Today, the official Notice of Appeal was filed in the United States Court of Appeals for the
Third Circuit in Pennsylvania. It appears the ABIM's legal headaches regarding Maintenance of Certification (MOC) are far from over.
Working physicians can help the plaintiffs in their David-versus-Goliath effort to end the unproven American Board of Medical Specialties' MOC program by contributing to Practicing Physicians of America's GoFundMe page created on their behalf. We have almost reached our $400,000 goal. (Your contribution may be tax deductible before year's end - please consult your tax advisor.)
-Wes
Monday, December 30, 2019
Thursday, December 12, 2019
Just In Time for Christmas: The MOC Legal Juggernaut Intensifies
With the recent back-to-back announcements that the class action antitrust and racketeering lawsuit against the American Board of Internal Medicine (ABIM) and the antitrust lawsuit against the American Board of Radiology were dismissed (e.g., the ABIM announcement and ABR announcement), doctors everywhere - both young and old - seemed resigned to the fact that they will have to be subjects to lifelong extortion of private American Board of Medical Specialties member boards and their affiliates if they wanted to practice medicine in the United States.
But fear not, dear colleagues. I bring you tidings of great joy. The first great Supplemental Opposition to the Motion to Dismiss the lawsuit against the American Board of Psychiatry and Neurology (ABPN) was filed yesterday that promises to renew the call for justice on the basis of proper legal procedural grounds:
We can anticipate that the multitude of moneyed interests behind Maintenance of Certification will stop at nothing to assure this unlawful program continues unchecked.
Still, a bit of hope and cheer is always welcome for working physicians this time of year.
Merry Christmas!
-Wes
P.S.: On a separate legal note:
Remember the Puerto Rican physician, Jaime Salas Rushford, MD, whom the ABIM revoked his board certification and dragged him through the court system since 2012 with a dismissed time-barred cheating claim while the President and CEO of the ABIM simultaneously failed to disclose her conflicts of interest with Kaiser and Premier Inc? Yesterday, the judge issued the following order to expedite the counterclaim suit filed against ABIM by Salas Rushford:
Readers wishing to support the brave physician plaintiffs involved in these lawsuits trying to end the unlawful Maintenance of Certification program are encouraged to contribute to their GoFundMe campaign.
But fear not, dear colleagues. I bring you tidings of great joy. The first great Supplemental Opposition to the Motion to Dismiss the lawsuit against the American Board of Psychiatry and Neurology (ABPN) was filed yesterday that promises to renew the call for justice on the basis of proper legal procedural grounds:
Defendant American Board of Psychiatry and Neurology (“ABPN”) illegally ties its initial certification product, which it sells to new doctors to demonstrate completion of their medical education and assess the quality of their residency program, and its MOC product, which it requires some older doctors, but not all, to purchase throughout their careers to demonstrate lifetime learning or forfeit their initial certification. ABPN brings to the court’s attention Kenney v. American Board of Internal Medicine, No. 18-5260, 2019 U.S. Dist. LEXIS 164725 (E.D. Pa.Sept. 26, 2019) (“Kenney”), and Siva v. American Board of Radiology, No. 19 C 1407, 2019 U.S. Dist. LEXIS 200645 (N.D. Ill. Nov. 19, 2019) (“Siva”). Kenney came first, followed by Siva which “agree[d] with the reasoning in Kenney.” Id. at *11.1The supplemental opposition to the ABPN motion to dismiss then outlines multiple legal reasons why the plaintiffs believe the decisions were wrongly decided. In essence, the attorneys are arguing that the facts in this case were not even allowed to be considered past the judges' chambers.
Nothing in those opinions changes ABPN’s unlawful conduct. A critical reading of the opinions and application of the universally accepted rule that well-pleaded factual allegations and all reasonable inferences therefrom must be taken as true compels the conclusion that Kenney and Siva were, respectfully, wrongly decided.1 The tying claims in Kenney were dismissed with prejudice without plaintiffs being allowed to amend, the court finding as a matter of law that separate products could never be alleged. Plaintiffs are appealing that ruling. The claims in Siva were dismissed without prejudice and plaintiff is filing an amended complaint on January 10, 2020.
We can anticipate that the multitude of moneyed interests behind Maintenance of Certification will stop at nothing to assure this unlawful program continues unchecked.
Still, a bit of hope and cheer is always welcome for working physicians this time of year.
Merry Christmas!
-Wes
P.S.: On a separate legal note:
Remember the Puerto Rican physician, Jaime Salas Rushford, MD, whom the ABIM revoked his board certification and dragged him through the court system since 2012 with a dismissed time-barred cheating claim while the President and CEO of the ABIM simultaneously failed to disclose her conflicts of interest with Kaiser and Premier Inc? Yesterday, the judge issued the following order to expedite the counterclaim suit filed against ABIM by Salas Rushford:
The American Board of Internal Medicine may file its motion for judgment on the pleadings no later than December 18, 2019. Dr. Salas-Rushford will respond no later than January 2, 2020. The Board may reply no later than January 9, 2020. The case schedule will be discussed at the scheduling conference to be held on January 31, 2020. Signed by Judge Francisco A. Besosa on 12/11/2019. (brc) (Entered: 12/11/2019)It seems that case will soon be coming to a head, too.
Readers wishing to support the brave physician plaintiffs involved in these lawsuits trying to end the unlawful Maintenance of Certification program are encouraged to contribute to their GoFundMe campaign.
Wednesday, December 04, 2019
ABIM's Dark Side Needs More Light
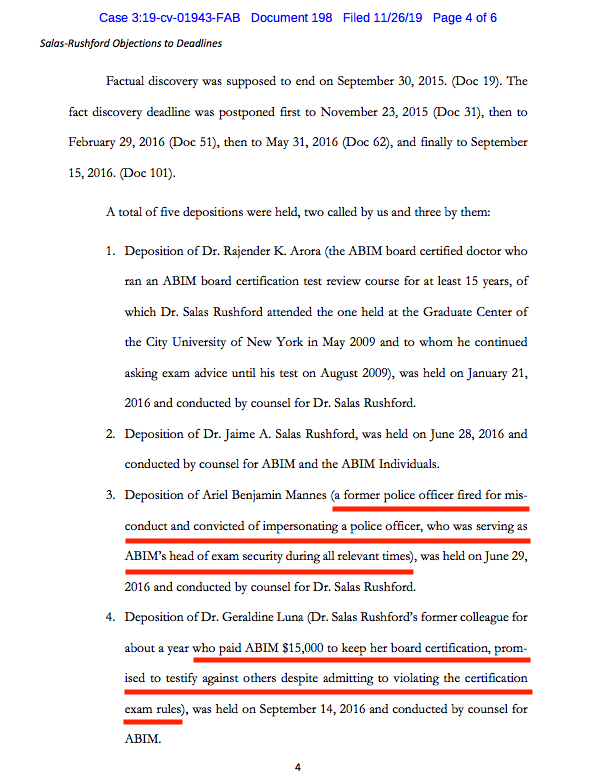
From the recently filed "Objections to Deadlines due to Completion of Discovery" by Plaintiff Jaimie Salas Rushford, MD in Puerto Rico Federal Court comes public evidence of mafia-like tactics used against physicians by the American Board of Internal Medicine (ABIM) to protect their certification testing monopoly:
So to summarize some of what has transpired at the ABIM to maintain their physician testing monopoly:
 |
| (Click image to enlarge) |
So to summarize some of what has transpired at the ABIM to maintain their physician testing monopoly:
- The ABIM secretly created the ABIM Foundation in 1989 for the purpose of laundering over $70 million of physician testing fees from 1990-2007 for various personal and political agendas, including the purchase of a 2-bedroom luxury condominium, art collection, and offshoring of Cayman Island retirement funds.
- They published a white paper in 2002 in two major medical journals, the Annals of Internal Medicine and the Lancet, entitled "Medical Professionalism in the New Millennium: A Physician Charter" (which, given these revelations, should both be retracted in my opinion).
- They used a strongman convicted of impersonating a police officer and carrying an unregistered firearm as their Director of Test Security with access to physicians' most sensitive personal information.
- They forced a physician who admitted to wrongdoing to pay $15,000 to remain board certified on the condition that physician also serve as an informant.
- They continue to drag a vulnerable physician through the court system for what will be at least eight years to maintain their monopoly and hide the truth.
The American Board of Internal Medicine needs to be held accountable to working US physicians and the public for their actions. I believe their irresponsible and undisclosed financial and political dealings, paired with these mafia-like tactics, deserve full transparency and appropriate judicial scrutiny.
Physicians deserve better. The public deserves better.
It's past time we shine a bright light on this racket.
-Wes
Saturday, November 30, 2019
Watching Our Healthcare Hindenburg Burn
Just before Thanksgiving, 15 physicians were notified they will be replaced by less-experienced and cheaper nurse practitioners at the nearly $1 billion Edwards-Elmhurst healthcare system here in Chicago. Doctors, the article says, were "broadsided," perhaps because they were naive to events that occurred in Springfield, IL earlier this year. Thanks to aggressive lobbying, recent legislation was unanimously passed in both the House and Senate Illinois legislature allowing nurse practitioners to practice independently of physicians in any capacity except surgery. Working doctors likely missed this since they don't populate legislative halls - they populate clinics and hospitals caring for patients - or at least most did.
This trend of using more and more nurse practitioners in lieu of physicians appears to be accelerating nationwide as large hospital systems or consolidated primary care clinics with bloated numbers of midlevel administrators look to cut costs. Nurse practitioners are everywhere now: staffing ICUs, Emergency Rooms, and yes, primary care clinics. Some nurse practitioners are used to preferentially fill lucrative surgical pipelines armed with little other knowledge than what a routine case for surgery requires. And while advanced practice nurse practitioners do treat common ailments like earaches and sore throats, often quite well, how many can recognize the warning signs of a case of epiglottitis? What happens to patients then?
Is compromising years of physician training and care experience for cost efficiency really about patient care or cost savings or a facility's bottom line? Is the inevitable pitting of nurses against doctors in the patient's best interest or the institution's? Who sees the costs supposedly saved by hiring cheaper advanced practice nurses? Will Edward-Elmhurst Healthsystem suddenly stop spending millions on collection agents who served as second-largest contractor for Edward-Elmhurst Healthsystem in Fiscal Year 2018?
Working physicians aren't without some blame either. Where were the physicians on the Medical Executive Committee of Edward-Elmhurst Healthsystem with this announcement? Did they approve replacing 15 physician-colleagues for lesser-trained nurse practitioners or fearful of losing their jobs if they didn't "align" themselves with this administrative move? Who is advocating for patients at Edward-Elmhurst Healthsystem (or any other large non-physician run hospital system) now? Anyone?
Can Dr. Google and inexperienced physician posers safely replace the highly trained, experienced physician? No one really knows. This latest move is little more than a grand experiment promoted by healthcare consultants with patients' lives on the line. Which leads us to ask: is touting a shortage of US physicians really a concern of the Association of American Medical Colleges or just a ploy by other member organizations of Accreditation Council for Graduate Medical Education (like the American Hospital Association) to justify these physician firings so hospitals can pad their bottom line?
Our Healthcare Hindenburg is burning: a bubble of excessive prices, high middleman salaries, a rapidly accelerating physician shortage, competition of healthsystems and patients increasingly unable to pay even basic co-pays for healthcare, medications, and procedures, as they are left to take the financial hit to maintain the health care industrial complex's status quo.
In healthcare, it's "Winner Takes All" with the likes of PriceWaterHouseCooper, McKinsey, and the Advisory Board at the helm. The competition is fierce.
Patients (and their better-trained frontline physicians) be damned.
-Wes
This trend of using more and more nurse practitioners in lieu of physicians appears to be accelerating nationwide as large hospital systems or consolidated primary care clinics with bloated numbers of midlevel administrators look to cut costs. Nurse practitioners are everywhere now: staffing ICUs, Emergency Rooms, and yes, primary care clinics. Some nurse practitioners are used to preferentially fill lucrative surgical pipelines armed with little other knowledge than what a routine case for surgery requires. And while advanced practice nurse practitioners do treat common ailments like earaches and sore throats, often quite well, how many can recognize the warning signs of a case of epiglottitis? What happens to patients then?
Is compromising years of physician training and care experience for cost efficiency really about patient care or cost savings or a facility's bottom line? Is the inevitable pitting of nurses against doctors in the patient's best interest or the institution's? Who sees the costs supposedly saved by hiring cheaper advanced practice nurses? Will Edward-Elmhurst Healthsystem suddenly stop spending millions on collection agents who served as second-largest contractor for Edward-Elmhurst Healthsystem in Fiscal Year 2018?
