Monday, July 31, 2006
Stun Guns and the Heart
They studied 150 discharges of two different manufacturers' stun guns in 6 anesthetised pigs. Nearly half (74) of these discharges stimulated the pigs' hearts. Stimulation was documented by intracardiac electrodes that were shielded from outside electrical interference. All cardiac stimulations occurred when the barbs from the device were attached to the pigs' thorax - none occurred when the barbs were off the pigs thorax.
The researchers were able to fibrillate (i.e., cause cardiac arrest) one pig when adrenaline (epinephrine) was administered before the application of the "stun."
What was most interesting, was that the rate of stimulation was different for the two models of stun guns tested: The X26 Advanced Taser (with its 6 Watts of power delivering 0.36 Joules of energy per pulse, that delivers a big first pulse of 1.5 microseconds, followed by a longer wave of 50 microseconds causing 195 mV of stimulation) was more likely to cause cardiac stimulation than the M26 Taser (with its 26 Watts of power 1.76 Joules of energy with each pulse, but delievers it in a single short impulse causing 77 mV of stimulation).
Deaths from perpetrators subdued with stun guns are rare: one study they cited reported 3 deaths in 218 subjects (1.4%). Seeing as 5000 law enforcement agencies in North America have these among some 130,000 officers, there are several implications:
1) Police forces should review the model of device they have, and
2) They might want to aim low (guys, beware!), and
2) Further research in humans might be warranted, but use of guns to subdue victims still seems more dangerous than stun guns.
--Wes
Sunday, July 30, 2006
T-shirts Do Good Again
The three teenagers, Tifani Timback (18) of Lombard, Ari Carlson (15) of Oswego, and Laura Rank (19) of Hinsdale, have been making this shirt and contributing their $12 proceeds to the Highland Park(IL)-based National Association of Anorexia Nervosa and Associated Disorders (ANAD). Amazingly, all of ANAD's services are provided free of charge to people with these disorders. Says Dembeck:
I truly believe that everything happens for a reason, and I believe...my eating disorder happened so that I could come through it and help others. Making the shirts makes me feel like I'm being productive and helping a good cause."Here are three lovely ladies, who have worked with the mantra "fake it until you make it" while in treatment at the center, but from the looks of their picture and the kindness of their hearts, they've already made it.
So support their cause. And help other young women believe in themselves.
--Wes
To order an Angel Strength t-shirt, e-mail angel.strength -at- yahoo.com for details.
Friday, July 28, 2006
Drug Lunches
The pharmaceutical industry deals in drugs, and doctors dispense drugs. The pharmaceutical industry wants doctors to use their drugs. So they market. This is America - we do this. Look at Starbucks, Panera offering WiFi, McDonalds giving away Disney Toys, Nike, Apple. They all have products, and they market these products to the average American who often can't afford higher prices for their products. Yet these companies spend zillions of dollars marketing their products. Their shareholders demand it, revenues rely on it. And guess what.... people buy their products. Can you believe? Yep, doctors might actually be influenced by a drug company buying them lunch! And companies might profit!
But in the case of marketing to doctors, well that's not okay, because they're rich! They are single-handedly increasing the cost of health care! Look at those drug lunches! Look at all that fat! See? I told you! And those free pills they get - those are driving up the cost of health care to American's, I tell you! See how unethical and unprofessional they are? I'm sure that's why the cost of healthcare is spinning out of control! It's the doctors having lunch! And free lunch at that!
But I would remind the casual reader that there are few professions that have sustained a negative reimbursement rate for services rendered like the medical profession. The July-August issue of Physicians Practice published a survey of internists, family practice doctors, and pediatricians salaries by Merritt, Hawkins and Associates. The average generalists' salary was $150,000 per year, over half of the doctors were "dissapointed" with their income relative to their work effort, and 28.6% of doctors stated that in retrospect, they would not choose to go into medicine again at all. All this with an aging and growing population that needs these guys more than ever.
Look, what the drug companies feel is useful or not is up to them. It's a great country and this is the American Way. The free market has permitted our health care system to be the best in the world. Certainly, I can elect not to attend drug lunches. My employer can elect to stop permitting drug lunches. But will this self-virtuous act change the cost or quality of healthcare?
