He arrived at the emergency room diaphoretic, hypotensive, and with substernal chest pressure. The patient was brought immediately to an emergency room care area and a stat EKG disclosed classic ST segment elevation in the inferior leads. The cath lab team was immediately summoned as the ER team worked to stabilize the patient. Within minutes, the attending cardiologist was on the scene, reviewed the EKG, examined the patient, and explained to the hoardes of family members with the patient what was taking place. In the interest of being expeditious with his consent process as the team was arriving to take the patient to the cath lab, the attending said:
"There is a 1% risk that anything bad that you can think of could happen with this procedure. If you'd like me to detail those things, I can."
The patient didn't want to hear, and off to the cath lab they went to open the patient's occluded right coronary artery to great relief of the patient and family.
Later, in follow-up, the attending cardiologist was making rounds and asked the patient his occupation.
"I'm a malpractice attorney."
Smiling, the cardiologist immediately asked, "How was my consent?"
"Perfect. Absolutely perfect."
-Wes
Friday, May 31, 2013
Thursday, May 30, 2013
A Critical Review of the Insurance Claim Denial Process
"If you can speak what you will never hear,
if you can write what you will never read,
you have done rare things."
-Henry David Thoreau
"Doctor, how much longer?"
The case had gone smoothly, but the challenges of mapping the infrequent skipped beats that signified the initiating sequence to the tachycardia was getting more difficult. "Could it be left sided?" I wondered. "Anterior or posterior? I've tried the posterolateral area and that timing was late. Clearly anteromedial was earlier. All the darn beats look so similar with pace-mapping."
I had been working for an hour and a half without effect when I had an idea: "Maybe the 3D mapping system would help."
And so, I deployed a highly sophisticated three-dimensional (3D) electroanatomical (EAM) mapping system that sped her successful ablation. She was relieved. That is until the bill arrived and the 3D EAM mapping was denied by her insurance carrier.
***
On December 19, 2012, I wrote about the insurance denial for this case. I was surprised that a denial for payment was made for a portion of a ventricular tachycardia (VT) ablation procedure that was commonplace in my field: three-dimensional (3D) electroanatomic mapping. Worse, I was even more surprised that the denial came from an unknown physician who lacked training in my field and appeared to be nothing more than a foot-soldier of a Cigna insurance company medical coverage policy. Such a denial had never happened to one of my patients before.
Since that blog post was written many months ago, my administrative staff and I have been enduring the appeal. Here's how it's gone.
Shortly after my piece was published, I was notified that someone at Cigna had called our hospital and inquired if they were aware of my blog post. They were. My workplace has graciously permitted me to have this blog since 2005, provided I clearly state the views in that blog are my own, which they are.
Second, I learned that the individual who sent the original coverage denial letter to me was not our local Cigna "regional" medical director. After my post was published, my local medical director from Cigna wanted to talk and explain the proper way that claim denials should handled. A telephone conference was arranged between myself and my the medical director (a local pediatrician from a local academic center which will go un-named) along with another non-medical representative of the local regional office of Cigna. I offered them the opportunity to publish a rebuttal to my post at this site if they desired, but they declined the offer. Instead, I was asked to contact them via e-mail or phone before going public with my concerns about their decision on a blog - "we have a set way of handling disagreements with policy decisions" I was told. Was this because Cigna's leadership didn't want the bad press or was it a polite way of saying "cease and desist?" I wasn't sure.
So, in the interest obtaining a reversal of my patient's claim denial as easily as possible, I complied. I sent them my first rebuttal in writing and communicated with them via email as requested. My rebuttal went something like this:
Cigna's original denial letter, dated 1 March 2012 stated:
Since that blog post was written many months ago, my administrative staff and I have been enduring the appeal. Here's how it's gone.
Shortly after my piece was published, I was notified that someone at Cigna had called our hospital and inquired if they were aware of my blog post. They were. My workplace has graciously permitted me to have this blog since 2005, provided I clearly state the views in that blog are my own, which they are.
Second, I learned that the individual who sent the original coverage denial letter to me was not our local Cigna "regional" medical director. After my post was published, my local medical director from Cigna wanted to talk and explain the proper way that claim denials should handled. A telephone conference was arranged between myself and my the medical director (a local pediatrician from a local academic center which will go un-named) along with another non-medical representative of the local regional office of Cigna. I offered them the opportunity to publish a rebuttal to my post at this site if they desired, but they declined the offer. Instead, I was asked to contact them via e-mail or phone before going public with my concerns about their decision on a blog - "we have a set way of handling disagreements with policy decisions" I was told. Was this because Cigna's leadership didn't want the bad press or was it a polite way of saying "cease and desist?" I wasn't sure.
So, in the interest obtaining a reversal of my patient's claim denial as easily as possible, I complied. I sent them my first rebuttal in writing and communicated with them via email as requested. My rebuttal went something like this:
Cigna's original denial letter, dated 1 March 2012 stated:
"Use of an intracardiac electrophysiological 3-dimensional mapping system in the diagnosis, treatment, or management of ventricular arrhythmias or any other condition because there is insufficient scientific evidence to support its use does not meet Cigna guidelines for coverage because it is considered experimental, investigational, and/or unproven (E/I/U)."Cigna's 2012-2013 Medical Coverage Policy regarding 3D electroanatomic mapping systems for VT ablation (which I have copied on my own server, lest it disappear) stated:
The authors state, "although not yet established as requisite or "core" equipment for the EP laboratory, these and other emerging technologies have had, and will continue to have, a major impact on the practice of cardiac arrhythmia management. It is also anticipated that additional new technologies will be developed at ever faster rates in the future" (Tracy, et al., 2006). There has been no update to this statement since 2006.Baloney. The EHRA/HRS Expert Consensus statement on VT ablation was subsequently published in in 2009 and that document specifically addresses the use of 3D EAM for VT ablation. It said:
Technological advances have been critical to the development of the field and will continue to play an important role in improving outcomes. The evaluation of new technologies has generally been based on uncontrolled series. There is limited head-to-head comparison of different technologies. Although new technologies generally increase the cost of a procedure when they are introduced, the costs may be justified if they improve outcomes.