Working physicians aren't without some blame either. Where were the physicians on the Medical Executive Committee of Edward-Elmhurst Healthsystem with this announcement? Did they approve replacing 15 physician-colleagues for lesser-trained nurse practitioners or fearful of losing their jobs if they didn't "align" themselves with this administrative move? Who is advocating for patients at Edward-Elmhurst Healthsystem (or any other large non-physician run hospital system) now? Anyone?
Can Dr. Google and inexperienced physician posers safely replace the highly trained, experienced physician? No one really knows. This latest move is little more than a grand experiment promoted by healthcare consultants with patients' lives on the line. Which leads us to ask: is touting a shortage of US physicians really a concern of the Association of American Medical Colleges or just a ploy by other member organizations of Accreditation Council for Graduate Medical Education (like the American Hospital Association) to justify these physician firings so hospitals can pad their bottom line?
Our Healthcare Hindenburg is burning: a bubble of excessive prices, high middleman salaries, a rapidly accelerating physician shortage, competition of healthsystems and patients increasingly unable to pay even basic co-pays for healthcare, medications, and procedures, as they are left to take the financial hit to maintain the health care industrial complex's status quo.
In healthcare, it's "Winner Takes All" with the likes of PriceWaterHouseCooper, McKinsey, and the Advisory Board at the helm. The competition is fierce.
Patients (and their better-trained frontline physicians) be damned.
-Wes
Sunday, November 24, 2019
The AMA and ABMS Member Boards: Banking on the Promise of Private Equity
Recently, I was sent a prospectus for a medical device company that caught the eye of a local Venture Capital funding group. On that prospectus was this paragraph for a "vision" of future of a "clinical decision support system:"
In short, this is what health care market investors see now: a vision where fewer staff, more data entry, and less humanity and human touch are sold as better health care. Worse still, working physicians who remain are being grown and matured in a muzzled petri dish where dissent is openly discouraged by employers and "certifying" bodies.
This data-driven model didn't work out so well for Boeing.
And it won't work so well for health care either.
But don't tell that to the American Medical Association. Because to the AMA, working physicians in the US are little more than data entry ports "Moving Medicine" toward the AMA's latest vision for a business-oriented private equity-driven health care model for tomorrow.
-Wes
Collects data from the electronic medical record, medical literature, regulatory warnings and other internet-based public information. Provides analysis of intra-procedural progress that integrates this data with procedural imaging and patient status. Includes predictive analytics with the use of cognitive computing to support optimal clinical decision making."This pitch was little more than a marketed promise of artificial intelligence, of instant processing of black-box algorithms, of equity funding to solve healthcare's less-than optimal patient outcomes using the internet, numbers, cut-copy-and-paste data entry, physician testing scores, in one big algorithmic, dehumanized, robotic mess.
In short, this is what health care market investors see now: a vision where fewer staff, more data entry, and less humanity and human touch are sold as better health care. Worse still, working physicians who remain are being grown and matured in a muzzled petri dish where dissent is openly discouraged by employers and "certifying" bodies.
This data-driven model didn't work out so well for Boeing.
And it won't work so well for health care either.
But don't tell that to the American Medical Association. Because to the AMA, working physicians in the US are little more than data entry ports "Moving Medicine" toward the AMA's latest vision for a business-oriented private equity-driven health care model for tomorrow.
-Wes
Friday, November 15, 2019
Timeline for Justice: ABIM v Salas Rushford
A young resident physician, Jaime Salas Rushford MD, came to New Jersey from Puerto Rico to study for his initial American Board of Internal Medicine (ABIM) board certification examination with an ACGME-approved Arora "Unusual Board Review" course. He later took his examination and passed, making him officially board certified on 8/20/2009.
Over three years later, he received a letter from Ms. Lynn O. Langdon, Chief Operating Office of the ABIM at the time, that his board certification was suddenly, indefinitely revoked because of claims he "collected and compiled hundred of ABIM examination questions from multiple sources" and that he "sent hundreds of ABIM examination questions" from his email to Arora Board Review. The letter implied he did "not maintain moral, ethical, or professional behavior satisfactory to the Board," engaged in "misconduct adversely affecting " his integrity, and engaged in "behavior that subverts the examination process."
Because the ABIM felt he violated their "Pledge of Honesty," the Board elected to "indefinitely revoke" his certification and "notify the Medical Board in every jurisdiction" that he was licensed.
He had 10 days to appeal that decision through a never-disclosed ABIM "three-stage appeal process" that lasted two years. Following this, he later discovered the ABIM had filed a copyright infringement lawsuit against him.
He describes the ordeal in detail here. In that description, he notes the additional reprimanding of some "2700 physicians," the use of a "spy" sent to the board review course he attended, the secret funneling of millions of dollars of ABIM Diplomate testing fees to create the ABIM Foundation, the raid using federal Marshals of Dr. Arora's home to copy computer files and secure physician's email addresses, and the undisclosed conflicts of interest of Christine Cassel, MD, former President and CEO of the ABIM, none of which were known to Diplomates of the ABIM at the time.
Instead, the ABIM issued a press release that was picked up by the Wall Street Journal and shocked the medical community on June 9, 2010, detailing the sanctioning of 139 physicians for claims of "cheating:"
On 7 Nov 2019, the case management order for this lawsuit was published by the federal judge Francisco A. Besosa with the following timeline:
Perhaps now light will shine on the inner dealings of the so-called "voluntary" US Physician Board Certification process that has harmed practicing physicians without accountability or means of due process for years.
-Wes
Over three years later, he received a letter from Ms. Lynn O. Langdon, Chief Operating Office of the ABIM at the time, that his board certification was suddenly, indefinitely revoked because of claims he "collected and compiled hundred of ABIM examination questions from multiple sources" and that he "sent hundreds of ABIM examination questions" from his email to Arora Board Review. The letter implied he did "not maintain moral, ethical, or professional behavior satisfactory to the Board," engaged in "misconduct adversely affecting " his integrity, and engaged in "behavior that subverts the examination process."
Because the ABIM felt he violated their "Pledge of Honesty," the Board elected to "indefinitely revoke" his certification and "notify the Medical Board in every jurisdiction" that he was licensed.
He had 10 days to appeal that decision through a never-disclosed ABIM "three-stage appeal process" that lasted two years. Following this, he later discovered the ABIM had filed a copyright infringement lawsuit against him.
He describes the ordeal in detail here. In that description, he notes the additional reprimanding of some "2700 physicians," the use of a "spy" sent to the board review course he attended, the secret funneling of millions of dollars of ABIM Diplomate testing fees to create the ABIM Foundation, the raid using federal Marshals of Dr. Arora's home to copy computer files and secure physician's email addresses, and the undisclosed conflicts of interest of Christine Cassel, MD, former President and CEO of the ABIM, none of which were known to Diplomates of the ABIM at the time.
Instead, the ABIM issued a press release that was picked up by the Wall Street Journal and shocked the medical community on June 9, 2010, detailing the sanctioning of 139 physicians for claims of "cheating:"
"Any high-school kid knows that cheating is unfair," said Dr. Christine Cassel, president and chief executive of the ABIM, who called the sanctions "a message and a deterrent."The ABIM subsequently lost the copyright infringement lawsuit against Salas Rushford, but his counterclaim lawsuit filed against the ABIM goes on after being recently moved to Puerto Rico Federal District Court.
The ABIM's move springs from a case involving test-prep firm Arora Board Review, which it sued last year. The ABIM's suit alleged that Arora instructors told class members the review questions were from the actual exam and solicited them to supply the company with additional questions they remembered after taking certification exams.
The ABIM and an attorney for Livingston, N.J.-based Arora both said they are in settlement talks. Arora's website says it has "put [its] business on hold until a settlement is reached in the near future."
Materials seized from Arora in December as part of the case included 2,000 emails and audio and other communications from physicians disclosing exam questions, according to the ABIM.
Based on these materials, the ABIM sued Monica Mukherjee of Washington, D.C.; Anastassia Todor of Aurora, Colo.; Pedram Salehi of Los Angeles; Sarah Von Muller of Tulsa, Okla.; and Frederick Oni of Warner Robins, Ga.
Dr. Mukherjee couldn't be reached for comment. Dr. Todor and Dr. Salehi had no comment. Dr. Oni said he didn't know the questions he purchased were from previous tests.
Dr. Von Muller said courses like Arora's are necessary for busy physicians attempting to get their optional board certification.
Dr. Cassel said she doesn't believe sharing or selling actual questions is common. "We have a great deal of confidence that most people don't cheat on this exam," she said, adding that there are "legitimate board-review programs that continue to function." (The ABIM doesn't offer its own review courses.)
The "hundreds" of allegedly infringing questions used by the course were removed from the pool of questions used on the computerized tests starting in 2009. Doctors who took the Arora course but weren't sanctioned or sued will get letters of reprimand, the ABIM said.
On 7 Nov 2019, the case management order for this lawsuit was published by the federal judge Francisco A. Besosa with the following timeline:
- 29 Nov 2019 - Objections to Case Management Deadlines and all outstanding pleadings due.
- 3 Dec 2019 - Motions to amend the pleadings or add parties to be filed.
- 31 Jan 2020 - initial Case Management and Settlement Conference
- 29 May 2020 - Motions to Dismiss must be filed
- 30 Dec 2020 - All discovery must be completed
- 9 Apr 2021 - Pretrial and Settlement Conference
- 19 Apr 2021 - Trial Shall Begin (09:00AM)
Perhaps now light will shine on the inner dealings of the so-called "voluntary" US Physician Board Certification process that has harmed practicing physicians without accountability or means of due process for years.
-Wes
Tuesday, November 12, 2019
Is CMS's Value-Based Healthcare System Already Being Gamed?
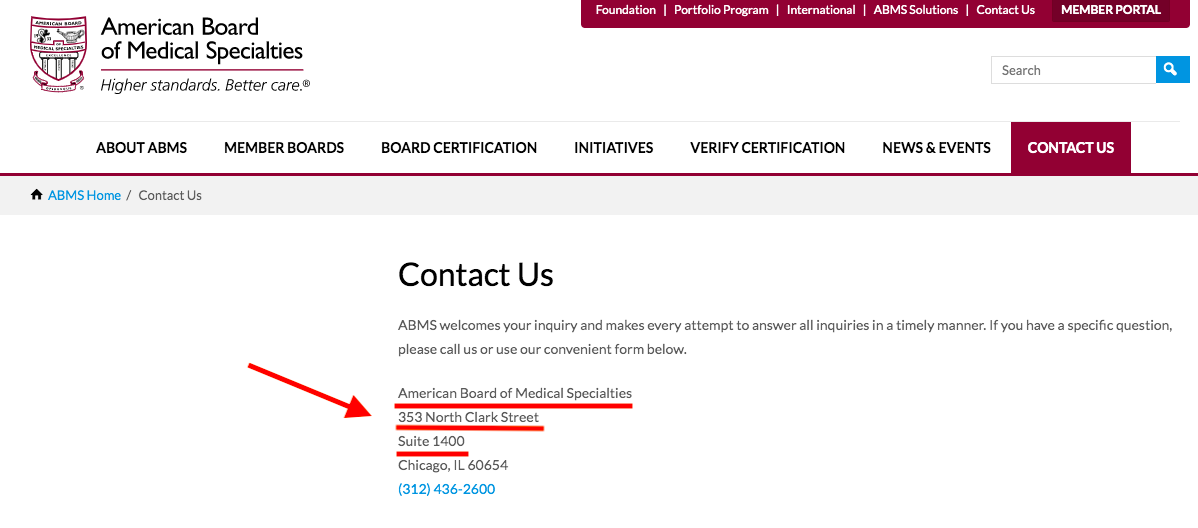
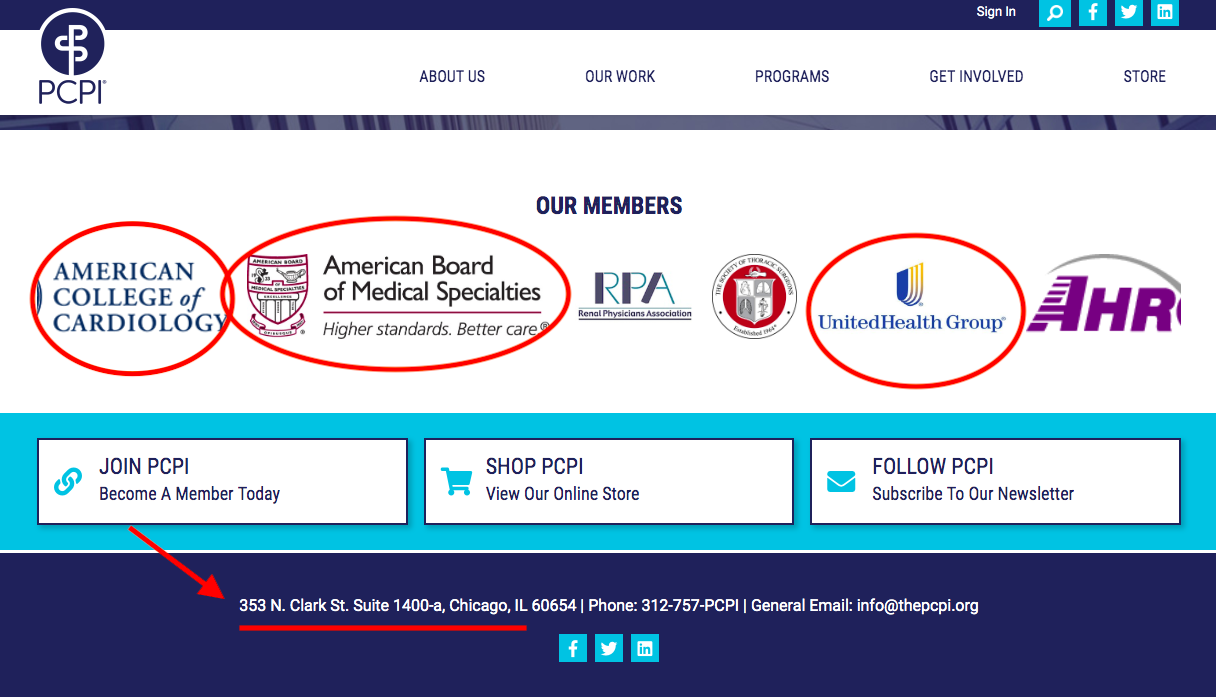
Take a look at the address of the American Board of Medical Specialties (ABMS) that owns the Maintenance of Certification (MOC®) trademark that is the subject of at least six anti-trust lawsuits (see here, here, and here for instance) underway because MOC binds physicians to their hospital privileges and insurance payments to made to hospitals on behalf of their employed physicians:
Now look at the address of the American Medical Association (AMA)-sponsored PCPI Foundation with board members from UnitedHealthcare, Premier, the American College of Cardiology, the American College of Physicians, several trustees of the AMA, and others:
Recall that the AMA maintains a monopoly on the procedure codes (CPT® codes) for every medical procedure performed in the United States and sells the rights to use that database to insurers and electronic medical record companies. Each of the AMA codes, then, have particular "value" to hospitals and insurers.
