If there was one place research should be easy to perform, it’s on a disease that’s incredibly common.
Further, if there are two generally-accepted strategies to treating symptomatic patients with that ailment – one invasive and the other not – it should be pretty easy to compare which is best, right?
Maybe. Maybe not.
Welcome to the real life world of comparative effectiveness research, that politically and pundit-popular means to decide which treatment approach doctors should utilize and which, based on the results of these studies, our government will decide which approach they will fund.
But first, before starting the study, decide which way you’re leaning. Call that your “hypothesis”. Make sure your desired approach is the invasive one (this is very important) - that way, patients feel that at least you are trying to do something.
Good.
Now, be sure there are plenty of articles in the literature supporting your approach, but also discussing the substantial risks that might occur if that option is used and an accident happens.
Then have plenty of articles in the literature that talks about the other non-invasive but potentially dangerous treatment option.
Then go before your Investigational Research Board (IRB). Show them how cool it is and convince them this is the first prospective randomized trial comparing the two forms of treatment for this incredibly common disorder. Have a 15-page all-inclusive consent for the patient describing the good, the bad, and the potentially ugly. No, make it 17 pages just to be sure. (They’ll like that). Get the IRB’s blessing.
Then announce the trial to your colleagues and patients.
Then wait for the patient referrals from your colleagues who do not have the same vested interest in the trial as you, or wait for the Perfect Patient to enter your exam room.
Spend an hour with them telling them about the trial.
Then tell them that you really don’t know which option for therapy is best (and that's why you're doing the study), even though they have come to you in hopes you’ll explain to them which treatment option is best.
Look at their confused faces.
Offer plenty of time for them to decide if they want to be in the trial or not.
When they don’t call back, call them again to remind them about the importance of the trial. Talk to them for two more hours to answer their questions. Try to stay neutral to let them decide.. Hear them looking up things on the internet. Clarify the purpose of the trial to them. Sense their pressure.
Then watch them decline simply because they can’t decide whether to be in the trial or not.
Lather. Rinse. Repeat.
* * *
Sound familiar to others trying to do this work?
Now look at which topic was #1 of the Institute of Medicine’s Top 100 stand-alone topics for the First Quartile in which to perform Comparative Effectiveness Research.
Yep, atrial fibrillation.
Here’s the sad reality: the first comprehensive NIH and industry-sponsored comparative effectiveness trial studying the best approach to treat atrial fibrillation, the CABANA Trial, is having one hell-of-a-time enrolling subjects.
No one knows why.
But I suspect there are several reasons:
1) CER is complicated. Perhaps too much is being asked of these trials and their investigating centers since not only are clinical endpoints being studied, but costs as well.
2) These trials cost more to perform than they are funded. People can only work so long out of the goodness of their hearts until they must turn to some income-producing endeavor to justify their existence. In our current cost-conscious era, resources are limited for any complex, underfunded study.
3) Patients are better informed about their treatment options than ever before. This affects recruitment of subjects in several ways: (a) because of pre-conceived biases favoring one therapy over the other before a patient is even invited in to a trial, (b) a more educated subject population regarding the risks of any proposed therapy.
The real question becomes, can we really expect to put all our health care reform financial eggs in the unrealized promise of comparative effectiveness research trials when it’s so damn hard to enroll patients in these trials?
-Wes
Tuesday, August 31, 2010
EKG Du Jour #20 - The Wide and Fast Temptation
And now, another in the "EKG Du Jour" educational series:
-Wes
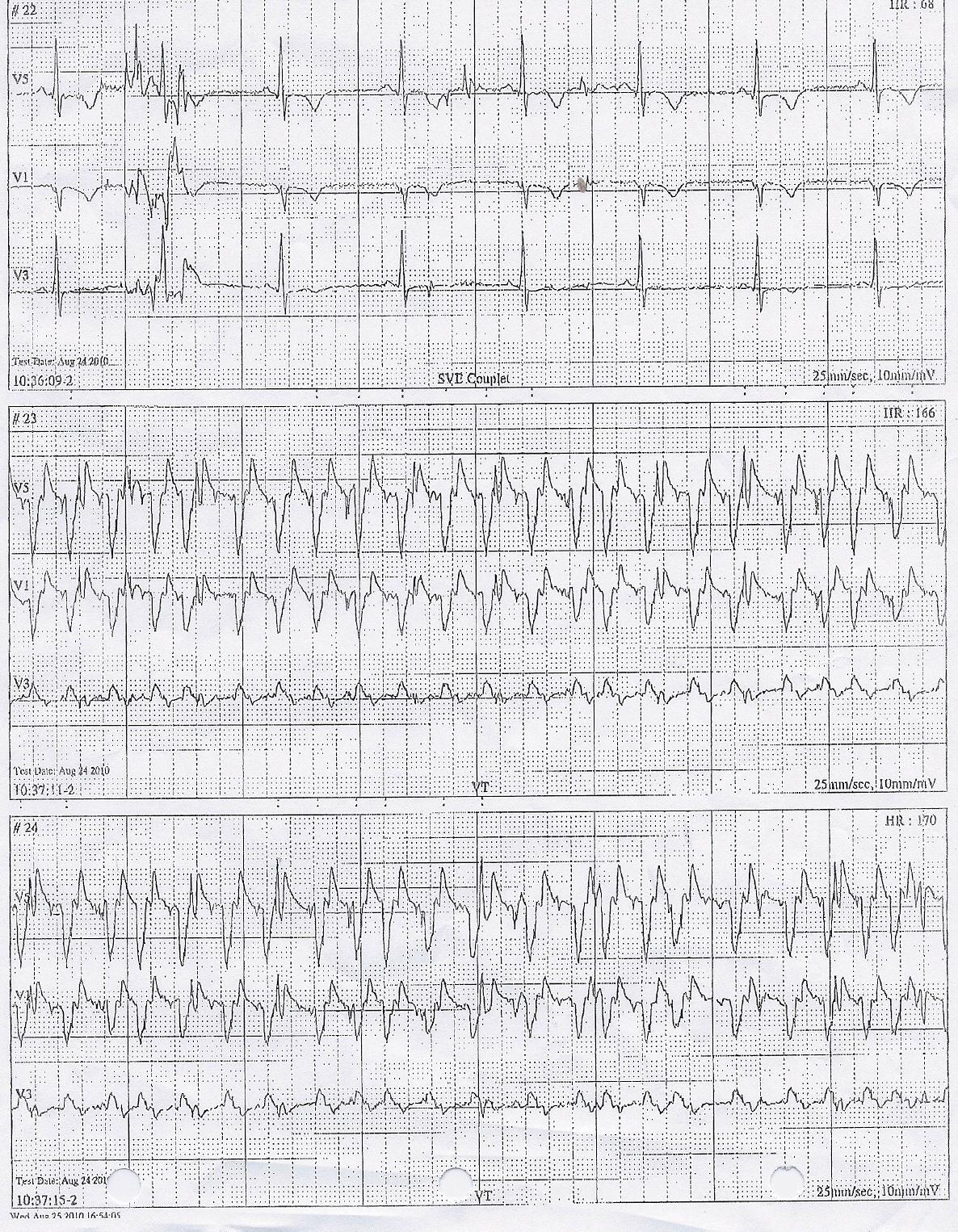
He was just under 30 years of age and had the unfortunate circumstance of having a posterior myocardial infarction two weeks ago while on vacation out of state. Fortunately, it was properly diagnosed at the local hospital and he was rushed to the cath lab for stenting with relief of his symptoms.What's the rhythm?
All went well and he was discharged shortly thereafter.
A few days later he noted new palpitations, brief at first, then more frequent. He sought evaluation with the same local cardiologist that performed the stent procedure and a Holter monitor was obtained just before he returned home.
Just after he arrived home, the patient received a call from his cardiologist explaining that his Holter results were very concerning and recommending that he report to the closest Emergency Room for evaluation.
The cardiologist faxed the following tracings to the Emergency Department. You are called to see the patient and review the Holter tracings below:Click image to enlarge
Click image to enlarge
-Wes
Medical Device Bracelets with Pacers and Defibrillators
There was some interesting Wall Street Journal's coverage on medical bracelets this morning, but pacemaker and defibrillator patients should note the following:
From the article's graphic that states:
Secondly, if you have a medical alert bracelet that notes that you have a pacemaker or defibrillator, consider adding the name of the manufacturer to the bracelet, since the machinery to program the device is specific to each manufacturer's device and this information can speed your treatment should the device need to be interrogated or adjusted.
