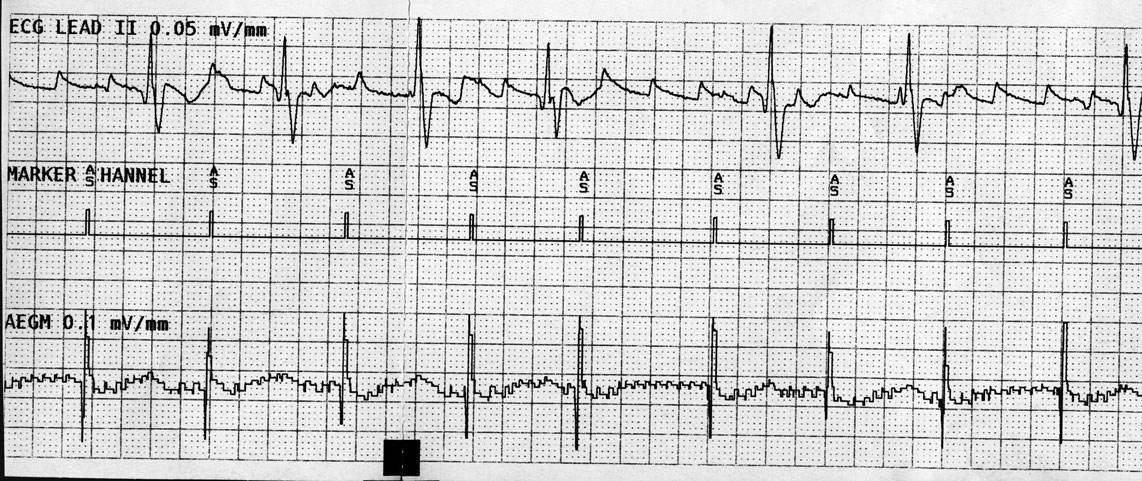
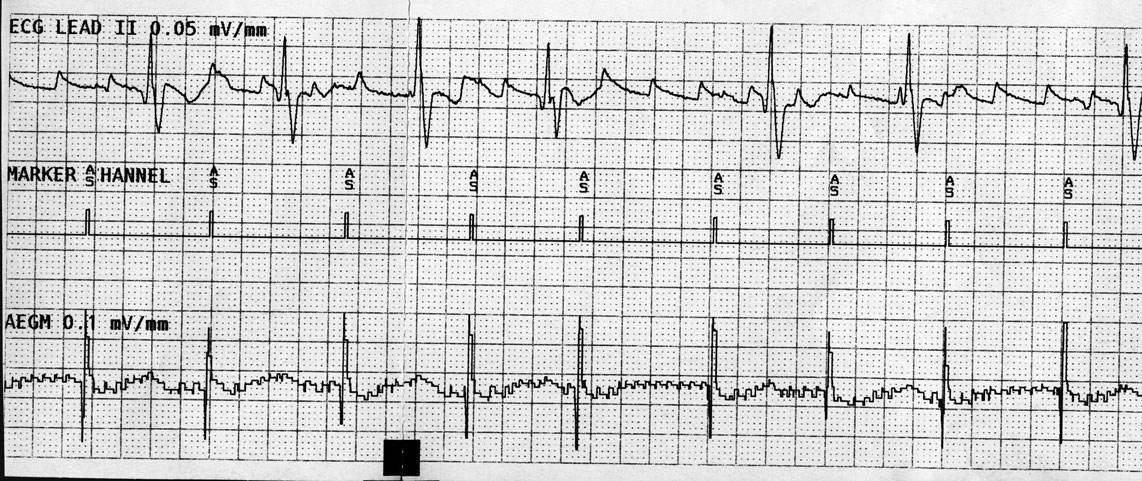
Here's a recent pacemaker interrogation showing a simultaneous surface EKG (top tracing), right atrial marker channel (center tracing) and right atrial electrogram (bottom tracing) from a patient who underwent aortic valve replacement over 30 years ago and later mitral valve replacement about 6 years ago. He has had multiple bouts of symptomatic atrial flutter that have responded to electrical cardioversion. His echocardiogram has demonstrated a nearly 7-centimeter left atrium, among other things. He was now fairly asymptomatic at the time of this recording:
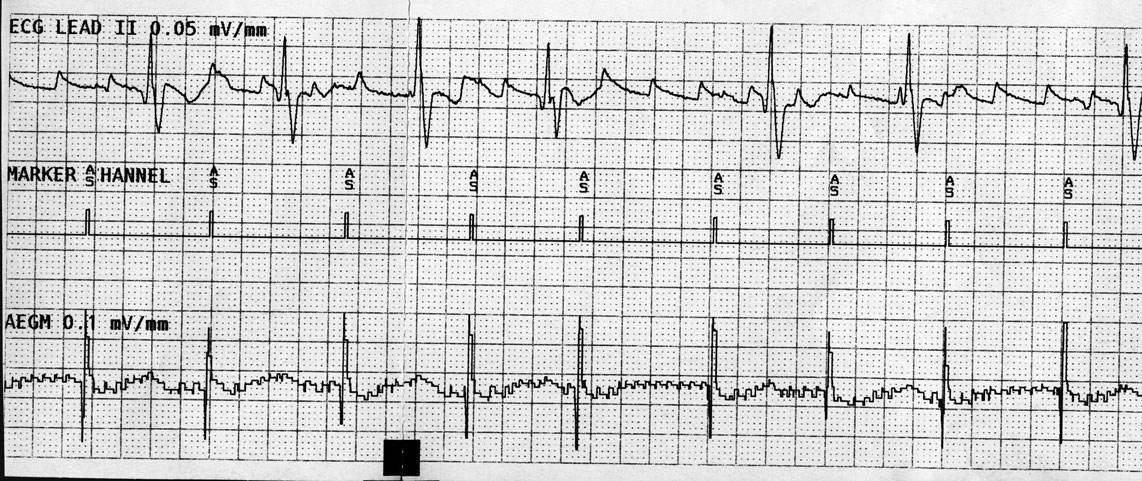
Click image to enlarge
How does one explain what's seen?
-Wes
hat tip: Alan D. Kogan, MD for supplying the tracing.
7 comments:
that's really weird.
his surface tracing looks like flutter, but there is no flutter on the marker channels or the atrial lead electrogram, and those seem to be consistent with irregular discrete atrial beats. they don't conduct to the ventricle with regularity, and there doesn't seem to be oversensing of the ventricular beat.
somehow the dilated atrium is creating channels or pathways that allow flutter to occur without being sensed in the atrial lead?
i was going to say tremor, but i don't think it is tremor because of the irregularity of the qrs and the lack of conduction to the ventricle from the atrial marker channel
i'm not sure what else to guess?
It looks like the atrial depolarizations are not conducted, like a 2nd-degree AV block. I'd guess the atrial lead isn't "recognizing" the extra depolarizations due to the device's atrial refractory period; meaning the device is expecting a ventricular depol. after the atrial depol. and thus turns off sensing to prevent feedback. So I'd say it's an AV block and the device atrial refractory period should be shortened.
