Welcome to this week's mid-term edition of the medical blog-o-sphere's Grand Rounds! Before we begin, be SURE to get to the polls to VOTE!
This week submissions were classified by state or country of origin. Politically incorrect posts by state were colored
RED whereas politically correct posts by state were colored
BLUE. (States with both extremes are represented in
PURPLE.)
Now what would any political post be without a
POLITICAL MAP of the states represented in this week's Grand Rounds?
(Scroll down or click on a desired state)
TENNESSEE
It is rare to find such a wonderful example of our great democracy in action, where even the little guy can run for governor. But along came
this must-see video, by far the most politically-incorrect submission to this week's Grand Rounds. This post should serve as a reminder to all of us why we MUST get out and vote today. (Submitted by the
Happy Hospitalist). Go Basil!
(Return to map)GEORGIAThe Peach State has both extremes,
- From the very politically correct: Kimberly Manning, MD takes one heck-of-a-big-breath as she offers a refreshingly realistic view of the tenacity required to manage medicine, kids, home and a bit of social life. Doctor-moms never get enough credit. (Via: the ACP Hospitalist blog)
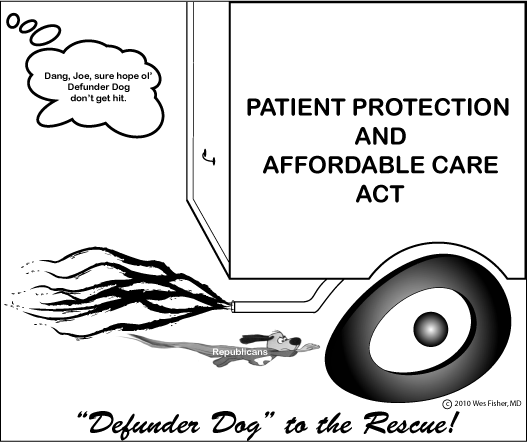
- To the very politically incorrect: Insurance executive Bob Vineyard isn't too happy with the Department of Health and Human Services granting "Obamacare waivers" to large, influential companies and wants to make sure you know about it. Tell us how you feel! (Return to map)
PENNSYLVANIADr. Rich, ever politically incorrect yet astute over at the
Covert Rationing blog, shares with us why he feels
this midterm election cycle is a yawner: the fat lady, er, man, has already sung.
(Return to map)KENTUCKYDr. John Mandrola of the
Dr. John M blog, always a bastion of political correctness,
explains who should be on
death expert panels if he were in charge and why.
(Return to map)ARKANSASDoctors who blog add depth to medical stories found on the internet. A fantastic example is Dr. Ramona Bates's
coverage of California Republican U.S. Senate Candidate Carly Fiorina’s recent hospitalization due to an infection related to her post-mastectomy breast reconstruction. We need more like this. I wonder if she's thought about a run for Congress...
(Return to map)ILLINOISFile these under politically correct:
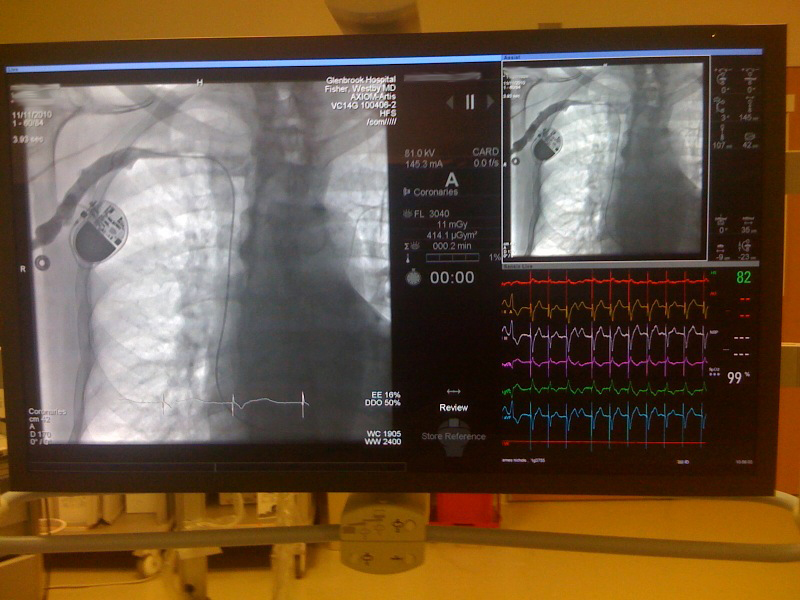
Ever have something break (like an exploding ICD) and want to find out if others have seen the same thing? Check out Tony Chen's FDAZilla search engine that makes it easy to search the FDA's MAUDE database.
John H. Schumann, FACP uses President Obama's handling of the career USDA employee Shirley Sherrod's contextual kerfuffle as an example for "making nice" after we screw up. And while errors are inevitable and this is probably the best way to handle them once they've occurred, the story also reinforces principles to which all blog readers should ascribe: checking sources before drawing conclusions. (Return to map)
NEW YORK(Political Action Committee) Chris Langston, Program Director of the John Hartford Foundation, happily
reintroduces us to the must-see satirical video that lampoons a clueless “health care executive” who has read in
Modern Healthcare how to create an Accountable Care Organization (ACO) and “have lots of meetings” to make his board happy. While Langston acknowledges "...everyone interested in health care reform is hoping that ACOs will provide a miracle cure for our ailing health system, no one is really sure how they will work." But like the true executive that he is, he then explains (with the help of
Modern Healthcare, of course), how they will work. It's hard to find a better example of executive political correctness.
Elaine Schattner, M.D.
shares her review of a new Broadway play
Bloody Bloody Andrew Jackson and shares these tag lines:
Some times you have to take the initiative.
Some times your whole family dies of cholera.
Some times you have to make your own story.
Some times you have to shoot the story teller in the neck.
Some times you have to take back the country….
Hmmm. A metaphor?
(Return to map)NEBRASKARegarding sentiment for health care reform, the Happy Hospitalist reminds us that
some former supporters are throwing in the towel. In a word: change.
(Return to map)MASSACHUSETTS(Political Action Committee) Julie Rosen of the
Bedside Manner blog explains why
health literacy matters and brings our attention to the need for good public education and its benefits of such later health care.
(Return to map)INDIANA(Political Action Committee) Walter Jessen of Highlight HEALTH reports on how the National Breast Cancer Coalition (NBCC) has
thrown down the glove to push for a breast cancer vaccine by 2020. This is a great example how special interests confront our legislators every day. (Note: they listen more if you bring lunch!)
(Return to map)CANADAIn "From Plain Film to 3D: Radiologists as Superstars," Notwithstanding Blog
argues that radiologists are the economic superstars of American Medicine. Funny to hear this from Canada. Still, it's acknowledged "... the challenge facing American radiologists in my lifetime may not be justifying their value in patient care so much as justifying their value over and above their American-boarded Indian-based counterparts." Exactly.
(Return to map)UNDISCLOSEDDr. Fizzy over at
A Cartoon Guide to Becoming a Doctor explains, as only a cartoon can, why
Health Insurance Sucks. Too bad Dr. Fizzy may soon be mandated by law to buy it.
(Return to map)* * *Before closing, I'd like to point you to a few more salient
election day thoughts by Paul Levy, CEO and President of Beth Israel Deaconess Medical Center:
I hope the very good people who lose in tomorrow's balloting will keep up their fights, whether they are incumbents or challengers. They, especially, deserve our thanks for participating in our election process.
Amen.
Next week's Grand Rounds will be hosted by Mother Jones, RN at
Nurse Ratched's Place.
-Wes