...
The focal VT origin can be identified from activation and/or pace mapping.4,381,385,410 Systematic point-by-point activation mapping is the initial preferred technique.233,234,385,409 Some investigators use three-dimensional EAM systems to assist in relating the anatomy to the mapping data.4,124,125,233,381,385,428–430
Wrong.
Two MORE submissions for higher-order reviews and over four months later, the verdict was handed down: my patient had exhausted all avenues of appeal for the claim. The insurance company would not pay this portion of my patient's bill, no matter what.
Parsing Truths
When deciding what therapies are effective for our field, who should set the requirements for the level of evidence required to determine effectiveness of any therapy, EP societies or the insurance industry? While it is true that prospective randomized trials comparing mapping techniques head-to-head for localizing ventricular arrhythmias have not been done, we should also understand that such a study will never be performed. Why? First, who would pay for such a study to be conducted? The utility of 3D mapping for SVT has been demonstrated and proven effective, in large part because of the greater safety (and greater likelihood of obtaining FDA approval) when supraventricular rhythms are studied compared to ventricular arrhythmias. Second, because the occurrence of the arrhythmia (in this case RVOT VT) is relatively rare, a compelling reason for industry (or government) to fund such a study doesn't exist.
But like SVT ablation, there are three real advantages to these 3D mapping systems for VT ablation that has been repeatedly demonstrated in the literature: (1) catheters can be returned to prior locations accurately whether the arrhythmia is occurring in a location or not, (2) real reductions in fluoroscopy times can be achieved and (3) certain 3D EAM systems that use mathematical algorithms (non-contact balloon mapping) can localize the origin of an arrhythmia using a single heart beat. For the rare patient (like mine) that has infrequent arrhythmias, how would a randomized trial be constructed in hopes of proving the utility of such a technology over conventional mapping by point-to-point techniques? Would such a trial be even ethical to conduct? So, just because a prospective trial has not been performed to demonstrate the utility of a technology in rare circumstances, does this mean electrophysiologists should never utilize such a technology to achieve a successful ablation outcome when other means fail even though such a technology has been shown to be effective in single-center studies? According to Cigna's policy statement, the answer to this question is "yes."
Too bad insurers never have to speak with patients when an ablation fails.
One Last Try
Because I did not want to take "no" for an answer, I asked my administrative staff to see if they could obtain the name of the Cigna "external" reviewer. We had been assured that the case was externally reviewed by an electrophysiologist. We were given the name of an individual but were surprised to find that the physician was a paid employee of Cigna with credentials as an internist and general cardiologist with a nuclear medicine background. To me, it seemed Cigna "external" review was actually an "internal" review performed by a paid employee of different regional office of Cigna (hence "external" to our region) who was a general cardiologist, not a cardiac electrophysiologist.
I brought this concern to the attention of my local medical director of Cigna by e-mail. In that email I also expressed my concerns about the long time each review had taken. I asked him to examine both issues, since I felt my patient had not received a fair and unbiased claim review. Also, while my patient had received a final denial letter, I never received a notification of their final determination for coverage. After some delay, the director promised to look into my concerns and contacted me by phone later in the week as promised.
In our subsequent discussion, it appeared the director felt the timeliness of their reviews was satisfactory, despite a timeline that stretched over fourteen months for this entire process. In regards to my concerns over who reviewed my patient's claim denial, he claimed there were two "internal" Cigna reviewers and reviewers "external" to Cigna who supported the denial. Of the external reviewers, the director claimed one was board-certified in internal medicine and interventional cardiology and the other external reviewer was board-certified in internal medicine, cardiology and cardiac electrophysiology. He refused to disclose either of the external reviewers' names. When asked, the director stated that the electrophysiologist was in active practice. I reiterated that I still felt the EHRA/HRS Expert Consensus statement suggested the 3D-mapping falls well within the standard of care. Surely they should reconsider. But despite my pleas for reconsideration, no reversal was forthcoming.
I hung up the phone.
Amazingly, there is little else I can do for my patient's insurance payment denial now. Here I am, a non-anonymous board-certified cardiac electrophysiologist with over twenty years experience who was caught in a challenging case with my patient and am now being told by a pediatrician from an insurance company that there's no merit to my concerns about an unfair denial for coverage of the 3D mapping portion of my patient's claim. I am dumbfounded, confused, and heartbroken for my patient.
So what have I learned?
1) In Cigna's case, some insurance coverage decisions disregard current standards of care and up-to-date expert consensus statements in lieu of poorly-updated corporate medical coverage policies.
2) Specific challenges I encountered with my patient's RVOT VT ablation case had no bearing on Cigna's decision.
3) Physician reviewers often do not hold expertise in the specialty areas they are asked to review. Because they are first and foremost paid employees of the insurer, they turn to corporate medical coverage directives for guidance, even though they are woefully lag current medical practice. As health care dollars get tighter and medicine becomes increasingly codified, significant conflicts of interest will continue to rise for a fair and impartial review of payment denials.
4) If the insurance company claims to have an individual of the same specialty externally review a case, physician providers are not notified of the basis for the denial nor given the names of the reviewers, limiting one's ability to verify the reviewer's credentials or to understand the rationale for the denial. As a result, there is no transparency to the process, nor opportunity for learning or system improvement. To me, this practice should not be condoned. Health care requires continuous quality improvement. More importantly, health care requires trust of all those who touch the field, especially when the care provided, no matter how seemingly far removed, impacts a patient's physical or socioeconomic well-being.
5) Cardiac electrophysiologists should be aware that both Cigna (here) and Aetna insurance companies (here) in Illinois now have coverage policies that may opt to deny payment for three-dimensional electroanatomic mapping for VT ablation because they claim they are experimental procedures for this indication based on their outdated internal review of the literature.
6) When confronted about the obsolete nature of their medical coverage policy, Cigna refused to take this into consideration and still refused to overturn by patient's payment denial. Instead, the medical director only promised to include the EHRA/HRS document I sent them in their next annual review of their corporate medical coverage policy for 3D mapping scheduled for 2013-2014.
7) There are technologies that have certain niche benefits for patients, but because they are not "proven" beneficial by randomized trials, in some cases they are no longer be paid for by insurers.
