 Sometimes, even our best efforts to save lives fails us.
Sometimes, even our best efforts to save lives fails us.In an effort to minimize the time to deliver shocks in patients in cardiac arrest, hospitals across the country have turned to automatic external defibrillators to reduce the time to first shock, thereby improving cardiac arrest outcomes. More often than not, this policy has been effective at assuring that nursing staff and even locally-available non-medical personnel can at least treat a patient as soon as possible after a cardiac arrest.
But might there be an instance where the AED gets it wrong?
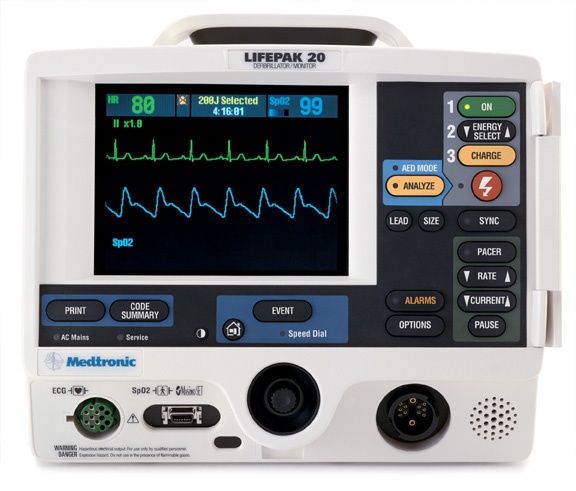
Well, of course. No shock algorithm is perfect. Take a look at this strip obtained from a Medtronic's Life Pak 20 defibrillator set to default to AED mode after a telemetry alarm prompted nursing personnel to rush to be patient's room, only to see the patient lose consciousness:
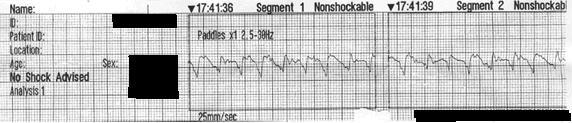
Click image to enlarge
CPR is started, but no shock was delivered. Why? Because the AED considered the rhythm "NONSHOCKABLE."
A quick call to the company suggests the algorithm (which is not published anywhere to my knowledge) involves five factors to attempt to be highly sensitive and fairly specific for ventricular arrhythmias: heart rate over 120, amplitude of the signal, slope of the received EKG morphology, QRS width, and something called "flat line content." Careful review of this rhythm demonstrates that it represents a heart rate over 120, is irregular, has varying QRS widths, and probably has different "slopes" and has an unknown "flat line content," whatever that represents.
While these findings are interesting for engineers, man (and women) must be allowed to intervene when it is perceived a machine is in error and anyone in a new, wide complex rhythm that causes a team of people to initiate CPR should consider the obvious:
Shock 'em anyway (synchronized to the QRS, of course).
Oh, and how do you deactivate the automatic nature of the AED on a Lifepak 20? Push any button besides the "Shock" button on the device and you'll be placed in manual mode.
-Wes
2 comments:
With a pulseless patient the AHA no longer recommends synchronized cardioversion. I think that they have had so many cases of operator error with the synchronization function, that they figure any shock is better than no shock.
If the machine will not shock a shockable rhythm, but it is clearly a shockable rhythm, the precordial thump is another option. I found it to be very effective long ago with a LifePak 5, when I ran out of batteries on a patient with recurrent VT.
Pulseless.
Wide complex.
Rate well over 150 by ECG, but some of the QRSs are low amplitude and probably not counted by the software.
Slopes - are they preventing the machine from acting?
Flat line content - so it does not mistakenly shock a pulseless AFib or sinus tachycardia with aberration? This has too much of a secret recipe feel to it.
Maybe they will use this example to refine their algorithm.
Telemetry and ICU nurses seem to be the ones who use precordial thump most often. They have a monitored patient, who suddenly deteriorates and the rhythm is available, but the crash cart may be several minutes from being able to deliver a shock. In this case a lifetime away from delivering a shock.
We had an event in our institution with the LifePak 20 being used inappropriately in AED mode - the staff did not know how to over ride the AED and convert to manual mode. An RCA led to the AEDs in the ICU, RR, PACU, cardiology being programmed so that they do not default to AED and the doors were removed.
Thanks for that clarification re: sync vs non sync Rogue Medic - just took ACLS and as a former EP lab RN am "programmed" to sync when there is VT. Suspect that it is lack of familiarity with holding down the shock button in the sync mode probably leads to delay in defib, thus the change in the protocol. Those who do it routinely know what to do.
CardioNP
Post a Comment