It's very generous of Sanolfi-Aventis's marketing department to make this offer (pdf) for me to serve as an "advisor" for dronedarone today, but seriously, I was a bit skeptical that they wanted my "feedback on the reasons for and against utlilization of Multaq® in the appropriate patient as well as to understand communication and educational needs with regard to Multaq® and the atrial fibrillation state in general."
Where were they when the drug launched? Might it be because it's this drug has not been quite the blockbuster they'd hoped for?
But of course I'd never be swayed to use more of this drug by this important consulting work.
No, really.
-Wes
P.S.: To Sanolfi-Aventis marketers: Please update your prescriber database with my correct workplace.
Friday, March 26, 2010
Thursday, March 25, 2010
Vacation
When I was a young boy, I remember the sleepless nights in anticipation of the upcoming family vacation. The day of the trip, my father would wake us at 4AM and we'd stagger to the Oldsmobile stationwagon in pajamas with pillows in tow, then climb into the bench-like back seat in the pre-warmed car. As the car pulled out from our driveway, we'd quickly settle in to another hour or two of sleep as my father tried to beat rush-hour traffic. Later, we'd wake to the sun hitting the windows of the car and peer our the window to an unfamiliar vastness, heading to somewhere new, exciting.
Now it is much different, but that is life, I suppose.
Now cases and schedules are either arranged before or after your absence from work. It is not wise to just to schedule patients, lest your productivity wane. Cell phones accompany you, capable of constant internet (and therefore e-mail) connection worldwide. With a handy-dandy key fob, internet access to patient charts can follow. Conference calls are a mere international 800 number and conference number away. I've even noticed by physician blogging colleagues Twittering from their vacation spots.
Which leads me to wonder, is this vacation?
I don't know, but the chance to be in a new spot for a while soaking some rays, playing some tennis and taking a boat ride on occassion sure is different than what I'm doing here, so this 'ol boy's gonna be outta here for vacation for a bit.
Hold down the blog-o-sphere, okay?
-Wes
Now it is much different, but that is life, I suppose.
Now cases and schedules are either arranged before or after your absence from work. It is not wise to just to schedule patients, lest your productivity wane. Cell phones accompany you, capable of constant internet (and therefore e-mail) connection worldwide. With a handy-dandy key fob, internet access to patient charts can follow. Conference calls are a mere international 800 number and conference number away. I've even noticed by physician blogging colleagues Twittering from their vacation spots.
Which leads me to wonder, is this vacation?
I don't know, but the chance to be in a new spot for a while soaking some rays, playing some tennis and taking a boat ride on occassion sure is different than what I'm doing here, so this 'ol boy's gonna be outta here for vacation for a bit.
Hold down the blog-o-sphere, okay?
-Wes
Wednesday, March 24, 2010
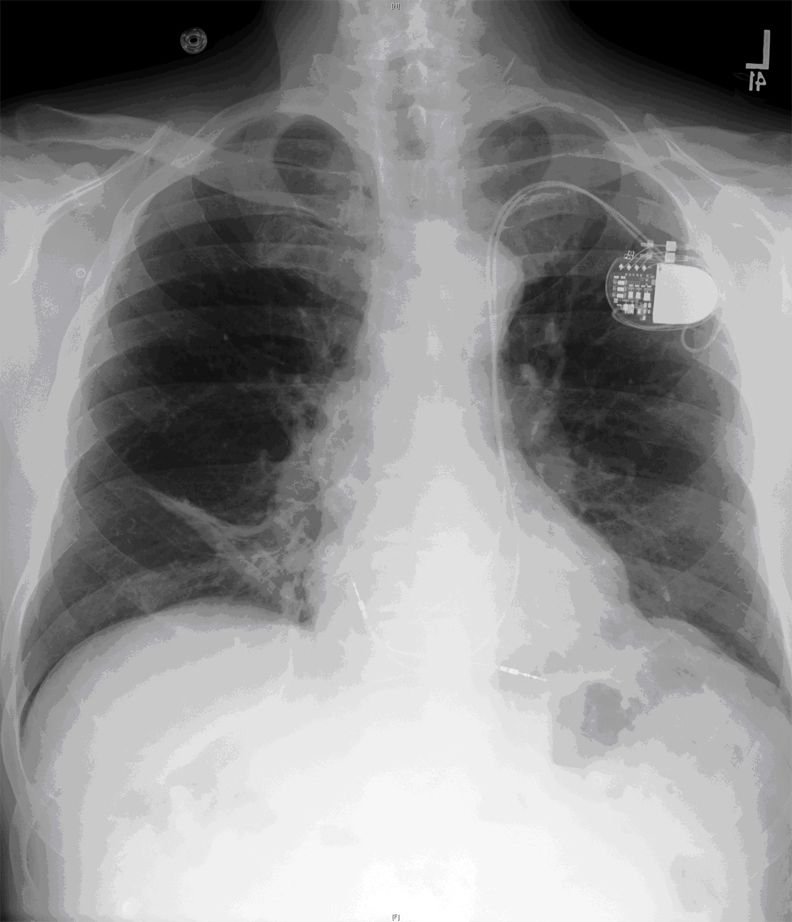
Just Another Friday Pacemaker
Monday, March 22, 2010
Health Care's Pyrrhic Victory
It is hard to put into words what the health care reform bill about to be signed today by the President means to doctors as a group. After all, doctors were as divided about the health care reform bill as the rest of the country was.
The birth of the bill was anything but pretty with infighting, favors, legislative slights-of-hand, enticements, and even threats occurring, but like a difficult breech birth, it still brought forth our new legislative baby. We have learned much from the bill's gestation:
Like King Pyrrhus of Epirus, whose army suffered irreplaceable casualties in defeating the Romans during the Pyrrhic War, the President, the Speaker, and our Congress has set us on a new course.
Hail to the victors.
Let's just hope their victory was worth it.
-Wes
The birth of the bill was anything but pretty with infighting, favors, legislative slights-of-hand, enticements, and even threats occurring, but like a difficult breech birth, it still brought forth our new legislative baby. We have learned much from the bill's gestation:
First, our legislators in Washington rarely read complicated bills before them. Sound bites carry the day when important policy is at stake.Yet here we are.
Second, the people have felt too disenfranchised and disempowered for too long. They are tired of feeling powerless to the ever-increasing costs in health care, yet still insist on the new, the shiny, the whizbang. This cultural disconnect will continue to plague our policy makers moving forward.
Third, we have watched the centralization of power and money in health care cede decisions to our Big Box retail-purveyors of health care delivery in favor of the local physician and the patient. Now with government regulators and oversight committees and health czars, a new world order is now upon us. Will it be better? Hard to know. But costs concerns will take precedence over health concerns from time to time, and America is going to have a hard time adjusting to this new paradigm. For doctors, there will be a push for greater efficiencies to care for the greater volume of patients yet paradoxically, taking one's time and being inefficient is usually synonymous with patient satisfaction.
Fourth, despite the outcome of the vote in the House of Representatives, the government isn't perfect either. Like the Big Box retailers they aim to regulate, the government is also centralized, oversized, disorganized, and slovenly yet affects every corner of our country. Whether you're a Southern Baptist or Jewish Rabbi, better get ready for what the government's health board says, because their decision we be the same for all of us. God forbid they get it wrong: as we've seen, changing things takes a while. Still, it's here, we're all going to have to chew on it this legislation, digest it, and expel the parts that stink.
Perhaps more than anything is that the war has begun that pits the power of our current health care "stakeholders" and our government. It is sad that it's come to this - that we could not collectively determine a simpler way to provide health care to our populace with local self-determination that preserves innovation and economies of scale over central oversight of issues affecting our most personal health decisions.
Like King Pyrrhus of Epirus, whose army suffered irreplaceable casualties in defeating the Romans during the Pyrrhic War, the President, the Speaker, and our Congress has set us on a new course.
Hail to the victors.
Let's just hope their victory was worth it.
-Wes
Saturday, March 20, 2010
Toward Black Sunday
From an anonymous question in my comments:
But I find it interesting how prescient my post on Our Healthcare Hindenburg appears in retrospect now. We are in crisis, just as predicted. We must act. We have a President who has thrown down the glove to his constituents, and if nothing else, should be admired for his commitment at trying to tackle this seemingly impossible challenge. But behind the President, we also have a group with a political philosophy that thinks nothing of ripping up Mieg's field in Chicago because, well, they can. Like the pilot who tried to land there the day after the carnage, we'll be left to clean up the mess. But if the bill passes, no one will want to touch this. Not Democrats, certainly, fearing the results of the November elections, and certainly not Republicans since they didn't like the bill anyway. Who the hell wants to raise taxes and cut benefits for seniors? Are you crazy?
Doctors, despite our relationship with our patients (which will endure), are really mere pawns at this point. The bill appears to throw some money to support primary care physicians, and that's a good thing. But our "leadership" (as defined, almost comically, as the American Medical Association) has endorsed the bill, even though there is no "doctor fix" for the flawed SGR payment formula to physicians. Why? Because to do so would add $320 billion to the current CBO "scoring" of the bill and take the bill over the dreaded $1 trillion dollar amount. (Funny how $940 billion is okay, though). Thank you, AMA, for taking such a firm stand. All doctors are looking forward to the 21% pay cut and are waiting anxiously to see how the AMA will "hold Congress's feet to the fire."
Meanwhile, more predictions coming true: we have hospitals raising rates at an unprecedented rate just to cover costs, despite (at least here in Chicago) some with near record returns at a time of an unprecedented economic downturn. We have insurers, cranking their rates to new heights, crying foul that hospitals are raising theirs. (How unfair!) We have huge corporate displays from medical device, pharmaceutical, and electronic medical record companies at the American College of Cardiology meeting in Atlanta, standing to gain handsomely with the larger portion of insured coming their way. Certainly we would never want to rain on their profit parade - they're just trying to run a business, based much in part on our government-funded health entitlement programs.
Better to publish, conveniently and just before the vote, the inflated salaries of doctors as told by a recruiting company, so those filthy rich doctors can be further slapped into submission for making too much money. Politically, those salaries are easy pickin's, especially if you compare those salaries to their physician-counterparts overseas (just don't mention what it costs to train and insure those same US doctors).
This is not to say doctors have now had a part in price inflation in health care, they have. But the days of ordering an EKG, stress test, echocardiogram and nuclear scan on every patient who presents with chest pain are over. And rightly so. But in a government-developed system that rewards payments for procedure rather than the time spent with a patient, what did you expect? Wouldn't a time-based system make so much more sense? But alas, that would not be productive in the eyes of the business-savvy health care institutions. More time means fewer patients, so sorry, dear doctor, that won't work - take this lower salary instead.
So what does all this mean for doctors? First, doctors will still be seeing patients Monday after the vote. But the effects of the health care reform efforts have already been felt by today's doctors unwilling to wait until the final shoe drops. More and more doctors are selling their practices and moving to the relatively sheltered environs of a large hospital system who, at least for now, will subsidize their salaries because they generate the patient volume for these health systems. Stalwart doctors not bowing to these health systems are turning to a concierge-style pricing alternatives to compensate for the cuts to payment rates received from insurers and Medicare. For those private practice doctors, this model restores a modicum of realism to health care delivery for both the doctor and the patient and makes sense. Look for it to become the norm as these times press ahead...
...at least until state licensure prerequisites prohibit such concierge payments. Then, if the bill passes, we'll all be government employees, one way or another.
-Wes
Dr Wes, can you explain how this house vote and recon is going to affect doctors? I note that in a MSNBC article they say they'll increase primary care reimbursments for MediCAl to that of Medicare in 2013,so are they leaving specialists, proceduralists out of this deal? where would the Primary refer the patient if speciali(s)ts don't take the MediCAL? Would this reform have impact on doctors pay? Insur, Drug companies, Hospitals all seem Ok with it's passage.I have no idea what is going to happen on Sunday when the house bill as amended (thanks to Scott Hensley for this link) is voted on. Like many, I have a son who is a recent college graduate working part-time with no health insurance and an incredibly bleak job market before him. While I can afford insurance for him, it is incredibly expensive. I am sure others are not so fortunate. I would be foolish to say we do not have a serious problem in American health care right now.