8) My patient will now has four months from the date of her final denial letter to ask for an state-directed independent external review of the Cigna's coverage decision via the Illinois Insurance Fairness Act as her only remaining avenue for recourse.
So now what?
As I reflect on this case, I used this sophisticated mapping technology because I felt I needed it to improve my patient's outcome and safety. I wonder what this denial of coverage does to the relationship with my patient. Has trust been eroded? As I look forward, how I will perform my next RVOT VT ablation? What do I say to the next patient with a similar arrhythmia? Should I warn all my future patients requiring VT ablation that some of the technology we routinely use to expedite their procedure might not be paid for by their insurer because of a paucity of prospective randomized trials exist (and never will)? Will I have to avoid the use of this technology knowing my patient may have to pay for it because a pediatrician or a general cardiologist who knows nothing about my field might not approve its use? Can I afford to devote this amount of time for wrestling future insurance payment denials that surface?
These are not minor concerns.
So there's the current status of this long, arduous months-long insurance denial review process for just one patient, critically reviewed. It would be easy to make this post a screed against one insurer, and while I have to say that the way this claim denial process was handled was poor at best, we should recall that other insurers have similar policies. It is in the interest of insurers to make the payment denial/review process as difficult as possible for patients and providers. It is also in insurers' best interest to keep out-of-date medical coverage policies in place that consider new technologies "experimental." Better yet, it is even better for insurers to claim niche technologies are "unproven" despite evidence to the contrary and should therefore never be paid. Finally, it is in insurers' best interest to perform internal reviews by uninformed physician reviewers of another subspecialty rather than peer-to-peer independent reviews.
What will it take to change this system?
Maybe we should start with the truth.
-Wes
Transitions
 |
The world was ahead of him now as the year ended. He had so much to do, so much ahead: a graduation, new city, wife with a new job, a need to find a home and new nanny, the need to learn a new hospital, community, and yes, even a need to sit through four hours of EPIC training, again, to fulfill his educational prerequisite for his new hospital's orientation.
"You bet," his mentor said, "good luck with everything. This will be an incredibly exciting time for you" as the fellow left. Silently, the older doctor reflected on the excitement and stress that change brings. He could see that the young fellow was already gone, his attention turned elsewhere. Good for him: focused, excited, slightly anxious, but eager to move forward.
 |
 |
Good for her, he thought.
As the cool carbonated bubbles of a lime Lacroix slid down his throat, he sat back, eyes closing, thankful he wasn't on call this night.
Good for me, he thought.
-Wes
Wednesday, May 22, 2013
Status Check
For my regular followers, I apologize for being so negligent on updating this blog recently. Rest assured, I'm not dead, sick, or having family troubles - I'm just busy as hell. Taking a week off for attending a Scientific Session wreaks havoc on one's professional life these days.
I also find that I am more judicious about what I post these days. For me, I enjoy supplying original content to the blog-o-sphere rather than just links to cool articles. Sure, there's a place for that and, honestly, I could probably monetize this blog to a rockin', sockin' monetary powerhouse by doing little else, but that's not why I'm here. (My Adsense volume is about enough to pay for my server fees.) I do this, I've finally realized, because I enjoy writing, having a voice, and advocating for a cause. Doctors, you see, need a voice in this huge, increasingly corporate world of medicine these days. This is my place of refuge, my therapist, my touchstone for what matters.
So if I'm not posting all the time, consider it a sign of blogging maturity, not negligence. I'd rather post something of relevance rather than just drivel. Rest assured, there are things cooking in the background that I can't wait to share with you.
Thanks for hanging in there.
-Wes
I also find that I am more judicious about what I post these days. For me, I enjoy supplying original content to the blog-o-sphere rather than just links to cool articles. Sure, there's a place for that and, honestly, I could probably monetize this blog to a rockin', sockin' monetary powerhouse by doing little else, but that's not why I'm here. (My Adsense volume is about enough to pay for my server fees.) I do this, I've finally realized, because I enjoy writing, having a voice, and advocating for a cause. Doctors, you see, need a voice in this huge, increasingly corporate world of medicine these days. This is my place of refuge, my therapist, my touchstone for what matters.
So if I'm not posting all the time, consider it a sign of blogging maturity, not negligence. I'd rather post something of relevance rather than just drivel. Rest assured, there are things cooking in the background that I can't wait to share with you.
Thanks for hanging in there.
-Wes
Sunday, May 12, 2013
Heart Rhythm Society 2013 Scientific Session Wrapup
 |
| Opening Day HRS2013 |
First, we should acknowledge the efforts by the Heart Rhythm Society to limit the bling at the meeting. There were fewer large advertising displays, trucks driving through the streets with ads on top of them, and late-night rendezvous. Heart Rhythm Society handbags were like paper-thin grocery bags or recycled from prior years. Technology was used to a much greater extent, especially for smart phones, with an iPhone app meeting organizer that showed promise, but still needs some fine-tuning, especially in its scheduling functionality. As a result, aside from the Bill-Fest, the meeting felt more like a scientific session rather than a trade show.
Next we saw the evolution of thinking about the most common arrhythmia that electrophysologists treat: atrial fibrillation. Work on our understanding of atrial fibrosis via MRI assessment as it might pertain to long-term success of ablation was intriguing. Even more, since the introduction of the mystical focal impulse and rotor modulation (FIRM) mapping several years ago, attention is clearly returning back to understanding of the electrophysiology of atrial fibrillation from one of just approaching the disease anatomically. Many of the abstracts and studies presented revolved round (pun intended) an understanding of rotors or point sources (or both) for the genesis of atrial fibrillation. With this comes an entirely new vocabulary of cardiac electrophysiology with terms like "clockwise or counterclockwise rotor," "phase mapping," "frequency gradients," and "singularities." The black box nature of Topera Medical's FIRM mapping technique with it's 1960's music box-like maps (video) (that are difficult to interpret) adds to the mysticism of the moment, but it was clear that there was an appreciation that they are on to something.