I know there are colleagues who are emphatic about this issue: that we, the doctors, should live a puritanican lifestyle and not interface in any way with peddlers of products that might influence our decisions. Especially medical decisions. But we interface with these products every day. Nearly every major medical profession I can think of receives a significant portion of its operating budget from the pharmaceutical or medical device industries. Look at any "Scientific Session" or "professional society" in medicine. Even the AMA peddles our prescribing habits to the drug industry to receive funds.
Certainly physicians should take a lead in reducing the costs of healthcare for our patients. But we should not be disingenuous about our dealings with these companies either. I'd like to think I'm capable of independent thought on the subject of drug marketing. Believe me, as the article suggests, enticements were much more prevalent before 2002 and yet here we are, with a healthcare system that is emulated by many and yet with higher costs than ever before. Was this from doctor's lunches? Will we stop deluding ourselves to thinking that stopping this practice will influence the cost of medications? Newsflash: it won't. The days of the $10 pill are here. And drug lunches didn't start this.
--Wes
Watching the Wheel
I made up my mind back in Chelsea,
When I go, I'm going like Elsie.
Start by admitting
From cradle to tomb
Isn't that long a stay.
Life is a Cabaret, old chum,
Only a Cabaret, old chum,
And I love a Cabaret!"
- From the musical, Cabaret
It's been a tough week.
Three men - all friends, all men, all struggling to live.
One: arthritis, pain, daily struggle to walk, difficult to get out, schizoid, introverted, afraid, waiting.
Two: neck lump, squamous cell carcinoma, resected, margins clear except at base of skull. On to radiation.
Three: gregarious, outgoing, regal, arm weakness, calls 911, hospital in 30 min, thrombolytic, intracranial bleed, on ventillator.
Why, after all the countless human tragedies, working with people daily that have survived sudden death, does there come a time when I reflect on the human condition? I suppose the blind eye I turned on my cadaver during its dissection the first day of medical school, the compartmentalization of signs, symptoms, and pathologies that we learn so carefully in medical school, the intellectualization of medicine, has helped me cope.
But when we've played the game, step back and look at the big picture, the way people live and die, we see the futility of the rat-race, the striving to get ahead, to be wiser, richer both intellectually and financially. It is the very nature of the human condition that we must stop and really realize the limits of life and consider how we want to live. That every day is a gift to be cherished. That no matter what happens in the end, it's all about friends and family. And our faith that helps us understand that there's a meaning to it all.
"I'm just sittin' here watching the wheel go round and round.
I really love to watch it roll.
No longer riding on the merri-go-round
I just had to let it go."
- John Lennon
--Wes
Wednesday, July 26, 2006
Microsoft Forays Into Health Care Software
--Wes
Cardiothoracic Surgery - Dying?
--Wes
Tuesday, July 25, 2006
Defibrillators in Athletes
The debate over whether athletes with heart conditions should be allowed to play raises issues of free will, medical ethics and legal liability. Is the love of sports -- and the dream of a professional career -- worth risking death? Should doctors be in the position of prohibiting adults from playing? What's the difference between competing with a heart defect and pursuing risky adventures like climbing Mount Everest? Should fans be forced to watch a player risk his life?
And there are probably not two more opposing views than those shared by Dr. David Cannom from Los Angeles and Dr. Barry Maron from the Hyopertrophic Cardiomyopathy Center at the Minneapolis Heart Institute Foundation. On one side, Dr. Cannom is careful to evaluate certain players and work in tandem with the players to structure a possible mechanism for them to continue playing competitive sports. On the other more conventional side, Dr. Maron argues that sudden death strikes 200 to 300 young athletes annually, and these might be prevented by restricting play. Dr. Maron is keenly aware of the changes in hemodynamic loads to the left ventricle during athletics in patients with hypertrophic cardiomyopathy. In fact, one recent study demonstrated the poor efficacy of external defibrillators (AED's) in saving athletes' lives. One wonders if internal defibrillators (like those recommended by Dr. Cannom) would be equally ineffective. But as acknowledged in the WSJ:
There's little solid medical evidence to guide doctors in assessing this risk. Studies show that barely one out of 100,000 athletes suffers sudden cardiac death. Yet as many as one in 500 people suffer from HCM. That suggests that dozens of athletes would need to be sidelined to save a single life. The risk of playing sports with a heart defect and a defibrillator has barely been studied. The number of people with defibrillators who want to play competitively is small. Dr. Cannom is now pursuing a study with a Yale University cardiologist.There does seem to be consensus that contact sports, like football, are ill-advised, since the defibrillator could be easily damaged. But I feel the same is true for basketball. It can get pretty physical, and jumping up and down certainly puts significant stressors on the lead inside the heart. If leads can be fractured from weight lifting and jogging - why not basketball?