The AMA also determines the "relative value system" used by the government coding for weighting physician compensation that strongly incentivizes physician behavior. Some procedures, then, have more "value" to physicians than others. Hospitals know this, too.
Gee, I wonder, with all these codes and friends that stand to profit on the backs of working physicians and our patients, is the Affordable Care Act's value-based healthcare already being gamed?
-Wes
Now look at the address of the American Medical Association (AMA)-sponsored PCPI Foundation with board members from UnitedHealthcare, Premier, the American College of Cardiology, the American College of Physicians, several trustees of the AMA, and others:
Recall that the AMA maintains a monopoly on the procedure codes (CPT® codes) for every medical procedure performed in the United States and sells the rights to use that database to insurers and electronic medical record companies. Each of the AMA codes, then, have particular "value" to hospitals and insurers.
The AMA also determines the "relative value system" used by the government coding for weighting physician compensation that strongly incentivizes physician behavior. Some procedures, then, have more "value" to physicians than others. Hospitals know this, too.
Gee, I wonder, with all these codes and friends that stand to profit on the backs of working physicians and our patients, is the Affordable Care Act's value-based healthcare already being gamed?
-Wes
Saturday, November 09, 2019
MOC®: It's All About Physician Data
The Facebook–Cambridge Analytica data scandal was a major political scandal in early 2018 when it was revealed that Cambridge Analytica had harvested the personal data of millions of peoples' Facebook profiles without their consent and used it for political advertising purposes. The scandal, first exposed by The Guardian in 2015, revealed that Cambridge Analytica had managed to obtain data on millions of Facebook users in the UK, US, and beyond, made possible through "improper sharing" practices conducted between the "This Is Your Digital Life" Facebook app developer and the company. By giving this third-party app permission to acquire their data, back in 2015, this also gave the app access to information on the user's friends network; this resulted in the data of about 87 million users, the majority of whom had not explicitly given Cambridge Analytica permission to access their data, being collected.
Because patients do not give consent for the use of their data, who better to target for access to sensitive patient-related information than those entrusted with their care? As details come to light about the American Board of Medical Specialties' (ABMS) Maintenance of Certification (MOC) program that has plagued physicians since 1990, many similarities to the Cambridge Analytica data-sharing scandal are appearing. The adhesion contract that forms the basis for MOC and is increasingly tied to physician hospital privileges and insurance reimbursements, assures this data pipeline remains open:
Group purchase organizations (GPOs) and Pharmacy Benefit Managers (PBMs) decide what equipment appears on a database for hospitals to purchase. Companies pay those GPOs and PBMs to be on the list. Doctors' equipment choices and pharmaceutical preferences influence that list. Companies want to know what doctors are using and who doctors are seeing. By knowing their patterns and knowing the procedures performed on patients, highly sensitive patient information can be deduced. Registries owned by procedurally-heavy specialty societies (like the American College of Cardiology) are a particularly ripe source of procedural data, particularly when it can be made doctor-specific (where MOC comes in). More data sales occur. Repeated MOC testing and demographic data entries required by physicians assures these physician-specific databases are kept current. Having the President and CEO of the American Board of Internal Medicine on the President's Council of Advisors for Science and Technology assured uninterrupted marketing access to physicians and their patients.
By using physician information and their patient care information for these corporate purposes, the ABMS/ABIM MOC® product looks more like Cambridge Analytica than a physician education tool and affects far more people's health care than the Cambride Analytica ever did.
So how how do all these organizations coordinate and connect their MOC data, registries, and corporate databases?
Through a virtually undisclosed tax-exempt AMA-funded private foundation shamelessly called the Physician Consortium for Performance Improvement (PCPI).
Reportedly formed in 2000 with the help of the AMA, the PCPI Foundation is located just blocks away from the AMA's corporate headquarters in downtown Chicago. The organization describes itself as follows:
The remainder of the Board of Directors include:
Members get to "access the latest tools and insights on performance measurement, clinical registries, and quality improvement" as well as "influence through representation on the PCPI board, committees, advisory and other, as well as expert panels and task forces."
Members of this organization, according to the revolving banner on the PCPI website, include:
AvaMed, FigMD (MOC data collectors), AMA, ACP, ACC, ABMS, Informed Patient Institute, CMSS, Am Society of Clinical Oncology, The American Health Quality Association, Am College of Occupational Medicine, Primaris (A healthcare consulting and data abstraction company), American Academy Foot and Ankle Orthopedics Society, UnitedHealth Group (Market cap: $262B), The Society of Thoracic Surgeons, Pharmacy Quality Alliance, American Gastroenterology Association, Health Care Services Platform, American Optometric Association, Academy of Nutrition and Dietetics, American Heart Association, American College of Radiology, and on, and on...
It's handsomely paid CEO and Executive Director, Kevin Donnelly, is a non-physician, too. Here's their latest 2017 IRS filing that confirms a cool $2.78M contribution from the AMA to the PCPI and contains this explanation why the organization is not a true public "charity" after all:
Are UnitedHealth, Humana, Blue Cross Blue Shield, Premier, AvaMed (and all the medical device companies they represent), FigMD, and Primaris really about "quality" or their own bottom line?
Is there any wonder, then, that when a physician points out certain conflicts to medical editors of the Journal of the American Medical Association (JAMA) or the New England Journal of Medicine (owned by the Massachusetts Medical Society), he can't get a straight answer and is referred by the conflicted party to IRS tax filings?
One thing's for sure, to the best of my knowledge and belief, these multiple organizations are colluding with each other for their own best interests ("covert rationing" - a concept coined by the prescient Dr. Richard Fogoros) and using our physician MOC® data to drive their bottom lines while hiding behind non-profit tax law and the ruse of assuring the public it's all in the name of "quality."
-Wes
Because patients do not give consent for the use of their data, who better to target for access to sensitive patient-related information than those entrusted with their care? As details come to light about the American Board of Medical Specialties' (ABMS) Maintenance of Certification (MOC) program that has plagued physicians since 1990, many similarities to the Cambridge Analytica data-sharing scandal are appearing. The adhesion contract that forms the basis for MOC and is increasingly tied to physician hospital privileges and insurance reimbursements, assures this data pipeline remains open:
I also understand that ABIM may use my examination performance, training program evaluations, self evaluations of knowledge and practice assessment, and other information for research purposes, including collaboration with other research investigators and scientific publications."Unbeknownst to most physicians, the ABMS has been involved with the sale and sharing of physicians' demographic and sensitive MOC data with third parties for years. Each clinical physician in the United States may see 2000-3000 patient's each annually. Marrying physician data with their patient's data and targeting patient markets becomes possible with physician-specific MOC information. Procedural and pharmaceutical data allows medical suppliers, pharmaceutical companies, device companies, and others virtually unlimited opportunities to sell their products while optimizing most their bottom lines through increased sales and offering rebates to health care facilities (aka, kickbacks).
Group purchase organizations (GPOs) and Pharmacy Benefit Managers (PBMs) decide what equipment appears on a database for hospitals to purchase. Companies pay those GPOs and PBMs to be on the list. Doctors' equipment choices and pharmaceutical preferences influence that list. Companies want to know what doctors are using and who doctors are seeing. By knowing their patterns and knowing the procedures performed on patients, highly sensitive patient information can be deduced. Registries owned by procedurally-heavy specialty societies (like the American College of Cardiology) are a particularly ripe source of procedural data, particularly when it can be made doctor-specific (where MOC comes in). More data sales occur. Repeated MOC testing and demographic data entries required by physicians assures these physician-specific databases are kept current. Having the President and CEO of the American Board of Internal Medicine on the President's Council of Advisors for Science and Technology assured uninterrupted marketing access to physicians and their patients.
By using physician information and their patient care information for these corporate purposes, the ABMS/ABIM MOC® product looks more like Cambridge Analytica than a physician education tool and affects far more people's health care than the Cambride Analytica ever did.
So how how do all these organizations coordinate and connect their MOC data, registries, and corporate databases?
Through a virtually undisclosed tax-exempt AMA-funded private foundation shamelessly called the Physician Consortium for Performance Improvement (PCPI).
Reportedly formed in 2000 with the help of the AMA, the PCPI Foundation is located just blocks away from the AMA's corporate headquarters in downtown Chicago. The organization describes itself as follows:
The AMA-convened PCPI, in partnership with its members, has developed more than 350 measures, many of which are used in the Physician Quality Reporting System (PQRS) and Meaningful Use, as well as private health plan payment models. (emphasis mine)Not surprisingly, it's Board of Directors is lead by John S. McIntyre, MD of the American Psychiatric Association, who has never participated in MOC and is not required to do so:
In 2011, American Medical Association staff to the PCPI worked with a group of committed volunteer leaders to launch the NQRN®, a national, multi-stakeholder network of clinical registry stewards and others interested in registries. The NQRN has created tools and educational opportunities and increased the visibility and value of clinical registries as reporting and improvement systems. In 2016 NQRN was merged into the PCPI as a key program. In 2013, the AMA-convened PCPI launched the PCPI Quality Improvement Program to support its members improvement needs beyond measurement.
In 2014, the AMA and AMA-convened PCPI leadership undertook an evaluation to determine the optimal governance structure to meet the growing demand for value-based health care. The result of this evaluation was the adoption of new By-Laws in June 2015, which set the course for the PCPI Foundation (PCPI), an independent organization with an expanded membership.
The remainder of the Board of Directors include:
- Thomas Granatir, MD, Senior Vice President for Policy and "External Relations" of the ABMS (formerly from Humana)
- Lewis G. Sandy MD, FACP of the UnitedHealth Group
- Non-physician Nancy E. Lundebjerg, MPA of the American Geriatric Society (Vice Chair)
- Non-physician Laura J. Cranston, RPh of the Pharmacy Quality Alliance (Secretary)
- Non-physician Dianne V. Jewell PT, DPT, PhD, FAPTA of the American Physical Therapy Association (Treasurer)
- Larry A. Allen, MD, MHS of the American Heart Association
- Bruce S. Auerbach MD, FAECP of the American College of Emergency Physicians
- Arlene S. Bierman MD, MS of the Agency for Healthcare Research and Quality
- Claire Bradley, MD, MPH who oversees "Quality Improvement"
- Non-physician Carol A Cronin MA, MSW of the Informed Patient Institute
- Non-physician Melissa Danforth of the Leapfrog Group
- E. Scott Ferguson, MD - A radiologist on the AMA Board of Trustees and AMA representative to the National Quality Forum but does not appear to participate in MOC.