But I find it interesting how prescient my post on Our Healthcare Hindenburg appears in retrospect now. We are in crisis, just as predicted. We must act. We have a President who has thrown down the glove to his constituents, and if nothing else, should be admired for his commitment at trying to tackle this seemingly impossible challenge. But behind the President, we also have a group with a political philosophy that thinks nothing of ripping up Mieg's field in Chicago because, well, they can. Like the pilot who tried to land there the day after the carnage, we'll be left to clean up the mess. But if the bill passes, no one will want to touch this. Not Democrats, certainly, fearing the results of the November elections, and certainly not Republicans since they didn't like the bill anyway. Who the hell wants to raise taxes and cut benefits for seniors? Are you crazy?
Doctors, despite our relationship with our patients (which will endure), are really mere pawns at this point. The bill appears to throw some money to support primary care physicians, and that's a good thing. But our "leadership" (as defined, almost comically, as the American Medical Association) has endorsed the bill, even though there is no "doctor fix" for the flawed SGR payment formula to physicians. Why? Because to do so would add $320 billion to the current CBO "scoring" of the bill and take the bill over the dreaded $1 trillion dollar amount. (Funny how $940 billion is okay, though). Thank you, AMA, for taking such a firm stand. All doctors are looking forward to the 21% pay cut and are waiting anxiously to see how the AMA will "hold Congress's feet to the fire."
Meanwhile, more predictions coming true: we have hospitals raising rates at an unprecedented rate just to cover costs, despite (at least here in Chicago) some with near record returns at a time of an unprecedented economic downturn. We have insurers, cranking their rates to new heights, crying foul that hospitals are raising theirs. (How unfair!) We have huge corporate displays from medical device, pharmaceutical, and electronic medical record companies at the American College of Cardiology meeting in Atlanta, standing to gain handsomely with the larger portion of insured coming their way. Certainly we would never want to rain on their profit parade - they're just trying to run a business, based much in part on our government-funded health entitlement programs.
Better to publish, conveniently and just before the vote, the inflated salaries of doctors as told by a recruiting company, so those filthy rich doctors can be further slapped into submission for making too much money. Politically, those salaries are easy pickin's, especially if you compare those salaries to their physician-counterparts overseas (just don't mention what it costs to train and insure those same US doctors).
This is not to say doctors have now had a part in price inflation in health care, they have. But the days of ordering an EKG, stress test, echocardiogram and nuclear scan on every patient who presents with chest pain are over. And rightly so. But in a government-developed system that rewards payments for procedure rather than the time spent with a patient, what did you expect? Wouldn't a time-based system make so much more sense? But alas, that would not be productive in the eyes of the business-savvy health care institutions. More time means fewer patients, so sorry, dear doctor, that won't work - take this lower salary instead.
So what does all this mean for doctors? First, doctors will still be seeing patients Monday after the vote. But the effects of the health care reform efforts have already been felt by today's doctors unwilling to wait until the final shoe drops. More and more doctors are selling their practices and moving to the relatively sheltered environs of a large hospital system who, at least for now, will subsidize their salaries because they generate the patient volume for these health systems. Stalwart doctors not bowing to these health systems are turning to a concierge-style pricing alternatives to compensate for the cuts to payment rates received from insurers and Medicare. For those private practice doctors, this model restores a modicum of realism to health care delivery for both the doctor and the patient and makes sense. Look for it to become the norm as these times press ahead...
...at least until state licensure prerequisites prohibit such concierge payments. Then, if the bill passes, we'll all be government employees, one way or another.
-Wes
Friday, March 19, 2010
A Piece of Equipment Every Electrophysiology Lab Needs
File this under the "totally cool" file.
I've written several posts on this blog about close entomological encounters that occasionally occur during pacemaker implants. No doubt others have experienced similar moments in other operating rooms or procedure rooms around the world.
Now, thanks to clever military engineers working to eradicate malaria, a new approach is being tested on mosquitoes that would have applicability in every operating room across the country to keep the flying foreign bodies at bay: using a LASER to fry the buggers' wings (See the third video at the link).
Awesome.
-Wes
I've written several posts on this blog about close entomological encounters that occasionally occur during pacemaker implants. No doubt others have experienced similar moments in other operating rooms or procedure rooms around the world.
Now, thanks to clever military engineers working to eradicate malaria, a new approach is being tested on mosquitoes that would have applicability in every operating room across the country to keep the flying foreign bodies at bay: using a LASER to fry the buggers' wings (See the third video at the link).
Awesome.
-Wes
Concierge Cardiology
Concierge medicine is not just for internal medicine or primary care any more, it seems the concept is starting to take hold in cardiology, too:
Starting April 1, patients at Pacific Heart Institute can choose one of four plans for care. In the first option, they pay no "participation fee." In the next, called "Select," they pay $500 a year for priority appointments, warfarin adjustments, defibrillator and pacemaker follow-up, notification of non-urgent lab, and test results, according to Pacific Heart Institute.-Wes
In the third, called "Premier," they pay $1,800, for everything in "Select," plus e-mail communication with their doctor, same-day visits during regular office hours, priority lab testing and scheduling of diagnostics, free attendance at speaker seminars on cardiovascular issues, and a dedicated phone line to reach an institute nurse.
In the fourth, "Concierge," they pay $7,500 for everything in "Premier," plus direct 24-hour access to a cardiologist via pager, e-mail, text message, plus the patient's PHI cardiologist's personal cell phone, annual personalized cardiovascular wellness screening, night and weekend access to a PHI cardiologist for hospital or emergency services, (regardless of whether he or she is on call) same-day visits with the cardiologist, evening and weekend office appointments and personal calls from the cardiologist.
Thursday, March 18, 2010
A Case of an Appropriate Inappropriate Shock
He was 60 year old man who underwent implantation of an implantable cardiac defibrillator (ICD) implant approximately 3 years prior who was returning to the clinic for routine follow-up. He felt well and had no other complaints.
He was connected to the EKG and the programmer's wand placed over the device. I interrogated his device and when the initial screen appeared, there it was: a single shock from his device, received two weeks ago.
"Mr. Smith, are you aware that you had an ICD shock about two weeks ago?"
"Yeah."
"Why didn't you call us?"
"I don't know."
"Did it bother you?"
"Not really."
"Why not?"
There was a pause. I looked up from the programmer and took a quick look at him. He was looking away. Instantly, I realized the answer.
"Never mind," I answered. "Here, I'll just change the VT detect rate."
"No, doc, please don't. Leave the settings as they are."
"Are you sure?"
"Absolutely." He looked at me as I doubted him. "Seriously doc, I mean it."
"How come?"
"She liked it."
-Wes
He was connected to the EKG and the programmer's wand placed over the device. I interrogated his device and when the initial screen appeared, there it was: a single shock from his device, received two weeks ago.
"Mr. Smith, are you aware that you had an ICD shock about two weeks ago?"
"Yeah."
"Why didn't you call us?"
"I don't know."
"Did it bother you?"
"Not really."
"Why not?"
There was a pause. I looked up from the programmer and took a quick look at him. He was looking away. Instantly, I realized the answer.
"Never mind," I answered. "Here, I'll just change the VT detect rate."
"No, doc, please don't. Leave the settings as they are."
"Are you sure?"
"Absolutely." He looked at me as I doubted him. "Seriously doc, I mean it."
"How come?"
"She liked it."
-Wes
Wednesday, March 17, 2010
Part II - Compare and Contrast: A Chance to Size Up Two Health Care Systems
BACKGROUND
For those who are landing on this page for the first time, be sure to read the background FIRST to these case presentations. The intent here is to compare and contrast two patients, one insured and the other uninsured, from the United States and England as care is delivered today. The US cases are described in detail in this blog and the corresponding cases, British-style, are described on Sarah Clarke, MD's blog from England.
CASE #1: The U.S. Case of Mr. Thurgood Powell
The ER radio sounds: (*bleeeeee, deeeeeeeeeppppp*) "Rampart, we have a 57 year old white male en route with a 45 minute history of substernal chest pain and diaphoresis. Initial single-lead EKG discloses ST segment elevation. One ASA given, nitro given, BP 96/47, pulse 110, respirations 22, pt diaphoretic..."
ER doctor: "Code cor activated. Cath lab ready. Proceed as soon as possible."
Pt arrives. Looks poorly. A 12-lead EKG is obtained in the ER and confirms an evolving acute anterior myocardial infarction. There is no contraindication to proceeding directly to cath lab. Given loading dose of Plavix, integrelin. Shuttled to lab. Angio performed. 95% LAD stenosis and significant 3-vessel disease is noted. Ventriculogram not performed due the patient's condition. His BP drops, intraaortic balloon pump placed. Due to his age and lack of comorbidities, it is decided to place a drug-eluting stent in LAD artery. Aside from some VT during case and one episode of ventricular fibrillation during his procedure requiring countershock, but patient tolerates remarkably well. Patient is transfered to ICU.
After the dust settles, hospital administration comes to take patient's valuables and to register Mr. Powell. They inquire about his insurance: he produces a platinum policy card from Blue Cross Blue Shield of Illinois which Mr. Powell chose amongst several insurance policies offered by his employer. He could cover his entire family for approximately $400 per month ($200 per paycheck): total annual outlay $4800. Employer also picks up a more significant portion of the cost (approximately $14,000 per year) but can deduct this amount from their profit for tax purposes. Mr. Powell cannot deduct the price of his insurance from his income amount and has a $5000 annual family deductible. Also, Mr. Thurgood's income falls into the 33% federal tax bracket ($67,643 per year). Still, all is good - he's covered.
Mr. Powell is started on Toprol XL 25 mg daily, Altace, aspirin, Plavix, and Crestor - all at the doctor's discretion (He is young, after all). Patient has development of congestive heart failure on day two, requires ongoing balloon pump support. Some atrial fibrillation occurs, requiring titration of medications to control. Echocardiogram performed to assess LV function. Balloon pump but eventually is weaned on Day #3. He leaves the ICU on Day 4. His room outside the ICU is private (due to infection control efforts, they say) and equipped with a flat screen TV from which he orders his food (it is, after all, a brand new heart hospital that has been tastefully appointed.) He spends two more days on the ward and then is discharged to follow-up in Clinic in one month.
Pt returns home and later receives a bill for his hospital stay. On his Explanation of Benefits, he notices a total bill for $180,000. Insurance has agreed to pay about $150,000 due to a pre-negotiated arrangement of the insurer with the hospital. The insurer has likewise negotiated with the employer to offer a price point with a comfortable profit "spread." Mr. Powell is not responsible for understanding the difference - he just has to pay his annual deductable of $5000.
Despite his care, Mr. Powell continues to have ongoing angina. Because of his recurrent pain, he is admitted and another angiogram performed which was unchanged. It is decided that because of his young age and pain refractory to medical therapy, he is referred to bypass. He is seen by the surgeon the same day, and elective surgery scheduled for the following day.
His post operative stay is uncomplicated and he returns home in 4 days. Cost for surgery and hospital stay: About $100,000.
Approximately 6 weeks later, Mr. Powell notes palpitations and lightheadedness. He returns to ER where his is found to be in sustained monomorphic ventricular tachycardia. Another angiogram performed. All bypass vessels are open and his native disease unchanged. A dual chamber ICD is scheduled for next day of manufacturer of the electrophysiologist's choice* (patient had atrial fibrillation in the past, after all) and implanted uneventfully. Mr. Powell later returns home.
Again a bill is sent to his home: cost of hospitalization with ICD implant $160,000. Insurance has prenegotiated a lower price with hospital - $110,000 - but has agreed to pay the full negotiated amount with the remainder "forgiven" as far as Mr. Powell is concerned. Mr. Powell is amazed by the state-of-the art technology installed in his chest.
