A 74 year old man with a biventricular pacemaker placed for a history of congestive heart failure is placed on telemetry following a total hip replacement. The "low rate alarm" on telemetry sounds, the nurses look, and note pacemaker spikes "everywhere" and want to transfer the patient to the ICU. You are called and review the strips:
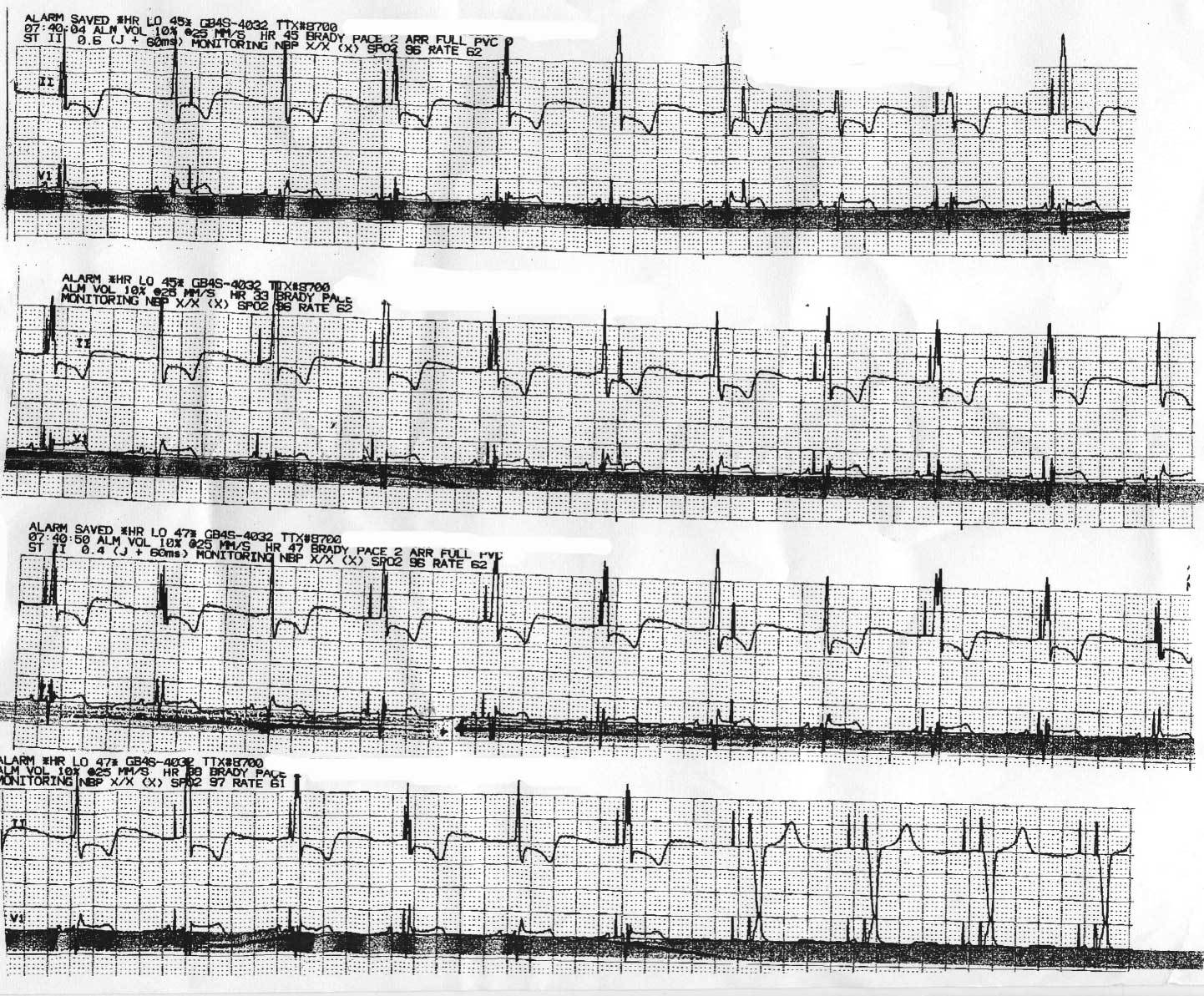
Click image to enlarge
Should the patient transfer? What's going on?
-Wes
12 comments:
My best guess is that somehow the cautery from the total hip caused the pacer to swap modes due to interference. It kind of looks like it is running in a AAO/VVO mode, in other words, asynchronously, but I'm not 100% sure on that due to the lack of pacing He doesn't need the ICU, just a pacer check to start. It's either that or the battery needs to be changed.
