Money does that to people. We should not be surprised.
In keeping with the reviews from 2015 and 2016, here is the wrap-up of some of key events concerning Maintenance of Certification® (MOC®) for 2017:
4 January 2017 - Richard Baron, MD and Clarence H. Braddock, III, MD publish a promotional article for ABIM in the New England Journal of Medicine and given the comments, probably wish they hadn't.
20 January 2017 - Stationary sidebars can be revealing: The interconnected conflicts of interest with University of California, San Francisco, MOC®, the New England Journal of Medicine, and the ABIM/ABIM Foundation are disclosed.
6 February 2017 - Practicing Physicians of America, Inc is born and requests IRS investigation of the ABIM at the Library of Congress in Washington, DC.
6 February 2017 - TeamHealth eats the Department of Justice's $60 million judgment for Medicare fraud, but is swallowed quietly by Blackstone Group.
17 March 2017 - Federal judge dismissed ABIM's copyright infringement suit against Puerto Rican Dr. Salas Rushford. Salas Rushford's countersuit to proceed.
21 March 2017 - Wallstreet lawyer attempts to attack the integrity of the investigative reporting on this blog concerning the ABIM's Director of Test Security. Rebuttal appears in Pennsylvania Medicine Magazine and becomes the most read blog post of 2017 thanks to the Streisand Effect.
31 March 2017 - ABIM announces their much-anticipated "modifications" to their MOC program, gets it wrong again.
3 April 2017 - State legislative anti-MOC® battles continue in Tennessee
12 April 2017 - Elizabeth's Rosenthal's book An American Sickness appears on the New York Times best seller list, includes reference to the ABIM $2.3 million condo story.
29 April 2017 - The state legislative battle continued in Texas.
3 May 2017 - Journal of the American Medical Association devotes an entire issue to conflicts of interests in medicine, but forgets to disclose its own.
26 June 2017 - Antitrust suit against American Osteopathic Association is allowed to proceed to the discovery phase
30 June 2017 - Anti-MOC legislation in Texas passes with some concessions, goes into effect 1 Jan 2018.
3 July 2017 - Practicing Physicians of America, Inc starts fund drive to assist with anti-MOC legislative efforts.