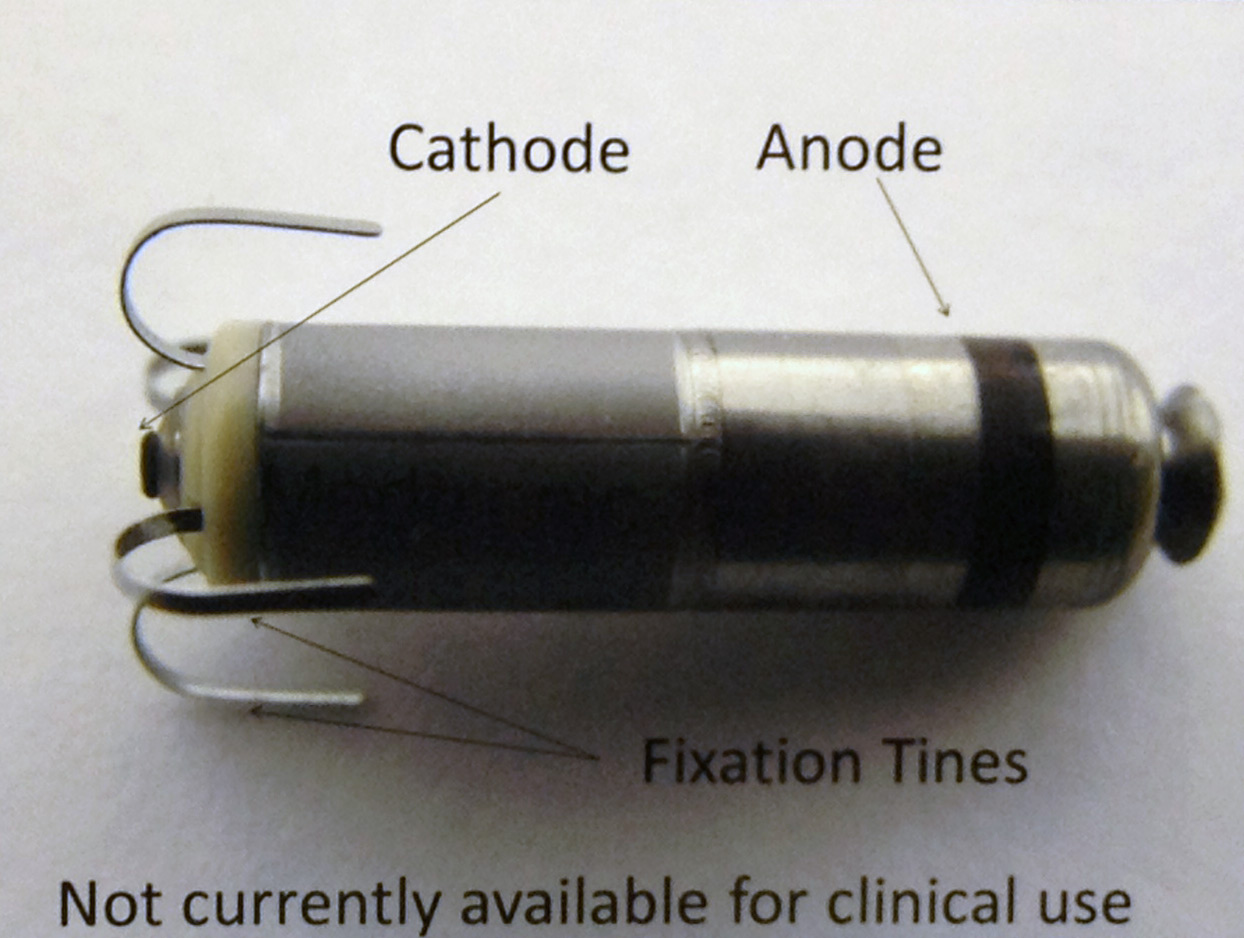 |
| Medtronic's version of the leadless pacemaker |
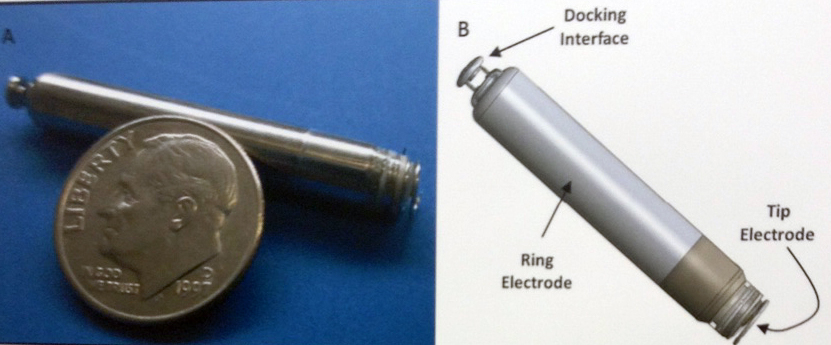 |
| Boston Scientific's version of the leadless pacemaker |
 |
| "Physician in Social Media" participants (L to R) Mr. Bob Coffield, yours truly, John Mandrola, MD, and Edward J. Schloss, MD |
-Wes
Thursday, May 09, 2013
Former President Bill Clinton Kicks off Heart Rhythm Society Meeting
While the above title is true, I admit that it was used more for garnering readership than suggesting that former U.S. President Bill Clinton had any real news to share with the world's pool of heart rhythm specialists. Oh how we hoped he would tell us about his pacemaker or implantable defibrillator that he had installed but, alas, it was not to be.
But the man can still draw a crowd. The large auditorium was filled by just about everyone that attended the conference it seemed, and he received a standing ovation upon entry. He seemed relaxed, but often glanced down a bit toward the floor when he spoke on occasion as he gauged the audience and weighed his commentary. For the first part of his talk, he stood behind the podium with teleprompters at its side, but unlike other presidents we know, those seemed more for those introducing the former president, rather than the former president himself.
Mr. Clinton was politely received by what could have been a viper's den of cardiac subspecialists. He's a gifted speaker and many of us were impressed by the depth and breadth of humanitarian efforts taken on by his Clinton Foundation following his stint in the White House. It was interesting to hear about all of the places hes been and the work his organization has done and at the outset. After the polished introductory video of the Clinton Foundation's excellent work was shown to the audience of political neophytes, many of whom had never seen a president before, it was clear no one was going to kill the baby seal. This was to be the Bill Show and sadly, there was never a single mention of the support team behind his foundation.