- Deeraj Mahajan, MD FACP, CMD, CIC, CHCQM ("Certified Medical Doctor, Certified Infection Control, Certified Health Care Quality Measures") of the Medical Specialty
- Lawyer Melanie G. Phelps JD of the North Carolina Medical Society who previously worked in the Government Affairs Department of Blue Cross Blue Shield
- Non-physician Aisha T. Pittman MPH of Premier, Inc, the largest hospital Group Purchase Organization
- Amir Qaseem MD, PhD, MHA, FACP of the American College of Physicians
- Martha J. Radford, MD FACC, FAHA of the American College of Cardiology
- David Shahian MD of the Society of Thoracic Surgeons
- Computer Scientist Kurt Skifstad, PhD CEO of ArborMetrix, a data analytics company
- Sandra Adamson Fryhofer, MD MACP from the Board of Trustees of the AMA
- Richard D. Zorowitz MD, FAAPMR of the American Academy of Physician Medicine and Rehabilitation
Members get to "access the latest tools and insights on performance measurement, clinical registries, and quality improvement" as well as "influence through representation on the PCPI board, committees, advisory and other, as well as expert panels and task forces."
Members of this organization, according to the revolving banner on the PCPI website, include:
AvaMed, FigMD (MOC data collectors), AMA, ACP, ACC, ABMS, Informed Patient Institute, CMSS, Am Society of Clinical Oncology, The American Health Quality Association, Am College of Occupational Medicine, Primaris (A healthcare consulting and data abstraction company), American Academy Foot and Ankle Orthopedics Society, UnitedHealth Group (Market cap: $262B), The Society of Thoracic Surgeons, Pharmacy Quality Alliance, American Gastroenterology Association, Health Care Services Platform, American Optometric Association, Academy of Nutrition and Dietetics, American Heart Association, American College of Radiology, and on, and on...
It's handsomely paid CEO and Executive Director, Kevin Donnelly, is a non-physician, too. Here's their latest 2017 IRS filing that confirms a cool $2.78M contribution from the AMA to the PCPI and contains this explanation why the organization is not a true public "charity" after all:
The organization is filing this 990PF after the extended due date of November 15, 2018 (extension was for Form 990). Upon completion of schedule it was determined that the public support test had not been met for the second year. Research into IRS code and regulations was done to determine the next steps, which took the organization past the due date. The organization did not intentionally disregard the filing requirement, but rather, took time to ensure that that (sic) the appropriate filings were being made. Going forward, now that the requirements are understood, all 990PF filings will be timely. Additionally the organization properly extended the 2018 return as fling a Form 990PF.I'm sensing some BS here, but I'll leave that to my readers (and the IRS) to decide.
Are UnitedHealth, Humana, Blue Cross Blue Shield, Premier, AvaMed (and all the medical device companies they represent), FigMD, and Primaris really about "quality" or their own bottom line?
Is there any wonder, then, that when a physician points out certain conflicts to medical editors of the Journal of the American Medical Association (JAMA) or the New England Journal of Medicine (owned by the Massachusetts Medical Society), he can't get a straight answer and is referred by the conflicted party to IRS tax filings?
One thing's for sure, to the best of my knowledge and belief, these multiple organizations are colluding with each other for their own best interests ("covert rationing" - a concept coined by the prescient Dr. Richard Fogoros) and using our physician MOC® data to drive their bottom lines while hiding behind non-profit tax law and the ruse of assuring the public it's all in the name of "quality."
-Wes
Wednesday, October 30, 2019
What Gives?
WHAT GIVES the American Board of Internal Medicine the ability to take away years of schooling, mountains of prior testing, sleepless nights of residency, and months of study for initial Board certification that we all had to pass?
WHAT GIVES the American Board of Internal Medicine the authority to magically un-certify physicians for not purchasing or their Maintenance of Certification program?
WHAT GIVES the American Board of Internal Medicine the right to take away over 25 years of my expertise with catheter ablation or pacemaker implantation when they've never once examined the quality of my work or spoken with my patients?
WHAT GIVES the American Board of Internal Medicine the right to tell insurance companies and hospitals when my board certification expires so those companies can suddenly refuse to issue payments or revoke my hospital privileges claiming by skills as a physician have expired?
The American Board of Internal Medicine says it is developing new strategies of physician testing in the name of improved patient care, but WHAT GIVES for those physicians it has de-certified and are now jobless?
Removing physicians with years of patient care experience because they refuse to pay a fee or perform needless computer tasks is not in the best interest of patient safety or quality of care.
So WHAT GIVES?
-Wes
PS: Please help support the legal efforts underway to end Maintenance of Certification for all subspecialties by contributing to at https://www.gofundme.com/practicing-physicians-of-america
(Every dollar helps. Please share this video with your colleagues, too.)
Friday, October 25, 2019
A Case Study in the Wrong Way to Fix Clinician Burnout
Asking the system to fix the system in regards to physician and nursing burnout is like asking the fox to watch the henhouse.
They have no clue.
Case in point: the recent article published online before print in the Journal of the American Medical Association (JAMA) (where else?) preaching a "systems-based approach to clinician well-being and provide better patient care."
What "system" is recommending this "approach? None other than the Accreditation Council for Graduate Medical Education comprised of the American Medical Association (AMA), the American Hospital Association (AHA), and the American Board of Medical Specialties (ABMS), among others, with work performed by a committee comprised of friends from Blue Cross Blue Shield.
Most concerning, however, is this report was co-authored by one of the most conflicted authors in the health care business, Christine K. Cassel, MD. Recall that Dr. Cassel failed to disclose her board seats (and income) with Kaiser Hospitals and Health Systems and Premier (the largest health care Group Purchase Organization for the nation's hospitals) while serving as President and CEO of the American Board of Internal Medicine.
Christine K. Cassel, MD was President and CEO of the ABIM from 2004-2014. During her tenure at the ABIM, Dr. Cassel received a highly influential political appointment on the President's Council of Advisors for Science and Technology under President Obama in April 2009, just before the Affordable Care Act was signed into law in 2010.
The same day she announced that political appointment, the ABIM contracted with Washington lobbying firm Jennings Policy Strategies, Inc. yet never publicly disclosed this relationship. Instead, ABIM tax forms from 2010 listed this firm as hired for "consulting services." It appears to this lay physician that these "services" were in direct violation of IRS regulations concerning lobbying, especially given Dr. Cassel's substantial non-disclosed financial ties to Premier, Inc., one of the nation's largest Group Purchase Organizations for the nation's hospitals. At least one other lobbying firm was retained by ABIM (named Mehlman Castagnetti Rosen Bingel and Thomas, Inc.) until June 30, 2015, and this relationship was never publicly disclosed to ABIM's physician diplomates, the IRS, or the public either.
According to a Newsweek reporter, the ABIM used obfuscatory accounting techniques during and after Dr. Cassel's tenure: "I had an easier time figuring out the compensation of officials at Enron, WorldCom and Adelphia—all famous for lying on financial filings—than I did for those at the ABIM, where enormous effort seems to have been taken to make murky what should be crystal clear." The ABIM reportedly paid Dr. Cassel $1.7 million in her final year.
Some things never change: Dr. Cassel once again claimed "no conflicts" in the disclosures to this most recent JAMA article on physician burnout either.
Gaslighting physicians and nurses is not the way to fix burnout.
It would be far better for the members of the ACGME to hold a mirror before themselves to understand how their conflicts of interest have systematically done more to harm our profession over the years. Our current house of Medicine has gleefully created the world's most expensive typing pool with physicians and nurses as little more than data entry clerks clicking away whether home or at work. Our current non-transparent health care system has evolved this way thanks in large part to the AMA's behind-the-scenes business model dependent on licensing its ever-changing "Current Procedural Terminology" (CPT) codes for use by the electronic medical record companies and insurance companies to covertly ration care. At the same time, the ACGME supported and promoted the transition from lifetime ABMS board certification to an unproven and wasteful "continuous board certification" by insisting on lifetime testing and payments from physicians for themselves, the lucrative publishing and testing industries, and a vast network of physician specialty societies without ever examining the harms this extortion has caused physicians and the patients they care for. It is telling there was no mention in the recent JAMA article of the "Maintenance of Certification" (MOC) controversy that has led to multiple ongoing federal class action antitrust and racketeering lawsuits, deprives physicians of personal and family time, and steals any semblance of self-educational autonomy from physicians for the benefit of the ACGME members and their collaborators.
To fix burnout we need doctors and nurses looking up at patients rather than looking down at computer screens. We don't need hand-holding wellness exercises, life coaches, and yoga classes. We especially dont need them right after witnessing the unfortunate death of a child or having a patient die beneath our hands despite our best efforts.
Doctors and nurses are not babies or widgets in an assembly line.We entered into this real-life drama of medicine with eyes wide open knowing full well that medicine and health care can be challenging. Yet much of corporate medicine has taken on its role to push our limits to make the system more "productive" for the system at the expense of its caregivers. Medicine is hard damn work that is both emotionally draining yet exhilarating all at the same time. We take the ultimate responsibility for our patients. The ACGME and their protected bureaucratic workshop do not. We risk falling prey to this exploitation if we fail to expose these many undisclosed conflicts of interest with the authors and "committee" wrote and published this paper in JAMA.
This is not to say I see a day where medicine will occur without the use of computers. But computers and secret sharing of data health care data can have its consequences if patients and physicians are kept in the dark. The depersonalization that computers bring to medicine has a nasty side effect on the care we provide: physicians and nurses need face-to-face, hand-to-hand, and heart-to-heart time with patients and their colleagues, not computers, procedure codes, and recommendations from people who foisted MOC upon us, stood to gain financially from it, but never participated in MOC themselves.
Distrust of our self-imposed corporate overlords is a large part of why we're where we are currently, particularly when they insult us with their self-serving "mission" to have physicians help themselves. What do these physician-bureaucrat posers know what's really happening on the front line of health care today?
Humility at admitting mistakes would go a lot further at curing physician burnout than beating the same corporate drum that wedges itself between what really matters: doctors and nurses caring for patients without the self-appointed, politically- and industry-funded National Academy of Medicine and their cronies telling us how to do our jobs. It would be far better if they took off the chains they bind us with and let us do what we do best.
-Wes
They have no clue.
Case in point: the recent article published online before print in the Journal of the American Medical Association (JAMA) (where else?) preaching a "systems-based approach to clinician well-being and provide better patient care."
What "system" is recommending this "approach? None other than the Accreditation Council for Graduate Medical Education comprised of the American Medical Association (AMA), the American Hospital Association (AHA), and the American Board of Medical Specialties (ABMS), among others, with work performed by a committee comprised of friends from Blue Cross Blue Shield.
Most concerning, however, is this report was co-authored by one of the most conflicted authors in the health care business, Christine K. Cassel, MD. Recall that Dr. Cassel failed to disclose her board seats (and income) with Kaiser Hospitals and Health Systems and Premier (the largest health care Group Purchase Organization for the nation's hospitals) while serving as President and CEO of the American Board of Internal Medicine.
Christine K. Cassel, MD was President and CEO of the ABIM from 2004-2014. During her tenure at the ABIM, Dr. Cassel received a highly influential political appointment on the President's Council of Advisors for Science and Technology under President Obama in April 2009, just before the Affordable Care Act was signed into law in 2010.
The same day she announced that political appointment, the ABIM contracted with Washington lobbying firm Jennings Policy Strategies, Inc. yet never publicly disclosed this relationship. Instead, ABIM tax forms from 2010 listed this firm as hired for "consulting services." It appears to this lay physician that these "services" were in direct violation of IRS regulations concerning lobbying, especially given Dr. Cassel's substantial non-disclosed financial ties to Premier, Inc., one of the nation's largest Group Purchase Organizations for the nation's hospitals. At least one other lobbying firm was retained by ABIM (named Mehlman Castagnetti Rosen Bingel and Thomas, Inc.) until June 30, 2015, and this relationship was never publicly disclosed to ABIM's physician diplomates, the IRS, or the public either.
According to a Newsweek reporter, the ABIM used obfuscatory accounting techniques during and after Dr. Cassel's tenure: "I had an easier time figuring out the compensation of officials at Enron, WorldCom and Adelphia—all famous for lying on financial filings—than I did for those at the ABIM, where enormous effort seems to have been taken to make murky what should be crystal clear." The ABIM reportedly paid Dr. Cassel $1.7 million in her final year.
Some things never change: Dr. Cassel once again claimed "no conflicts" in the disclosures to this most recent JAMA article on physician burnout either.
Gaslighting physicians and nurses is not the way to fix burnout.