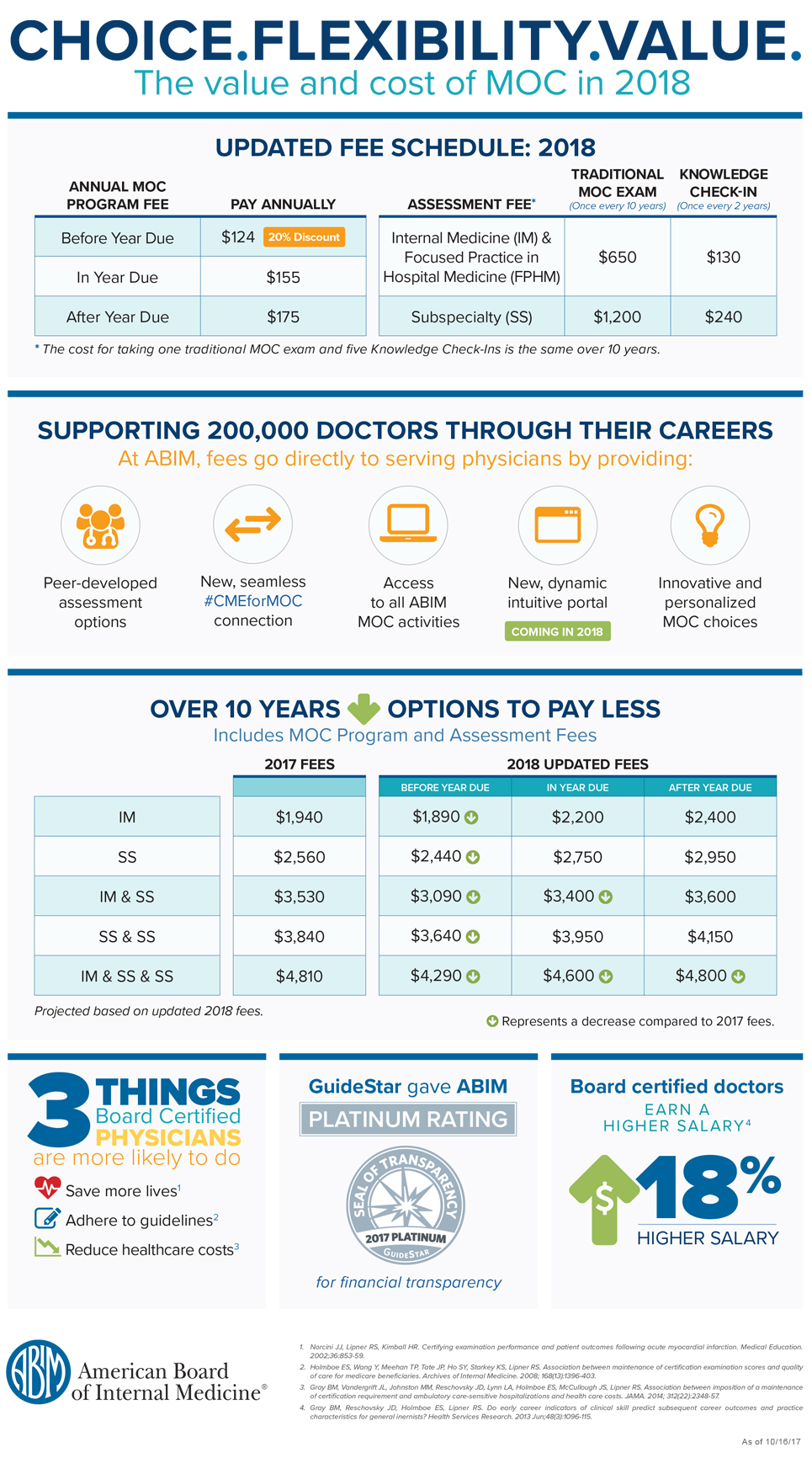
1 August 2017 - Research letter detailing the costs and fees for Maintenance of Certification® appears in JAMA.
6 Aug 2017 - ABMS responds to JAMA article on MOC® costs as "crucial to sustain and evolve."
11 October 2017 - Ohio legislature receive my testimony and an evidence packet on anti-MOC House Bill 273 regarding the corruption of the ABIM before the Health Committee.
31 October 2017 - ABIM joins the Human Diagnosis project
4 December 2017 - A key meeting of State Medical Societies, ABMS and ABIM leadership, and numerous medical specialty societies convenes to discuss problems with MOC®; admits the MOC® process is "problematic."
13 December 2017 - ABMS and "partners" from other ACGME organizations including the AAMC and CCMS, alongside some select medical specialty societies, announce new "Vision Commission" to re-brand MOC®. More coverup seems inevitable.
13 December 2017 - Federal judge in the Northern District of Illinois dismisses the antitrust suit by the AAPS against the ABMS using a curious timeline, but leaves a door open to "file an amended complaint that cures the deficiencies discussed in this Memorandum Opinion."
* * *
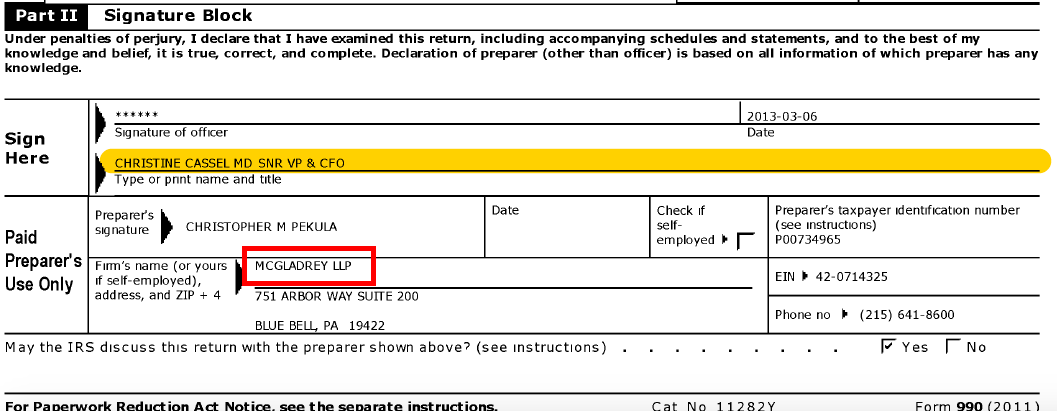
Today is New Year's Eve. Whether ABIM is solvent or not is uncertain. We will likely have to wait until May of 2018 to know for sure, since 501(c)(3) corporations can file a request to delay publishing of their Form 990 for Fiscal year 2017 until then. But the financial trend toward collapse of the ABIM and ABIM Foundation, legal troubles, and the unannounced closure of divisions within the ABIM, like the Division of Test Security and the Division of Policy in January 2017 give some hints to what is (and has been) going on there.
Bit by bit, real clinic doctors are making a difference in fighting MOC®. I encourage all readers of this blog to consider joining or donating to Practicing Physicians of America or to become certified by the National Board of Physicians and Surgeons to help continue this fight.
Together practicing physicians can make 2018 a successful and prosperous anti-MOC® new year for those of us on the front line of patient care.
-Wes