Still, there were moments in his speech that were captivating, especially the part where he described his own post-bypass ordeal of being told that he had fluid around his heart after his heart surgery and how he had to return to the operating room to have "my chest cracked open again" to manage it. We got a glimpse at his real fears and his real appreciation for his doctors and the technologies that cared for him. We heard how he ignored his chest tightness that occurred at rest after his bypass operation and how foolish he felt in retrospect after receiving two stents to a "badly mangled artery." Then we heard about how all of this lead his efforts to change his own dietary habits and to work with PepsiCo to develop policy for school kids to lower caloric intake of sugary drinks: "We found a way to change the system without having to take it down. That's what we need to do."
But his efforts to circle back to health care reform were disjointed much of the time as he waxed back and forth from his experience in Rowanda building clinics and providing logistics to the US, and then to comparing the relatively small Netherlands' health care system to the US's system, leaving many doctors wondering when he was going to say anything of real substance. Still, he tried to make the point about a "systems approach" and paying for "performance" rather than "procedures" as a partial way to fix things. He seemed to yearn for a simpler system than the one we've got. When asked point blank if his perspective on health care had changed since having his expensive care, he masterfully deflected the question by saying "I have a deeply personal regard for the American health care system, but we're limp at preventing errors." No doubt doctors who worked so hard on his behalf appreciated that comment.
Overall, most people I spoke with after the event seemed generally pleased with Mr. Clinton's performance, especially when he admitted the limitations of the Affordable Care Act (ACA). They liked his quip about how 99.5% of people's DNA are identical, yet we spend so much time focused on making sure others know the differences in the remaining 0.5% of their genome. It was clear he was a master at reaching across the aisle and he opined for a more collaborative approach to resolving our nation's health care problems. When asked whether he thought the ACA (Affordable Care Act) would fix what's wrong with America's health care system, he said honestly "Maybe. Maybe not." But he stuck with the partisan narrative of error management, paying by "performance" rather than procedures and asking doctors to do their part to fix the system, seemingly unaware of the 30% drop in RVU payments that took hold 1 January 2013 and the 2% Medicare payments to physicians that recently affected many members of his audience. It seems he felt doctors needed to do more, but many doctors wondered silently how much more we can take.
It was clear the Europeans I spoke with after the talk loved his speech. But they were also quick to point out another little fact: Mr, Clinton's appearance fee is somewhere in the order of $250,000. A quick fact check showed that was a gross understatement: it's closer to $500,000 or more. If this is the price we've paid for this hour of entertainment it's no wonder our health care's cost crisis is such a mess.
And if so, maybe Mr. Clinton should do his part for health care reform, too, and stay home.
And if so, maybe Mr. Clinton should do his part for health care reform, too, and stay home.
-Wes
Wednesday, May 08, 2013
HRS2013 Pre-meeting Reflections
This morning I sit quietly in my hotel room, contemplating the day ahead at the 2013 Heart Rhythm Society Scientific Sessions in Denver. Emotions clash.
On one hand, it will be great to see old friends an colleagues, to be spoon-fed information, and to relax. On the other hand, I find myself in an electrophysiologic angst: how I can spend the time upbeat knowing that the relative value of the work that heart rhythm specialists do was cut at least 30% on 1 January 2013, thanks to new billing codes that bundled multiple codes into one?
Can I afford to be here?
I do not say this lightly. Our first quarter's pay this year compared to last year was recently disclosed and the results were striking. Guys like me who have devoted years to our training, stood at bedsides for countless hours, and endured training that finally ended at age 36 (counting a brief two-year hiatus for a general medical officer stint as an ER physician for the US Navy), got a whopping 30% cut from CMS for the much of the procedure work we do, stealthy cloaked in codes.
It is real. It has happened. And its effects are being felt by many, real time, even now, at #HRS2013.
I realize in these economic times that many professions are feeling similar pressures. I am not here to lament nor ask for pity, but rather to describe. In many ways, I am lucky: lucky to have good friends, a fascinating skill, and wonderful colleagues and support staff to work with. But I wonder, how all of this will change things.
Certainly, we tabled our plans to hire another EP. No wonder EP fellows are finding it tough to get a job. Hospitals are not hiring. Wards are being consolidated. Pennies are being pinched, and so are staff. Patients are waiting more to see guys like me. Attendance at continuing education conferences is falling. While the effect on physician care "quality" are probably uncertain at best, but it is becoming quite obvious that "innovation" in my field of medicine as we've known it is stagnating or moving overseas.
It is all change - I get that - part of the Great Experiment of our nation's health care reformation project that is moving fast and furious to places unknown. But change is difficult. It shakes things up. Anxiety and restlessness at times like these can consume a psyche or, in ideal circumstances, lead to something new, something liberating, something better.
So off I go to the 2013 Heart Rhythm Scientific Sessions, hoping to keep my chin up, my ear to the ground, and my eyes open.
You never know what you might learn.
-Wes
Sunday, May 05, 2013
Physician Blogger Insights On Social Media
A recent e-mail exchange between myself (WGF) and fellow-physician bloggers John M. Mandrola MD (JMM), Edward J Schloss MD (EJS) and Ves Dimov MD (VDMD) resulted in some interesting insights about how physicians are using social media tools today. The following is a lightly edited version of the thread (used with permission). It began with an e-mail from Dr. Mandrola:
* * *
* * *
* * *
* * *
For those attending the 2013 Heart Rhythm Society Scientific Sessions in Denver, CO next week, Drs. Schloss, Mandrola and myself (as well as Robert Coffield, Esq. of the Health Care Law Blog fame) will be speaking at the Rhythm Theatre at 3:15pm on 10 May 2013 on Physicians in Social Media.
Hope to see you there!
-Wes
PS: For doctors considering the leap to social media, here's a basic Twitter Primer.