It would be far better for the members of the ACGME to hold a mirror before themselves to understand how their conflicts of interest have systematically done more to harm our profession over the years. Our current house of Medicine has gleefully created the world's most expensive typing pool with physicians and nurses as little more than data entry clerks clicking away whether home or at work. Our current non-transparent health care system has evolved this way thanks in large part to the AMA's behind-the-scenes business model dependent on licensing its ever-changing "Current Procedural Terminology" (CPT) codes for use by the electronic medical record companies and insurance companies to covertly ration care. At the same time, the ACGME supported and promoted the transition from lifetime ABMS board certification to an unproven and wasteful "continuous board certification" by insisting on lifetime testing and payments from physicians for themselves, the lucrative publishing and testing industries, and a vast network of physician specialty societies without ever examining the harms this extortion has caused physicians and the patients they care for. It is telling there was no mention in the recent JAMA article of the "Maintenance of Certification" (MOC) controversy that has led to multiple ongoing federal class action antitrust and racketeering lawsuits, deprives physicians of personal and family time, and steals any semblance of self-educational autonomy from physicians for the benefit of the ACGME members and their collaborators.
To fix burnout we need doctors and nurses looking up at patients rather than looking down at computer screens. We don't need hand-holding wellness exercises, life coaches, and yoga classes. We especially dont need them right after witnessing the unfortunate death of a child or having a patient die beneath our hands despite our best efforts.
Doctors and nurses are not babies or widgets in an assembly line.We entered into this real-life drama of medicine with eyes wide open knowing full well that medicine and health care can be challenging. Yet much of corporate medicine has taken on its role to push our limits to make the system more "productive" for the system at the expense of its caregivers. Medicine is hard damn work that is both emotionally draining yet exhilarating all at the same time. We take the ultimate responsibility for our patients. The ACGME and their protected bureaucratic workshop do not. We risk falling prey to this exploitation if we fail to expose these many undisclosed conflicts of interest with the authors and "committee" wrote and published this paper in JAMA.
This is not to say I see a day where medicine will occur without the use of computers. But computers and secret sharing of data health care data can have its consequences if patients and physicians are kept in the dark. The depersonalization that computers bring to medicine has a nasty side effect on the care we provide: physicians and nurses need face-to-face, hand-to-hand, and heart-to-heart time with patients and their colleagues, not computers, procedure codes, and recommendations from people who foisted MOC upon us, stood to gain financially from it, but never participated in MOC themselves.
Distrust of our self-imposed corporate overlords is a large part of why we're where we are currently, particularly when they insult us with their self-serving "mission" to have physicians help themselves. What do these physician-bureaucrat posers know what's really happening on the front line of health care today?
Humility at admitting mistakes would go a lot further at curing physician burnout than beating the same corporate drum that wedges itself between what really matters: doctors and nurses caring for patients without the self-appointed, politically- and industry-funded National Academy of Medicine and their cronies telling us how to do our jobs. It would be far better if they took off the chains they bind us with and let us do what we do best.
-Wes
Saturday, October 12, 2019
Plaintiffs to Appeal ABIM Class-Action Lawsuit in Full
With the time to amend the earlier class action antitrust and racketeering lawsuit against the American Board of Internal Medicine (ABIM) past, this statement was issued by C. Phillip Curley, the Plaintiffs' lead attorney:
-Wes
Physicians wishing to support the plaintiffs in this unprecedented action are encouraged to contribute here.
“Plaintiffs plan to appeal in full the dismissal of their case. While we respect the district court, we believe it was wrong at this early stage of the litigation to dismiss Plaintiff’s case and deprive them of their day in court. Plaintiffs look forward to the vindication of their claims on appeal.”ABIM may have thought they won this case on dismissal, but it looks the plaintiffs' claims will get a second more critical review of the case with the 3rd Circuit Court of Appeals.
-Wes
Physicians wishing to support the plaintiffs in this unprecedented action are encouraged to contribute here.
Saturday, October 05, 2019
You Know There's a Problem with MOC When...
... yet another antitrust lawsuit is filed against ANOTHER American Board of Medical Specialties' member board. This time, the American Board of Orthopaedic Surgery joined the antitrust litigation fray on September 11, 2019.
Look for those Maintenance of Certification® (MOC®) fees to continue to skyrocket as the certification cartel extracts more fees from workingstiffs doctors to help pay their mounting legal bills.
-Wes
PS: Want to help with this David vs Goliath battle to help end MOC®? Click here.
Look for those Maintenance of Certification® (MOC®) fees to continue to skyrocket as the certification cartel extracts more fees from working
-Wes
PS: Want to help with this David vs Goliath battle to help end MOC®? Click here.
Wednesday, October 02, 2019
Why Working Physicians Deserve Their Day in Court
Ask any physician who shares 24-hour call with his colleagues: what time is the worst time to get called into the hospital? Most will tell you just before midnight.
That's because you miss out on those most precious first few hours of deep sleep needed for the next day.
For me, the call this particular evening came at 10:47 PM. Seventy-nine years old. Complete heart block. Wide complex escape rhythm at 34. Started to feel poorly early that morning. Stable blood pressure: 134/60.
A decision was needed.
So, I pulled my head off the pillow, glanced at the clock, grabbed by cellphone, and stumbled toward the other bedroom where the home computer rests. Giggling the mouse, the 45,000 watt screen light illuminated, blinding me as I struggled to type in the cellphone-derived time-sensitive passcode needed to log into EPIC alongside my username and password. I entered by username and password again (once is not enough, I guess), then found the particular hospital (I cover four at night when on call), then the Emergency Room patient list, then the room, and there it was: just as advertised, but with the dreaded one-triage note entry in the chart that basically just noted the time the patient arrived. That is the tell-tale sign that no real decision-making is needed for the ER staff. Just "call EP" (aka, me.)
The decision: pacemaker now or pacemaker later?
The mind does strange things with little sleep, but the decision at that time of night was mine and mine alone. No one else was there. No one else in medicine has this much responsibility. No nurse practitioner, medical administrator, or bureaucrat could make this call, but there I was: dead tired with my mind playing tricks on me. I would hear my inner-self rationalizing with the rapid-fire voices dancing in my head:
After a few hours sleep I woke, knowing I did the right thing. But reflecting back to that brief moment of decision-making the night before, I wondered to myself. Could things have gone differently?
Which brings me to the point of this blog post.
For the past five years, there has been tremendous uproar about the payments and unproven requirements of the Maintenance of (Board) Certification (MOC) mandate for US physicians created out of thin air by the American Board of Internal Medicine (ABIM) and marketed by the American Board of Medical Specialties (ABMS) to fund their bloated salaries, lobbying activities, and for-profit corporate subsidiaries that sell data. Thanks in part to the ACA law that includes the MOC mandate as a "quality" metric included by their lobbying, MOC's payments and needless exercises have became mandatory for employed physicians without their knowledge or consent. And with every passing day, the programs and exercises are promised to be easier, faster, less intrusive, because these bureaucrats continuously claim to know what's best for working physicians on the front-line of 24-hour patient care. They wallow in a sense of schadenfreude as they wield their undeserved power over their working colleagues, purposely naive to the most dangerous side effect their unwarranted and potentially illegal actions risk creating.
Longtime readers know that at least five different antitrust lawsuits have been filed against various non-profit entities that comprise the ABMS member boards in regards to MOC. The largest member board of that consortium is the ABIM, who recently breathed a partial sigh of relief when a Pennsylvania judge dismissed most of the claims of anti-trust tying, monopolization, racketeering, fraud, and unjust enrichment brought by four working internists. While the monopolization, fraud, and racketeering claims remain unresolved at this time, we should note that there might be significant consequences if working physicians don't get their day in court, and it's not what most people expect.
Not having an unbiased judgement in court before a jury of one's peers in these untested legal waters risks the development of US physician apathy.
Too many examples of lying, cheating, and stealing physicians' certification fees for political and economic purposes have occurred since MOC was mandated by the ABMS member boards in 1990. From the quiet movement of nearly $70 million from the ABIM to the secretly created ABIM Foundation from 1990-2007 in the name of "Choosing Wisely," the falsification of tax forms, holding political and corporate appointments while serving as the President and CEO of the ABIM, performing undisclosed lobbying, transferring funds to the Cayman Islands, and using felonious strongmen to invade doctors' houses with Federal Marshals and lawyers, were all accomplished just so their monopoly and partnership with insurers, hospitals, and medical specialty societies could flourish. By quashing the chance for justice against these actions, the courts risk irreparably damaging the integrity of the entire US medical profession and crushing the souls of those who make huge sacrifices on behalf of their patients every day.
This whole ABMS MOC fiasco, especially with the recent opinion to dismiss doctors claims of impropriety against this racket of monied tax-exempt corporations so broadly, risks making doctors apathetic. Could such apathy lead to less-than ideal decision-making in the wee hours of the morning?
I wonder.
For the sake of our profession and our patients, it's time to make sure working physicians get their day in court.
-Wes
That's because you miss out on those most precious first few hours of deep sleep needed for the next day.
For me, the call this particular evening came at 10:47 PM. Seventy-nine years old. Complete heart block. Wide complex escape rhythm at 34. Started to feel poorly early that morning. Stable blood pressure: 134/60.
A decision was needed.
So, I pulled my head off the pillow, glanced at the clock, grabbed by cellphone, and stumbled toward the other bedroom where the home computer rests. Giggling the mouse, the 45,000 watt screen light illuminated, blinding me as I struggled to type in the cellphone-derived time-sensitive passcode needed to log into EPIC alongside my username and password. I entered by username and password again (once is not enough, I guess), then found the particular hospital (I cover four at night when on call), then the Emergency Room patient list, then the room, and there it was: just as advertised, but with the dreaded one-triage note entry in the chart that basically just noted the time the patient arrived. That is the tell-tale sign that no real decision-making is needed for the ER staff. Just "call EP" (aka, me.)
The decision: pacemaker now or pacemaker later?
The mind does strange things with little sleep, but the decision at that time of night was mine and mine alone. No one else was there. No one else in medicine has this much responsibility. No nurse practitioner, medical administrator, or bureaucrat could make this call, but there I was: dead tired with my mind playing tricks on me. I would hear my inner-self rationalizing with the rapid-fire voices dancing in my head:
"Really, now?" ("Yeah, now")So the pacemaker representative and the rest of the team were called as I drove to see the patient (none are happy, but they understood). I placed a temporary pacing wire for backup (thank goodness), implanted the pacemaker, spoke with the grateful family, then drove home for my head to finally meet my lonely pillow at 2 AM. Thankfully without another interruption that morning.
"His blood pressure is stable, and the ER doctor says he looks fine, maybe this can wait until the morning?" (But that nice escape rhythm could quit, the pacer pads might not work, and you'll have to scramble those 10 miles up the road to make it in time.")
"The rep on call lives far away." (Too bad.)
"The staff will be spent, too. They are overstretched and need their sleep." (But this is why we're on call.)
"Maybe just a temp wire, then pacer in the morning daylight hours? (I have to drive there anyway. The temp wire might dislodge, then the patient has NO rhythm... )
"Dude, just do it. It'll save time in the long run and let you sleep without worrying."
After a few hours sleep I woke, knowing I did the right thing. But reflecting back to that brief moment of decision-making the night before, I wondered to myself. Could things have gone differently?
Which brings me to the point of this blog post.
For the past five years, there has been tremendous uproar about the payments and unproven requirements of the Maintenance of (Board) Certification (MOC) mandate for US physicians created out of thin air by the American Board of Internal Medicine (ABIM) and marketed by the American Board of Medical Specialties (ABMS) to fund their bloated salaries, lobbying activities, and for-profit corporate subsidiaries that sell data. Thanks in part to the ACA law that includes the MOC mandate as a "quality" metric included by their lobbying, MOC's payments and needless exercises have became mandatory for employed physicians without their knowledge or consent. And with every passing day, the programs and exercises are promised to be easier, faster, less intrusive, because these bureaucrats continuously claim to know what's best for working physicians on the front-line of 24-hour patient care. They wallow in a sense of schadenfreude as they wield their undeserved power over their working colleagues, purposely naive to the most dangerous side effect their unwarranted and potentially illegal actions risk creating.
Longtime readers know that at least five different antitrust lawsuits have been filed against various non-profit entities that comprise the ABMS member boards in regards to MOC. The largest member board of that consortium is the ABIM, who recently breathed a partial sigh of relief when a Pennsylvania judge dismissed most of the claims of anti-trust tying, monopolization, racketeering, fraud, and unjust enrichment brought by four working internists. While the monopolization, fraud, and racketeering claims remain unresolved at this time, we should note that there might be significant consequences if working physicians don't get their day in court, and it's not what most people expect.
Not having an unbiased judgement in court before a jury of one's peers in these untested legal waters risks the development of US physician apathy.
Too many examples of lying, cheating, and stealing physicians' certification fees for political and economic purposes have occurred since MOC was mandated by the ABMS member boards in 1990. From the quiet movement of nearly $70 million from the ABIM to the secretly created ABIM Foundation from 1990-2007 in the name of "Choosing Wisely," the falsification of tax forms, holding political and corporate appointments while serving as the President and CEO of the ABIM, performing undisclosed lobbying, transferring funds to the Cayman Islands, and using felonious strongmen to invade doctors' houses with Federal Marshals and lawyers, were all accomplished just so their monopoly and partnership with insurers, hospitals, and medical specialty societies could flourish. By quashing the chance for justice against these actions, the courts risk irreparably damaging the integrity of the entire US medical profession and crushing the souls of those who make huge sacrifices on behalf of their patients every day.