Mr. Powell follows up in two weeks after his surgery with his electrophysiologist, two weeks after that with his cardiologist, and about a month later, his internist. He is followed for his ICD every three months thereafter. Home monitoring of his ICD is instituted on his first follow-up visit. The device company sends the monitor to his home, free of charge.
CASE #2: The U.S. Case of Mortimer T. Schnerd
The ER radio sounds: (*bleeeeee, deeeeeeeeeppppp*) "Rampart, we have a 43 year old white male en route with a 45 minute history of substernal chest pain and diaphoresis. Initial single-lead EKG discloses ST segment elevation. One ASA given, nitro given, BP 96/47, pulse 110, respirations 22, pt diaphoretic..."
ER doctor: "Code cor activated. Cath lab ready. Proceed as soon as possible."
Pt arrives. He looks poorly. A 12-lead EKG is obtained in the ER and confirms an evolving acute anterior myocardial infarction. There is no contraindication to proceeding direct to cath lab. Given loading dose of Plavix, integrelin. Shuttled to lab. Angio performed. 95% LAD stenosis and severe underlying 3-vessel disease is noted. Ventriculogram not performed. His BP drops, intraaortic balloon pump placed. Due to his age and lack of comorbidities, it is decided to place a drug-eluting stent in LAD artery. Aside from some VT during case and one episode of ventricular fibrillation, Mr. Schnerd tolerates his procedure remarkably well. He is transferred to ICU.
After the dust settles, hospital administration comes to take patient's valuables and to register Mr. Schnerd. They inquire about his insurance: he has none. Hospital clerk notes situation (annual income $17,400, 15% tax bracket (Taxes $2,193 per year) - knows patient has little means to pay his bill and gets on the horn to social work. A social worker arrives and tries to apply on his behalf for Public Aide to pay for the cost of his hospitalization. The patient is responsible for a "spend down" of approximately $500-$1000. Unfortunately, because he is male, employed part time, and has no dependents, he does not qualify for Public Aide. The hospital then submits its bill for his care to the Medicaid program. He will be enrolled in the public clinic at the hospital to receive his follow-up care after discharge.
Mr. Schnerd is started on Toprol XL 25 mg daily, lisinopril, aspirin, Plavix, and simvastatin (to limit his out-of-pocket expense) - all at the doctor's discretion. Mr. Schnerd develops congestive heart failure on day two, requires ongoing balloon pump support. Echocardiogram performed to assess LV function. Balloon pump eventually is weaned on Day #3. He leaves ICU on Day 4. Mr. Schnerd's room outside the ICU is private (due to infection control efforts, they say) and equipped with a flat screen TV from which he orders his food (it is, after all, a brand new heart hospital that has been tastefully appointed.) He spends two more days on the ward and then is discharged to follow-up in Clinic in one month.
Pt returns home and does not receive a bill for his hospital stay and and receives follow-up care via the public clinic at the hospital. He is still somewhat short of breath.
Despite his care, Mr. Schnerd continues to have ongoing angina. Because of his recurrent pain, he is admitted and another angiogram performed which was unchanged. It is decided that because of his young age and pain refractory to medical therapy, he is referred to bypass. He is seen by the surgeon the same day, and elective surgery scheduled for the next day.
His post operative stay is uncomplicated and he returns home in 4 days. Again the cost of his inpatient stay and surgery is submitted to Medicaid and his follow-up care arranged via the public clinic.
Approximately 6 weeks later, Mr. Schnerd notes palpitations and lightheadedness. He returns to ER where his is found to be in sustained monomorphic ventricular tachycardia. He is cardioverted. Another angiogram performed and his bypass vessels are patent and his native vessels unchanged. An dual-chamber ICD is scheduled for next day (he had atruial fibrillation before) of the doctor's choice*. Again, Mr. Schnerd is seen by the social worker and arrangements made for this hospitalization to be paid by Medicaid as well. If it is determined that he signficantly disabled as a result of his current illness, Mr. Schnerd could be eventially be enrolled in Medicare. The device is implanted uneventfully and he returns home.
Mr. Schnerd follows up in two weeks after his surgery with his electrophysiologist and every three months thereafter. Home monitoring of his ICD is instituted on his first follow-up visit and the device company sends the monitor to his home, free of charge.
Now, head on over to Sarah Clarke's blog from the UK and read these same patient's care as rendered by the British health care system.
Disclaimer: The dollar amounts entered here are only very gross estimates of costs incurred. Both patients and their scenarios are COMPLETELY fictitious, but rather used to illustrate important clinical care differences between the two health care systems today.
-Wes
For those who are landing on this page for the first time, be sure to read the background FIRST to these case presentations. The intent here is to compare and contrast two patients, one insured and the other uninsured, from the United States and England as care is delivered today. The US cases are described in detail in this blog and the corresponding cases, British-style, are described on Sarah Clarke, MD's blog from England.
CASE #1: The U.S. Case of Mr. Thurgood Powell
The ER radio sounds: (*bleeeeee, deeeeeeeeeppppp*) "Rampart, we have a 57 year old white male en route with a 45 minute history of substernal chest pain and diaphoresis. Initial single-lead EKG discloses ST segment elevation. One ASA given, nitro given, BP 96/47, pulse 110, respirations 22, pt diaphoretic..."
ER doctor: "Code cor activated. Cath lab ready. Proceed as soon as possible."
Pt arrives. Looks poorly. A 12-lead EKG is obtained in the ER and confirms an evolving acute anterior myocardial infarction. There is no contraindication to proceeding directly to cath lab. Given loading dose of Plavix, integrelin. Shuttled to lab. Angio performed. 95% LAD stenosis and significant 3-vessel disease is noted. Ventriculogram not performed due the patient's condition. His BP drops, intraaortic balloon pump placed. Due to his age and lack of comorbidities, it is decided to place a drug-eluting stent in LAD artery. Aside from some VT during case and one episode of ventricular fibrillation during his procedure requiring countershock, but patient tolerates remarkably well. Patient is transfered to ICU.
After the dust settles, hospital administration comes to take patient's valuables and to register Mr. Powell. They inquire about his insurance: he produces a platinum policy card from Blue Cross Blue Shield of Illinois which Mr. Powell chose amongst several insurance policies offered by his employer. He could cover his entire family for approximately $400 per month ($200 per paycheck): total annual outlay $4800. Employer also picks up a more significant portion of the cost (approximately $14,000 per year) but can deduct this amount from their profit for tax purposes. Mr. Powell cannot deduct the price of his insurance from his income amount and has a $5000 annual family deductible. Also, Mr. Thurgood's income falls into the 33% federal tax bracket ($67,643 per year). Still, all is good - he's covered.
Mr. Powell is started on Toprol XL 25 mg daily, Altace, aspirin, Plavix, and Crestor - all at the doctor's discretion (He is young, after all). Patient has development of congestive heart failure on day two, requires ongoing balloon pump support. Some atrial fibrillation occurs, requiring titration of medications to control. Echocardiogram performed to assess LV function. Balloon pump but eventually is weaned on Day #3. He leaves the ICU on Day 4. His room outside the ICU is private (due to infection control efforts, they say) and equipped with a flat screen TV from which he orders his food (it is, after all, a brand new heart hospital that has been tastefully appointed.) He spends two more days on the ward and then is discharged to follow-up in Clinic in one month.
Pt returns home and later receives a bill for his hospital stay. On his Explanation of Benefits, he notices a total bill for $180,000. Insurance has agreed to pay about $150,000 due to a pre-negotiated arrangement of the insurer with the hospital. The insurer has likewise negotiated with the employer to offer a price point with a comfortable profit "spread." Mr. Powell is not responsible for understanding the difference - he just has to pay his annual deductable of $5000.
Despite his care, Mr. Powell continues to have ongoing angina. Because of his recurrent pain, he is admitted and another angiogram performed which was unchanged. It is decided that because of his young age and pain refractory to medical therapy, he is referred to bypass. He is seen by the surgeon the same day, and elective surgery scheduled for the following day.
His post operative stay is uncomplicated and he returns home in 4 days. Cost for surgery and hospital stay: About $100,000.
Approximately 6 weeks later, Mr. Powell notes palpitations and lightheadedness. He returns to ER where his is found to be in sustained monomorphic ventricular tachycardia. Another angiogram performed. All bypass vessels are open and his native disease unchanged. A dual chamber ICD is scheduled for next day of manufacturer of the electrophysiologist's choice* (patient had atrial fibrillation in the past, after all) and implanted uneventfully. Mr. Powell later returns home.
Again a bill is sent to his home: cost of hospitalization with ICD implant $160,000. Insurance has prenegotiated a lower price with hospital - $110,000 - but has agreed to pay the full negotiated amount with the remainder "forgiven" as far as Mr. Powell is concerned. Mr. Powell is amazed by the state-of-the art technology installed in his chest.
Mr. Powell follows up in two weeks after his surgery with his electrophysiologist, two weeks after that with his cardiologist, and about a month later, his internist. He is followed for his ICD every three months thereafter. Home monitoring of his ICD is instituted on his first follow-up visit. The device company sends the monitor to his home, free of charge.
* In reality, hospital has asked doctor which company's devices he's willing to work with and hospital negotiates bare bones pricing on ICD and up charges device approximately two to three times cost to provide margin for hospital operations.
CASE #2: The U.S. Case of Mortimer T. Schnerd
The ER radio sounds: (*bleeeeee, deeeeeeeeeppppp*) "Rampart, we have a 43 year old white male en route with a 45 minute history of substernal chest pain and diaphoresis. Initial single-lead EKG discloses ST segment elevation. One ASA given, nitro given, BP 96/47, pulse 110, respirations 22, pt diaphoretic..."
ER doctor: "Code cor activated. Cath lab ready. Proceed as soon as possible."
Pt arrives. He looks poorly. A 12-lead EKG is obtained in the ER and confirms an evolving acute anterior myocardial infarction. There is no contraindication to proceeding direct to cath lab. Given loading dose of Plavix, integrelin. Shuttled to lab. Angio performed. 95% LAD stenosis and severe underlying 3-vessel disease is noted. Ventriculogram not performed. His BP drops, intraaortic balloon pump placed. Due to his age and lack of comorbidities, it is decided to place a drug-eluting stent in LAD artery. Aside from some VT during case and one episode of ventricular fibrillation, Mr. Schnerd tolerates his procedure remarkably well. He is transferred to ICU.
After the dust settles, hospital administration comes to take patient's valuables and to register Mr. Schnerd. They inquire about his insurance: he has none. Hospital clerk notes situation (annual income $17,400, 15% tax bracket (Taxes $2,193 per year) - knows patient has little means to pay his bill and gets on the horn to social work. A social worker arrives and tries to apply on his behalf for Public Aide to pay for the cost of his hospitalization. The patient is responsible for a "spend down" of approximately $500-$1000. Unfortunately, because he is male, employed part time, and has no dependents, he does not qualify for Public Aide. The hospital then submits its bill for his care to the Medicaid program. He will be enrolled in the public clinic at the hospital to receive his follow-up care after discharge.
Mr. Schnerd is started on Toprol XL 25 mg daily, lisinopril, aspirin, Plavix, and simvastatin (to limit his out-of-pocket expense) - all at the doctor's discretion. Mr. Schnerd develops congestive heart failure on day two, requires ongoing balloon pump support. Echocardiogram performed to assess LV function. Balloon pump eventually is weaned on Day #3. He leaves ICU on Day 4. Mr. Schnerd's room outside the ICU is private (due to infection control efforts, they say) and equipped with a flat screen TV from which he orders his food (it is, after all, a brand new heart hospital that has been tastefully appointed.) He spends two more days on the ward and then is discharged to follow-up in Clinic in one month.
Pt returns home and does not receive a bill for his hospital stay and and receives follow-up care via the public clinic at the hospital. He is still somewhat short of breath.
