The patient was admitted with some vague chest discomfort. The initial EKG and troponins were normal, but they decided to admit the patient anyway for observation. Once on the ward after being given some heparin and aspirin, the patient was feeling perfectly fine - wanted to go home - but the second set of troponins returned positive. The first year resident decided to order a second EKG.
The EKG technician came dutifully, performed the EKG, and before she knew it, all hell broke loose:
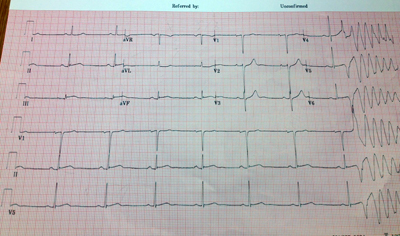 |
| Click image to enlarge |
Fortunately, the patient did well after a quite bit of work in the cath lab.
Remember this story. It might just save a life.
-Wes
8 comments:
Looks like inferior ST elevation then R on T initiating VT. Would cardiac sympathetic denervation prevent this?
I'm not a cardiologist, but did the first year resident use the Bazzett formula to correct the QT interval?
Interpretation:
(1.) Sinus bradycardia (rate about 48-52/min interrupted by a . . .
(2.) . . . ventricular premature beat (VPB; 8th beat), presumably from the left ventricle (LV), which precipitates . . .
(3.) . . . polymorphic ventricular tachycardia (PMVT).
(4.) Early acute inferior infarction.
This is so early in the development of the infarction that I wouldn't be surprised if the ECG machine failed to flag the 12-lead ECG with the statement ** ***ACUTE MI** **. The computer's programmed algorithm criteria probably hasn't been met but it's more obvious to the eye of the human observer. Slight ST elevation in the inferior leads. Extremely subtle ST depression in lead I with measurable reciprocal ST depression in aVL. The VPB lands at about the apex of the T-wave (R-on-T phenomenon) during the vulnerable period of ventricular repolarization. The QRS morphology in lead V1 is wholly positive R-wave with slurring on the downstroke (a so-called taller left "rabbit-ear" equivalent.) This same initiating VPB also displays a typical QS complex in V6. Dr. Marriott always said that statistically, VPBs from the LV are more malignant than VPBs from the RV. The QT interval looks appropriately normal for a rate this slow. This PMVT is not pause-dependent and not in the setting of a disproportionately prolonged QT interval. I would not call this Torsades de Pointes (TdP) but rather just label it PMVT. This would probably quickly degenerate into ventricular fibrillation.
Good work.
I agree with Jason on PMVT vs TdP as at first glance the QTi is < 1/2 the RR, and I calculated the QTc at 400ms (440ms QTi, RR ~1240ms).
Interesting EKG. It would be a challenge for residents and even cardio fellows. What was the management?
DRAgustin-
Privacy laws prevent me from discussing any case specifics on this blog.
Sorry-
-Wes
According to Dr. Marriott's book "ECG/PDQ", the method involving a measured QT interval that is less-than half of the RR interval is only reliable between the rates of 60 to 90/min. Any rate below or above those two parameters is going to produce results that are less reliable. The rate here is only averaging at about 50/min.
Post a Comment