This whole ABMS MOC fiasco, especially with the recent opinion to dismiss doctors claims of impropriety against this racket of monied tax-exempt corporations so broadly, risks making doctors apathetic. Could such apathy lead to less-than ideal decision-making in the wee hours of the morning?
I wonder.
For the sake of our profession and our patients, it's time to make sure working physicians get their day in court.
-Wes
Sunday, September 29, 2019
Some Thoughts on the Recent ABIM Lawsuit Ruling
Nothing is going to get better. It's not.”
― Dr. Seuss, The Lorax
After researching, investigating, and writing about the activities and finances of the American Board of Internal Medicine (ABIM) and the ABIM Foundation for the past five years, it would figure that a ruling on the class-action lawsuit challenging the ABIM Maintenance of Certification (MOC) program would occur during the week that I am on call. I simply have not had much time to put my thoughts in writing.
Perhaps that's a good thing.
But as the time has passed since the ruling, I believe I have more clarity now.
Initially, I must say I was surprised by Judge Kelly's ruling, but not shocked. We have encountered significant naiveté with non-physician legislators when attempting to pass anti-MOC legislation at the state legislative level. Most non-physicians do not have a clue what ABIM Board Certification and MOC are, let alone their history and current relationship to obtaining and maintaining physician hospital credentials and insurance payments.
I suspect the judge in the ABIM antitrust case was (and remains) similarly naive. (Just as I am naive about what it takes to be a lawyer or judge.) Perhaps nowhere is this naiveté more evident than the judge's paragraph concerning "grandfathering" of older physicians:
"Finally, Plaintiffs allege that ABIM does not consider MOC to be a requirement of initial certification because it has “grandfathered” those that purchased a lifetime certification prior to 1990. (Pls.’ Mem. Law in Opp’n Mot. to Dismiss 13.) However, Plaintiffs provide no support as to why ABIM should not be allowed to modify its certification process over time. We see no problem that at some point ABIM realized there was a need to have its certified internists undergo an MOC program, whether because the internists could not keep up with the advances in their particular field, saw their skills diminish, or any other reason. In fact, the need to require a MOC program is highlighted in this case, as Murray initially failed her infectious disease MOC program in 2009 and Joshua was unable to pass her required MOC program in 2014. (Am. Compl. ¶¶ 85, 109.)"But the judge's logic falls apart here because he mentions only the plaintiffs' need to "keep up," and not the "grandfathers'" similar "need." Aren't older, grandfathered physicians who do not have to participate in MOC more likely to have "failed to keep up with the advances in their field or seen their skills diminish?" Why are they granted an ABIM board certification "hall pass" while the younger Plaintiffs in this case were not? Why is such an age- and gender-discriminatory double standard acceptable for board certification in the judges eyes? (Remember, younger physicians who must perform MOC are increasingly comprised of females and physicians of color.)
Would the judge feel similarly if he had to retake his bar examination and pay monopolistic fees to the Bar Association every 2-10 years to maintain his appointment to the bench?
Concerning the unjust enrichment dismissal, the judge makes a similar blunder and fails to even consider the Plaintiffs' concerns:
"Our analysis is again constrained by Plaintiffs’ misunderstanding of the product they purchased. Clearly, the first two elements of unjust enrichment are met for Plaintiffs that purchased MOC. However, the third element is not met because it is not inequitable for ABIM to keep the benefit since it did not “force” Plaintiffs to purchase MOC.(emphasis mine) Plaintiffs were, of course, free to decide to no longer be certified by ABIM and to, therefore, not purchase MOC."The Plaintiffs in this case were free to decide that they did not need to purchase MOC just as they are free to decide to stop breathing. How long could the Plaintiff internists earn a living and work as internists if they cannot hold hospital privileges or receive insurance payments unless they purchase MOC?
This judges' entire ruling in favor of ABIM seems thin to me.
I look forward to seeing where the next chapter of this ongoing legal battle takes us in the weeks and months ahead.
-Wes
It is important to realize this case is far from over as the legal battle against MOC continues. Please help the Plaintiffs' efforts to end MOC by contributing here.
Friday, September 27, 2019
Federal Judge Dismisses MOC Class-Action Lawsuit, For Now
On 26 September 2019, a Pennsylvania judge has dismissed the current claims filed by the four internists challenging ABIM’s Maintenance of Certification (MOC) program (The full opinion here). The judge, however, has invited the plaintiffs to file amended claims on the monopolization and racketeering claims in the lawsuit in the next 14 days and, in contrast to what the ABIM said in their public statement, the case is far from over. Even if the plaintiffs are ultimately unsuccessful at the trial court level, all available appeals will be pursued.
No one ever thought this would be an easy fight - it is a David vs. Goliath effort after all - we remain committed to do whatever we can to bring an end to MOC.
-Wes
No one ever thought this would be an easy fight - it is a David vs. Goliath effort after all - we remain committed to do whatever we can to bring an end to MOC.
-Wes
Tuesday, September 24, 2019
ABMS's Vision: Doubling Down on MOC
Since the American Board of Medical Specialties' (ABMS) "Vision Commission" issued its corporate white-paper "final report," it has become abundantly clear that the American Board of Medical Specialties (ABMS), medical subspecialty societies, and the entire Accreditation Council for Graduate Medical Education (AAMC, AMA, AHA, etc), have no intention of ending mandated re-certification requirements for US physician or osteopaths (also known as Maintenance of Certification (MOC), Continuous Certification, Maintenance of Certification in AnesthesiologyTM (MOCA®), ConCert™, or OCC).
Instead, they are doubling down.
One only has to look at the list of sponsors at this week's 2019 ABMS Conference here in Chicago to understand why.
Their "Premium Sponsor?" Certemy.com - a VC-funded startup from San Francisco infused with a cool $3 million investment run by a venture capitalist and Kaiser Permanente urologist eager to capitalize on the lucrative credentialing business. Or how about this ironically-named company in the ABMS co-branding line-up: MOCingbird that reminds you when all your lifelong credentialing paperwork and payments must be completed?
The data-selling opportunities are endless!
Might the for-profit ABMS-subsidiary ABMS Solutions, LLC provide Certemy.com, MOCingbird, and a whole host of other business middlemen the personal information, NPI numbers, addresses, cell-phone numbers, emails, MOC expiration dates, and test scores of physician, parsed psychometrically-designed test questions to insurers, hospitals, and anyone else who wants to hold physicians hostage for their financial purposes?
When you control a monopoly, anything's possible - especially when physicians are forced to "sign" an adhesion contract while paying for and enrolling in MOC as a condition of remaining employed.
From ABMS's own website, a dark, physician data deep-state has evolved:
Given this ABMS corporate line-up and their self-serving focus demonstrated so clearly by their "conference," the intent of ABMS "continuous certification" is obvious.
It's time to put an end to this computerized madness masquerading as "physician improvement" because this MOC game that ABMS has doubled down on is getting utterly ridiculous.
-Wes
Instead, they are doubling down.
One only has to look at the list of sponsors at this week's 2019 ABMS Conference here in Chicago to understand why.
Their "Premium Sponsor?" Certemy.com - a VC-funded startup from San Francisco infused with a cool $3 million investment run by a venture capitalist and Kaiser Permanente urologist eager to capitalize on the lucrative credentialing business. Or how about this ironically-named company in the ABMS co-branding line-up: MOCingbird that reminds you when all your lifelong credentialing paperwork and payments must be completed?
The data-selling opportunities are endless!
Might the for-profit ABMS-subsidiary ABMS Solutions, LLC provide Certemy.com, MOCingbird, and a whole host of other business middlemen the personal information, NPI numbers, addresses, cell-phone numbers, emails, MOC expiration dates, and test scores of physician, parsed psychometrically-designed test questions to insurers, hospitals, and anyone else who wants to hold physicians hostage for their financial purposes?
When you control a monopoly, anything's possible - especially when physicians are forced to "sign" an adhesion contract while paying for and enrolling in MOC as a condition of remaining employed.
From ABMS's own website, a dark, physician data deep-state has evolved:
The world of the ABMS "continuous certification" monopoly is not only Orwellian, it's just plain creepy. Is this monopoly about lifelong physician continuing education or lifelong physician manipulation?
- An exhibit hall representing innovators in areas of assessment, test development and administration, data collection and measurement, and more.
- Organizations can use data to better monitor and guide physicians’ work, trigger point-of-care decision making, and assess the impact of physicians’ improvement activities. In this session, the presenters will share how they identify the correct data and the appropriate source(s) of data and will discuss how data can be used to improve clinical decision making.
- Discuss how data can be used at the point of care to improve clinical decision making
- Psychometric analysis to create legally defensible exams
Given this ABMS corporate line-up and their self-serving focus demonstrated so clearly by their "conference," the intent of ABMS "continuous certification" is obvious.
It's time to put an end to this computerized madness masquerading as "physician improvement" because this MOC game that ABMS has doubled down on is getting utterly ridiculous.
-Wes
Sunday, September 22, 2019
How ABIM's MOC Product Ends Physician Careers
From Medical Economics:
Except physicians like Dr. Lopatin. Dr. Lopatin demonstrates something that MOC and all those costly pushed quizzes to our mobile phones will never be able to test...
... leadership and integrity.
Thanks, Mark.
Here's hoping others will follow your lead.
-Wes
Mark Lopatin, MD, has been a vocal opponent of ABIM’s MOC process for several years, but says that these new options are similar to changes he’d like to see in his subspecialty of rheumatology. His 1986 board certification in internal medicine is still considered valid, even though he hasn’t practiced in the field for 30 years, he says. But because rheumatology boards were not available in 1989, he took and passed the exam in 1990—one year too late to achieve grandfathered status—and has gone through the MOC process every 10 years since. He won’t be taking a fourth exam in 2020, however. “To take rheumatology boards means that I have to spend about three months preparing—at least three months—studying rote memorization of facts, esoteric stuff, trivial pursuit kinds of stuff that is not relevant to what I do on a day in, day out basis,” he says. “I’ll be 63 years old at that time, so if I took it and retired at 65, it buys me another year or two. It’s not worth it.”MOC and these subspecialty "continuous certification" products are (and always were) about financial coercion, strongman threats, false claims, monopoly-making and deception. Medicine has no place for these things. Unfortunately, only a small percentage of doctors have donated to help end the MOC product's threat to a physicians hard-earned right to work.
While pleased to see ABIM collaborating with medical societies in some subspecialties, Lopatin says the testing component is still fundamentally flawed. “They’re still focused on that high-stress, timed exam that needs to be passed. What really needs to be measured is due diligence,” he says.
And despite his impending exit from medicine, Lopatin has already donated twice to PPA’s GoFundMe campaign. “I’ve been very outspoken about this, and this is my chance to put my money where my mouth is,” he says. “I am stopping my career because of this. To me, that’s a pretty strong statement about how I feel about what ABIM has done and is doing.”
Except physicians like Dr. Lopatin. Dr. Lopatin demonstrates something that MOC and all those costly pushed quizzes to our mobile phones will never be able to test...
... leadership and integrity.
Thanks, Mark.
Here's hoping others will follow your lead.
-Wes
Friday, September 20, 2019
When the Whole is Greater Than the Sum of Its Parts
- Aristole
Since May 2018, over 1,600 physicians have made over 1900 contributions to our GoFundMe effort in support of physician plaintiffs involved in three class action antitrust lawsuits against the American Board of Internal Medicine (ABIM), the American Board of Radiology (ABR), and the American Board of Psychiatry and Neurology (ABPN). Details on those lawsuits can be found elsewhere on this blog.
Over the past months, I have watched us approach our funding goal for this effort bit by bit, as more and more physicians learn of the lawsuits and this work to help our working colleagues.
I recently completed an original 18" x 24" (acrylic) painting (with a hat tip to Chuck Close) celebrating this group effort by physicians. Up close, it doesn't look like much:
But viewed from farther away, the whole looks very different than those individual parts:
There is strength in numbers.
I just received a batch of full sized (18" x 24") limited-edition high-quality professional giclees of this artwork printed on heavy canvas paper that I will offer to $1000 donors to our GoFundMe campaign until we meet our funding goal, signed by yours truly. Just send me me the shipping address via the GoFundMe sight email after a donation is made if you'd like one and I'll be sure to send one on.