Despite his care, Mr. Schnerd continues to have ongoing angina. Because of his recurrent pain, he is admitted and another angiogram performed which was unchanged. It is decided that because of his young age and pain refractory to medical therapy, he is referred to bypass. He is seen by the surgeon the same day, and elective surgery scheduled for the next day.
His post operative stay is uncomplicated and he returns home in 4 days. Again the cost of his inpatient stay and surgery is submitted to Medicaid and his follow-up care arranged via the public clinic.
Approximately 6 weeks later, Mr. Schnerd notes palpitations and lightheadedness. He returns to ER where his is found to be in sustained monomorphic ventricular tachycardia. He is cardioverted. Another angiogram performed and his bypass vessels are patent and his native vessels unchanged. An dual-chamber ICD is scheduled for next day (he had atruial fibrillation before) of the doctor's choice*. Again, Mr. Schnerd is seen by the social worker and arrangements made for this hospitalization to be paid by Medicaid as well. If it is determined that he signficantly disabled as a result of his current illness, Mr. Schnerd could be eventially be enrolled in Medicare. The device is implanted uneventfully and he returns home.
Mr. Schnerd follows up in two weeks after his surgery with his electrophysiologist and every three months thereafter. Home monitoring of his ICD is instituted on his first follow-up visit and the device company sends the monitor to his home, free of charge.
* In reality, hospital has asked doctor which company's devices he's willing to work with and hospital negotiates bare bones pricing on ICD and up charges device approximately two to three times cost to provide margin for hospital operations.
Now, head on over to Sarah Clarke's blog from the UK and read these same patient's care as rendered by the British health care system.
Disclaimer: The dollar amounts entered here are only very gross estimates of costs incurred. Both patients and their scenarios are COMPLETELY fictitious, but rather used to illustrate important clinical care differences between the two health care systems today.
Finally, I would be remiss to not thank Dr. Clarke for her hard work in getting this done after many hours of overseas travel and a full day of megaclinic.
-Wes
Could This Be the ACC Meeting of the Future?

Click image to enlarge
I couldn't help but notice the "Heart Hub" at the American College of Cardiology Meeting this year, pictured above. There were doctors nicely nuzzled up to a bar in a relaxed atmosphere where a bartender served cranberry juice, soft drinks and perhaps a small snack, as doctors watched and interacted with any of four talks occurring simultaneously at the meeting. Some were interesting case discussions with a question and answer format where you could text message your answer to a multiple-choice question on your cell phone and, like American Idol, the results would be instantly displayed on the screen for the audience to view before the correct answer was given.
Which made one wonder, with all the concern about industry influence that was aired publicly at the meeting with gargantuan corporate displays that stretched 25-30 feet in the air for over a quarter of a mile in the display hall as a backdrop, might his be a better way to provide education for tomorrow's doctors?
But there was only one problem:
This is very expensive to produce. Who the heck would pay for it?
-Wes
Tuesday, March 16, 2010
Part I - Background: A Chance to Size Up Two Health Care Systems
Being here at the American College of Cardiology Scientific Sessions in Atlanta, Georgia, USA, I have had a unique opportunity to meet with an interventional cardiologist from "across the pond" in England: Sarah Clarke, MD. Sarah is a Consultant Interventional Cardiologist at Papworth Hospital, Cambridge UK. Her undergraduate years were spent at the University of Cambridge, UK and postgraduate training was undertaken in the region. She attained an MD from the Univeristy of Cambridge. She was awarded a Fellowship in Interventional Cardiology at the Massachusetts General Hospital in Boston, and returned to take up her Consultant post in the UK in 2002. In 2006 Dr Clarke was appointed the Clinical Director of Cardiac Services at Papworth. Papworth Hospital is a 240ish-bed hospital that performs about 2,000 interventional cardiology procedures per year.
We thought it would be interesting to compare and contrast two heart patients - one with insurance and one without insurance - from our two health care systems, to illustrate how these patients obtain health coverage, might be managed, and how things look from the patient's perspective. It should be noted that Dr. Clarke has had an experience with the American health care system first-hand when her father (from England) suffered a myocardial infarction while visiting her in Boston. Her interest in contrasting our health care system prompted her to attend the session between Chris Jennings and Congressman Paul Ryan and she gave her take earlier. I, on the other hand, have no experience with health care from the UK, other than working to occlude my left anterior descending artery while sipping tea with a few biscuits and clotted cream in Oxford. (Smashing!)
Right.
Any way, I will be performing the US perspective on this blog, and Sarah will be writing about the UK perspective on her blog. We simply cannot cover every patient scenario or income range due to length (and time) considerations. Still, these posts might serve as a background for discussion as we consider the health care reform efforts underway in the United States.
For the purposes of the exercise, we'll take two patients, Mr. Thurgood Powell, a highly successful 57 year-old businessman making $250,000 (£166,128) per year with his company PoshPosh Entertainment, and Mortimer T. Schnerd, a pleasant 43 year old man who is unemployed but working part-time in the local K-mart, earning $17,400 (£11,562) per year. Both men will experience heart attacks, both men will present to Emergency Rooms in both countries, and both men with require 4-day ICD stays and require the implantation of an automatic defibrillator and follow-up for the first year after the heart attack. Beyond that, heck, who knows. But that will at least give us a starting point to discuss the good, the bad, and the ugly of both health care systems and to compare and contrast the two systems. We will purposely refrain from political commentary in our posts (that's for you to do in the comments section!). We only ask that the commentary discussion be respectful and civil. I would be thrilled to hear what the British think of their health care system/costs/etc. over on Sarah's blog and the U.S. perspectives on this blog. (Whether this works out or not, I have no idea, but at least we're trying...)
So check back later today after we have a chance to confer a wee bit before we post our case scenarios. And by all means, have fun at today's meeting!
-Wes
We thought it would be interesting to compare and contrast two heart patients - one with insurance and one without insurance - from our two health care systems, to illustrate how these patients obtain health coverage, might be managed, and how things look from the patient's perspective. It should be noted that Dr. Clarke has had an experience with the American health care system first-hand when her father (from England) suffered a myocardial infarction while visiting her in Boston. Her interest in contrasting our health care system prompted her to attend the session between Chris Jennings and Congressman Paul Ryan and she gave her take earlier. I, on the other hand, have no experience with health care from the UK, other than working to occlude my left anterior descending artery while sipping tea with a few biscuits and clotted cream in Oxford. (Smashing!)
Right.
Any way, I will be performing the US perspective on this blog, and Sarah will be writing about the UK perspective on her blog. We simply cannot cover every patient scenario or income range due to length (and time) considerations. Still, these posts might serve as a background for discussion as we consider the health care reform efforts underway in the United States.
For the purposes of the exercise, we'll take two patients, Mr. Thurgood Powell, a highly successful 57 year-old businessman making $250,000 (£166,128) per year with his company PoshPosh Entertainment, and Mortimer T. Schnerd, a pleasant 43 year old man who is unemployed but working part-time in the local K-mart, earning $17,400 (£11,562) per year. Both men will experience heart attacks, both men will present to Emergency Rooms in both countries, and both men with require 4-day ICD stays and require the implantation of an automatic defibrillator and follow-up for the first year after the heart attack. Beyond that, heck, who knows. But that will at least give us a starting point to discuss the good, the bad, and the ugly of both health care systems and to compare and contrast the two systems. We will purposely refrain from political commentary in our posts (that's for you to do in the comments section!). We only ask that the commentary discussion be respectful and civil. I would be thrilled to hear what the British think of their health care system/costs/etc. over on Sarah's blog and the U.S. perspectives on this blog. (Whether this works out or not, I have no idea, but at least we're trying...)
So check back later today after we have a chance to confer a wee bit before we post our case scenarios. And by all means, have fun at today's meeting!
-Wes
Monday, March 15, 2010
Back By Popular Demand: Sex, the Heart, and ED
Today, I proved what I suspected: if you want readership, write or Tweet about sex and the heart.
Needless to say, in a little over 30 minutes, I garnered 30 new Twitter followers by live-tweeting what I learned in the "Sex, the Heart, and Erectile Dysfunction (ED)" session at the American College of Cardiology meeting in Atlanta. For those who might have missed it, I have organized the tweets in chronicalogical order for yourenjoyment benefit:
I must admit, that was, by far, the most fun I've ever had attending a scientific session.
-Wes
Needless to say, in a little over 30 minutes, I garnered 30 new Twitter followers by live-tweeting what I learned in the "Sex, the Heart, and Erectile Dysfunction (ED)" session at the American College of Cardiology meeting in Atlanta. For those who might have missed it, I have organized the tweets in chronicalogical order for your
Okay, at Sex/Heart session: Standing room only. Docs, pharma here. Um, will doctors attending please stand up?So there you have it.#acc10
NEWS! Most people with CAD have ED! Up next: Cardiac response to sexual activity... #acc10
10 healthy married couples studied: all kinds of positions and O2 consumption measured. #acc10 orgasm rocks the heart rate up 72%!
Guys on top: MUCH more exertion for men. Who knew? #acc10 Large variability of HR & VO2 - younger men a bit more, um, vigorous.
Man on top: 3.3 Mets, partner on top 2.5 Mets. Uh oh: Topic now not PG-13 rated... #acc10
Extramarital sex: HR 96->150; later same day w/wife: HR 62->92. REAL data. Conclsn: extramarital sex more risky #acc10< In more ways than 1
2 flights of stairs w/o stopping equals one romp in the hay in terms of workout #acc10
Oops, seems 6 Mets of exertion on treadmill tolerated means sex is safe. #acc10 Rock on, folks!
RT @gruntdoc: twitter rank skyrocketing. NEWS! Most people with CAD have ED! Up next: Cardiac response to sexual activity...< heh #acc10
OMG! Lots of therapeutic options if meds don't work: topical, intrcavernosal or intrarethral options; implants too. #acc10 Can I go now?
Remember nitrate warning...wait 48 hrs after stopping nitrate b4 using Viagra or Cialis or Levitra. #acc10 Now if u have CP, don't call me.
RELAX trial: randomized trial (evaluating use of ED drugs) looking at "stiff hearts" (diastolic dysfn) underway. #acc10 Wait, I thought stiff was good.... [kidding]
Revatio 20tid & Adcirca 20 qd used for pulmonary HTN to decrease pulmonary pressures. #acc10 Looks like juicy sex stuff has to wait.
Email inbox full after twittering sex/heart info. #acc10 (well, not quite, but 13 new followers in under 30 min) < Proof that sex sells!
Zzzz. Discussing sildanefil (Viagra) in mice. #acc10 Mice have enough sex, can we move on?
Great! A woman is about to speak! #acc10 Endocrine aspects of sex - awww, talking about male hypogonadism. Sorry ladies...
Yikes! 2000 men with low testosterone had higher mortality in Europe. #acc10 Arnold (Swartzenegger) is safe.
Peak testosterone level in men is age 28! #acc10 I'm dyin'.... [scratch that] I'm dead.
Can we use ED to prevent heart disease? #acc10 ED is assoc w/ incr CV death. ID of pts offers opportunity to steal cases from urologists!
ED is, after all, a VASCULAR disease. #acc10 I've heart of a throbbing heart but... er, never mind. (Urologists beware).
Asking about ED is as good as drawing CRP level in men! #acc10 hey, great way to save $$$$!
We were introduced to a new concept: A cardiac sexologist! #acc10 I'm in!
Q: what about women? A: Women getting Viagra. Women w/pulmonary HTN report greater sexual activity #acc10 honey, you're script's waiting 4u!
I must admit, that was, by far, the most fun I've ever had attending a scientific session.