The difficult choice between passion and protection makes some cardiologists yearn for a middle ground. Michael Ackerman, a Mayo Clinic cardiologist who has worked with Drs. Maron and Cannom, says, "I wish we could have a detailed discussion with the families instead of the default -- you have a defibrillator, you're kicked off the team."
Further, defibrillators are complicated devices that work on a simple principle - heart rates that are too fast are abnormal. It seems that Dr. Cannom programs his athletes' defibrillators to a detect rate of 250 b/min in some cases. That means that only rates over 250 beats per minute will be shocked. This rate might make sense in athletes, but could also sacrifice sensitivity of detection for specificity - that is, abnormal rhythms of, say, 240 beats per minute would go undetected. So when we read about the following about Mr. Will Kimble of Peperdine University's evaluation after practice:
As he has done dozens of times, Mr. Kimble slid a round wand over his T-shirt and the defibrillator implanted in his left shoulder. A minute later, a Medtronic representative printed out a beat-by-beat report on Mr. Kimble's device and his post-game heart. There were no irregularities.This might not be true - it just means the programmed settings of his defibrillator device didn't see any heart rates that exceeded 250 beats per minute.
Further, why would the University of Texas, El Paso decide that a Medtronic rep and trainer be adequate coverage for a game, rather than a physician?
Mr. Kimble played two seasons at the University of Texas El Paso without needing a shock from the defibrillator. "I love being out there," he says. "I wouldn't have done it if I had a doubt in my mind." But basketball team trainer Michael Gutierrez says he was nervous during each practice, and each time Mr. Kimble fell.
After playing 18 minutes in his second-to-last collegiate game in March, Mr. Kimble sat with the team trainer and a sales representative for Medtronic Inc., the maker of his defibrillator. The school required a company representative to be at every game, to test the device.
Hmmm. Great service, Medtronic. But how much liability is Medtronic willing to assume? (I've always noted that it's never good to have your company in Column 1 of the front page of the Wall Street Journal.)
Well, enough for now. Best of luck to you Mr. Kimble, but please realize the limitations of what the Medtronic reps are reporting to you after your practices.
--Wes
Monday, July 24, 2006
Nazi Virtuosity
"I get all my health care from Borders (bookstore)," she said. "I mean, conventional medicine offers so little to people. Why go to a doctor? If people just ate the right foods, lived the right lifestyle... I mean, they bring so much of their illness upon themselves, living their lives in such stressful, toxic ways!"
My wife choked back her tofu. A pulmonologist seated at the table smiled politely, and calmly made a quip about the importance of seeing a doctor. She heard nothing of it. So my wife opened with both barrels...
"You haven't been sick, have you?," my wife asked. "No. Of course not!" said the woman. "And what will happen when you are diagnosed with cancer some day?" my wife asked.
Boy, did the room get quiet.
Nazi virtuosity. That's what this woman demonstrated. Such a proclamation reveals this woman's solipsistic perspective to issues faced daily by people with chronic illnesses. Is a child with Type I diabetes the victim of poor lifestyle or a genetic short-straw? What about the person with breast cancer, cystic fibrosis or a million other diseases? To think that we can control what life throws at us by always eating the right foods, exercising incessantly, living a calm existence without clutter or noise, is ignorant to the issues faced by anyone with a chronic ailment. Worst of all, comments like these are opprobrious epithets and serve no useful purpose when illness is involved.
Certainly, a proper lifestyle that limits alcohol and smoking, moderates dietary intake, and practices regular exercise has merit. These things might prevent or slow a disease. But we all will be afflicted with our own unique ailment - and I have yet to read about a clean-living individual who did not age and die - including the lamas, gurus and shamans. Sorry, friend. And after all the books I've read, there are no two patients that are the same, and I've yet to read about anyone's specific problem list and physical findings in a book at Borders.
