is send in three cereal box tops and you'd be sent all the prerequisite items. Of course, when the plastic trinkets arrived weeks later, there always seemed to be the air of buzzkill when the reality of what you received for your efforts was revealed.This could never happen with board certification, could it?
Yesterday, we learned that this year, every specialist has to re-certify to maintain their status as a board certified specialist. In the past, this was a voluntary process that doctors participated in to show a jury of their peers that they had the right stuff to practice medicine at the highest level possible. It was a respected term. Doctors generally knew that a board certified specialist meant something. Even though doctors pay thousands of dollars to the American Board of Internal Medicine for the opportunity to study for and take the certification exam, once passed doctors were proud to hang that certificate on their wall. In effect, it is the crowning achievement of one's career.
But what if that certificate on the wall had the value of certificate purchased from a cereal box top spy club? Doctors might be pretty upset, right?
Well guess what. Although the majority of those certificates hanging on the wall are the real deal, many are not.
That's because the term "board certification" is not a legally protected term in most states of the United States, and if you want a "board certificate," you can just purchase one and hang it on your wall. No test, no nothing. Just send a guy several hundred bucks and fill out a very important sounding questionnaire and you're a member of the club!
Now this has been against the law. This has been illegal for many years. But none of this has made much difference - the scams continue. The sad reality is, the government does not have a history of effective oversight of these shiny new "certifying" initiatives.
For long-time readers of this blog, many are aware of my dealings that I stumbled upon by way of an anonymous comment that appeared on this blog several years ago that exposed a certain individual known to be operating such a fraudulent board certification scam. This scam is known by the American Board of Internal Medicine. This scam is known by the Illinois States Attorney's office and the Connecticut States Attorney's Office. But despite knowing about this individual for over nine years and his over thirty specialty "certificates" that he targets to primarily foreign medical graduates, he continues to operate this scam on-line.
Doctors who pay thousands of dollars for legitimate board certification should demand their states protect the term "board certification" to mean what it's supposed to mean: certification by the American Board of Internal Medicine. It must imply that they have taken the steps necessary to demonstrate they are at the top of their specialty. They should also demand from the American Board of Internal Medicine that they get something in return for their significant financial investment that is increasingly mandated by credentialing bodies: protection of the value of their certification.
And that means bringing these scam artists to justice.
Otherwise those certificates will be nothing more than a piece of paper from a cereal box top.
-Wes
Monday, April 05, 2010
Pacemakers and CERT Audits
Not only are doctors enjoying the prospects of a 21% pay cut this month, we're also beginning to see increase statistically-generated audits of our medical care directed solely from Medicare billing codes from 1996-2002 and applying them to 2010 practice patterns.
Here's a news release we received last week about dual chamber pacemakers:
So how to avoid these denials?
Document, document, document, and then document some more.
Still, despite adequate documentation, look for more time, expense and hassles to complete the CMS Medicare Determination Request Forms that are sure to come our way as we try to dispute these statistically-generated denials for our patients.
Funny how these costs of these administrative hassles are never tallied by CBO estimates of the cost of providing government-directed health care. Then again, given the $500-billion of Medicare cuts we are to expect from Medicare, this has been the plan all along.
-Wes
Here's a news release we received last week about dual chamber pacemakers:
National Government Services has recently received denials resulting from Comprehensive Error Rate Testing (CERT) audits of medical records for implantation of dual-chambered cardiac pacemakers. Denials for these types of claims can be very costly. In an effort to help decrease such denials, National Government Services would like to provide some information. The Centers for Medicare & Medicaid Services (CMS) published guidelines for coverage in the CMS Internet-Only Manual (IOM) Publication 100-03, Medicare National Coverage Determinations (NCD) Manual, Chapter 1, Part 1, Section 20.8, Cardiac Pacemakers, (437 KB) specifically Group II: Dual-Chambered Cardiac Pacemakers (effective since May 1985). We also would like to provide examples of denials we received from the CERT contractor.It appears government regulators will be auditing charts for evidence of the need for an atrial lead implantation in patients requiring dual chamber pacemakers for complete heart block or in cases of tachycardia/bradycardia syndrome. Coording to this release, examples of denials for dual chamber pacemakers have included:
Example 1: Beneficiary had a single chamber pacemaker for complete heart block which is covered by NCD 20.8. Replacement of a single chamber pacemaker with a dual chamber pacemaker requires documentation of NCD criteria such as “pacemaker syndrome” or ventricular asynchrony or the medical need based on cardiac status (needs to have atrial pacing in addition to a ventricular).It seems if there are no symptoms, then no atrial lead is likely to be permitted.