-Wes
Boston Scientific Issues New ICD Advisory and Halts Sales of All ICDs
Despite the excitement of the American College of Cardiology meeting in Atlanta, Boston Scientific issued a self-reported advisory about all of their high-voltage defibrillators (pacers are not affected) stopping sales until "administrative issues" regarding a change in manufacturing processes and changes of their IS-4 lead connector. This advisory does NOT affect existing implanted devices, but rather halts the sales of further devices:
-Wes
The Company has determined that some manufacturing process changes were not submitted for approval to the U.S. Food and Drug Administration (FDA). At this time, the company has identified two instances of changes that, while successfully validated, were not submitted to the FDA. Boston Scientific has informed the FDA and plans to work closely with the agency to resolve this situation as soon as possible.But the interesting part of this news is who knew first. According to theheart.org:
The Company has no indication that the manufacturing process changes pose any risk to patient safety, and it is not recommending explantation of the devices.
Product families included in this advisory include: COGNIS®, CONFIENT™, LIVIAN™, PRIZM™, RENEWAL®, TELIGEN® and VITALITY™. The Company's pacemakers and other products are not affected by this advisory.
Analyst reports were among the first to trumpet the news, even before Boston Scientific issued its alert. Larry Biegelsen of Wells Fargo Securities predicted early this morning that the news will mean "reputational damage" for the company, despite the fact that the problem appears to be "administrative."And here I thought the big news of the day was going to be at the meeting.
-Wes
How to Follow the ACC Meeting in Near Real-Time

Both Sarah Clarke, MD (@doctorsarah), pictured above, and I (@doctorwes) will be trying to Twitter (is that a verb?) several of the ACC Sessions while providing running commentary on the meeting today. (Stopping to open a laptop as I run from session to session just isn't realistic, I'm finding.)
If you have no idea how to get set up on Twitter, I explain it here. Also, comments made by ourselves and others in attendance can be viewed by searching for the hashtag "#ACC10" or "#acc10".
See you there.
-Wes
Do Patient Satisfaction Surveys Guarantee Quality Medicine?
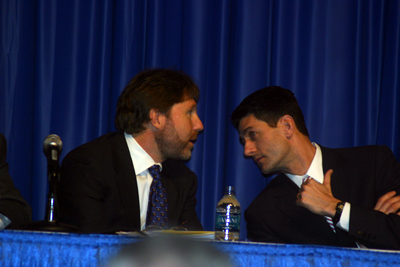
Chris Jennings and Congressman Paul Ryan confer before their 14 March 2010 session at the ACC10 meeting
This morning, Kevin Pho, MD has published on op-ed on a commonly-used tool to determine "quality medicine" from the patient's perspective: patient satisfaction surveys. Like pay-for-performance, this seems like a great idea. One might even logically conclude that doctor's pay should be tied to both pay-for performance measures and patient satisfaction.
But Kevin and Edwin Leap, MD (whose article is referenced in Kevin's piece) point out their concerns with this approach:
Quality health care sometimes means saying "no" to patients, denying them habit-forming pain medications that can feed an underlying, destructive drug addiction, or refusing to order unneeded CT scans that can facilitate harmful radiation exposure.While it's helpful to receive feedback from patients' experiences in the office to improve the quality of the patient's experience and the all-important "brand loyalty" of large health systems in an increasingly competetive health care marketplace, tying the tallied results of these surveys to physician's salaries is a flawed concept.
But Edwin Leap, a physician and columnist, notes that doctors "are constantly under the microscope to give patients what they want, since 'giving people what they want' has been tragically (and falsely) equated with good medicine."
Satisfaction scores give patients a needed voice to express their concerns, which can help medical professionals improve their patient relations. But it's a mistake to use patient satisfaction as a doctor's financial carrot.
-Wes
Sunday, March 14, 2010
ACC10 March 14, 2010: A Few Noteable Quotables
"If we're going to count radiation exposure an adverse event, perhaps we should consider sternotomy one, too."
-Ted Feldman, MD
Principle Investigator of the Everest II Trial, responding to a critique of minimally invasive mitral valve repair compared to open chest valve repair surgery.
"This is one of the most amazing things I've ever done in medicine."
Cardiologist - (Sorry, missed his name)
Maine Medical Center investgiator from the Everest II trial
"What 22 year-old wants to rack up $300,000 in debt to pursue medicine just to become a government employee?"
-U.S. Congressman Paul Ryan
"It is an outrage we keep doing this year after year, but the SGR (physcian payment formula) will NOT be fixed this year."
Chris Jennings
President, Jennings Policy Strategies, Inc.
Former Senior Health Care Adviser to the White House from 1993 to 2000.
"Legal reform is the only reform that increases patient access to health care while simultaneously reducing costs."
- Richard Anderson, MD
CEO, The Doctors Company
-Wes
Principle Investigator of the Everest II Trial, responding to a critique of minimally invasive mitral valve repair compared to open chest valve repair surgery.
"This is one of the most amazing things I've ever done in medicine."
Maine Medical Center investgiator from the Everest II trial
"What 22 year-old wants to rack up $300,000 in debt to pursue medicine just to become a government employee?"
"It is an outrage we keep doing this year after year, but the SGR (physcian payment formula) will NOT be fixed this year."
President, Jennings Policy Strategies, Inc.
Former Senior Health Care Adviser to the White House from 1993 to 2000.
"Legal reform is the only reform that increases patient access to health care while simultaneously reducing costs."
CEO, The Doctors Company
-Wes
Basics of Atrial Fibrillation Pharmachologic Management
... nicely reviewed by interventional cardiologist and a fellow physician blogger, Sarah Clarke, MD over at the BCS blog.
-Wes
-Wes
Why the ACC Meeting Is Great
When Hospitals Mandate Where Patients Are Treated
... it can lead to conspiracy and racketeering charges.
From a letter from the Chairman of the Board of Citizens Medical Center to one of the cardiologists filing suit:
Ouch.
-Wes
From a letter from the Chairman of the Board of Citizens Medical Center to one of the cardiologists filing suit:
"While it is certainly your right to exercise your medical judgement as you see fit, likewise, it is the responsibility of the Board of Directors at Citizens Medical Center to exercise their judgement as to what is in the interest of the business of Citizens Medical Center and its patients and Medical Staff. It is the Board's firm belief that it is in the best interest of Citizens Medical Center for patients who are capable of being treated at Citizens Medical Center to be treated at Citizens Medical Center and not be transferred elsewhere."Business interests before doctor-patient interests?
Ouch.
-Wes
Saturday, March 13, 2010
Tracking Medical Procedures via the iPhone
If it's free, it's for me.
Especially if it's an iPhone app to track medical procedures:
-Wes
Especially if it's an iPhone app to track medical procedures:
That’s why Dr. Shanti Bansal developed a free iPhone application — “app” in Apple-talk — that lets doctors keep a record of each case and which procedure, from a cardiac MRI to a biopsy, they perform.Here's the link to ProcedureTracker.com
“The goal is to help physicians in training be the best physicians they can,” said Bansal, who practices at Yale-New Haven Hospital. “One of the reasons I came up with this is that I’m a cardiologist and in cardiology we do a lot of procedures. I lost track of hundreds of procedures during my first and second year” of residency.
Now, in about 30 seconds, each procedure can be entered into the iPhone.
-Wes
Blogging the ACC: A Note from the Unwashed
Forgive me Lord, for I have sinned...
I was a speaker for Medtronic a while back, I'm not sure when. I was paid a fee to do this, but I can't recall exactly how much. (No doubt Senator Grassley knows by now.) I'm not even sure if my contract with Medtronic is still in effect, but I disclosed that former relationship to the American College of Cardiology before their upcoming meeting since I am blogging the conference this year.
And I was shunned.
Oh sure, they paid my registration fee - that was the original agreement (my "pay" if you will) - but because of my unwashed status as a former speaker for a company, there will be no coffee and donuts, no access to cell phone rechargers, no sit-down laptop computer space, and no early access to press releases and interviews with investigators.
*Sigh*
It seems no press pass can be issued to people with my unwashed status. Also, I cannot blog about anything having to do with Medtronic.
So there you have it. I've come clean. Full transparency. Out in the open. (FTC, you listening?)
But I'm not worried.
In a way, it's liberating to be excluded from the press room and thepre-market pre-announcement hype. Instead, I will be on the outside watching the proceedings from where I should be watching them from anyway: from the clinical doctor's perspective.
And that, as they say, will either be my downfall or my redemption.
Amen.
-Wes
I was a speaker for Medtronic a while back, I'm not sure when. I was paid a fee to do this, but I can't recall exactly how much. (No doubt Senator Grassley knows by now.) I'm not even sure if my contract with Medtronic is still in effect, but I disclosed that former relationship to the American College of Cardiology before their upcoming meeting since I am blogging the conference this year.
And I was shunned.
Oh sure, they paid my registration fee - that was the original agreement (my "pay" if you will) - but because of my unwashed status as a former speaker for a company, there will be no coffee and donuts, no access to cell phone rechargers, no sit-down laptop computer space, and no early access to press releases and interviews with investigators.
*Sigh*
It seems no press pass can be issued to people with my unwashed status. Also, I cannot blog about anything having to do with Medtronic.
So there you have it. I've come clean. Full transparency. Out in the open. (FTC, you listening?)
But I'm not worried.
In a way, it's liberating to be excluded from the press room and the
And that, as they say, will either be my downfall or my redemption.
Amen.
-Wes
Working the Backup Plan

With health care reform going as it has in the US, it might be useful to consider blending a little cardiology and country music, like cardiologist Cleve Francis, MD did:
A woman hobbles up to Francis and leans on her cane. "You were wonderful!" she says. "I had to come see you; you gave me my stress test before I had knee surgery."Heh.
Francis asks how she's getting along. "I'm still going!" she says. He smiles.
"Do you mind taking a picture with us?" says a young fan with a parent on either arm. "You saved my dad's life." Francis obliges, putting an arm around the man, who whispers something into his physician's ear before ambling into the night.
A couple asks Francis to sign a CD of his self-released live album, "Story Time," which was recorded during an earlier Birchmere concert. A man inching up the line in a walker can't believe it. "You want his autograph? I get it on a prescription every three weeks," he says.
-Wes
For Cardiologists: A Twitter Primer
With the explosion of social media, I am amazed at how many cardiologists I encounter who know little to nothing about blogs, Twitter, Facebook, Google Buzz and the like. "I'm too busy." "Who has time for that stuff?" "I wouldn't have time for anything else." "How can I possibly keep up?"
And yet today, as more and more patients reach out to the web to find medical information or, more importantly, their doctor, physician specialists of all types should probably be asking, "Can I afford to not be connected with social media in one way or another?"
Google yourself.
That's right. Type your name in Google's search box. What appears first? Your name or someone else's? Not there? How many pages down do you have to search to find something about yourself?
For me, I was surprised to find that my Facebook page and blog precedes my professional workplace's website, professional articles, and other sundry information. Hence, it's one small reason I have an online presence.
But for doctors, there are good reasons to be resistant. First, many do not want their details out there. Fair enough. Maybe you've been around enough to have enough references to do the Internet search heavy lifting. Also, there are important reasons, like patient privacy that need to be respected, and the Internet is the last place such conversations regarding patient care should occur. Realize this is not for those kinds of professional conversations. Finally, procedurally-heavy specialists have a hard time sitting behind a keyboard having near-real time conversations with comment streams on a blog. Also, while blogs create an important static chronological log of written works, they also take considerable discipline and time to get off the ground - whether one posts daily, weekly, or monthly. Simply put, if you want readership, you have to post often to your blog. Most cardiologists tell me they feel they are too busy to devote significant time to such an endeavor.
So is there something that can take less of a front-load?
Enter Twitter.
What is Twitter?
For lack of a better way to think about it, Twitter is to blogging as a person with ADHD is to an obsessive compulsive. Twitter is like a flight of ideas, streaming by very quickly, and if you miss the last few hours, you've probably missed the conversation. This is because Twitter only allows brief, 140-character text messages to be posted to the Internet as thoughts, ideas, or interesting web-based articles appear that the author wants to share with others. While it can be a powerful business or networking tool, it can also be a colossal waste of time if the content is unfocused or not used judiciously.