-Wes
From the article's graphic that states:
Jewelry With a PurposeFirst, if the patient needs a shock to correct a heart rhythm disturnance, pacemakers and defibrillators are engineered so this will not hurt the circuitry of the devices. Treatment with medications or shock therapy should not be delayed, if indicated, in people with these devices should it be necessary.
Medical alert bracelets and other identification systems are important for notifying emergency responders about medical conditions. Here's what could go wrong in some situations if a patient isn't wearing one:
If a patient has...
Pacemaker or implanted defibrillator
Medics may mistakenly treat with drugs for heart arrhythmia or try to shock the patient.
...
Secondly, if you have a medical alert bracelet that notes that you have a pacemaker or defibrillator, consider adding the name of the manufacturer to the bracelet, since the machinery to program the device is specific to each manufacturer's device and this information can speed your treatment should the device need to be interrogated or adjusted.
-Wes
Monday, August 30, 2010
Our Not-So-Cheap Generic Drugs
I received the following e-mail from a patient (paraphrased):
Since the companies that make generics did not have to absorb research and development costs, how do they justify the exorbitant prices?
Simple: the middle men still have to get theirs.
-Wes
"Dear Dr. Fisher,Interesting how the generic drug market for some drugs only marginally discounts prices.
Thank you for trying to switch me from lisinopril to generic losartan (Cozaar) to help me with the irritating cough that has been nagging me since I was placed on lisinopril. I did not pick up my prescription, though. At nearly $200 for a three-month supply, I've decided to live with the cough, since the same amount of lisinopril costs me about $12.
-Ms. Patient
Since the companies that make generics did not have to absorb research and development costs, how do they justify the exorbitant prices?
Simple: the middle men still have to get theirs.
-Wes
Sometimes, You Have To Be a Doctor
... so the blog suffers.
Sorry about my recent absence, but priorities exist and this blog comes third behind family and work.
(Don't even ask about where sex fits in.)
-Wes
Sorry about my recent absence, but priorities exist and this blog comes third behind family and work.
(Don't even ask about where sex fits in.)
-Wes
Friday, August 27, 2010
Good Thing or Bad?
From an innovation standpoint, there's no question that this is a good thing.
But a percutaneous aortic valve at 101?
Guess it depends on how old you are when you look at this.
Given the cost of this procedure and the projections for when Medicare will go bust, young folks might have a legitimate concern that the funds for health care might not be available for such a procedure by the time they're eligible.
-Wes
But a percutaneous aortic valve at 101?
Guess it depends on how old you are when you look at this.
Given the cost of this procedure and the projections for when Medicare will go bust, young folks might have a legitimate concern that the funds for health care might not be available for such a procedure by the time they're eligible.
-Wes
The Terror of It All
For fathers and daughters at a certain point of life, it becomes a late night, almost weekly, ritual and bonding moment - the late might Walgreen's hit. Last night was no exception.
My daughter, realizing she needed a few last-minute school supplies and a few other cosmetic/facial/hair/nail/chewing gum necessities, asked me to take her to Walgreen's. It was a beautiful night - perfect temperature, low humidity, full moon. It was clear she was excited for the new school year ahead.
But as she got out of the car, she turned and delivered a blow:
-Wes
My daughter, realizing she needed a few last-minute school supplies and a few other cosmetic/facial/hair/nail/chewing gum necessities, asked me to take her to Walgreen's. It was a beautiful night - perfect temperature, low humidity, full moon. It was clear she was excited for the new school year ahead.
But as she got out of the car, she turned and delivered a blow:
"Dad, do you realize that next week I get my learner's permit?"I'm not sure which was scarier: the fact that this was my third and final trip around this block with a child, or the fact that soon the next time we'll be driving together to Walgreen's, it'll be for my Depends undergarments.
-Wes
Wednesday, August 25, 2010
Some Blogging Insights for Doctors
Nearly five years ago, I started this blog. As you can tell, I gave it a bit of a facelift yesterday. Over the years I have struggled with the question: should I have ads? Will they make my blog look cheezy? Am I less of a purist if I have ads?
So I started slow and tried to keep the blog as unencumbered by ads as possible, placing Google Adsense ads in the footer area of this blog. I made about $1-3 dollars per month with that approach. In essence - pretty worthless.
But recently I embarked on an Google Adsense experiment. I added one Google Adsense ad below my post of the day and to my RSS feed. That one move increased my ad revenue about 10-fold - not much, but a significant jump up. With my readership, that amount should just about over the cost of renting server space so my co-workers can see the images on my blog at work. (I appreciate my "Deep Throat" contributors at work who contribute ideas for new content here...)
Many wonder, why not just use Google's servers for your images?
Well, there's several reasons. The main reason is our workplace firewall. You see Google uses multiple servers on which it holds its images. While images might be easily retrieved using their picture manager software, Picasa, the server on which those images might be held might be held at very different internet addresses. This wreaks havoc on workplace firewalls - until I started using my own server (which my employer has approved), many of my images could not be seen by my co-workers.
The second reason is simply one of organization - I know where my images are and how they're organized. I can resize them or edit them as I need and place them on my own server for later use and recall. Just my preference.
But renting your own server space costs about $150 (or so) per year. (In contrast, Google offers about 5 Megabytes of server space for free - plenty for most - then charges a bit for more) So, to offset this server expense, I have placed some ads on this blog. No I can't quit my day job, but it appears these ads will help at least defray my server expenses.
Not to say that I don't market my ads in the sidebar for considerably more. The relative paucity of cardiology blogs out there makes that space valuable for some. But even when I place an ad there for a month or more, I find that the revenue generated will never serve as my day job. (Moral of the story: be nice to your employer - you need 'em). But more importantly, I have found that this blog has opened many entrepreneurial ventures that are much better drivers for revenue than advertising revenue. I'm betting most serious bloggers find this. (Quick definition: a "serious blogger" is anyone who is crazy enough to do this for over three years) Bottom line: Blogs, in and of themselves, are very poor ways to try to make a living, but can open doors.
I also have invested in liability insurance for this blog. It costs about $100-$300 per year, depending on the type of blog you have, but my one experience with defending a frivolous "cease and desist" letter that set me back about $14K in legal expenses makes this expense worth it to me. Learning point #2: Be careful, blogs can be risky.
There are tons of resources out there to help anyone who wants to start a blog and try to keep with it. Consider reading just about everything at Problogger.net, for instance. I completely understand the challenges for doctors maintaining a blog - it's damn hard work. But it also serves as a useful avenue for teaching, advocating, venting (when done professionally and with an appropriate amount of restraint) and fills a little creative void that I still enjoy.