-Wes
Thursday, September 19, 2019
Plaintiff Lawyer Explains ABMS Medical Board Lawsuits
This past Saturday, A Zoom video conference sponsored by Citizen Health.io was held with the members of Practicing Physicians of America's (PPA) board and an invited speaker, Laura Feldman, one of the plaintiff attorneys with Robinson Curley, P.C. - the law firm that has brought suits against several American Board of Medical Specialty (ABMS) member boards. For my reader's convenience, I took the liberty of transcribing the first portion of the conversation that explained the ABMS Maintenance of Certification(MOC) antitrust lawsuits underway and their status. The transcription begins at approximately 06:12 of the video and participants at this point include myself (WF), Judith Thompson, MD (JT - President and Chairman of the PPA's board), and Laura Feldman (LF):
I hope this has been informative and will continue to update my readers with the status of these suits as information on them comes available. If you find these efforts useful, please consider contributing what ever you can to the voluntary GoFundMe page in support of the plaintiffs. Hopefully together we can end MOC's stranglehold on working physicians nationwide.
Thanks-
-Wes
WF: Awesome, Well I think many of the people who have joined PPA or been involved with the Maintenance of Certification (MOC) process have realized there’s a lot of problems with it. We have problems that we now think may have been illegal and as a result of that, some physicians have been harmed through this process. For that reason, a number of physicians ultimately filed suit in December, 2018 against the American Board of Internal Medicine (ABIM).An extensive question and answer session was held later in the video conference where viewers could post questions, and can be found at about 27:10 and contains additional valuable insights about MOC and the litigation underway.
That suit is a very complicated and far-reaching lawsuit and we’ve been fortunate enough to have Laura Feldman from Robinson Curley, the law firm that brought the suit…
JT: Wes? Wes? I hate to interrupt you for a minute. Listeners, please verify that your device is on mute. There is apparently background noise that’s interfering with other peoples’ ability to hear. Thank you, Wes.
WF: Yeah, no worries. So anyway, in December of 2018, four internists filed suit against the American Board of Internal Medicine and the basis of the suit were two allegations, main allegations anyway. It is a “class action lawsuit,” and it involves antitrust issues and racketeering issues. I thought it would be smart since most physician don’t know what these things are, to invite Laura to give us a quick, brief rundown what “antitrust” and the RICO portions of this lawsuit mean so that maybe we could have a better understanding before we go into more detail.
LF:Absolutely, so Dr. Wes thank you so much for the invitation and for including me in this group. I am delighted to be here and really delighted to be a piece of this litigation.
As Dr. Wes mentioned, the first suit challenging MOC was brought against ABIM. And it is a class action – an opt-out class action – and what that means is that any physician whether a DO or MD that has been forced to purchase MOC to maintain their initial certification is part of the class unless he or she chooses to opt out. There’s a couple of exceptions: if you’re related to the judge or affiliated with one of the boards, you’re not going to be part of the class – but otherwise you’re in the class unless you chose to withdraw.
Subsequent to the ABIM lawsuit, two plaintiffs filed suit against the ABPN which is the Psychiatry and Neurology board, … (smiling) Dr. Dixon is excited…, and one radiologist filed suit against the American Board of Radiology and we, along with our co-council, are the attorneys challenging those boards’ MOC programs. So over the next couple of minutes I’ll be brief. I’ll go over the Complaints, what’s happened so far in the suits, and the next steps in the litigation.
So as Dr. Wes mentioned, our main plaintiffs brought claims of anititrust violations and also unjust enrichment. And then against the ABIM, there’s also a racketeering claim.
So first, antitrust. So the main plaintiffs in the litigation accused the three boards , ABIM, ABPN, ABR, of illegally tying the initial certification product to the continuing, the MOC certification product. And what they’re alleging is that doctors are forced to purchase MOC and jump through all the hoops that MOC requires – its not just handing out some money – they’re forced to purchase MOC to order to maintain their underlying certification that they purchased. No in addition to this antitrust claim that is a tying claim, they’re also bring up a monopoly claim, alleging that these three boards have illegally created and maintained a monopoly power in the MOC marketplace stymying the efforts of competition like NBPAS (National Board of Physicians and Surgeons) and making it so that any other competition can’t enter the marketplace.
Now each of the three suits brings a state common law which is called “unjust enrichment” accusing the boards of unjustly enriching themselves at the expense of doctors like you. I mean, taking money off of your backs and unjustly enriching themselves.
Now racketeering, or the RICO claim, against ABIM is stating that ABIM waged a campaign to deceive the public about MOC’s benefits. So you’ve heard about their allegations if its benefits to physicians and to patients and to the public as a whole, and part of that racketeering claim is their inappropriate campaign to suggest that MOC constitutes "self-regulation." I know it’s a big buzzword. The complaint alleges ABIM misrepresented what passing MOC actually shows: the tests’ ability to actually demonstrate doctors’ qualifications or their lack thereof.
So those suits have been filed, we’re in litigation mode. Each defendant has filed a Motion to Dismiss, and those motions are fully briefed. What that means is that we have submitted to the Court our opposition to get rid of the suits and those briefs are pending before the three respective courts and we’re waiting for all three of those courts to decide whether or not to dismiss the lawsuits. We feel like we’re filed really strong briefs. You can read them online if you’d like at ABIMlawsuit.com, ABPNlawsut.com, or ABRlawsuit.com. So that’s where we are in the litigation. We’re waiting for them. We expect it could take several more months and in the meantime, we are preparing for discovery, which is the phase of litigation where you share information – we’ll be seeking information from the board and third parties and they’ll be seeking information from us. So sit tight.
WF: Let me ask a quick question if I may. What do you think the timeline is to get a decision on any of these lawsuits?
LF: Good question. We wish we knew, litigation is like a lot of hurrying up and waiting, so we’re busy, busy, busy, then we wait. They we’re busy, busy, busy, then we wait some more. We expect ABPN may be the last ruling we get because we were just assigned a new judge that just came onto the bench here in Chicago. So we’re guessing, I mean we’re looking at crystal ball, that we’ll get ABIM’s ruling or a ruling in ABR first. It’s our position that we’d be lucky if we hear something by the end of the year, but some judges turn thing around quicker than others. We just don’t know if we’re number 2 in the pile in the judge’s docket or number 200.
WF: Great, thanks so much.
I hope this has been informative and will continue to update my readers with the status of these suits as information on them comes available. If you find these efforts useful, please consider contributing what ever you can to the voluntary GoFundMe page in support of the plaintiffs. Hopefully together we can end MOC's stranglehold on working physicians nationwide.
Thanks-
-Wes
Thursday, August 29, 2019
American Board of Emergency Medicine Resorts to Adhesion Contract to Limit Its Liability and Legal Costs
A question posed recently by a physician on Facebook:
Contributions can be made here.
We'll see what the courts decide on the legality of this practice of coercing physicians using unavoidable adhesion contracts.
-Wes
Can anyone tell me if this is legal? I have to check the American Board of Emergency Medicine's website for info regarding MOC and the Concert Exam. In order to have access, I have to agree to this statement. This leaves me no choice, yet MOC is mandatory. It feels like blackmail. And would this be enforceable in a class action lawsuit?I would encourage all Emergency Physicians to join our fight against the American Board of Internal Medicine that has a similar adhesion contract embedded on its website behind its firewall, too. The RICO portion of the lawsuit addresses this collusion between the ABMS member boards to further their monopoly on physicians' initial board certification for their financial, political, and promotional purposes.
RELEASE OF ABEM
I agree to indemnify, and waive any right to sue, ABEM and its directors, examiners, committee members, officers, employees, and agents; to hold them harmless from any claims or damages including, but not limited to, attorneys’ fees and costs incurred in connection with my participation in activities to stay ABEM-certified, including but not limited to any action they, or any of them take or fail to take in connection with my participation in certification activities; my eligibility for examination; the gathering, furnishing and use of information about my training and practice; the grading or conduct of my tests or examination(s); and/or the failure of ABEM to issue me a certificate.
CONTROVERSY OR CLAIM RESOLUTION
I agree that if, despite the Release of ABEM in the paragraph above, I sue ABEM, I will bring that suit in Chicago, Illinois and that I will pay all of ABEM’s costs and attorneys’ fees in connection with such suit.
Contributions can be made here.
We'll see what the courts decide on the legality of this practice of coercing physicians using unavoidable adhesion contracts.
-Wes
ACP Supports ABIM Plans for More Continuous Certification
Yesterday, the American College of Physicians (ACP) issued a press release in support of the American Board of Internal Medicine's (ABIM) plans to develop a new "longitudinal continuous certification" educational product to maintain their initial board certification. In that press release, they confirmed that this "option" was in response the the American Board of Medical Specialties' (ABMS) Vision Commission's Final Report and the ACP's lengthy comments to that report that included a "Recommendation 12" for "annual participation" by internists.
Somewhat ironically (but not surprisingly), the press release contradicted ACP's earlier Recommendation 10 of those comments:
First of all, where are the data that longitudinal continuous certification (a product not yet developed for internists) provides "internal continuous quality improvement" of the ABMS or practicing physicians? Or is such a product really a means to just "improve the effectiveness and efficiency" of monetary collections for all of these independent non-profit organizations?
Importantly, does such an unsubstantiated statement "build and sustain our members' trust in the continuous certification process," particularly in light of the important and well-written antitrust and RICO lawsuit underway against the ABIM? Should participation in any physician ongoing educational program have the potential to limit a physician's ability to maintain their insurance panel participation, malpractice coverage, or hospital privileges like this "Continuous Certification" program does?
Of course not.
The ACP would be wise to distance themselves from support of the ABIM, lest they reinforce evidence for racketeering. But then again, I'm just a physician. Let's see if the courts decide there might be a basis for the claims made, especially in light of this latest ACP press release.
-Wes
Somewhat ironically (but not surprisingly), the press release contradicted ACP's earlier Recommendation 10 of those comments:
Recommendation 10: ABMS Boards must collectively engage in a regular continuous quality improvement process and improve the effectiveness and efficiency of continuing certification programs.
ACP agrees with the need for ABMS and its member boards to engage in internal continuous quality improvement, to build and sustain our members’ trust in the continuing certification process.
First of all, where are the data that longitudinal continuous certification (a product not yet developed for internists) provides "internal continuous quality improvement" of the ABMS or practicing physicians? Or is such a product really a means to just "improve the effectiveness and efficiency" of monetary collections for all of these independent non-profit organizations?
Importantly, does such an unsubstantiated statement "build and sustain our members' trust in the continuous certification process," particularly in light of the important and well-written antitrust and RICO lawsuit underway against the ABIM? Should participation in any physician ongoing educational program have the potential to limit a physician's ability to maintain their insurance panel participation, malpractice coverage, or hospital privileges like this "Continuous Certification" program does?
Of course not.
The ACP would be wise to distance themselves from support of the ABIM, lest they reinforce evidence for racketeering. But then again, I'm just a physician. Let's see if the courts decide there might be a basis for the claims made, especially in light of this latest ACP press release.