OK Wes I'll take a stab at this one. Whatever the disturbance is here resolves with the last 4 intervals on the 4th strip where you have DDD pacing with atrial and ventricular capture, I'll say a paced AV delay of approx 150ms. Prior to that there is a consistent narrow complex rhythm which is holding at a rate 0f 58-62 BPM. Not every complex receives an atrial or ventricular pace impulse and several intervals have shorter AV intervals suggesting a safety pacing mechanism, most likely due to intermittent atrial undersensing. I am curious as to the etiology of the competing rhythm. My first guess was an accelerated junctional rhythm but it looks like a consistent P wave in V1 with a PR interval of about 150ms. There appears to be some sort of isorhythmic competition going on with atrial and ventricular undersensing present. Please tell me you are going to post some marker channel data from the pacer interrogation? Us pacer geeks get kinda spoiled on that stuff you know.
Oh forgot to mention.....if the patient is hemodynamically stable there really isn't really any reason to transfer the patient solely based on this pseudomalfunction.
Dr. Wes -
My guess is that the pacemaker is functioning in DVI or DOO mode. Maybe the apparent shorter AV intervals can be explained by bivent pacing rather than AV timing.
I would think a transfer to ICU would be made based on the patient's clinical status and not the behavior of the device (treat the patient, not the monitor).
You're one of the few people who can stump me with ECGs! :)
Tom
Good ideas.
Let me offer a little clue that might direct the thinking. (By the way, I hate faxed monitor strips, too).
All right -
In light of the clue, I'll amend my answer and say atrial undersensing with occasional triggered activity.
In other words, I'm with the pacer geek (and aspire to be one)!
:)
Tom
accelerated junctional rhythm.
all good....just let him wake up a little bit more, monitor him and stay put as long as everything else stays copacetic.
SK
Are you EVER going to get around to filling us in on this one????
I agree with Anonymous #1 (pacer geek). Probably from industry. Way too smart to be a doctor.
To understand this tracing, it is best to look to the end of the strip where dual-chamber pacing is seen. This defines the lower rate of the pacemaker (60 b/min) and the AV delay (slightly over 120 msec->actually 130 msec). Note there is an atrial response to the pacing output here (last two arrows on the “clue” tracing).
What is puzzling is the QRS morphology difference of most of the QRS complexes that occur before these last paced beats. Careful inspection of the partially-obscured lower EKG tracing (V1) discloses that there is a native P wave that occurs before the first paced beat on many occasions (the earlier arrows on the “clue” tracing above). Hence, the change in QRS morphology is because of an intrinsically-conduced QRS complex (the patient’s native rhythm).
But this does not explain the pacing spikes that occur with varying AV intervals and both before and after the QRS complex. To explain these, we have to understand the timing cycles of dual-chamber pacemakers.
In order for any pacemaker to work properly, it must be able to both sense the patient’s intrinsic rhythm and pace (eg, capture) the appropriate heart chamber when a beat fails to occur. Further, the output spike from one chamber must not be seen by the other chamber’s sensing circuitry, a phenomenon called “cross-talk,” otherwise appropriate pacing output might be inhibited.
To prevent one chamber from being sensed by the other chambers, engineers “blind” the opposite chamber from sensing the paced chamber’s pacing output, by “blanking” the sensing circuitry both during, and immediately after pacing output. This blanking period is programmable, but lasts at least 12 msec in most pacemakers. Therefore, if a ventricular event occurs during atrial pacing output (and during the atrial blanking period), it is not “seen” by the pacemaker, so it is ignored. An example of this is seen on the second beat of the tracing, where the QRS lands on the atrial pacing spike and the ventricular pacing spike fires when the ventricle is refractory (and hence, does not capture). Pacing spike, then, are seen late after the QRS complex in the ST segment, but do nothing.
Also, engineers devised a way to assure pacing output to the ventricle in case an atrial lead dislodged. In this case, the atrial response to pacing might be seen by the ventricular lead and inhibit its output. To prevent this, if a ventricular sensed signal occurs within the earlier part of the programmed AV delay, ventricular safety pacing occurs 110 msec after the atrial output (hence the narrowly coupled pacing spikes near the QRS complex) to assure that the ventricle is always paced. Many examples of this can be seen on this tracing.
So, as can be seen in lead V1 of the faxed tracing, the patient’s native P wave occurs on many occasions before the two pacing spikes making it clear that the pacemaker is undersensing the atrial signal. This malfunction of the atrial lead sensing does not require transfer to the ICU, but rather a minor pacemaker programming adjustment.
A good review of pacemaker malfuntion can be found here.
Dr. Wes:
Is the V-V timing zero then for this bi-V pacemaker?
Anony 10:46-
Yes.
I was at least right when I said they needed a setting tweak and didn't need to go to the Unit!
Post a Comment