My Steps to Acceptance of Twitter
I was a Doubting Thomas when I first decided to register on Twitter. I was already an established physician blogger. Twitter seemed like a huge time sync. How the heck was I supposed to write a blog and send "tweets" out at the same time? Are you kidding? Seriously?
But then I realized that I can send my blog's RSS (Really Simple Syndication) feed over to Twitter using Feedburner or Twitterfeed. Instantly, another large group of people could be automatically notified that I placed a new post on my blog, expanding my blog's reach. Twitter suddenly became a huge networking amplifier above and beyond my current blog subscribers.
Alright, maybe Twitter had a purpose after all.
Later, I would attend a medical blogging conference in Las Vegas. Everyone there was on Twitter, or so it seemed. (I was the only cardiologist, at the time.) Want to send a message to the attendees? Send them a "tweet." It was instant messaging on your cell phone in near real-time. I found it useful to arrange a get-together or meet at a specific time with a specific group of individuals.
That was kind of cool.
Still later, I was watching one of the President's many talks on health care reform on TV. I decided to follow what others were saying about what the President was saying, so I searched Twitter using this thing called a "hash tag term" that always begins with a "#" character. A hash tag is nothing more than a labeled term that represents a topic for discussion. That night I searched on "#hcreform" on Twitter and could see everyone who was kind enough to place that text in their tweet about health care reform. As a result, I learned something and found some other like-minded souls who I could follow further.
Suddenly, Twitter had relevance to at least one cardiac electrophysiologist.
And so I have grown to appreciate Twitter with time. Not as a panacea to all that ailes medicine, cardiology, or my social life, but as a means to transmit information publicly VERY fast and keep up with the constant stream of ideas emanating from others with similar interests to me.
So What Do You Need to Know?
First to start, sign up on Twitter.com and use a short, descriptive name (it's easier to type) and put a good description of yourself under the "Bio" section so people will know your background and to differentiate yourself from marketing spammers (yes, they exist on Twitter, too). If you register as "drjoeblow", then your twitter name becomes @drjoeblow.
Second, you have to "follow" some people on Twitter. This is done by either typing "follow doctorwes" in the text box (without the @ sign), for instance, or clicking on some of the people's pictures of people I follow, reading about who they are, and deciding if you want to follow them too. If you want to send a public message to me, all you have to do is type "@doctorwes Here's my message." and it will come to me. If you want to privately message me (so the rest of the world can't see, I first must be following you on Twitter. Once I follow you, then you can send me a message privately using a "direct message" feature in Twitter by typing "d doctorwes This is my private message." The "d" or "D" at the beginning of the message tells Twitter to send that message to me privately. It also sends me an email telling me you've sent me a private message. (I like that.)
Third, realize people on Twitter as as diverse as there are personalities out there: some are the histrionics's "hyper-tweeting" every detail of their lives ("Heading to Starbucks") while others might be more schizoid and rarely ever tweet, but like to follow along conversations (we call them "lurkers.") Naturally, there are plenty of people in between. Read through what a few of them have "tweeted" and note how many tweets they transmit, then follow only those who appear to have relevance to you and whose frequency of tweets you can tolerate.
Fourth, when you see "RT" in the tweet, it means "re-tweet." This suggests that you like what they broadcast on twitter or wanted to restate their tweet and add come snarky commentary. Either way, the originating tweet gets mentioned so that others can follow that idea thread (or person) and also comment or follow the person.
Another common notation in a tweet you'll see on Fridays is "#FF". The Follow-Friday hash tag is a way to spread the word about your favorite people that you follow and you think might be worthwhile for others to follow. Perhaps one of the more popular #FF folks has been @ConanObrien lately.
Fifth, load a software program like Tweetdeck or HootSuite (available for free) on your computer and/or cell phone to help organize tweets. These software packages can also automatically shorten long URL's of interesting articles into smaller abbreviated URL's that are better to send along side a tweet.
Sixth, if you decide to try this, there are also things called "Lists." Lists can be either public or private. If you want to follow all the people I am that are part of my public ACC10 list, then type "follow @doctorwes/ACC10" and you'll be able to follow all the doctors, nurses and techs attending the American College of Cardiology's ACC10 conference in Atlanta this year that I am. You can also make your own very private lists for your own use.
Finally, some important suggestions:
Give it a try.
You should find Twitter can be immensely valuable tool to build a valuable professional network while simultaneously assuring an important and relevant online presence.
-Wes
And yet today, as more and more patients reach out to the web to find medical information or, more importantly, their doctor, physician specialists of all types should probably be asking, "Can I afford to not be connected with social media in one way or another?"
Google yourself.
That's right. Type your name in Google's search box. What appears first? Your name or someone else's? Not there? How many pages down do you have to search to find something about yourself?
For me, I was surprised to find that my Facebook page and blog precedes my professional workplace's website, professional articles, and other sundry information. Hence, it's one small reason I have an online presence.
But for doctors, there are good reasons to be resistant. First, many do not want their details out there. Fair enough. Maybe you've been around enough to have enough references to do the Internet search heavy lifting. Also, there are important reasons, like patient privacy that need to be respected, and the Internet is the last place such conversations regarding patient care should occur. Realize this is not for those kinds of professional conversations. Finally, procedurally-heavy specialists have a hard time sitting behind a keyboard having near-real time conversations with comment streams on a blog. Also, while blogs create an important static chronological log of written works, they also take considerable discipline and time to get off the ground - whether one posts daily, weekly, or monthly. Simply put, if you want readership, you have to post often to your blog. Most cardiologists tell me they feel they are too busy to devote significant time to such an endeavor.
So is there something that can take less of a front-load?
Enter Twitter.
What is Twitter?
For lack of a better way to think about it, Twitter is to blogging as a person with ADHD is to an obsessive compulsive. Twitter is like a flight of ideas, streaming by very quickly, and if you miss the last few hours, you've probably missed the conversation. This is because Twitter only allows brief, 140-character text messages to be posted to the Internet as thoughts, ideas, or interesting web-based articles appear that the author wants to share with others. While it can be a powerful business or networking tool, it can also be a colossal waste of time if the content is unfocused or not used judiciously.
My Steps to Acceptance of Twitter
I was a Doubting Thomas when I first decided to register on Twitter. I was already an established physician blogger. Twitter seemed like a huge time sync. How the heck was I supposed to write a blog and send "tweets" out at the same time? Are you kidding? Seriously?
But then I realized that I can send my blog's RSS (Really Simple Syndication) feed over to Twitter using Feedburner or Twitterfeed. Instantly, another large group of people could be automatically notified that I placed a new post on my blog, expanding my blog's reach. Twitter suddenly became a huge networking amplifier above and beyond my current blog subscribers.
Alright, maybe Twitter had a purpose after all.
Later, I would attend a medical blogging conference in Las Vegas. Everyone there was on Twitter, or so it seemed. (I was the only cardiologist, at the time.) Want to send a message to the attendees? Send them a "tweet." It was instant messaging on your cell phone in near real-time. I found it useful to arrange a get-together or meet at a specific time with a specific group of individuals.
That was kind of cool.
Still later, I was watching one of the President's many talks on health care reform on TV. I decided to follow what others were saying about what the President was saying, so I searched Twitter using this thing called a "hash tag term" that always begins with a "#" character. A hash tag is nothing more than a labeled term that represents a topic for discussion. That night I searched on "#hcreform" on Twitter and could see everyone who was kind enough to place that text in their tweet about health care reform. As a result, I learned something and found some other like-minded souls who I could follow further.
Suddenly, Twitter had relevance to at least one cardiac electrophysiologist.
And so I have grown to appreciate Twitter with time. Not as a panacea to all that ailes medicine, cardiology, or my social life, but as a means to transmit information publicly VERY fast and keep up with the constant stream of ideas emanating from others with similar interests to me.
So What Do You Need to Know?
First to start, sign up on Twitter.com and use a short, descriptive name (it's easier to type) and put a good description of yourself under the "Bio" section so people will know your background and to differentiate yourself from marketing spammers (yes, they exist on Twitter, too). If you register as "drjoeblow", then your twitter name becomes @drjoeblow.
Second, you have to "follow" some people on Twitter. This is done by either typing "follow doctorwes" in the text box (without the @ sign), for instance, or clicking on some of the people's pictures of people I follow, reading about who they are, and deciding if you want to follow them too. If you want to send a public message to me, all you have to do is type "@doctorwes Here's my message." and it will come to me. If you want to privately message me (so the rest of the world can't see, I first must be following you on Twitter. Once I follow you, then you can send me a message privately using a "direct message" feature in Twitter by typing "d doctorwes This is my private message." The "d" or "D" at the beginning of the message tells Twitter to send that message to me privately. It also sends me an email telling me you've sent me a private message. (I like that.)
Third, realize people on Twitter as as diverse as there are personalities out there: some are the histrionics's "hyper-tweeting" every detail of their lives ("Heading to Starbucks") while others might be more schizoid and rarely ever tweet, but like to follow along conversations (we call them "lurkers.") Naturally, there are plenty of people in between. Read through what a few of them have "tweeted" and note how many tweets they transmit, then follow only those who appear to have relevance to you and whose frequency of tweets you can tolerate.
Fourth, when you see "RT" in the tweet, it means "re-tweet." This suggests that you like what they broadcast on twitter or wanted to restate their tweet and add come snarky commentary. Either way, the originating tweet gets mentioned so that others can follow that idea thread (or person) and also comment or follow the person.
Another common notation in a tweet you'll see on Fridays is "#FF". The Follow-Friday hash tag is a way to spread the word about your favorite people that you follow and you think might be worthwhile for others to follow. Perhaps one of the more popular #FF folks has been @ConanObrien lately.
Fifth, load a software program like Tweetdeck or HootSuite (available for free) on your computer and/or cell phone to help organize tweets. These software packages can also automatically shorten long URL's of interesting articles into smaller abbreviated URL's that are better to send along side a tweet.
Sixth, if you decide to try this, there are also things called "Lists." Lists can be either public or private. If you want to follow all the people I am that are part of my public ACC10 list, then type "follow @doctorwes/ACC10" and you'll be able to follow all the doctors, nurses and techs attending the American College of Cardiology's ACC10 conference in Atlanta this year that I am. You can also make your own very private lists for your own use.
Finally, some important suggestions:
1. Follow smart people doing work that is relevant to yours. Trash most others.So there you have it. A crash course on Twitter for Dummies.
2. Post relevant, valuable content of interest to your followers.
3. Watch your time on Twitter. At most, I spend 20 minutes a day on Twitter, and I think it would take me far more time offline to gain and share the same information.
4. Do not EVER post patient information - Twitter is public and searchable on Google. 'nuf said.
Give it a try.
You should find Twitter can be immensely valuable tool to build a valuable professional network while simultaneously assuring an important and relevant online presence.
-Wes
Friday, March 12, 2010
The Waning Popularity of Scientific Sessions as Told By Google Trends
What has the been the marketing impact of the American College of Cardiology's Scientific Sessions been each year?
Just turn to Google Trends to see the answer:
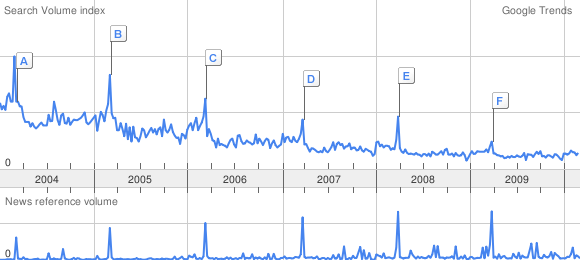
It appears the search spikes for the American College of Cardiology" each March are shrinking in amplitude significantly while the news reference volume spikes are increasing as marketers try as hard as they can to ensure doctors get their message anyway.
One wonders, given all that is transpiring in health care today, what it would take to reverse the trend?