--Wes
Sunday, July 23, 2006
Gleevec Weakens Hearts
For a great description of dealing with CML from the patient's perspective, there's a long-standing "Cancer Diary" by Erin Zammett Ruddy, an editor at Glamour Magazine. She, too, is taking Gleevec.
--Wes
The Poop
--Wes
Source: Rand Simberg via Instapundit
My Best Friend

As the oscillatory frequency of her tail-wag accelerates, I am reminded of the incredible value a pet can have to those who are homebound or alone. Their companionship brings a smile and a momentary interlude to the monotony of chronic illness. They force us to get up, to get out, and to greet each new day anew. All while asking very litle in return.
--Wes
Saturday, July 22, 2006
FDA Overreaches
Off-label use of medications occurs all the time. Even aspirin, used for years as a mainstay therapy for myocardial infarction (heart attack) because of its anti-platelet effects, was never approved by the FDA for this use. And yet over the years aspirin administration in the setting of myocardial infarction has become a "best practice guideline" therapy.
"F.D.A. rules allow doctors to prescribe federally approved drugs for any purpose, even if it is not indicated on the medicine’s label. ... And at least one former F.D.A. official says that the government appears to be overreaching in going after Dr. Gleason and may chill a common and legitimate form of medical discussion. “This is a very, very scary development,” said Daniel E. Troy, a partner at Sidley Austin and the former chief counsel of the F.D.A."This issue goes beyond drugs as well. Perhaps one of the most obvious recent examples of this was in the early-development years of catheter ablation (burning electrical short circuits in the heart using a wire threaded there through a vein). With the development of radiofrequency energy to perform catheter ablation, it was clear to doctors that therapy using steerable ablation catheters (wires) posed less risk to their patients than subjecting them to open heart surgery for the same treatment. Thousands of patients underwent catheter ablation procedures without FDA approval of the steerable ablation catheters used in the procedure. Doctors discussed the risks and benefits of these catheters for years in a public forum known as the North American Society of Pacing and Electrophysiology (NASPE). Finally, the FDA realized they could not move as quickly as medical developments and issued their "Catheter Ablation Catheters Generic Arrhythmia Indications for Use; Guidance for Industry" document on 1 July 2002, written with the guidance of doctors who had used off-label catheters for years.
While illegal use of controlled substances should be diligently prosecuted, doctors must have the right of free speech that is unencumbered by intrusive government intervention. To do otherwise will stifle creative innovation and important public discourse in medicine.
--Wes
Friday, July 21, 2006
The Shift from Cure to Care
Yesterday the New York Times let us see the face of Dr. Anna M. Pou who is accused of using lethal injections to kill several patients who were in extreme distress after Hurricane Katrina. She's a real person, who made some real, difficult, and human decisions. The circumstances are unclear but the situation was clearly difficult. Were her actions sinister or benevolent? And while the courts will be asked to decide this case, realize that these tough life-and-death decisions occur every day in our hospitals.
An example: recently doctors were asked to place a pacemaker in a 99-year old man who had just suffered a large heart attack several days earlier and was not felt to be a candidate for open heart surgery due to his other medical conditions (he was "too old"). His heart rate limited the number of heart medications he could take for his pain. He had some blood in his stool when previously anticoagulated, so angioplasty was not an option. In the interest of supporting his heart rate safely while receiving more heart-related medications, a pacemaker was recommended.
But was he also "too old" for a pacemaker? Is there an upper limit to the age a patient should receive such a device? How much money should be spent in end-of-life healthcare? With the ever-rising cost of healthcare today, is there a place for such a discussion? What assurance is there that the pacemaker will be effective or that the patient will not suffer a complication of the implant procedure? What are the implications for withholding pacemaker therapy? Would pain medications like morphine, with its known analgesic effects, be more immediately therapeutic for the patient? Or would morphine's use expose these doctors to litigation, like Dr. Pou?
Decisions like these are never easy. Sometimes, our toughest decisions in medicine occur when we stop trying to cure our patients and instead decide to continue caring for them.
And we must not lose sight that we are involved in healthcare, not healthcure.