-Wes
Inherited Arrhythmogenic Disorders - A Review
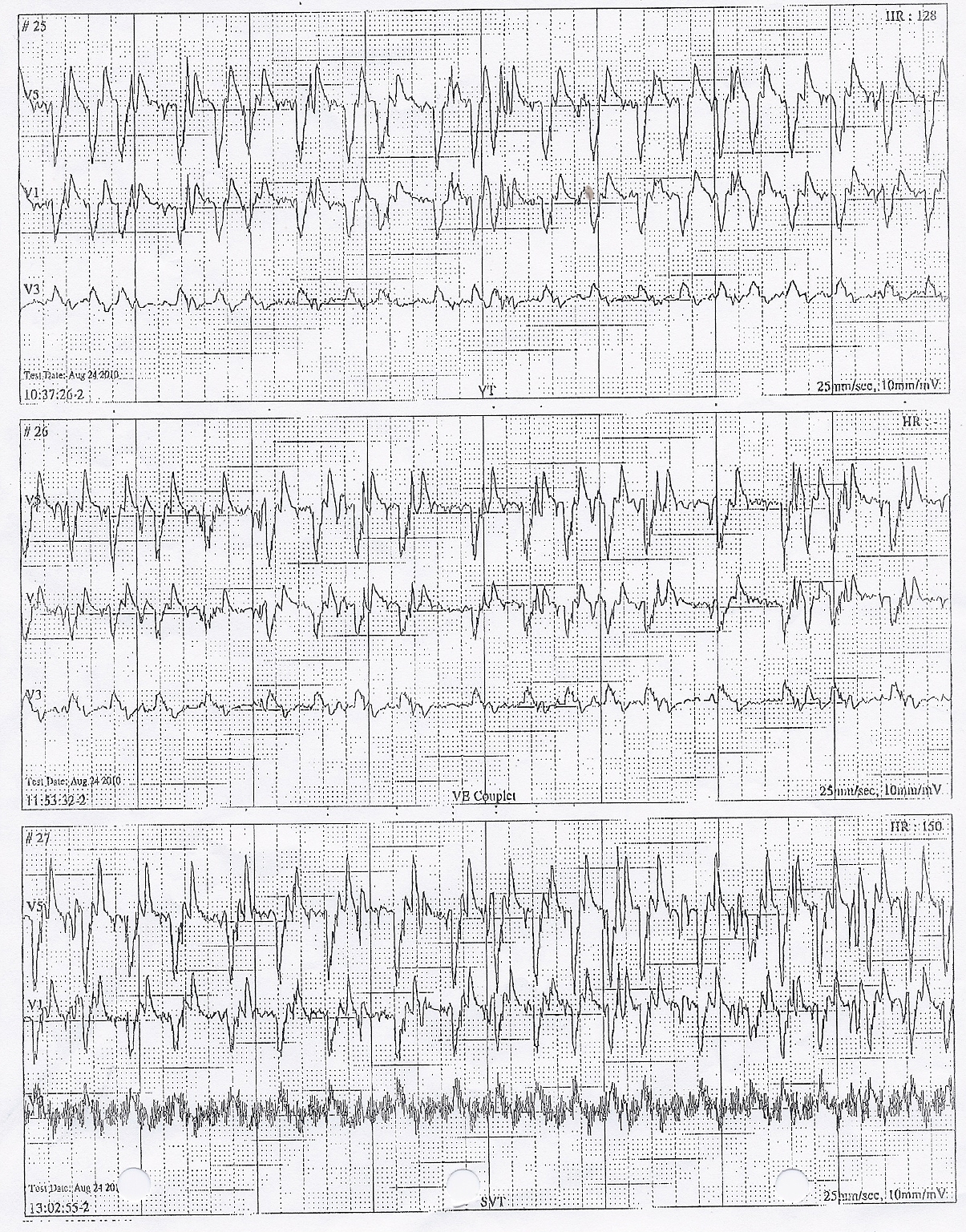
(Click to enlarge)
Proteins involved in inherited arrhythmogenic disorders.
We will now return to our more non-scientific commentary...
-Wes
Tuesday, August 24, 2010
Conflicts Galore
The public has a very clear need for disclosing conflicts of interest in medical journals. Today, the Annals of Internal Medicine published "The Affordable Care Act and the Future of Clinical Medicine: The Opportunities and Challenges" authored by Robert Kocher, MD; Ezekiel J. Emanuel, MD; and Nancy-Ann M. DeParle, JD. The only author affiliations disclosed were that of Dr. Kocher ("Dr. Kocher's service at The White House ended on 9 July 2010. He wrote the paper while he was working for the National Economic Council.").
Should Dr. Emanuel not have noted his relationship as White House advisor for health care policy and his relationship with his brother, White House Chief of Staff Rahm Emanuel? And should Ms. DeParle's disclosed her role as President Obama's so-called health czar with significant ties to private equity firms?
According to the Annals own Conflict of Interest Policy (emphasis mine):
But we should ignore this editorial blunder, right? After all, the "Affordable" Care Act is our next great health care challenge ahead!
But the veiled threat in the opening paragraph of this work might not be the best way forward:
Edicts are not away to lead health care reform. Unless and until doctors feel there is meaningful collaboration between the bureaucratic powers responsible for the Affordable Care Act that shares mutually agreeable goals, there will continue to be even bigger conflicts with doctors that will make moving this legislation forward challenging.
-Wes
Ref: The Reuter's news release.
Should Dr. Emanuel not have noted his relationship as White House advisor for health care policy and his relationship with his brother, White House Chief of Staff Rahm Emanuel? And should Ms. DeParle's disclosed her role as President Obama's so-called health czar with significant ties to private equity firms?
According to the Annals own Conflict of Interest Policy (emphasis mine):
Conflict of interest exists when an author, editor, or peer reviewer has a competing interest that could unduly influence (or be perceived to do so) his or her responsibilities in the publication process. The potential for an author’s conflict of interest exists when he or she (or the author’s institution or employer) has personal or financial relationships that could influence (bias) his or her actions. These relationships vary from those with negligible potential to influence judgment to those with great potential to influence judgment. Not all relationships represent true conflict of interest. Conflict of interest can exist whether or not an individual believes that the relationship affects his or her scientific judgment.Perhaps such disclosures only for the little people in health care who try to publish their work.
Authors, editors, and peer reviewers must state explicitly whether potential conflicts do or do not exist. Academic, financial, institutional, and personal relationships (such as employment, consultancies, close colleague or family ties, honoraria for advice or public speaking, service on advisory boards or medical education companies, stock ownership or options, paid expert testimony, grants or patents received or pending, and royalties) are potential conflicts of interest that could undermine the credibility of the journal, the authors, and science itself.
But we should ignore this editorial blunder, right? After all, the "Affordable" Care Act is our next great health care challenge ahead!
But the veiled threat in the opening paragraph of this work might not be the best way forward:
To realize the full benefits of the Affordable Care Act, physicians will need to embrace rather than resist change. The economic forces put in motion by the Act are likely to lead to vertical organization of providers and accelerate physician employment by hospitals and aggregation into larger physician groups. The most successful physicians will be those who most effectively collaborate with other providers to improve outcomes, care productivity, and patient experience.But one only has to read Sermo's message board (registration required) to get of flavor of what many doctors think about the law and this article in particular:
They ignored us the whole time they were putting this monstrosity together and ramming it through the legislative process. They got sham-"providers" in white coats for photo-ops so they could pretend we were on board. They got the AMA to play ball, knowing that the public perception would be that we were on board. In short, they were soooooo sure they didn't need us.The reality on the ground is that the law has passed and change is coming. The reality on the ground is physicians continue to see significant cuts to their profits. The reality on the ground is the physician pay fix remains unresolved and will be expensive. And the reality on the ground is doctors provide the care and the administration needs doctors to facilitate the implementation of the many health care changes that lie ahead.
And now they're in a predicament with their white elephant, and begging us for some support after the deed's been done.
Edicts are not away to lead health care reform. Unless and until doctors feel there is meaningful collaboration between the bureaucratic powers responsible for the Affordable Care Act that shares mutually agreeable goals, there will continue to be even bigger conflicts with doctors that will make moving this legislation forward challenging.
-Wes
Ref: The Reuter's news release.
Grand Rounds Is Up
This week's Blog-o-sphere Grand Rounds is being hosted at a great new blog that I must add to my sidebar, A Cartoon Guide to Becoming a Doctor:
-Wes
Webster's Dictionary defines "grand rounds" as nothing, because it's not even in there.Well done!
I was a little worried about what kind of posts people would submit, because I've observed some people have a questionable sense of humor. When I was in med school, I was an editor for our humor magazine and someone once submitted a copy of last year's physiology exam (although admittedly, that exam was pretty funny). Anyway, I shouldn't have worried. I think we have a good mix of the goofy, the twisted, the witty, the intellectual, and... the risque.
-Wes
The 10 Most Powerful People In Health Care
In case you haven't seen it, the media's list of the 100 Most Powerful People in Health Care was published yesterday. In thinking about this list I realized that in reality, these people had little to do with my patients' health care delivery. So how did they became the most powerful people in health care? Quite simply, they are not the 100 most powerful people in health care, but rather they are the 100 most powerful people overseeing the funding of health care - at least for the moment. In as little as 11 months, many of the people on this list will be gone or have moved on to their next money-making venture.
So who are the most powerful people in health care?
Well, I'd like to propose my list - maybe not of a 100 people (frankly, nothing gets done if you have a committee of 100 people anyway) - but rather my own list of the Top 10 Most Powerful People in Your Health Care today:
So who are the most powerful people in health care?