JMM: "In prep for our Social Media session at HRS2103. I was just wondering…
Do you guys keep a list of favorites on Twitter? I have lists--but they aren't very effective logistically. I was wondering if I designed a list--say the Mandrola-twenty--of folks I did not want to miss, I might be able to use a column on TweetDeck. Right now, I follow 350 people--and it's unwieldy. But yet I have trouble parsing because I'll look at an acct and say to myself, "this one's pretty good; I don't want to unfollow." Also, I find TweetDeck sometimes intrusive. I use the reg Twitter app and often post with Hootsuite--because it allows me to link to 4 social networks at once--LinkedIn, FB, Twitter etc.
What Twitter app do you all use on Computer? On smartphone?
Do you have thoughts on Facebook (FB)? I see from the WSJ they are making a comeback so to speak. For a while there, I thought they might be dead.
Do you agree that Twitter seems more amendable to professional needs--the sort we all use it for: things like links, communication with colleagues, filtering of important medical news. I tend to use FB, the little that I do, for real life things like family, in-real-life friends and cycling stuff, for instance. I wonder whether this is a correct distinction, as most of the major journals and medical society have a FB presence. And likewise, Twitter has plenty of willy-nilly stuff like Hollywood, Athletes etc. The young people I know use Twitter more like I use FB."
EJS: "I also use Twitter almost strictly for professional stuff, especially my posts. I follow a few non-professional accounts, but am really choosy in general about followers. For my own posts, I try to picture someone looking down my timeline and trying to decide whether I'm worth their time to follow. If I put a bunch of cr*p up, I figure they'd move on. Twitter is also the predominant source of my online persona, and I'm really careful about maintaining this.
Right now I follow 239 accounts and not all are terribly active. That keeps the stream manageable. I actually get a popup on the laptop for every thing that posts to my timeline. Because I use my laptop for all hospital charting, this means I see A LOT of tweets. That setup is clearly not for everyone, but I've gotten good at just glancing up to see who is posting before I commit to reading. The tweets fill the dead and mindless spaces we get during EHR data entry (which are a lot). At any given time I'll also have 5 or 6 searches running that also generate popups. Right now these include meaningfuluse, St Jude Riata, Barry Meier, EHR, @burbdoc, #HRS2013 among others. All of these also generate popups.
If you want to filter down you list to highlight your most important accounts, you can set up a list in Tweetdeck (and I'm sure in the other clients, as well). That will become a column, and you could turn on alerts for just this stuff if you're not at ADD as me. I have a friends/family list that shows up on my front page so I can quickly see if I missed anything good without having to obsessively scroll back through everything.
On the laptop, I use Tweetdeck. The old version before Twitter bought it is the best, but will stop working in a few days. I've put up the new version, but don't like it as much. The biggest drawback is not having the profile photo on the popups. With the old Tweetdeck, it was easier to see who was posting with just peripheral vision.
On the iPhone and iPad I use Tweetbot. It's really good and worth the few bucks it costs.
I'd tell any cardiologist starting on twitter to follow a bunch of health care journalists, along with you guys. The interactions you get with the journalists are really rewarding, and truly are a two way street.
I really don't see much professional purpose for Facebook for an EP doc. If you were a plastic surgeon or ortho, maybe there would be a role. I'm actually trying not to market directly to patients, given the nature of my practice. Maybe you could pick up some AF that way, but I suspect a lot of nervous people with sinus tach or PACs would clog up your office if you did that.
VDMD: Hi John and colleagues,
Here are my answers:
re: "Do you guys keep a list of favorites on Twitter?" -- yes, I have 2 lists - 1. list of favorite tweets that I use as bookmark, 2. list of "allergists on Twitter".
re: "Mandrola-twenty--of folks I did not want to miss" - yes, KevinMD has that - top 20 Twitters he doesn't want to miss. I follow few people - less than 100, I think, and only 50 of them tweet regularly.
re: "What Twitter app do you all use on Computer? On smartphone?" - I use TweetDeck on my home PC, HootSuite at work (TweetDeck is blocked), and mobile Twitter on my Android phone. I "favorite"/bookmark the links I want to check later.
re: "Do you have thoughts on Facebook?" - Facebook (FB) is here to stay - until a new network replaces it. You have to use it to stay relevant if you have a blog. In addition, people look at the number of your likes to see how large a following you have as a blogger. FB has limitations and can be annoying but Google Plus is not a replacement yet. FB will evolve for sure, they are a young, aggressive company, and will keep searching for ways to combat "user fatigue".
These are some quick thoughts. Please let me know if you would like me to expand on any of these.
WGF: "Twitter is for the person with ADHD while blogs are for the obessive compulsive.
Twitter, by its very nature, has a low barrier for entry and can serve as an information "gatherer" initially. I'd encourage people to LURK first. It's easy to use and feeds lots of information of interest quickly to docs. As a "MUST HAVE" for doctors, they should follow the journals they subscribe to: Heart Rhythm, NEJM, Circulation, JACC, etc, as well as major news orgs: WSJ, CNN breaking news, local newsorgs or radios, etc. I also follow Steve Colbert for a laugh once in a while.
Twitter is also VERY useful for collaboration (as we have seen) and for "hunters" of information by using your network. I especially encourage follows of docs of the same subspeciality.
Facebook is for family/personal friends for me. No patients there. I find it's the best way to stay connected with my kids after they're out of the house.
As far as lists are concerned: I think they're a waste of time. I tried it, but since you cant send a targeted message or "tweet" to a list, it's only a way to group accounts.
I use Echofon on my iPhone (like it better than Hootsuite) - easy user interface and free. I use Tweetdeck on my PC and MAC.
I follow 446 people - probably too many - but it's a broad group that includes right and left-wing health care thinkers, IT nerds, politicians, bloggers, and you guys, and Steve Colbert. :)
Perhaps the most amazing use for Twitter (recently) was the immediacy of info provided there during the Boston bombings. It was unbelieveable how quickly updates happened and totally smoked the main news organizations. Imagine if doctors had a similar network at times of crisis! That's why I think it would be VERY cool to push that concept with our audience. Consider, for example, the need to get an EKG interpretation immediately (check my recent Twitter stream to see an example of just that) - lots of folks weighed in with ideas - some good - some bad - but in the end it was vetted pretty well.