-Wes
Sunday, August 25, 2019
Assuring Longitudinal Physician Exploitation and Burnout
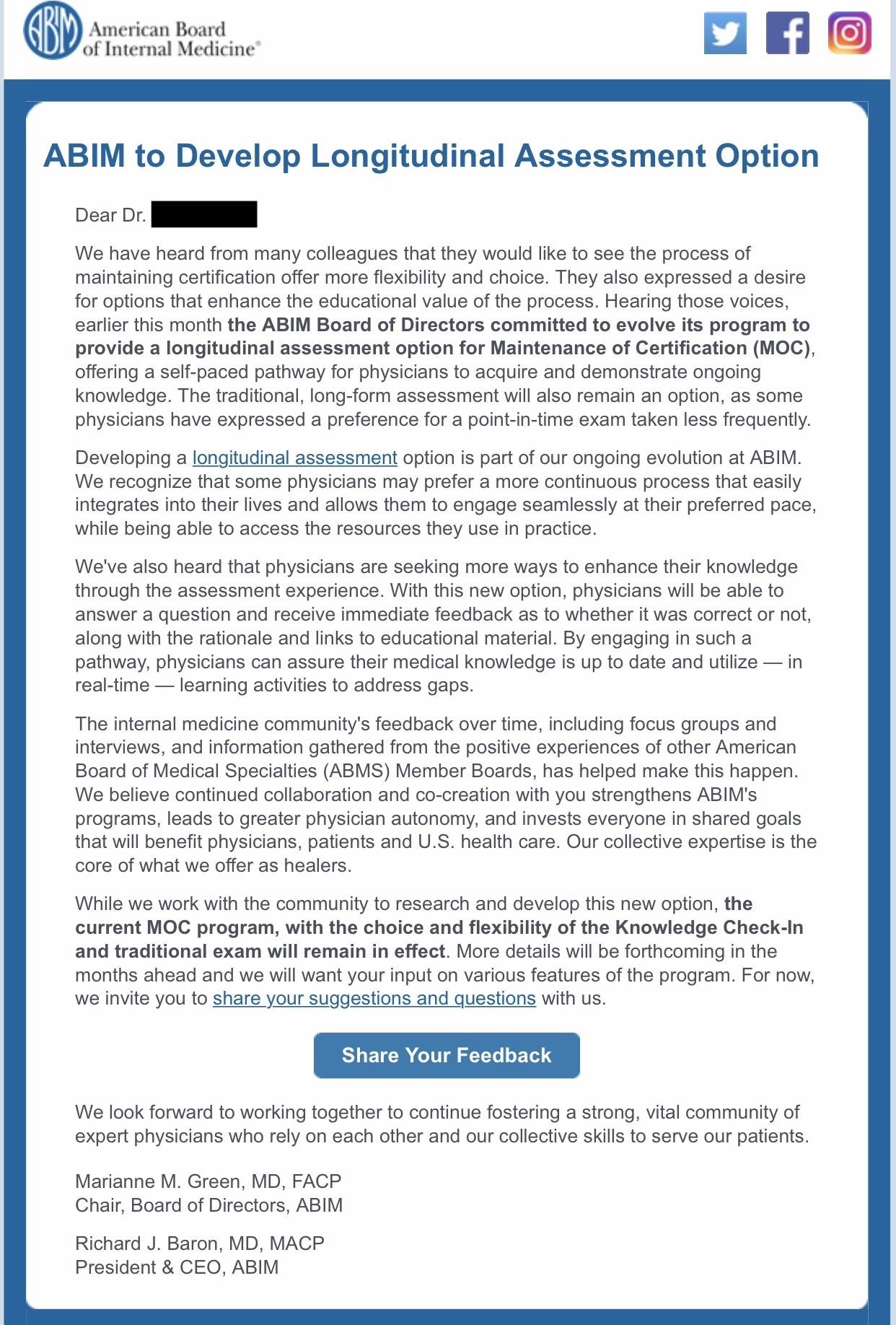 |
| ABIM Email Notification |
One of his emails included a notification that the American Board of Internal Medicine (ABIM) is developing a Longitudinal Assessment Option because they were "hearing those voices" from an overseas professor that implied "many of our colleagues have said they would like to see the process of maintaining certification offer more flexibility and choice." The ABIM now adapts behavioral and cognitive psychology to teach this busy electrophysiologist the "important competencies" of "professionalism, working in a team, and collaboration" promised by this new ABIM Longitudinal Assessment Option for MOC.
The ABIM stands on the head of a pin as it sends mixed messages about competency, professionalism, teamwork, and trust, all while maximizing the medical industrial complex's profit stream. It sends its email or tweets as they shape our next generation of physicians to continue to comply in being exploited and to make peace with the new medical group-think. A thinking person might see the contradictions inherent in these conflicting goals - but then this is the new MOC reality despite the lawsuits underway to end this program.
Pity the poor doc who now must decide at 10:45 PM whether he sits on his zafu, engages in relational maintenance with whoever is still up at home, or completes the graduated teaching assignment kindly forwarded by ABIM.
What we must never ask is whether there will ever be a MOC module or a pranayama sufficient to make this lifestyle sustainable.
-Wes
Thursday, August 15, 2019
MOC Issue Embroils EP Community
After I circulated my fund-raising video two weeks ago to the Electrophysiology Community via the Heart Rhythm Society (HRS) closed message board, a firestorm of challenges to the HRS leadership have erupted online. At their core, the HRS is now under increasing pressure to decide with whom they side: (1) their physician membership or (2) other corporate interests. The exchange has become so heated that the HRS has decided to issue a new "survey" to gage how their members feel about "continuous certification" and lifelong learning via the MOC paradigm. The re-issued survey closes 19 August 2019 and HRS members are encouraged to complete that survey just (re-)sent to them. (The first survey was shared publicly on social media and many physicians responded anonymously, making it difficult for HRS to determine their membership's responses, we are told).
Here are just a few of the comments being circulated, even as late as today, as HRS leadership try to defend their relationship with the American Board of Internal Mesicine (I have chosen to make comments anonymous out of respect to those who have made their feelings known publicly).
Working cardiac electrophysiologists know that HRS has advocated for many of their needs over the years, but on this issue and it potential to affect their right to work, the conflicts of interest inherent to MOC with insurers, group purchase organizations, and hospital systems present a formidable challenge to the entire HRS leadership going forward.
Trust take years to develop. Let's hope HRS doesn't lose what they've earned in a heartbeat.
-Wes
Here are just a few of the comments being circulated, even as late as today, as HRS leadership try to defend their relationship with the American Board of Internal Mesicine (I have chosen to make comments anonymous out of respect to those who have made their feelings known publicly).
I have warned prior physician-presidents of HRS about this controversy, but it never dawned on me at the time that physicians no longer control the organization. That task, like so many in medicine today, was relegated to a non-physician non-profit executive long ago. It will be interesting to see how this will play out going forward, especially since the MOC monetary and conflict of interest genie is out of her bottle. The HRS leadership, be they physician or not, has a very serious fundamental decision to make: side with their physician membership, or side with their conflicted corporate partners who will stop at nothing to assure their profit margins.
- "Love it or
leavelove it. I am so looking forward to my body frisk looking for cheating materials at the Pearson View testing center in December - a $1200 massage will put me in the right frame of mind to take a day-long test, much of the content of which has no relevance to the things that matter towards helping my patients to live longer or live better. But no worries, I'm sure the HRS Board Review course (estimate >10K with room, board and lost wages, not to mention deduction from time for meaningful CME) will enlighten you as to the latest nitty gritty in IKwtf, so you'll be awesome at parties."
- "As I’m sure you are fully aware, this money grab and power grab are far deeper reaching than most realize and your suggestion to deal with it locally cannot work. It’s extremely disingenuous of you to imply otherwise.
A few years ago I decided to stand up for what I considered right and take a stand against the ABIM/ABMS. I refused to participate in MOC (though I go to HRS and a few other meetings every year and consider myself beyond competent). When my 10 years were up I chose not to take the recertification exam. I became board certified by the NBPAS. My local credentials committee didn’t know what to make of it, but when I met with them and explained my objection they went along. I told them if they didn’t I was leaving and I’m the only one who does a lot of the things I do in my institution. Then the insurers (BCBS) net with administration and their opinions changed. BCBS said they could no longer pay for anything I did unless I was pursuing recertification. The hospital administration said I needed to take the ABIM recertification exam or they could no longer employ me. I told them that’s fine, then I’ll quit and go into private practice and just see CMS patients (they don’t require ABIM certification). Administration told me if I did that then my privileges would be revoked. As I send this message I’m waiting for the first session to start at the board review course. I will never take this exam again. If this same bullshit exists in 10 years then I’ll retire at 56.
Please don’t pretend that you are unaware that the NCQA which certifies insurance companies are in bed with the ABMS/ABIM who certify physicians. Don’t pretend that you are unaware that there are members who sit on both boards and profit tremendously off the backs of working physicians. I’ve met with the insurers who tell me they’d like to allow me an exception, but NCQA requires that all the physicians they contract with are ABMS (means ABIM in the EP world) board certified.
So there you have it. ABIM requires MOC. If physicians refuse they revoke their certification. If they continue to object or seek alternative certification (NBPAS, IBHRE) then the rely on the NCQA to pressure payers (they threaten to revoke the insurers NCQA certification if they have physicians on their panel who are not “certified” by the one true board) to force physicians back in compliance by removing them from their panels. If physicians continue to refuse the payers threaten hospital administration and they threaten to revoke the physicians hospital privileges. If you don’t see a problem with this then I suspect you have a conflict of interest. Again please don’t attempt to deceive the HRS membership."
Working cardiac electrophysiologists know that HRS has advocated for many of their needs over the years, but on this issue and it potential to affect their right to work, the conflicts of interest inherent to MOC with insurers, group purchase organizations, and hospital systems present a formidable challenge to the entire HRS leadership going forward.
Trust take years to develop. Let's hope HRS doesn't lose what they've earned in a heartbeat.
-Wes
Thursday, August 01, 2019
AntiMOC Lawsuit Update
As the summer winds on, I have been approached by more and more people who would like an update on where the litigation filed against the many member boards of the American Board of Medical Specialties stand since the lawsuits were filed. I will do my best to briefly summarize the status of those lawsuits as I understand them. (For background on why these lawsuits have been filed against so many of the American Board of Medical Specialties specialty boards, please review this video).
The antitrust suit against the American Board of Internal Medicine (ABIM) was originally filed 6 Dec 2018 and amended 23 Jan 2019 to include RICO charges, the antitrust lawsuit against the American Board of Radiology was filed 26 Feb 2019, and the antitrust lawsuit against the American Board of Psychiatry and Neurology (ABPN) was filed 6 MAR 2019. These cases were filed by a law firm based in Chicago. A fourth lawsuit was filed by a separate law firm in Southern District Court of California on 19 Feb 2019 against the American Board of Medical Specialties (ABMS), the American Board of Emergency Medicine (ABEM), and the American Board of Anesthesiology (ABA).
Each of the member boards are represented by different law firms.
Three of the specialty boards (ABIM, ABR, and ABPN) have appeared and, as expected, filed motions to dismiss with mostly overlapping arguments. The motion in the ABIM case was fully briefed a couple of months ago (Motion to Dismiss here, Opposition for Motion Dismiss here), the ABPN motion was fully briefed last month (Brief in Support of Motion to Dismiss here, Opposition to Motion to Dismiss here), and the briefing in the ABR case should be finished mid-August.
In the interim, a motion to consolidate the above cases (brought by the law firm representing the plaintiffs in the ABMS/ABEM/ABA case) which the plaintiffs in the ABIM, ABR, and ABPN cases opposed out of the concern that it might delay the cases and add to their cost, was denied. So these three cases (ABR, ABPN, and ABIM) will each continue on their own in the federal courts in Philadelphia (ABIM) and Chicago (ABR and ABPN).
It would not be unusual for the courts to take several months to decide the motions to dismiss, especially given their complexity and importance. Discovery for these cases will begin once the motions to dismiss are decided, which is hoped will be no later than the end of the year. As I am sure many of my readers have already observed, the litigation seems to be having a modest impact, as many specialty boards and specialty societies claim to be re-thinking their Maintenance of Certification (MOC) requirements, at least around the edges.
It is important that physicians continue to help fund the GoFundMe page sponsored by Practicing Physicians of America. (Remember, short of processing fees, every penny of those contributions will to toward these continuing legal efforts.)
In summary, I believe the legal cases are progressing as well as can be expected and I remain convinced that, together, working physicians CAN end Maintenance of Certification's stranglehold on US physicians nationwide.
-Wes
The antitrust suit against the American Board of Internal Medicine (ABIM) was originally filed 6 Dec 2018 and amended 23 Jan 2019 to include RICO charges, the antitrust lawsuit against the American Board of Radiology was filed 26 Feb 2019, and the antitrust lawsuit against the American Board of Psychiatry and Neurology (ABPN) was filed 6 MAR 2019. These cases were filed by a law firm based in Chicago. A fourth lawsuit was filed by a separate law firm in Southern District Court of California on 19 Feb 2019 against the American Board of Medical Specialties (ABMS), the American Board of Emergency Medicine (ABEM), and the American Board of Anesthesiology (ABA).
Each of the member boards are represented by different law firms.
Three of the specialty boards (ABIM, ABR, and ABPN) have appeared and, as expected, filed motions to dismiss with mostly overlapping arguments. The motion in the ABIM case was fully briefed a couple of months ago (Motion to Dismiss here, Opposition for Motion Dismiss here), the ABPN motion was fully briefed last month (Brief in Support of Motion to Dismiss here, Opposition to Motion to Dismiss here), and the briefing in the ABR case should be finished mid-August.
In the interim, a motion to consolidate the above cases (brought by the law firm representing the plaintiffs in the ABMS/ABEM/ABA case) which the plaintiffs in the ABIM, ABR, and ABPN cases opposed out of the concern that it might delay the cases and add to their cost, was denied. So these three cases (ABR, ABPN, and ABIM) will each continue on their own in the federal courts in Philadelphia (ABIM) and Chicago (ABR and ABPN).
It would not be unusual for the courts to take several months to decide the motions to dismiss, especially given their complexity and importance. Discovery for these cases will begin once the motions to dismiss are decided, which is hoped will be no later than the end of the year. As I am sure many of my readers have already observed, the litigation seems to be having a modest impact, as many specialty boards and specialty societies claim to be re-thinking their Maintenance of Certification (MOC) requirements, at least around the edges.
It is important that physicians continue to help fund the GoFundMe page sponsored by Practicing Physicians of America. (Remember, short of processing fees, every penny of those contributions will to toward these continuing legal efforts.)
In summary, I believe the legal cases are progressing as well as can be expected and I remain convinced that, together, working physicians CAN end Maintenance of Certification's stranglehold on US physicians nationwide.
-Wes
Subscribe to:
Posts (Atom)