Well, I'd like to propose my list - maybe not of a 100 people (frankly, nothing gets done if you have a committee of 100 people anyway) - but rather my own list of the Top 10 Most Powerful People in Your Health Care today:
10. The Doctor - They consider the differential, write the orders, follow-up on tests, and move the health care ball forward throughout your hospitalization or stay with a rehab facility. As such, they should be given their power due, even if many other members of the health care team are actually are the ones that make sure the care happens. Still, because the doctor gets most of the liability risk if things don't happen or happen incorrectly, they just make my power list.-Wes
9. The Food Service Personnel - These folks are powerful. They have the ability to make even a clear liquid diet look like real food - especially when they mix the colors and flavors of jello. Further, proper parenteral nutrition for an ICD patient greatly shortens the sickest patient's hospitalization. Get it right and everyone benefits. Power personified.
8. The Physical Therapist - If you can't eat your food, sit up, keep your muscles toned, maintain the range of motion of your limbs when sick, the chances of returning to independent living are limited. Physical therapist have come of the most helpful techniques to get going - both physically and mentally - like turkey bowling. Their power over our patients should definitely be appreciated more.
7. The Social Worker - Want to negotiate the complex Medicare and Medicaid rules for placement in an assisted living facility? Need to get a patient to rehab? Want to arrange transportation for a patient that doesn't have a penny to their name? Make something from absolutely nothing? Call the Social Worker - but call them early in the hospital stay. (They're never at their best with last-minute consults.)
6. The Nursing Supervisor - Trust me on this. No one has more power to assure adequate staffing on each patient care ward each day than the Nursing Supervisor. Medical students and residents that cross the directives issued by this individual do so at their own peril.
5. The Bed Coordinator - If you need to admit a patient to a hospital, they must first get a bed. With many hospitals working at or near capacity, no single person has more influence over the patients admitted to a hospital facility. They find beds when no one else can. After all, it's their job.
4. The Hospital Operator - Name one person who can activate a Code Blue (cardiac arrest), find the obscure specialist in the middle of the night when they're most needed, or mobilize a trauma team faster. Can't do it? That, my friends, is power.
3. The Night Shift Nurse - At three in the morning when you're lying there in the hospital bed and need something - anything - who's the most important person in the hospital who will assure you're needs are tended to? Need I say more? If the night shift nurse is inattentive, unresponsive, irresponsible for that 8-hour shift - you're screwed. On the other hand, if she's attentive, knows when to call for help, or provides pain relief when you need it most after surgery, or - most important - gives you that laxative at 3AM - his or her power in medicine pales in comparison to any bureaucrat, politician, or hospital system CEO.
2. The Patient's Family - Often forgotten, family members have huge influence over the care provided to their loved one - especially at times where their loved one might not be able to communicate. This power should not be ignored, but it cuts both ways, too. While family members can facilitate the treatment and rehabilitation of their loved one because they know them better than anyone else, they can also prolong undue suffering if they do not comprehend the limits of care that their loved one desires in the end-of-life setting. Families that communicate their needs and wishes before anyone gets sick avoid much of the confusion during this difficult time and serve as powerful allies to the health care team.
1. You, The Patient - No one has more influence and power over their care than you. Don't want care? Leave. No one can stop you. Want care and don't have a penny? Come to the Emergency Room. You won't be turned away. Wonder what all the big buildings, waterfalls, and fancy technology were built and bought for? You. Every single person involved in health care is there because of you. So make the most of it. Come prepared. Know your medical history, medicines and allergies. If you can't remember, keep a list with you. Ask questions. Insist on clear answers. Work with your care givers, don't fight them. If you're not sure, get a second opinion. Write a letter acknowledging those that made the extra effort and scolding those that didn't. Your constructive criticism makes the system better. And know that hospitals understand the importance of your word-of-mouth referral - it's the most powerful marketing strategy a health care system can generate. Finally, remember that you can vote for politicians that don't forget who's in charge. You are the ultimate power broker in health care. Don't forget it.
Monday, August 23, 2010
How Many Times Can the Heart Be Defibrillated and Still Work?
Many, many times - like this example of 28.
But if the underlying cause for the arrhythmia isn't discovered (like the blocked artery in this man's case), the number of times that defibrillation will be successful quickly becomes limited.
-Wes
But if the underlying cause for the arrhythmia isn't discovered (like the blocked artery in this man's case), the number of times that defibrillation will be successful quickly becomes limited.
-Wes
Game-changer: A Great Idea for AED Deployment
AED4.eu for everybody:
-Wes
h/t: ePatientDave via Paul Levy at Running a Hospital blog.
Radboud University Medical Center in Nijmegen has built an emergency Augmented Reality display that allows you to look through your mobile phone's camera view and locate the nearest automatic external defibrillators (AEDs) located in a public place. It's the first independent database of AEDs in the world operated by an Academic Hospital.This is proof that some of the best ideas are the simple ones.
-Wes
h/t: ePatientDave via Paul Levy at Running a Hospital blog.
Are You the Primary Care Type?
If you're considering primary care medicine as a career someday and want some great insights into what it takes to become a good one, Dr. Rob clarifies the personality type and tolerances required.
So what does it take to be a specialist?
Exactly the same.
Except the part where he describes a possible need for outward social status and only working on left fingers.
Just realize that those extra years of training that we not-so-specialists endure are really there just so we can completely forget most of what we once knew and how to fill out discharge paperwork.
-Wes
So what does it take to be a specialist?
Exactly the same.
Except the part where he describes a possible need for outward social status and only working on left fingers.
Just realize that those extra years of training that we not-so-specialists endure are really there just so we can completely forget most of what we once knew and how to fill out discharge paperwork.
-Wes
Sunday, August 22, 2010
Why Your Insurance Premiums With United Healthcare Are High
... because they're funding foot paths for the American Heart Association with them.
Never mind that walking can be done pretty much anywhere.
And I guess it would be presumptuous of me to ask the American Heart Association to fight on behalf of patients against the bureaucratic overhead imposed by United Healthcare's newly enacted Cardiology Notification Requirement starting 1 September in Illinois now that United Healthcare has given so much money to the American Heart Association, wouldn't it?
But look at it on the bright side: at least our patients will have some nice concrete to look at while they walk.
-Wes
Never mind that walking can be done pretty much anywhere.
And I guess it would be presumptuous of me to ask the American Heart Association to fight on behalf of patients against the bureaucratic overhead imposed by United Healthcare's newly enacted Cardiology Notification Requirement starting 1 September in Illinois now that United Healthcare has given so much money to the American Heart Association, wouldn't it?
But look at it on the bright side: at least our patients will have some nice concrete to look at while they walk.
-Wes
'Twas the Week Before School Starts
(With apologies to Clement Clarke Moore)
'Twas the Week Before School Starts
by Wes and Diane Fisher'Twas the week before school starts, and all through the land,
Came traveling families with SUV's crammed.
The book bills, the dorm tab, all paid with great care,
But one more time on probation and they'll no longer be there.
The teens were all snuggled, the back seats were beds.
We pulled on to campus, with hope but some dread.
We unloaded the duffles and bags with great care,
In hopes that we would not find beer stashed somewhere.
When out on the quad, came an unearthly whine,
As all texted each other, to say they were fine.
Away to my cell phone, we looked with concern,
But nary a message did we get in turn.
The piercings, the highlights, oh, how they glistened!
They checked out each other, while the parents just listened.
When what to my wondering eyes should appear,
But a parent liason, saying "Nothing to fear."
And the smiling dean, so lively and quick,
Asking each family to please buy a brick.
More rapid than eagles, the roommates they came,
I never knew my offspring had garnered such fame.
I need curtains, more CD's, a lamp and a chair,
A new pillow, some snacks and that gel for my hair.
To the Target, the Best Buy, a sweep through the mall,
Then dash away, dash away, dash away all.
They promised to study, they promise more mail,
Daddy was stoic, and Mommy was pale.
They threw out an "I love you," gave a hug, hands were shook.
Then away they all flew, without one second look.
Then I heard them exclaim, as I drove out of sight,
"My parents are gone, tonight's party night!"
Tuesday, August 17, 2010
Nay Fellow Way?
It was to be a routine pacemaker.