Looking forward to this..."
VDMD: re: Journals on Twitter - I'm not a big fan of these. It's mostly the administrative staff pushing some articles they have picked. RSS feeds for the journals are much better, in my opinion. They save time and include most (all) articles of each issue.So there you have it. A sneek peak behiund the social media physician curtain on their take of current software, apps, and uses they find for social media in health care today.
For those attending the 2013 Heart Rhythm Society Scientific Sessions in Denver, CO next week, Drs. Schloss, Mandrola and myself (as well as Robert Coffield, Esq. of the Health Care Law Blog fame) will be speaking at the Rhythm Theatre at 3:15pm on 10 May 2013 on Physicians in Social Media.
Hope to see you there!
-Wes
PS: For doctors considering the leap to social media, here's a basic Twitter Primer.
Saturday, May 04, 2013
The FDA Azithromycin Softshoe and Why It Matters
This week, a Danish study by Svanstrom and colleagues appeared in the New England Journal of Medicine that failed to show significant cardiovascular risk to azithromycin compared to other antibiotics in the Danish national health care system. This report was in direct contradiction to an earlier report from Ray, et al. published in the New England Journal of Medicine (and widely hailed in press) that suggested a significant risk of cardiovascular death attributed to azithromycin compared to other antibiotics in a Tennesse Medicaid population - and a report that the FDA used to justify the wide dissemination of a Drug Safety Communication for azithromycin.
While I have been quite critical of the conclusions drawn by Ray, et al. before, I was even more surprised by the Drug Safety Communication for azithromycin issued by the FDA that basically said: "any time a patient has a bunch of conditions that are known to cause prolonged QT interval, be careful prescribing azithromycin." Such warnings, of course, should apply to any drug that could cause prolongation of QT interval, but for some unclear reason, the FDA felt they had to act in the case of azithromycin.
Now it seems the FDA doing a softshoe on their earlier warning regarding azithromycin, trying to justify their warning that was based on retrospective data-mining techniques drawn from diagnosis and treatment codes, not randomized trials.
In a perspective piece from Andrew D. Mosholder et al, from the FDA that accompanied the report from Svanstrom et al, the authors acknowedge the many limitations of the original study by Ray et al.:
Fortunately, I think the FDA folks mean well: they give us salient advice in their final paragraphs of their perspective piece explaining their mistake. Things like "Clinicians must consider the arrhythmogenic potential not only of azithromycin but also of potential alternative antibacterial drugs." and "The risks and benefits of antibacterial therapy should be considered in prescribing decisions."
No kidding.
But we will not see a black box warning retracted - that would be too obvious. Nor will we see extensive news coverage about these new findings regarding this antibiotic's cardiovascular safety - that doesn't grab the main stream media's attention.
What we have, instead, is something much more concerning to me when the members of our own FDA make claims based on poor data: irrelevance.
Publishing warnings on QT prolongation that should apply to any drug administered to the patient that is older, bradycardic, with low potassium or magnesium levels, or already on known drugs that can cause prolonged QT - generates irrelevant noise for doctors. Like the Boy Who Cried Wolf, we risk compromising the FDA's relevance to patient safety. When they spend time on retrospective data-mining exercises that find risks in the neighborhood of 1 in 100,000, they risk failing to report important deaths related to new technologies with an incidence of at least 3 in 16,000 that reside in their own MAUDE database.
In today's internet age, doctors don't need any more Big Data-driven safety noise, we need razor-sharp analytic safety focus.
-Wes
While I have been quite critical of the conclusions drawn by Ray, et al. before, I was even more surprised by the Drug Safety Communication for azithromycin issued by the FDA that basically said: "any time a patient has a bunch of conditions that are known to cause prolonged QT interval, be careful prescribing azithromycin." Such warnings, of course, should apply to any drug that could cause prolongation of QT interval, but for some unclear reason, the FDA felt they had to act in the case of azithromycin.
Now it seems the FDA doing a softshoe on their earlier warning regarding azithromycin, trying to justify their warning that was based on retrospective data-mining techniques drawn from diagnosis and treatment codes, not randomized trials.
In a perspective piece from Andrew D. Mosholder et al, from the FDA that accompanied the report from Svanstrom et al, the authors acknowedge the many limitations of the original study by Ray et al.:
"The study by Ray et al. has limitations that are intrinsic to obervational, nonrandomized clinical studies. In particular, nonrandomized studies cannot exclude the possibility that patients receiving a drug under evaluation differ from the control patients in some important but undetected way, causing bias in the results. Such confounding may bias comparisons not only between patients receiving antibacterial drugs and those receiving no antibacterials but also between patients receiving different antibacterials."Yet in the very next paragraph of the FDA member's perspective piece, they persist in their indifference to their prior statement regarding the bias inherent to Ray et al.'s report and decide to focus on timing:
"Despite these caveats, the results presented by Ray et al. warrant serious attention. A chief strength of the study is the time-limited pattern of the risk: the azithromycin-associated increase in rates of death from any cause and from cardiovascular causes spanned days 1 through 5, reflecting the typical 5-day duration of azithromycin administration (e.g., Zithromax Z-pak)."The FDA authors refuse to believe that there could be any other confounding variables that might have occurred in the first five days of hospitalization that lead to the increased cardiovascular risk seen in their azithromycin-treated group. It is more important, I guess, to support retrospective data-mining and statistical data manipulation of diagnosis and procedure codes. This, you see, they must support. Big Data in our new era of expanded codes and computers is to be our new saving grace, you see.
Fortunately, I think the FDA folks mean well: they give us salient advice in their final paragraphs of their perspective piece explaining their mistake. Things like "Clinicians must consider the arrhythmogenic potential not only of azithromycin but also of potential alternative antibacterial drugs." and "The risks and benefits of antibacterial therapy should be considered in prescribing decisions."
No kidding.
But we will not see a black box warning retracted - that would be too obvious. Nor will we see extensive news coverage about these new findings regarding this antibiotic's cardiovascular safety - that doesn't grab the main stream media's attention.
What we have, instead, is something much more concerning to me when the members of our own FDA make claims based on poor data: irrelevance.