-Wes
Just turn to Google Trends to see the answer:
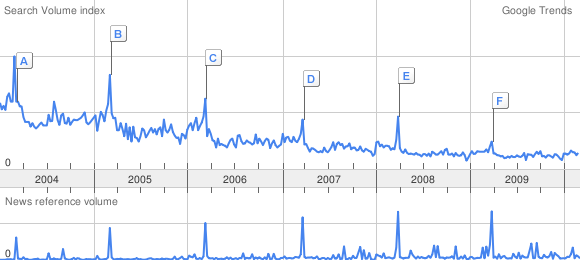
Click image to enlarge
It appears the search spikes for the American College of Cardiology" each March are shrinking in amplitude significantly while the news reference volume spikes are increasing as marketers try as hard as they can to ensure doctors get their message anyway.
One wonders, given all that is transpiring in health care today, what it would take to reverse the trend?
-Wes
Thursday, March 11, 2010
Meet My Counterpart Covering ACC.10 Across the Pond
Sarah Clarke, MD will be blogging ACC10 and i2 Summit from a uniquely British perspective over at The BCS Blog.
Geez. Competition?
Nah.
Camaraderie.
-Wes
Geez. Competition?
Nah.
Camaraderie.
-Wes
Will Physician Assistants Replace Cardiologists?
... in some remote areas, they already are:
-Wes
Officials with Saint Vincent Healthcare say current heart patients have already been notified two of the center's cardiologists will no longer be offering service come May 31st, 2010.I'm seeing excellence, aren't you?
Marketing Director for Saint V's, Margo Aldrich said Tuesday, the hospital will offer patients a chance to transition into other cardiology practices currently affiliated with Saint Vincent Healthcare. In the meantime, the Yellowstone Heart Center's two physician assistants, Heather Heggem and Tanja Wardell will continue to serve heart patients.
In a written response issued Tuesday by Aldrich, the company stated; "We will continue to grow our services, and plan to take our high-quality, award-winning cardiovascular program to the next level."
-Wes
Preview of the ACC: Percutaneous Mitral Valve Repair
"[The procedure is] very new and involves repairing my leaky valve using a clip device, without open heart surgery, so that my heart will function better"Percutaneous mitral valve repair will be the talk of the ACC Scientific Sessions for interventional cardiology this year, especially since coronary artery stent procedures are so, well, yesterday.-Elizabeth Taylor, via Twitter 6 Oct 2009
One valve repair technology popularized by Ms. Taylor's tweet that corrects a leaky mitral valve will be presented Sunday morning at the ACC meeting in Atlanta when the EVEREST II trial results are released (Larry Husten over at Cardiobrief.org has a nice outline of the late-breaking clinical trial schedule).
The EVEREST II trial is a phase 3 trial that compares the percutaneous mitral valve repair head-to-head with more conventional open mitral-valve surgery. The trial is sponsored by E-valve, Inc. (bought a year ago by Abbott). Since our center has participated in the trial (note to SEC: I have no clue about the results), it might be interesting to review the background and provide a few pictures on the technology. (By the way, this was NOT Elizabeth Taylor's procedure!)
(Important disclaimer: This device is NOT YET APPROVED for use in the US. Further, I have no financial interest in the manufacturer(s) and was not an investigator for the EVEREST I or EVEREST II trials, but I do work at one of the trial centers).
Background
In 1998, a report of correcting mitral valve insifficiency (leakage) was reported by Ottavio Alfieri and colleagues in the European Journal of Cardiovascular Surgery describing a technique to plicate (suture together) the mid-portion of the mitral valve, effectively creating a "bowtie" orifice to correct the leakage:
The experimental technique reported in this study could permit minimally invasive correction of the mitral insufficiency. These patients are often not referred for surgical repair, because they are believed “too sick” for conventional surgery. The experimental technology described in this report would avoid cardiopulmonary bypass and its consequences, and thus represents a more palatable alternative for these patients.The long-term results of this technique were favorable and lead to the development of a minimally-invasive (yet transthoracic) approach for this same repair and later, thanks to the wonders of clever engineers, a completely percutaneous approach using a clip instead of sutures.
Equipment
(Note: Thanks to Dr. Ted Feldman for use of these great pictures) and the clinical trial nurses who make this all possible.
While minimally invasive, this procedure takes a village, so to speak, to perform: the interventional cardiologists, an echocardiographer and a well-hidden anesthesiologist (can you say "Where's Waldo?") barely seen behind the plastic drapes above the patient's head (yes, the patient gets to sleep for the procedure):

The personnel and equipment required to perform percutaneous repair of the mitral valve as viewed from the patient's feet. Note the Frankenstein-like steering-and-release contraption with all the IV tubing coming from it in front of the doctors used to place the mitral clip.
(Click image to enlarge)

A view from behind the implanting physicians. Note that all eyes are on the echocardiographic images to the right as the clip is positioned, rather than the fluroscopic images immedicately in front of the operators.
(Click image to enlarge)
The back end of the catheter delivery system looks just a bit complicated, since it steers the clip, grasps each leaflet of the mitral valve, and releases the clip when seated properly:

Click image to enlarge
The business end of the device is a small mechanical clip that grasps the center of the posterior and anterior leaflets of the mitral valve in an attempt to replicate the "bowtie" surgical repair originally described:
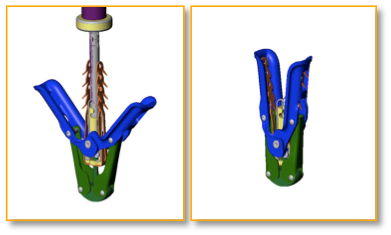

A cartoon rendition (top) and a photo of the clip (bottom) used to clip together the leaflets of the mitral valve
While the fluoro images of the procedure are interesting to view as the device is deployed:

An RAO fluoroscopic view of the mitral valve clip passed to the left atrium above the mitral valve.
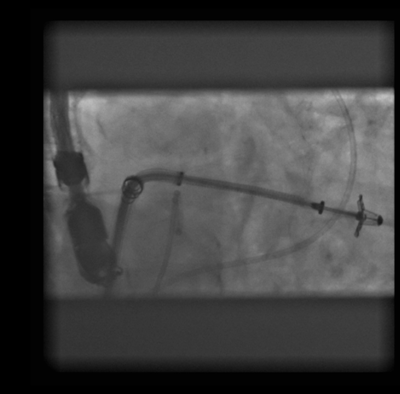
The mitral valve clip is advanced below the mitral valve into the left ventricle in preparation of grasping the mitral valve.
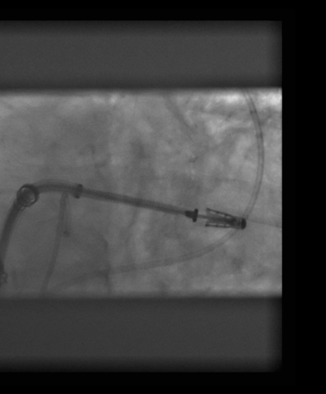
The valve leaflets are grasped and the side "wings" of the clip closed.
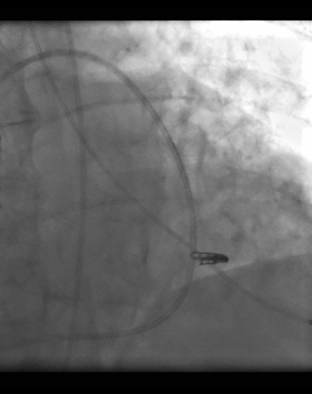
The clip is deployed and fixes permanently to the mitral valve leaflets.
Although these fluoroscopic images are amazing, this procedure would not be possible without the ability to see the valve leaflets in realtime using transesophageal echocardiography:
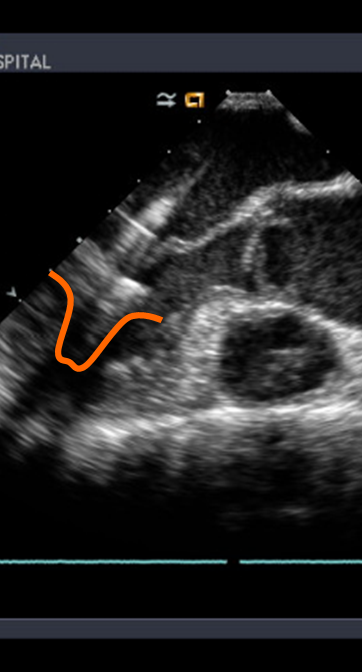
Transesophageal echocardiographic images of the clip (outlined in orange) being placed below the mitral valve leaflets.
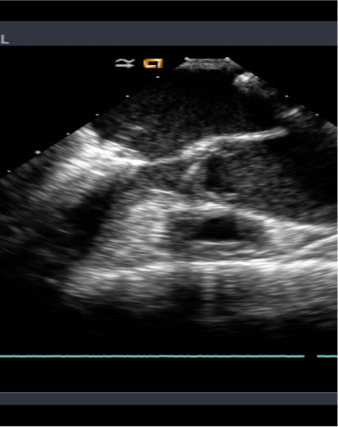
The clip is withdrawn until the leaflets of the mitral valve are engaged in the clip. (Note the "wings" of the clip are still open)
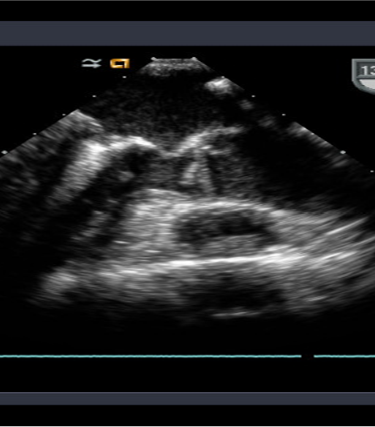
The wings of the clip are closed tightly to grasp the valve leaflets.
Will the Device Work?
Although preliminary results of the EVEREST I trial were promising, the EVEREST II trial will be the pivotal comparative effectiveness study comparing this approach to open mitral valve repair.
One thing's for sure after seeing all this: innovation in cardiology is alive and well!
See you Sunday!
-Wes
Turning Off Implanted Defibrillators
End-of-life issues with implantable cardiac defibrillators (ICDs) and the need (or not) for deactivation policies is being discussed at the palliative medicine blog, Pallimed.
Shoot on over and lend your $0.02 to the discussion.
-Wes
Shoot on over and lend your $0.02 to the discussion.
-Wes
On the Surgical Ablation of Atrial Fibrillation
It seems okay that if a surgeon wants to cut apart the atrium and sew it back together to fix atrial fibrillation (called the surgical MAZE procedure) during open heart surgery, that's okay.
But if the surgeon wants to use a device that heats the tissue non-invasively to create non-conducting lines in the atrium, that's not okay in the eyes of the law because it isn't labeled for that use specifically for use in the left atrium by the FDA, even though the FDA approved (one example) the device for medical use.
Using the current analogy, most of the catheters we've been using for years to ablate left-sided arrhythmias percutaneously aren't approved specifically for that use either, but rather right atrial type I flutter (See here or here, for example).
Uh, oh, sorry... (just trying to make a few hundred thousand dollars as a whistleblower....)
-Wes
But if the surgeon wants to use a device that heats the tissue non-invasively to create non-conducting lines in the atrium, that's not okay in the eyes of the law because it isn't labeled for that use specifically for use in the left atrium by the FDA, even though the FDA approved (one example) the device for medical use.
You may, therefore, market the device, subject to the general controls provisions of the Act. The general controls provisions of the Act include requirements for annual registration, listing of devices, good manufacturing practice, labeling, and prohibitions against misbranding and adulteration.Does anyone else find that strange?
Using the current analogy, most of the catheters we've been using for years to ablate left-sided arrhythmias percutaneously aren't approved specifically for that use either, but rather right atrial type I flutter (See here or here, for example).
Uh, oh, sorry... (just trying to make a few hundred thousand dollars as a whistleblower....)