The parties assembled. The room prepped. IV started. Chest scrubbed. Antibiotics given. His nervous eyes raised when he saw me before the procedure, relieved at the sight of at least one familiar face.
"Are you ready?" I asked.
"Yes," he replied, "I think so."
"Any last minute questions?"
"I don't think so," he said.
"Great! Then let's get this over with..." I turned to the lab staff and signaled them to proceed.
"Oh, doc! I forgot. Can I speak with you a second? Ya know, privately?"
"Sure," I said returning gurney-side. I drew the curtain.
He leaned forward and whispered: "Doc, no fellow, right?"
I stopped and contemplated the question, then acquiesced. "Would you mind if I use one as my scrub tech, but I'll be the primary operator?" I asked.
"Yeah, that would be okay - as long as you're the primary operator."
* * *
This little exchange got me thinking: what would I want? Honestly, I'd probably want an attending physician working on me, too. After all, it makes sense, right? Get the most experienced hands and all.
But there are good reasons to have a fellow involved with your surgery, if the opportunity presents itself:
It might just be the best thing you ever did.
-Wes
The parties assembled. The room prepped. IV started. Chest scrubbed. Antibiotics given. His nervous eyes raised when he saw me before the procedure, relieved at the sight of at least one familiar face.
"Are you ready?" I asked.
"Yes," he replied, "I think so."
"Any last minute questions?"
"I don't think so," he said.
"Great! Then let's get this over with..." I turned to the lab staff and signaled them to proceed.
"Oh, doc! I forgot. Can I speak with you a second? Ya know, privately?"
"Sure," I said returning gurney-side. I drew the curtain.
He leaned forward and whispered: "Doc, no fellow, right?"
I stopped and contemplated the question, then acquiesced. "Would you mind if I use one as my scrub tech, but I'll be the primary operator?" I asked.
"Yeah, that would be okay - as long as you're the primary operator."
* * *
This little exchange got me thinking: what would I want? Honestly, I'd probably want an attending physician working on me, too. After all, it makes sense, right? Get the most experienced hands and all.
But there are good reasons to have a fellow involved with your surgery, if the opportunity presents itself:
- We need to keep training. None of us will be doctors forever, and now more than ever with tons of people entering the health care marketplace there is a need to have well-trained doctors in place to meet the need ahead. You can read all you want about how to do a procedure, but until you've done one yourself on a living, breathing individual, you have no concept of the complexities involved. Starting slow in a closely supervised, supportive setting, makes for some very technically-savvy doctors of tomorrow.
- They improve your surgical technique. The better I can teach someone to do what I do, it seems the easier it is for me to do it, too. Throughout our careers as doctors, we work hard to solidify our competency "brand" amongst our patients and peers. Particularly for specialists: screw up a case or two and your "brand" is quickly tarnished. This is especially important as we train fellows - none of us wants to tarnish our "brand" when trainees work with us either. Therefore, you better bet that bottom dollar we'll be supervising those fellows closely.
- Fellows keep you sharp. Oh sure, they often ask mundane questions but occasionally they ask remarkably astute questions, too. When this happens, they make us think and as a result, we all get smarter.
- They're another set of eyes and hands.It never hurts to have another set of eyes contribute their interpretation to a tough case nor an extra set of hands for that extra retractor. Ever.
- They slow you down. There is no question that teaching someone else takes more time than doing a procedure yourself. This definitely has its downside. But time spent now might pay large dividends in the future when that same doctor has to work on you someday. Also, spending a bit more time can have it's upsides - especially if you really don't want to have dinner with your mother-in-law.
- More often than not, fellows are extra-careful. By their very inexperience and their desire to excel in training, I have found most fellows I work with especially conscientious when they dealing with patient and their procedures.
It might just be the best thing you ever did.
-Wes
Monday, August 16, 2010
Some Helpful Healthcare Advice for College-Bound Students
Call your lawyer first:
-Wes
h/t: Instapundit.
After a few clients ran into difficulty getting information about adult children who were ill, Sheila Benninger, an attorney in Chapel Hill, N.C., began recommending that clients' children designate a health-care power of attorney after they turn 18 to identify who can speak for them if they can't.It's good advice for those of us shipping one more child back to college this week.
She also includes a Health Insurance Portability and Accountability Act, or HIPAA, release form that allows patients to determine who can receive information about their medical care and whether information about treatment for substance abuse, mental health or sexually transmitted diseases can be disclosed.
You don't have to use a lawyer. Generic health-care power-of-attorney forms can be found online. If the school has a HIPAA release online, it's best to use that more-tailored document.
Parents should keep a copy in an email folder, where it can be easily accessed in an emergency. And students should designate a general power of attorney so someone can pay bills or handle other issues if they go abroad.
-Wes
h/t: Instapundit.
On the ACC's Growing Pains With Social Media
As discussed by Emily Zeigenfuse of the American College of Cardiology (ACC):
Of course, the greatest challenge will be getting doctors to realize the benefits of social media compared to the liabilities when interacting with patients this way. Still, the value of providing rapid, reputable content to patients while improving their understanding of complicated treatments should serve to improve the caliber of health information available to our patients and might just improve outcomes.
-Wes
We went live on June 14, 2010, and we’ve had a few challenges. The website wasn’t 100% perfect, and our readers let us know immediately. The comments box, where we expected readers to discuss medical content, was used instead for help-desk issues, which inhibited the discussion of cardiology topics.Kudos for the ACC for getting involved with social media. Their efforts will help pave way for others interested in using the medium creatively to address issues important to doctors and their patients.
Since then, we’ve added a separate button to report tech problems, collaborated directly with members who left complaints, and took a second look at usability. It’s been a sleepless summer, but we’ve solved a lot of problems quickly by honestly listening to and engaging our readership.
Lastly, what other trends do you see in health care social media? What’s next?
I’m very curious about how mobile devices will fit into a doctor’s daily workflow. We know our members, by virtue of being on their feet all day, spend less time in front of a computer than those of us with desk jobs. We’re also watching how patients with chronic diseases like heart disease use social media to talk about their condition so that we can reach them in those spaces.
Of course, the greatest challenge will be getting doctors to realize the benefits of social media compared to the liabilities when interacting with patients this way. Still, the value of providing rapid, reputable content to patients while improving their understanding of complicated treatments should serve to improve the caliber of health information available to our patients and might just improve outcomes.
-Wes
Sunday, August 15, 2010
Inhaled Incense "K2" May Cause Heart Damage
From Children's Medical Center in Dallas, Texas:
More from Fairplay, MO.
"We're theorizing that something in the K2 caused his coronary arteries to spasm, causing blockage of blood flow temporarily to his heart," said Dr. Colin Kane, a pediatric cardiologist who treated both cases. "He had a heart attack."And yet it appears some have not gotten that message:
Kane said he had never even heard of K2 before. He scoured journals and the Internet for legitimate medical research on it; right now, there isn't any.
He is now educating colleagues at Children's Medical Center about K2, including what to look for and especially what to ask teenagers who come in with unexplained heart problems. Since K2 has yet to be studied, no one is really sure what it can do to the body.
K2 is a mixture of herbs and spices manufactured as an incense. According to a company website, K2 is not meant for human consumption.
K2 is incense – a blend of herbs and spices sprayed with a synthetic compound similar to THC (delta-9-tetrahydrocannabinol) found in marijuana. The combination looks like crushed potpourri. Blends are traditionally burned in incense pots; however, teens roll the K2 incense in wrappers to make joints, or they smoke it in pipes. When smoked, K2 delivers a high similar to that of marijuana. Users claim it's almost impossible to tell the difference between the two.-Wes
More from Fairplay, MO.
How Old Is Too Old in Medicine?
With apologies to the Beatles...
When I get older, losing my hair, many years from now, ...This story presents an interesting dilemma in this era of shrinking retirement income for our seniors who want to continue to work.
Will you see need me, will you still feed me...
...when I'm ninety-four:Former NYPD chief cardiologist Dr. Irving Kroop retired in 1986 -- when he was 70 -- with a $64,364 disability pension awarded because of a bad heart, according to sources and city records.
All the while, he's maintained a private practice in Brooklyn and moonlighted at NYCERS, the New York City Employees Retirement System, which paid him $14,479 last year to help determine whether other city workers should get disability pensions.