--Wes
Making Lemonade Out of Lemons
Happiness = Morton's Steak House (during 4-hour delay) + 2 beers + Wireless Internet Connections in the Airport
Frustration + Happiness = Life
It all balances out.....
--Wes
Thursday, July 20, 2006
NEJM: Prevalence Data on Diastolic Heart Failure Flawed
Diastolic heart failure occurs in people with a normally contracting heart muscle that has difficulty relaxing to fill with blood. Because it cannot fill with blood, the amount of blood ejected with each heartbeat is compromised. Diastolic heart failure is different from the more commonly understood "systolic" heart failure caused by a weakened heart muscle).In today's New England Journal of Medicine, an interesting article entitled "Trends in Prevelence and Outcomes of Heart Failure With Preserved Ejection Fraction" by Owan, et al. describes what they perceive as an increasing prevalence of "heart failure in patients with preserved ejection fraction" (also known as "diastolic heart failure") in Olmstead County, Minnesota between 1987 and 2001. Wonderful graphs are depicted showing a rising prevalence of this problem.
But how was the diagnosis of heart failure made for this study? Not by physical exam or chart review, but rather by searching the Medicare database for "DRG 127" - the "Diagnosis Related Group" code for congestive heart failure, or ICD-9 code 428 (Congestive heart failure).
This study is another failed attempt to make meaningful population prevelance data from these Medicare codes, and amazingly, neither the authors nor editors considered the healthcare and reimbursement climate in which those codes were generated. They forgot the most SERIOUS source of bias in their study: money.
Bruce Psaty, MD, PhD et al in a commentary from the 1 Jul 1999 issue of the Am J of Cardiology, entitled "The Potential Costs of Upcoding for Heart Failure in the United States" stated:
"Although the incidence of validated episodes of heart failure did not differ significantly between 1981 and 1991 in Olmsted County, Minnesota, the number of initial hospitalizations coded for heart failure among persons ≥65 years of age in the United States (US) increased from 631,306 in 1986 to 803,506 in 1993. Potential explanations include the aging population, the improved survival after myocardial infarction, and the burden of risk factors (e.g., hypertension and diabetes)."But they also offer another rationale which I think is compelling:
"The US Health Care Financing Administration reimburses hospitals for Medicare patients on the basis of diagnosis-related groups (DRGs). Hospitalizations for heart failure (DRG = 127) received a reimbursement estimated to be $7,057.98 in 1997. For other primary diagnoses, the presence of a complication increased the level of reimbursement, and heart failure qualified as a complication. The additional discharge diagnosis of heart failure for a Medicare patient in 1997 increased the reimbursement for an acute myocardial infarction by $3,345.06, for pneumonia by $2,872.70, and for a gastrointestinal hemorrhage by $3,071.40. For these 3 common conditions, a secondary diagnosis of heart failure increased the reimbursement to hospitals by an average of $3,096.39."While this certainly does not diminish the importance of physicians appreciating that heart failure can occur in people with normal ejection fractions, I am skeptical that the prevalence of this disorder increases over time as the study suggests. To reinforce this finding, Psaty and colleagues noted:
"Among 485 subjects with a primary or secondary Medicare discharge diagnosis of heart failure, we were able to validate only 303 (positive predictive value 62.5%). For the other 182 patients, we were not able to find even modest levels of supporting evidence for the diagnosis of heart failure. The proportion of false-positive diagnoses was 37.5% (95% confidence interval [CI] 33.2% to 41.8%). In contrast, the proportion of false-negative diagnoses was low (10.1% of 832). The false-positive rate seen in the CHS is consistent with the findings of other studies, and it is much higher than the false-positive rate for diagnoses such as myocardial infarction, which tend to be ≤15%.I think we have to rethink this paper with this incentive in mind.
"Using the false-positive rate from the CHS, we estimate that in 1993, 301,315 of the 803,506 hospitalizations for heart failure may reflect incorrect diagnoses (95% CI 266,764 to 335,866). If the average excess cost of an upcoded diagnosis is $3,096.39, then US hospitals may have received excess reimbursements from Medicare of as much as $933 million a year (95% CI, $826 to $1,040 million). The high proportion of false-positive compared with false-negative diagnoses favors reimbursement to hospitals. If the CHS sample is representative, the estimated costs of upcoding, even after adjustment for the revenues lost by the false-negative diagnoses, would be still be high—about $502 million."