Publishing warnings on QT prolongation that should apply to any drug administered to the patient that is older, bradycardic, with low potassium or magnesium levels, or already on known drugs that can cause prolonged QT - generates irrelevant noise for doctors. Like the Boy Who Cried Wolf, we risk compromising the FDA's relevance to patient safety. When they spend time on retrospective data-mining exercises that find risks in the neighborhood of 1 in 100,000, they risk failing to report important deaths related to new technologies with an incidence of at least 3 in 16,000 that reside in their own MAUDE database.
In today's internet age, doctors don't need any more Big Data-driven safety noise, we need razor-sharp analytic safety focus.
-Wes
Friday, May 03, 2013
EKG Du Jour #31: A Case of Chest Pain
A 61 year old patient presented to your ER with chest pain, low blood pressure, and this EKG:
Now before you leap to the answer at the link provided below, ask yourself:
(a) What is this?
(b) What could cause this?
(c) How would you manage it?
And when you've really thought about it, click here for the answer but be prepared to describe what you see and what you'd do next.
-Wes
P.S.: (Yeah, I'm giving the answer now because it's Friday)
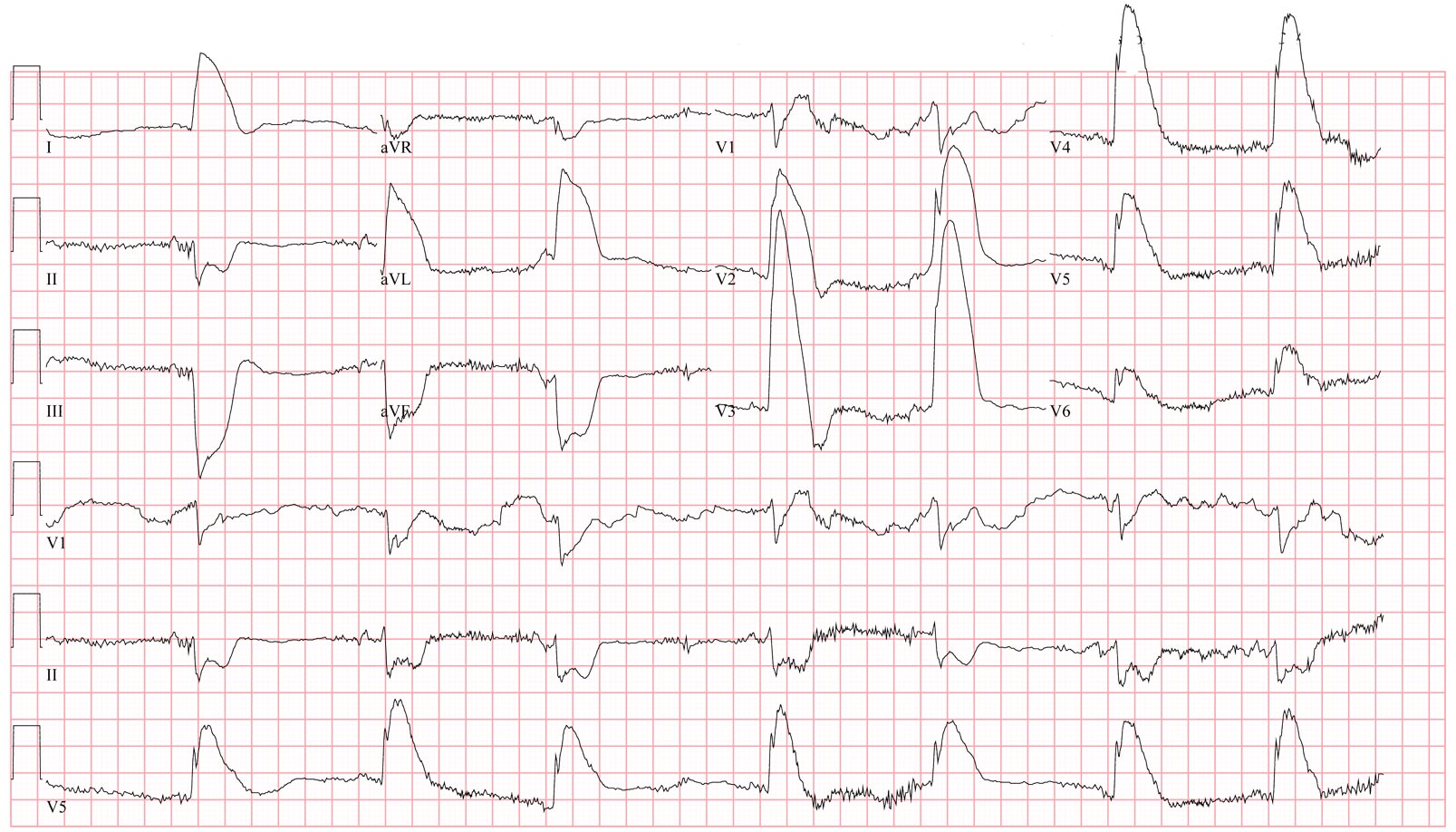 |
| (Click image to enlarge) |
Now before you leap to the answer at the link provided below, ask yourself:
(a) What is this?
(b) What could cause this?
(c) How would you manage it?
And when you've really thought about it, click here for the answer but be prepared to describe what you see and what you'd do next.
-Wes
P.S.: (Yeah, I'm giving the answer now because it's Friday)
Wednesday, May 01, 2013
Dr. John M: Autonomy vs beneficence? Shared decision-making in the patient considered for an ICD
Dr. Lin and Matlock were quoted in Dr. John Mandrola's post today:
-Wes
"Convincing physicians to engage in shared decision-making is a complex undertaking, as physicians may believe that they are following clinical practice guidelines in strongly recommending an ICD to eligible patients. Because quality-improvement efforts often focus on increasing physician adherence to guidelines and reward physicians for clinical processes or outcomes rather than high-quality decision-making, the message to physicians is that guideline adherence, rather than individualized care, is best."For implantable cardiac defibrillator (ICD) implanting physicians everywhere, if you read nothing else today, read this excellent post by Dr. John M.
-Wes
Subscribe to:
Comments (Atom)