Hats off to the man -- he's 94 years old but disabled? And still going strong?" said an incredulous Carol Kellerman, head of the Citizens Budget Commission.
Kroop, who gets $155 an hour as a private contractor for city's civilian pension board, shuffles into examining rooms with a cane and oxygen tank, sources say.
Should there be an age limit for practicing doctors? How do we assess if a doctor is "disabled" as they age? Should we care? Should cardiologists performing physical examinations at an advanced age have, say, an annual hearing and vision test to assure they can still hear heart sounds or see jugulovenous distension?
Or is the ability to walk into an exam room with a cane (rather than a walker) while wearing oxygen enough to certify them capable to practice medicine?
-Wes
PS: 94's chump change. How about 100 and still practicing?
(h/t @DrDeanBurke on Twitter)
Health Care's Dangerous Politics
"An election is coming. Universal peace is declared, and the foxes have a sincere interest in prolonging the lives of the poultry."* * *~George Eliot, Felix Holt, Chapter 5
This morning, the chickens learned from two former independent public trustees for Medicare and Social Security what the foxes in our political hierarchy were up to with their recent budget forecasts for Medicare :
... the program's long-term deficit may be roughly three times what the trustees projected.Politician's fudging the numbers?
. . .
In addition, for the third consecutive year there were no independent Medicare trustees to issue a separate statement. Without them, the Obama administration was able to put forward an unjustifiably positive outlook for the Medicare program and the impact of the health care legislation. If public trustees had been in place, they could have helped ensure that a more realistic view was presented in the report, possibly including a reasonable best estimate along the lines set out in the chief actuary’s alternative.
Say it ain't so!
But don't worry. It's only America's health care we're taking about. The new entitlement programs will be better. Much better.
Really.
. . .
What's that?
Why don't you trust me?
-Wes
Wednesday, August 11, 2010
Living the Questions
"Live the questions now. Perhaps then, without hardly noticing, you will live along some distant day into the answers.”With the tectonic shifts underway in America's health care delivery model, doctors influence in shaping the forces ahead seems to be dwindling.
- Rainer Maria Rilke
It started with the entire health care bill drafted by a team of some undisclosed, very influential academics, lawyers and policy wonks adept at social security and tax laws and was morphed by corporate and hospital interests with huge political and financial influence. Before the legislation was even read, the American Medical Association had stamped their seal of approval, worried that "they'd be eaten if they weren't at the table." As a result, a significant number, no, I'll stick my neck out here and say a majority of doctors, had little to do with shaping health care in America as we will come to know it.
But I would also bet that most of Americans want doctors with their best interests at heart to be integral participants in shaping our new health care system.
So now, as doctors align themselves with a single health system employer so they can beg for a portion of the government's soon-to-be-implemented "bundled" (bungled?) payment scheme to health care systems for episodes of care, how will doctors have any meaningful voice at improving health care for our patients and ourselves?
Enter social media.
I do not think social media, especially health care social media, is the best avenue to interact with patients. It's simply too risky on too many levels. But when interacting with colleagues on a professional level - it might be perfect.
It's fast. It's instantaneous. And most important:
It can influence.
But doctors must get used to creating influence not based on the scientific method as we know it. Doctors must get used to the influence imparted by lightning strikes.
As a simple analogy, Susan Boyle was a lightning strike (though not for medicine, per se). Her plain appearance meant little when it was contrasted with her powerful voice and its influence on the music scene at the time.
To administrators and regulators, doctors have a very plain employee-like appearance but carry powerful ties to their patients and are therefore uniquely situated to create their own lightning strikes in health care.
But doctors do not have time to sit in lengthy meetings planning strategies. Doctors (except a very few of us) have no interest in creating their own blogs. Doctors do not have time to endlessly perseverate on administrative and insurance issues as they try to repair a ruptured spleen.
But doctor are on line. Doctors do have cell phones. Increasingly, those cell phones are smart phones. And doctors can use social media to influence.
Of course, tons of websites are popping up all over promising to do just that for doctors. The New England Journal if Medicine, Sermo, iMedExchange, LinkedIn and a whole host of others - each with their registration process and promise of becoming the perfect Electronic Doctor's Lounge to interact (aka, waste time) with your peers. But these probably aren't going to influence health care policy and procedures in a meaningful way because there's just too many of them out there.
But I DO think doctors understand the need to know what's going on, but want a simple way to do it. Doctors want a simple way to connect and aire their concerns - irrespective of their employer. Doctors should participate in improving their care of patients.
And yes, right now, this minute, none of us has all the answers.
But here's the thought: we can all ask the questions. We can pose the problems we see today that influences our patients' care. We can collaborate and sign up for Twitter to follow our colleagues and maybe, just maybe, "without hardly noticing, we will live along some distant day into the answers."
Lightning strikes and all.
-Wes
Tuesday, August 10, 2010
Chicago Cardiology Market Shifting
"Come gather 'round peopleEven the largest private cardiology groups here in the Chicago area are bailing out of their practices and swimming to join a large health system:
Wherever you roam
And admit that the waters
Around you have grown
And accept it that soon
You'll be drenched to the bone.
If your time to you
Is worth savin'
Then you better start swimmin'
Or you'll sink like a stone
For the times they are a-changin'."
Midwest Heart Specialists, the state's biggest cardiology practice, with 50 physicians blanketing the west and northwest suburbs, is in sale talks with Advocate Health Care and possibly others, sources say. And last week another cardiology group, Illinois Heart & Vascular, was acquired by Adventist Midwest Health, which will add 15 heart doctors to two of Adventist's four west suburban hospitals.* * *
"The line it is drawn
The curse it is cast
The slow one now
Will later be fast
As the present now
Will later be past
The order is
Rapidly fadin'.
And the first one now
Will later be last
For the times they are a-changin'."
-- Lyrics from "The Times They Are a Changing" by Bob Dylan
-Wes
Lab Wars and the Doctor-Patient Relationship
From a somewhat threatening form letter I received from Peter McCauley, MD, Midwest Marketing Specialist, CIGNA, dated 1 August 2010:
What will I tell my employer whose lab services I use because they're integrated with our electronic medical record?
Let's see. Soon I will have to call one insurer to get an authorization to implant an emergent pacemaker and now I find I have to call another insurer's laboratory chain to obtain my patient's lab tests, even though that chain is not integrated with our EMR system.
Looks like it's time to add every patient's insurance provider to their medical problem list.
There is simply no way doctors can keep all of these insurance gymnastics straight AND provide health care, yet here we are with yet another example of how third parties are creating an adversarial relationship between doctors and their patients while actually decreasing the efficiency and quality of patient care.
-Wes
Dear Westby Fisher,And the letter goes on to describe why I must transition my patients to CIGNA's labs.
By using a CIGNA in-network laboratory, including two of the largest national laboratories, Laboratory Corporation of America (LabCorp) and Quest Diagnostics, Inc., as well as other regional and niche laboratories, you and your patients can have a greater choice and access to an extensive list of patient service center and quality service at competitive rates.
As highlighted below, using a non-participating laboratory has important implications:Patients
- Individuals, depending on the nature of their health benefits, face the potential of higher costs and avoidable impacts on their deductibles or health savings accounts.
- Individuals with no out-of-network benefits may have no coverage at all.
- Use of non-participating laboratories will decrease the amount of maximum lifetime benefits available to individuals.
Physicians
- Under your contract with us, you agreed to refer your CIGNA patients to contracted in-network laboratories, unless otherwise authorized by CIGNA. It is important that this agreement be honored.
- Unwarranted use of non-participating laboratories may adversely affect our business relationship
What will I tell my employer whose lab services I use because they're integrated with our electronic medical record?
Let's see. Soon I will have to call one insurer to get an authorization to implant an emergent pacemaker and now I find I have to call another insurer's laboratory chain to obtain my patient's lab tests, even though that chain is not integrated with our EMR system.
Looks like it's time to add every patient's insurance provider to their medical problem list.
There is simply no way doctors can keep all of these insurance gymnastics straight AND provide health care, yet here we are with yet another example of how third parties are creating an adversarial relationship between doctors and their patients while actually decreasing the efficiency and quality of patient care.
-Wes
Monday, August 09, 2010
Keepers
When fishing, you never seem to remember the fish you threw back because they were too small, but you would always remember the "keepers."