"A wise man should have money in his head, but not in his heart."
Jonathan Swift
Irish essayist, novelist, & satirist (1667 - 1745)
--Wes
Quote reference link.
Wednesday, July 19, 2006
Are You Who You Say You Are?
And therein lays the perplexing problem for today’s health care industry. Are you really who you say you are? Can we really assure that those test results REALLY belong to you? Are YOU really the one who needs their right lower extremity amputated, as the pathology report (tied to your identity), suggests? Check and recheck. Take a “time-out” before every operation. Read back the serial numbers on every bag of blood. Screw this up and the patient buys it! Screw this up and we won’t get paid! Please re-check! Then check again.
So it should come as no surprise that we read this report of Hackensack Medical Center, in collaboration with Horizon Blue Cross and Blue Shield, placing RFID tags made by VeriChip Corporation in 280 patient “volunteers” so the ER can pull up their records “as if they couldn’t communicate.” And why, pray tell, are we doing this? To avoid medical errors, so they say. To get paid faster, I say. And probably for bragging rights as winner of the 100-most Wired Hospitals ranking.
Things are moving so fast with this technology. Not only will you be able to be tracked using a simple numeric identifier, but new implanted tags capable of storing lots more information became a reality this week: like your history and physical, drug lists, blood type, relatives, smoking history, address, employer, and your credit card information. It’ll be billed as “convenience,” “safety,” “security.” But it’s going to happen. Slowly at first with your pets. Then with “early adopters” and “geeks.” Then your confused mother. Then you.
After all, safety matters. Just check.
--Wes
Via: starttherevolution.org
Tuesday, July 18, 2006
Exercise: Pain is Beautiful
And my wife knows it. She's watched the forces of gravity over the years tug and pull on every adipose cell on my body, kindly remarking, like the saying on the cereal boxes, that "some settling of contents has occurred during shipment and handling." Thanks, dear.
But at her insistence, I started something recently that I feel a bit guilty about. You see my wife is much more intelligent than me. It occurred despite my many objections about the time commitment (after all, I'm a doctor!), insecurity (can I do this?) and a feeling that I'd be over- self-indulgent.
I started exercising with a personal trainer. Okay, there, I said it. I know, not everyone can afford a personal trainer, but I have discovered a few things on this venture:
I still hate getting up and going in to exercise at 6 AM.
I always feel better afterward that I did get up and go in at 6AM.
I sweat a bunch.
It takes a long time to start to feel stronger.
Exercising 10 minutes burns about 140-200 calories, depending on my workload on an elliptical.
My back doesn't hurt as much.
It's not as hard as I thought.
I still hate getting up at 6 AM.
No matter how I conquer an exercise, that guy ALWAYS adds a new twist, and more weight.
My own body mass serves as enough weight for 97% of all the exercises I do.
I should never eat before I exercise.
It's tough to blog before you exercise, especially if you have to get there by 6AM.
Once many years ago, I took care of a Marine Gunney Sergeant who was having a LARGE posterolateral myocardial infarction (heart attack) in the Coronary Care Unit. Sweat dripped off his brow. His face grimmaced with in pain. And when I asked him how he felt, he barked in true drill-sergeant fashion:
"Pain is beautiful, Sir! ... "Extreme pain is extremely beautiful, Sir! ... "And agony is ecstacy, Sir!"
Those words spoke volumes about this incredible patient. He was remarkably strong in character, even in a time of great adversity. He hung in there as we mixed our thrombolytic (a clot-buster: we didn't have stents back then), and slowly infused the nectar until we saw his face brighten and the reperfusion arrhythmias occur, indicating effect. He later got his angioplasty and returned several days later to his delightful wife and four kids.
The Sergeant had a 'Charles Atlas' physique, exercised every day, didn't smoke, yet still had a heart attack. (Genetics aren't fair, I guess). I could have used his situation and misfortune as an excuse not to exercise now, but that Gunney Sergeant taught me a lot that day about attitude and its benefits in tough situations. Thanks, Gunney.
So, like him, I have hung in there. Reluctantly. But I think this exercise thing is starting to pay off. I feel stronger, can do more reps, and don't huff and puff as much. Maybe I can avoid his fate. Agony is ecstacy, indeed.