Example 2: The beneficiary’s predominant rhythm was atrial fibrillation with mention of bradycardia. The medical record is not sufficiently documented to show the heart rates and their correlation to the beneficiary's symptoms. For example the beneficiary's reported symptom of sweating but the symptom is not correlated to Holter monitor findings.
Example 3: The beneficiary had a history of atrial fibrillation and was treated with Coumadin. In addition the beneficiary had a history of prominent right heart failure and severe tricuspid regurgitation suggesting the beneficiary may have right atrial enlargement. The beneficiary had no history of prior pacemaker insertion. Dual chamber pacemaker was not supported in this case based upon the requirements listed in the NCD.
Example 4: Clinical findings of a history of hypertension, hyperlipidemia, and a Holter monitor indicating Tachy/brady syndrome. The beneficiary denied any SOB, dizziness, syncope, chest pain, weakness or fatigue. CMS criteria for single chamber pacemaker per the CMS IOM Publication 100-03, Medicare National Coverage Determinations (NCD) Manual, Chapter 1, Part 1, Section 20.8, Cardiac Pacemakers, (437 KB) not met for dual or single chamber pacemaker.
So how to avoid these denials?
Document, document, document, and then document some more.
Still, despite adequate documentation, look for more time, expense and hassles to complete the CMS Medicare Determination Request Forms that are sure to come our way as we try to dispute these statistically-generated denials for our patients.
Funny how these costs of these administrative hassles are never tallied by CBO estimates of the cost of providing government-directed health care. Then again, given the $500-billion of Medicare cuts we are to expect from Medicare, this has been the plan all along.
-Wes
Friday, April 02, 2010
Health Care Reform's Timeline
As the dust settles on the Great Health Care Reform Bill of 2010 passage in Congress, it's time to ask what we got for the effort. No matter what people thought of the bill before, like it or not, it's here.
Still, few people really understand what the bill contains and when the benefits and costs for the measure will be incurred on a year-by-year basis. Given the bill's complexity and tortuous path though Social Security and IRS tax codes, this really isn't a surprise, I suppose.
So here's my simplified broad-brush overview, broken down by year, culled from several sources referenced below:
TAX CHANGES
PRIVATE INSURANCE CHANGES
-Wes
Addendum:
These just in:
(1) (Video) Two doctors' perspectives on what health care reform will mean to them. Editor's note: Dr. Ivanovich's cowboy hat is a must-see)
(2) Kaiser Family Foundation does me one better.
Still, few people really understand what the bill contains and when the benefits and costs for the measure will be incurred on a year-by-year basis. Given the bill's complexity and tortuous path though Social Security and IRS tax codes, this really isn't a surprise, I suppose.
So here's my simplified broad-brush overview, broken down by year, culled from several sources referenced below:
TAX CHANGES
2010
New Tax Credit for Small Businesses: Provides a maximum credit of 35% of employers’ insurance premiums but is only available to those with fewer than 10 employees with wages under $25,000 per employee. This credit is completely phased-out for firms with more than 25 employees and wages above $50,000.
Ultra-Violet Treatment Tax: 10% tax on indoor UV treatments.
2011
Health Savings Accounts (HSAs)/Flexible Spending Accounts (FSAs): The federal government will prevent HSA and FSA patients from using their savings for over-the-counter medicine.
New Drug Tax: A new federal tax on sales of brand-name drugs for use in government health care programs.
W-2 Forms: The federal government will now require employers to disclose the full value of all benefits provided for every employee’s health insurance on the employee’s annual W-2 form.
2013
Medicare Payroll Tax: The federal government will increases the Medicare payroll tax by 0.9% to 3.8% for those with earned income above $200,000 individually or $250,000 for a couple.
New Investment Tax: The federal government will impose a new tax on investment income of 3.8% against all Americans with incomes above $200,000 individually or $250,000 for a couple.
New Medical Device Tax: The federal government will impose a new 2.3% tax on all medical devices (exempting just eyeglasses, contact lenses, hearing aids and devices they deem generally purchased by the retail public).
Higher Hospital Insurance Tax: The hospital insurance tax will increase 0.9 percentage points for those earning more than $200,000 ($250,000 for married filing jointly), and it includes net investment income.