Surgeons, too, have keepers, they just don't always show them to you.
But today, courtesy of one of my patients, I got to see some "keeper" gallstones (one of which measures about 2.5 cm in size) that were recently snatched from her belly and are now offered solely for your edification:



Boy, makes your mouth water, doesn't it?
-Wes
Surgeons, too, have keepers, they just don't always show them to you.
But today, courtesy of one of my patients, I got to see some "keeper" gallstones (one of which measures about 2.5 cm in size) that were recently snatched from her belly and are now offered solely for your edification:



Boy, makes your mouth water, doesn't it?
-Wes
Insurers Excluding Pricey Hospitals
From Crain's Chicago Business:
-Wes
Every one of the 60 workers at Amitron Corp. snapped up the suburban manufacturer's new health insurance plan this spring, even though they won't be able to use marquee hospitals like Northwestern Memorial, Children's Memorial or University of Chicago Medical Center.Now, imagine what would happen if patients could chose from a range of insurers across state lines, too...
Those pricey, brand-name places were among a handful left out of a new PPO plan from UnitedHealthcare of Illinois aimed at mid-sized businesses weary of spiraling health care costs. Cutting out more-expensive hospitals and doctors can save companies as much as 15% on premiums.
Amitron, a circuit-board maker, still offers UnitedHealthcare's standard PPO, which allows workers to go to any hospital in metro Chicago. “But nobody takes it because it's so expensive,” says Amber McKibben, office manager at the Elk Grove Village-based company.
-Wes
More on Doctors and Electronic Communication
Some thoughtful responses to my prior post on the devaluation of doctors' time were published this weekend as doctors set boundaries in their new role as uncompensated information technology managers:
Having said that, many patient inquiries to their doctors are for test results. I believe patients will continue to demand greater access to their test results whether doctors like it or not, espcially as they are responsible for paying more of their health care dime. We should look at this as a good thing. But our current model of the electronic medical record sending every single result to our inbasket, even though it contains previously read or acted-upon results is creating a "Boy-Who-Cried-Wolf" scenario for doctors suffering from information overload. The electronic medical record must to a better job of filtering the myriad of tests that end up in our inbasket each day (I'm thinking of EKG final results that I have already read or recurrent INR test results within a therapeutic range, for instance).
I suspect the day will come where we will move to releasing test results to patients before physician review out of necessity to avoid reporting delays. If that day happens, patients should understand that not all abnormal test results may require an action, but their doctor is the only one who should interpret the importance of any abnormal result based on their entire medical history.
-Wes
Bryan Vartabedian, MD gives his take on this issue, noting what happens if doctors request payment for their responding to e-mails:I'm not sure I agree with NO e-mail interaction with patients, since some simple requests or clarifications using the medium might actually reduce time for all involved. (It would be great e-mails were limited to a short length like Twitter, maybe 140-characters. Heh.) But Dr. Rob's approach is an appropriate effort to set limits on doctor's uncompensated time and until a model is created to compensate doctors for their work, few will tend to adopt it into their daily routines.I’ve seen it too many times: Physicians excited to please open the door to unlimited patient email only to see themselves shutting their families out at night as they answer questions – all for free. And those physicians who suggest that emails should carry a fee are indicted for greed.Dr. Rob over at Musings of a Distractible Mind and 14-year veteran of the electronic medical record counters with his group's approach: they simply don't take e-mails.
Having said that, many patient inquiries to their doctors are for test results. I believe patients will continue to demand greater access to their test results whether doctors like it or not, espcially as they are responsible for paying more of their health care dime. We should look at this as a good thing. But our current model of the electronic medical record sending every single result to our inbasket, even though it contains previously read or acted-upon results is creating a "Boy-Who-Cried-Wolf" scenario for doctors suffering from information overload. The electronic medical record must to a better job of filtering the myriad of tests that end up in our inbasket each day (I'm thinking of EKG final results that I have already read or recurrent INR test results within a therapeutic range, for instance).
I suspect the day will come where we will move to releasing test results to patients before physician review out of necessity to avoid reporting delays. If that day happens, patients should understand that not all abnormal test results may require an action, but their doctor is the only one who should interpret the importance of any abnormal result based on their entire medical history.
-Wes
Saturday, August 07, 2010
When The Doctor's Always In
 The devaluation of doctors' time continues unabated.
The devaluation of doctors' time continues unabated.As we move into our new era of health care delivery with millions more needing physician time (and other health care provider's time, for that matter) - we're seeing a powerful force emerge - a subtle marketing of limitless physician availability facilitated by the advance of the electronic medical record, social media, and smart phones.
Doctors, you see, must be always present, always available, always giving.
This is not a new trend. We saw a similar situation years ago with the advent of the digital beeper. Even the most basic of private bodily functions in the bathroom could be interrupted at a moment's notice. The expectation that phone calls should be returned instantly grew from this - personal context be damned. Doctors were accepting of these intrusions, however; the feeling of being omni-present, omni-available, and omni-beneficent fit nicely with the Marcus Welby, MD psyche of the time. After all, there were financial advantages to being available and the most responsive gained a competitive edge.
But medical care based on electronic communications is commandeering doctors' personal lives. Our instantaneous availability is breathlessly touted by health care systems eager to serve their patient customers. Batches of test results are reported electronically but still require human review - one at a time. With hundreds of thousands of patients registering online for their new level of doctor-patient communication, the requirement to respond quickly to patient requests taxes even the most diligent physician providers. To preserve their personal life and get home at a reasonable hour each day, test reviews and patient communications are increasingly performed from home - all for free. Worse, our similarly web-enabled patient population has learned that many of their health care issues can now be addressed online free of charge - just send a two-page e-mail - who needs an office visit?
Increasingly the question becomes - if we choose future doctors on their willingness to sacrifice for others without expectation of appropriate boundaries and compensation - will we be drawing from the same pool of people as the ones who will make the best technically-skilled clinicians? What type of person will enter medicine if they know that their personal life will always take second place to patient care? For the doctors who accept this choice, what are the risks to patients when they interact with doctors who are "crackberry" addicts without personal or family boundaries? Should our medical students expect that their lives will be surrendered to their patients, free of charge, as they answer the never-ending bounty of health care questions online?
Electronic medicine is here with all its bells and whistles - I get that. But it does not come for free nor without consequences to doctors' time and personal lives. Establishing appropriate boundaries for electronic physician access will be our next great challenge, otherwise the last drop of the milk of human kindness might just be wrung from us.
-Wes
Friday, August 06, 2010
Cardiology Contraction Continues
Health care reform continues to affect cardiologists through bankrupcy, hospital turf wars, and burnout:
-Wes
The ER also is on track to lose on-call cardiology coverage at the end of August, when Dr. Marvin Mills will stop taking calls around the clock.Decreased patient access to cardiologists is becoming more common, especially in rural communities.
Mills, who will continue to care for all his own patients, has been the hospital’s sole on-call cardiologist since Diagnostic Cardiology Group left the hospital in October. He declined to comment.
“Being the only on-call cardiologist for the length of time he has is a substantial burden,” Perlaky said. “Many times I’ve called him in the middle of the night because there’s been a patient with chest pains and he’s always been cordial, gracious and willing to help. It’s not like he’s abandoning us; he’s paid his dues.”
-Wes
Medicare's Escher-Like Budget Logic
 Everyone knows the doctor cuts will never happen:
Everyone knows the doctor cuts will never happen:"I’m not willing to do that by punishing hard-working physicians or the millions of Americans who count on Medicare. That’s just wrong."... except when they must happen to make the Medicare budget work.
- President Obama 12 Jun 2010
Oh, and rest assured we can continue to cut costs in Medicare without affecting the quality of care provided.
-Wes
Thursday, August 05, 2010
The Toughest Route to Becoming a Doctor
... occurs after a liver, heart, lung, and kidney transplant:
-Wes
Allison John, 32, made medical history in 2006 after she received her fourth organ transplant -- a kidney from her father, 61-year-old David John, to add to her previous heart, lung and liver transplants.Wow.
A life plagued by illness and frequent hospital visits has not deterred John from her dream of becoming a doctor, however. After 14 years of interrupted study, she finally received her medical degree from Cardiff University last month, according to the U.K. press.