The electrogram and marker channel don't seem to reflect the flutter waves. I don't know what the atrial lead is actually sensing, but something may be wrong with it, maybe a dislodgement or an insulation break. But I can't fully explain the tracings.
The tracing above was obtained by inhibiting the output of the pacemaker to see patient’s underlying rhythm and the right atrial signal present at the local atrial electrogram. At first, it was thought the surface EKG findings were artifact, so multiple leads were evaluated and all showed the same atypical atrial flutter pattern on the surface EKG. The right atrial electrogram however, is clearly dissociated from the left atrial “flutter” seen on the surface EKG. Hence, this finding represents sinus rhythm (with Wenkeback) in the right atrium while a separate left atrial rhythm (an atypical atrial flutter) is simultaneously occurring in the left atrium.
This finding is very rare and likely occurred because of the patient’s very abnormal left atrium which has been subjected to two prior surgeries. These surgeries, coupled with the ongoing fibrosis inherent to severe atrial disease, may have disrupted the normal inter-atrial connection points between the atria like Bachman’s bundle.
No attempt was made to “cardiovert” the left atrial flutter rhythm seen, since the patient was asymptomatic.
Thanks to all who ventured a guess. Admittedly, this one was tough, but it offered an interesting perspective on intra-atrial conduction.
Oops, sorry about the typo - Karel Frederik Wenckebach is rolling over in his grave....
I have seen this a number of times in older patients with previous surgeries or previous ablations in RA. My guess is that if the RA lead was septal, say cs ostium, one might see the flutter waves??
An EKG done during a heart attack may look normal or unchanged from a previous EKG. Do we need to repeat the EKG to look for changes? What do you suggest? Preparing for surgery Aortic replacement and Root Repair next month at Valve Replacement New York.
Post a Comment