-Wes
Tuesday, March 09, 2010
You Know It's Going to Be a Good Day in the EP Lab When
... you can find a contribution to SpontaneousSmiley.com on your blood pressure cuff just before it was placed on our first patient of the day:
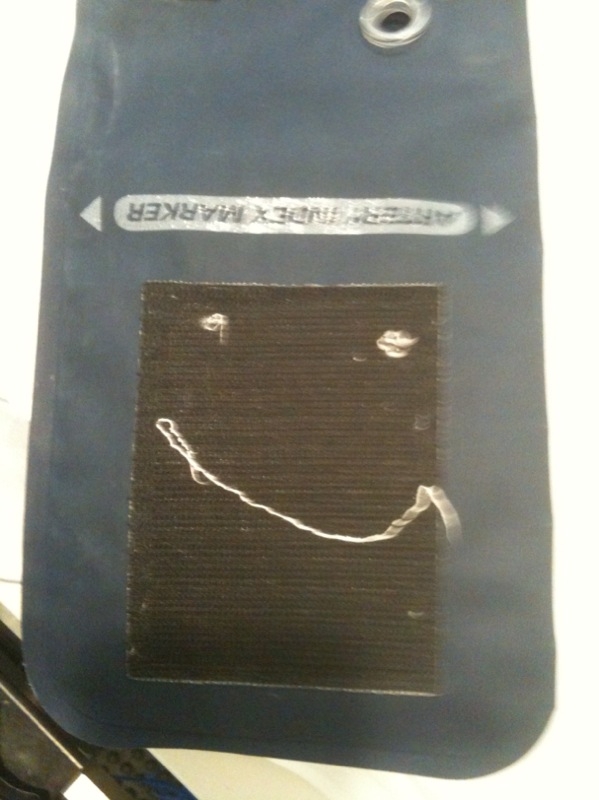
Yep. Good day all around.
-Wes
Yep. Good day all around.
-Wes
Monday, March 08, 2010
The History of Defibrillation
.. told in the New York Times:
Imagine if that happened today.
Boy, we've come a long way, haven't we?
-Wes
Reference: Barnett A. Greene, M.D. "Ventricular Fibrillation Abolished by Electric Shock" J Am Med Assoc. 1948;136(4):279.
While the surgeon massaged the man’s heart manually, the article said, “a makeshift ‘defibrillator’ was rigged to administer instantaneous electric shock treatment.”... just as the current article failed to mention that the first young man actually fibrillated from digitalis toxicity as tachycardia was being treated under anesthesia.
The article described a process that was shocking in more ways than one. When the man’s heart went into ventricular fibrillation — an event that means death in less than five minutes — operating room workers hooked two copper electrodes to an examining lamp that happened to be in the room, touched the other ends to the man’s heart, and shocked it into normal rhythm.
The “Philadelphia specialist” who dared to attach the wires “requested that his name be withheld from publication,” no doubt with good reason. But whoever he was, he was probably up to date on the latest in defibrillation. He may have known of a report, published in The Journal of the American Medical Association seven months earlier, of the first case of ventricular fibrillation in a human successfully treated with electric shock — an apparently dead 14-year-old boy brought back to life. He did not read of it in The Times, which took no note of it.
Imagine if that happened today.
Boy, we've come a long way, haven't we?
-Wes
Reference: Barnett A. Greene, M.D. "Ventricular Fibrillation Abolished by Electric Shock" J Am Med Assoc. 1948;136(4):279.
Innovation in Batteries - Coming to Pacemakers?
Solid state technology, could it be reliable enough to power a pacemaker? Perhaps, provided the patient keeps moving or is moved:
Imagine a pacemaker battery change every twenty years...
Pretty cool.
Then again, given the business model involved...
... maybe not.
-Wes
Imagine a pacemaker battery change every twenty years...
Pretty cool.
Then again, given the business model involved...
... maybe not.
-Wes
Wagging the Dog
"There's a crisis in the Whitehouse..." begins the trailer from the 1997 movie, Wag the Dog, "...and to save the election... you just gotta distract 'em..."
It seems people might be on to this tactic in Washington. From Peggy Noonan:
But then again, when it comes to the insurers, Dr. Rich nailed the Wag-the-Dog tactic earlier, didn't he?
-Wes
Durbin, D-Ill., said health insurance premiums could increase up to 60 percent in Illinois this year. Meanwhile, he said, insurance companies are experiencing some of their highest profits in history.Sixty percent rise in insurance premiums that could happen? That would be a crisis, indeed! Never mind that people would drop that insurance carrier faster than a speeding bullet.
"The outrageous premium prices which they have been pushing on the American people in order to drive up their profited are unacceptable and unfair." Durbin said. "We're going to start watching them more closely ... The party's over."-"Durbin blasts health insurance premiums," Chicago Tribune 8 Mar 2010
It seems people might be on to this tactic in Washington. From Peggy Noonan:
The president can't be a hope purveyor while he's a doom merchant, and he appears to believe he has to be a doom merchant to justify ramming through his legislation. This particular legislation is not worth that particular price.The facts on the cost of the current bill before Congress were nicely outlined by Congressman Paul Ryan in March's Wall Street Journal. What the White House administration is learning is that, like it or not, American's are sick of the scare tactics and are looking for real answers.
All this contributes to a second problem, which is a growing credibility gap. In his speech Wednesday, demanding an "up or down" vote, the president seemed convinced and committed—but nothing he said sounded true. His bill will "bring down the cost of health care for millions," it is "fully paid for," it will lower the long term deficit by a trillion dollars.
Does anyone believe this? Does anyone who knows the ways of government, the compulsions of Congress, and how history has played out in the past, believe this? Even a little?
But then again, when it comes to the insurers, Dr. Rich nailed the Wag-the-Dog tactic earlier, didn't he?
-Wes
Sunday, March 07, 2010
A Cardiology Website to Bookmark
Whether you're a medical student, resident, fellow, or staff cardiologist, once in a while you need a simple, succinct reference for a talk on the basics of cardiovascular disease. Who knew it would come from a radiologist:
-Wes
h/t: Dr. S. Venkatesan, MD.
LearningRadiology.com was conceived, designed, developed, is published, managed and maintained and its content is produced in its entirety by William Herring, MD, FACR. Dr. Herring is the Vice-Chairman and Radiology Residency Program Director at Albert Einstein Medical Center in Philadelphia, Pennsylvania, where he has been the Radiology Residency Program Director for over 25 years.Kudos to Dr. Herring.
All material on the site, except for the Faculty lectures by other members of the staff at Einstein, was produced by Dr. Herring. Started in June of 2002, the site was originally intended to replace the handout notes that accompanied lectures for the residents and medical students at Albert Einstein Medical Center. It now contains over 20,000 pages of content, and has grown in popularity so that currently over 9 thousand unique visitors access the site every day. Visitors access over 20 million pages of content every year.
The site has been, and continues to be, free to use. It requires no registration, no sign-in, no fee and is commercial-free.
-Wes
h/t: Dr. S. Venkatesan, MD.
Thursday, March 04, 2010
Why Nurse Supervisors Should Be Marines
... because you never know when their skills will come in handy:
The Few. The Proud. The Nurses!
-Wes
Witnesses told police that nurse (supervisor) Andy Hull, a 35-year-old former Marine, jumped in to disarm Lupienski when he pulled the gun out from under his gown and pointed it at another staff member. Hull was shot three times. He was being treated Wednesday in the hospital's intensive care unit for injuries that were described as serious but not life-threatening.I can hear it now....
The Few. The Proud. The Nurses!
-Wes
Wednesday, March 03, 2010
Coffee and the Heart - Good or Bad?
This week, it seems to be good:
But a quick Google search on Dr. Klatsky's earlier studies using the same questionaire database shows the problems with using questionaire data to make such sweeping conclusions. Take, for instance, these findings from 1973:
What they say is:
-Wes
h/t: The Happy Hospitalist for the story idea.
“People who are moderate coffee drinkers can be reassured that they are not doing harm because of their coffee drinking,” said Arthur Klatsky, the study’s lead investigator and a cardiologist at Kaiser’s Division of Research.These "surprising" data are to be presented at the AHA meeting March 5th. (You'll have to wait until then to get the REAL scoop, it seems.)
But a quick Google search on Dr. Klatsky's earlier studies using the same questionaire database shows the problems with using questionaire data to make such sweeping conclusions. Take, for instance, these findings from 1973:
"Coffee drinking is not an established risk factor for myocardial infarction."And yet a bit later, in 1990, there's a flip flop:
Because of conflicting evidence about the relation of coffee use to coronary artery disease, the authors conducted a new cohort study of hospitalizations among 101,774 white persons and black persons admitted to Kaiser Permanente hospitals in northern California in 1978–1986. In analyses controlled for eight covariates, use of coffee was associated with higher risk of myocardial infarction (p=0.0002). (By the way, British researchers failed to find a similar correlation in instant coffee drinkers)So what, really, do these data from the Kaiser questionaire data regarding heavy coffee consumption and the heart say?
What they say is:
- Questionaire data crunched to suggest correlations are insufficient to mean causation, irrespective of how the media parses it.
- Questionaire data are subject to significant sampling and reporting biases.
- Rehashing the same old questionaires using the same samples with newer data can dramatically alter prior findings.
- Researchers are getting paid way too much to keep rehashing the same data for large health systems.
- On the lighter side, college undergrads and medical students should note that they could use these types of questionaire data to justify significant caffeine consumption along with alcohol to protect themselves from developing cirrhosis.
-Wes
h/t: The Happy Hospitalist for the story idea.
Tuesday, March 02, 2010
Heart Rhythm Society's New Blog
The Heart Rhythm Society has launched a new blog called epinsights.org, co-authored by two members of the Heart Rhythm Society: John Day, MD and allied professional David Wiggins, RN, BS BME. They'll be writing on topics such as clinical guidelines, health policy and advocacy, professional education, practice information, quality improvement, research and Scientific Sessions.
Welcome to the fray, gents!
-Wes
Welcome to the fray, gents!
-Wes
Monday, March 01, 2010
The Implications of Our (Temporary) 21% Medicare Pay Cut
What we're learning from the 21% Medicare pay cut to physicians that occurred today:
As crazy as that might sound, I bet it would ultimately give us some real change we could believe in.
-Wes
- There really must be a cost-control crisis with Medicare and the only politically-acceptable way to implement those cost controls are by cutting working physicians' payments.
- There’s was widespread political support for blocking the scheduled pay cuts to doctors, but central government control moves very slowly. That's because doing so is expensive. For now, doctors have been asked to hold on to our billings for about 10 days so they can put through another temporary patch that will further delay the cuts until October 1 (pg 107) as part of a jobs bill, paid for by stimulus funds.
- If they are serious about not cutting physicians' payments, Congress must get rid of the sustainable growth rate formula that keeps calling for the cuts and acknowledge that the country is going to be on the hook for billions of dollars in additional Medicare costs. Right now, that's not sounding too popular. Better to stand by your plan and not mention these additional costs to the nation.
- We also see that Congress will not commit to fiscal conservancy when it is politically ill-advised to do so. Recall that the Sustainable Growth Rate (SGR) formula, part of the Balanced Budget Act of 1997 was enacted on August 5, 1997 to replace the Medicare Volume Performance Standard (MVPS). Section 1848(f)(2) of the Act specified the formula for establishing yearly SGR targets for physicians' services under Medicare and was intended to control the growth in aggregate Medicare expenditures for physicians' services. Since this formula to control Medicare costs is very likely to now be overturned, what does this say about other well-intentioned but politically unpopular policy initiatives planned to save costs in years ahead?
- Policy decisions run by a single central body affect the entire United States and not just a portion of it. Sweeping legislation that affects the entire United States carries high risks to the nation as a whole if initial planning assumptions are incorrect.
- As mentioned by others today, new primary care doctors are avoiding government healthcare because it cannot cover their costs. Even large institutions like Mayo clinic have done the math and aren't taking Medicare patients at some of their primary care sites. As others follow suit, this will put further strain on primary care physician availability.
As crazy as that might sound, I bet it would ultimately give us some real change we could believe in.
-Wes
Subscribe to:
Comments (Atom)