-Wes
Tuesday, August 03, 2010
Al Fine
“The family wants the pacemaker turned off.”
“We don’t typically turn them off.”
“They want it off.”
“It’s 2 am, can it wait?”
“I don’t think so.”
“I’ll head in.”
Bleary-eyed, I rose from bed, dressed, and was out the door. The cool air from the car window served as nature's wake-up call. The sky was clear, the moon hung brightly on the horizon and the cicadas’ shrill songs undulating high above. Driving in, the tires clapped rhythmically from one pavement segment to the next.
* Kla-lup, kal-lup, kal-lup *
For some reason the Emergency Room seemed farther away this night – perhaps because of my reluctance to go there. If the patient was pacemaker dependent, yet alive with a pulse and neurologic signs, the ethical dilemma was a real one: should I be responsible for stopping the patient's heart? Did the family really understand the implications of these actions?
* Kla-lup, kal-lup, kal-lup *
I turned the final time. The ER sign disrupted the dark sky. I parked and fumbled for my ID. The security guard looked remarkably cheery for that time of night.
Reviewing the case, it was a horrible fall, cerebral hemorrhage, neurosurgeon empathically discussed the prognosis with the family and me – little could be done.
On entering the room, what seemed like twenty pairs of eyes were upon me. Some older, some younger, older kids too. Questioning at first. Tearful. Some closed. It had been a long day. So glad I came. Others pointing the way to her, quietly huddled by his side, clutching his hand. She turn her gaze from him for a moment, offered a brief smile, then back to him again. "He was a great man," she said.
Except for the c-collar in place, he looked regal - staring up without movement. He looked younger than his age, an active lifestyle I guessed. His endotrachial tube had already been removed. "We don't want him to suffer."
I glanced at the monitor. 100% ventricular pacing.
Damn.
"We'd like the pacemaker turned off," they reinforced.
"You understand that he might die as a result."
"Yes."
"There's a chance his heart could slow significantly, and not stop."
"We understand. If that's God's will."
I turned to his wife. She seemed at peace. I asked her:
"Are you sure this is how he'd want it?"
"Yes."
"And you understand what we're doing?"
"Yes."
"Would you like to be the one to turn off his pacemaker?"
"Honestly, no. But I'm his wife. This is how he'd want it."
"I'll grab the programmer and be right back. I'm so sorry."
I left the room, wrote a thorough note and pondered the situation as I walked to get the programmer. Usually some other metabolic derangement assists us in stopping the heart of patients with pacemakers - we don't usually turn them "off." The natural consequence of other confounding diseases work to cause a lack of oxygen, too much potassium, or another metabolic problem that disconnects the electrical activity from the mechanical. When the mechanical stops, it really doesn't matter what the electrical system does, since the pumping stops irrespective of the electrical impulses applied to the heart.
* sigh *
I returned and checked the device. Naturally, there was still plenty of battery life left. The rhythmic sound of the monitor was heard in the background as I noted his underlying atrial fibrillation with ventricular pacing.
Da Capo
The family huddled together. They gave Grampa a kiss. More tears. What was I doing? She held his hand, leaned forward, and whispered something in his ear. She did not cry. She was turned and shuffled to the programmer, assisted by her daughter. They stood together, arms entwined. The monitor was hushed, the waveform still visible.
Pianissimo
I handed her the pen and pointed to the spot to touch to program his pacemaker to "off." She looked at the others. They stood together, resolute, tears flowing. She touched the screen. The programmer responded to make sure that this is what she wanted. She confirmed, "Yes."
The pacemaker responded in kind. A long pause, then a slow escape rhythm.
Larghissimo
We were all granted a reprieve. It was not time. A few more notes of the concert called life were still to be played. They thanked me. "Would you mind if we were alone with him?"
"No. Not at all."
I packed up the programmer and pulled the curtain to provide privacy. The monitor out side the room showed an escape rhythm just faster than before. I appended my note with the recent events, spoke with the ER staff, returned the programmer, and headed home.
D.C. al fine.
I was grateful that I could not predict the tempo of death. It was His concerto, not mine after all. As I drove home I noticed the moon was no longer visible on the horizon and in its place were millions of radiant stars.
His metaphor, too.
-Wes
“We don’t typically turn them off.”
“They want it off.”
“It’s 2 am, can it wait?”
“I don’t think so.”
“I’ll head in.”
Bleary-eyed, I rose from bed, dressed, and was out the door. The cool air from the car window served as nature's wake-up call. The sky was clear, the moon hung brightly on the horizon and the cicadas’ shrill songs undulating high above. Driving in, the tires clapped rhythmically from one pavement segment to the next.
* Kla-lup, kal-lup, kal-lup *
For some reason the Emergency Room seemed farther away this night – perhaps because of my reluctance to go there. If the patient was pacemaker dependent, yet alive with a pulse and neurologic signs, the ethical dilemma was a real one: should I be responsible for stopping the patient's heart? Did the family really understand the implications of these actions?
* Kla-lup, kal-lup, kal-lup *
I turned the final time. The ER sign disrupted the dark sky. I parked and fumbled for my ID. The security guard looked remarkably cheery for that time of night.
Reviewing the case, it was a horrible fall, cerebral hemorrhage, neurosurgeon empathically discussed the prognosis with the family and me – little could be done.
On entering the room, what seemed like twenty pairs of eyes were upon me. Some older, some younger, older kids too. Questioning at first. Tearful. Some closed. It had been a long day. So glad I came. Others pointing the way to her, quietly huddled by his side, clutching his hand. She turn her gaze from him for a moment, offered a brief smile, then back to him again. "He was a great man," she said.
Except for the c-collar in place, he looked regal - staring up without movement. He looked younger than his age, an active lifestyle I guessed. His endotrachial tube had already been removed. "We don't want him to suffer."
I glanced at the monitor. 100% ventricular pacing.
Damn.
"We'd like the pacemaker turned off," they reinforced.
"You understand that he might die as a result."
"Yes."
"There's a chance his heart could slow significantly, and not stop."
"We understand. If that's God's will."
I turned to his wife. She seemed at peace. I asked her:
"Are you sure this is how he'd want it?"
"Yes."
"And you understand what we're doing?"
"Yes."
"Would you like to be the one to turn off his pacemaker?"
"Honestly, no. But I'm his wife. This is how he'd want it."
"I'll grab the programmer and be right back. I'm so sorry."
I left the room, wrote a thorough note and pondered the situation as I walked to get the programmer. Usually some other metabolic derangement assists us in stopping the heart of patients with pacemakers - we don't usually turn them "off." The natural consequence of other confounding diseases work to cause a lack of oxygen, too much potassium, or another metabolic problem that disconnects the electrical activity from the mechanical. When the mechanical stops, it really doesn't matter what the electrical system does, since the pumping stops irrespective of the electrical impulses applied to the heart.
* sigh *
I returned and checked the device. Naturally, there was still plenty of battery life left. The rhythmic sound of the monitor was heard in the background as I noted his underlying atrial fibrillation with ventricular pacing.
Da Capo
The family huddled together. They gave Grampa a kiss. More tears. What was I doing? She held his hand, leaned forward, and whispered something in his ear. She did not cry. She was turned and shuffled to the programmer, assisted by her daughter. They stood together, arms entwined. The monitor was hushed, the waveform still visible.
Pianissimo
I handed her the pen and pointed to the spot to touch to program his pacemaker to "off." She looked at the others. They stood together, resolute, tears flowing. She touched the screen. The programmer responded to make sure that this is what she wanted. She confirmed, "Yes."
The pacemaker responded in kind. A long pause, then a slow escape rhythm.
Larghissimo
We were all granted a reprieve. It was not time. A few more notes of the concert called life were still to be played. They thanked me. "Would you mind if we were alone with him?"
"No. Not at all."
I packed up the programmer and pulled the curtain to provide privacy. The monitor out side the room showed an escape rhythm just faster than before. I appended my note with the recent events, spoke with the ER staff, returned the programmer, and headed home.
D.C. al fine.
I was grateful that I could not predict the tempo of death. It was His concerto, not mine after all. As I drove home I noticed the moon was no longer visible on the horizon and in its place were millions of radiant stars.
His metaphor, too.
-Wes
Subscribe to:
Comments (Atom)