2014
New Individual Mandate Begins: The federal government will require individuals to buy insurance or face tax penalties of up to $695 or 2.5% of income (whichever is greater).
New Employer Mandate Begins: The federal government will require that all employers with more than 50 workers who do not offer insurance or who offer coverage but their employees receive a federal insurance subsidy pay a new federal tax of up to $2,000 per employee for each employee over 30 employees.
New Insurance Subsidies Available: For individual or families above the Medicaid eligibility cutoff but below $88,200 (for a family of four) who are not offered or eligible for other insurance coverage, a tax credit is available to purchase insurance through the new government exchanges.
New Annual Tax on Health Insurance Providers: The federal government will levy a new tax on health insurance providers.
2018
New Premium Insurance Excise Tax: The federal government will impose a new 40% tax on high-quality insurance plans they define as “High-Cost”.
PRIVATE INSURANCE CHANGES
2010More highlights can be found here and here.
Dependent Coverage: Insurers are required to cover children up to age 26 on their parents’ plan.
Senior Drug Rebate: Seniors will get a $250 rebate to help fill the "doughnut hole" in Medicare prescription drug coverage, which falls between the $2,700 initial limit and when catastrophic coverage kicks in at $6,154.
High-Risk Pool for Pre-existing Conditions: Insurers will not be able to rescind policies to avoid paying medical bills when a person becomes ill. Funding is limited and individuals may be placed on a waiting list.
Pre-existing Conditions for Children: Limited protections to preclude insurance from excluding children with pre-existing condition.
2011
CLASS Program auto-enrollment: The federal government will establish a national insurance program for long-term care. The federal government will force employers to sign up their employees for payroll deductions in 2011 unless the employee specifically waives enrollment in writing.
2012
Nonprofit insurance coops developed: Sets up program to create nonprofit insurance co-ops that would compete with commercial insurers.
Accountable Care Organizations established: Hospitals and doctors "encouraged" to band together in quality-driven "accountable care organizations." Sets up an experimental "pilot program" to test more efficient ways of paying hospitals, doctors, nursing homes and other providers who care for Medicare patients from admission through discharge. Successful "experiments" would be widely adopted.
Readmission penalties: Establishes penalizes for hospitals with high rates of preventable re-admissions by reducing Medicare payments.
2014
Health Insurance Exchanges: The federal government will require states to establish an exchange for federally-approved health insurance.
Federal Standards for Insurance: The federal government will require all insurance plans to include federally-mandated benefits and coverage levels (Bronze, Silver, Gold, and Platinum).
Guaranteed Issue and Renewability: The federal government will require insurers to offer coverage to anyone wanting a policy and every policy has to be renewed.
Pre-Existing Conditions: The federal government will mandate that insurers cannot impose any pre-existing condition exclusion.
New Individual Mandate Begins: The federal government will require all Americans to buy insurance or face taxes up to $696 or 2.5% of income (whichever is greater). There is a phase-in to the penalties: If they do not have acceptable coverage, the penalty will be $95 in 2014, $325 in 2015, and $695 (or up to 2.5 percent of income) in 2016. Families will pay half the amount for children, up to a cap of $2,250 per family. After 2016, penalties are indexed to Consumer Price Index.
New Employer Mandate Begins: The federal government will require all employers with more than 50 employees who do not offer insurance or who offer coverage but their employees receive a federal insurance subsidy to pay a penalty of up to $2,000 per employee for each employee over 30 employees.
2016
State Compacts: If the federal government approves, states would be allowed to begin a multi-state compact for insurance.
2017
Large Group Market: If the federal government approves, states may allow large group insurers to sell in the exchange.
Waiver for State Innovation: If the federal government approves, states may ask for a limited waiver from certain federal requirements.
2018
New Premium Insurance Tax: The federal government will impose a new 40% tax on high-quality insurance plans that it defines as “High-Cost”. (The so-called "Cadillac Insurance" exemption negotiated for the powerful unions remained in the bill).
-Wes
Addendum:
These just in:
(1) (Video) Two doctors' perspectives on what health care reform will mean to them. Editor's note: Dr. Ivanovich's cowboy hat is a must-see)
(2) Kaiser Family Foundation does me one better.
One Heart Nailed
... and he lived (video) to talk about it:
-Wes
The man’s heart was pierced as he was nailing boards with a co-worker at a carpentry shop. The shop’s owner said the men were working together, when suddenly, they ran into each other resulting in the nail gun going off.Oops.
-Wes
Subscribe to:
Comments (Atom)