But I still hate getting to the gym by 6AM.
--Wes
Monday, July 17, 2006
RFID Tags on Surgical Sponges
Here's an idea: how about looking in the wound or doing sponge counts before you close?
--Wes
Hospital Administrators Must Control Costs Too
Mr. Andy Stern, President of the Service Employees International Union commented inthe WSJ today about the death of employer-based healthcare:
"CEOs know this best: They dread the meeting with HR managers who tell them, once again, that their health-care costs are through the roof. So they look for any way to control costs. Co-pays go up, subsidies go down, coverage is dropped all together. In the last five years alone, the percentage of businesses offering health benefits has plummeted to 60% from 69%. Here's how bad it will continue to get: McKinsey & Company projects that by 2008, the average Fortune 500 company will spend as much on health care as they make in profit. How can we possibly compete in the global economy with that kind of burden?CEOs know this best: They dread the meeting with HR managers who tell them, once again, that their health-care costs are through the roof. So they look for any way to control costs. Co-pays go up, subsidies go down, coverage is dropped all together. In the last five years alone, the percentage of businesses offering health benefits has plummeted to 60% from 69%. Here's how bad it will continue to get: McKinsey & Company projects that by 2008, the average Fortune 500 company will spend as much on health care as they make in profit. How can we possibly compete in the global economy with that kind of burden?"
If CEO's and hospital administration help (and they'll have to), then perhaps a fix to the health care crisis will have a chance of succeeding. To do nothing is NOT an option. As Mr. Stern says:
"To fix health care in America, we have to accept that we're living through the most profound transformative economic revolution in the history of the world. It's happening so fast we can barely keep track of it. Intense global competition. Contingent work. The explosive economies of China and India. Technology in the workplace. Outsourcing. By the time they are 35, young people entering the job market today will already have worked in eight to 12 jobs. Employers will be pit stops for them, not permanent homes. In other words, we are rapidly moving from employer-managed work lives to self-managed work lives, in which workers must figure out on their own how to maintain things like health insurance and retirement."And you can bet we won't tolerate wasted funds on plush trips to Colorado.
--Wes
Sunday, July 16, 2006
ED, The Heart, and Romance
This report, originally reported from the WSJ, suggests Viagra, Levitra, or Cialis can be helpful for screening for heart disease:
While erectile dysfunction has long been treated as a lifestyle issue, erection problems appear to be a very early warning sign of looming heart troubles. An Italian study showed that in two-thirds of patients who had known coronary-artery disease as well as erectile dysfunction, the erection problems showed up, on average, three years before other symptoms, such as the chest pain caused by angina.In addition:
The Archives of Internal Medicine (2006) reported on a study of nearly 4,000 Canadian men between the ages of 40 and 88 who were seen by primary-care doctors. The researchers found that men with erectile dysfunction were nearly 50% more likely to be diagnosed with diabetes or metabolic syndrome -- a collection of health risks that are associated with heart disease.
In med school we were taught this pneumonic for the causes of impotence (er, "ED"):
P - Psychologic
E - Endocrine
N - Neurologic
I - Ischemic (lack of oxygen due to vascular disease)
S - Substances (like alcohol, etc.)
So if your "little blue pill" doesn't work, realize that in half the cases it was because the drug was administered incorrectly, but you should also consider each of these other potential causes and review them with your doctor.
But is there a place for such a pill for women? Could we screen women in a similar fashion? Or perhaps, as in this story from close friends, might we shed light on another way ED drugs can screen for heart disease?
Recently we had a dinner party for several couples, one of whom had recently celebrated their 25th wedding anniversary with a weekend getaway at a famous romantic hotel here in the Chicago metro area called Sybaris. It was a surprise for the husband - his wife had arranged the weekend getaway secretly and anticipated the evening for weeks. She hinted to her husband that they would have plently of time to spend together and to come prepared for "fun and frolicking." Now as a typical guy, he suspected they were heading to some sleezey hotel for the weekend, and made sure he had a few Viagra thrown in his toiletry kit, "just in case."
Now imagine his surprise when they arrived - viewing the in-suite pool with waterfall and all the romantic accommodations - it made the Poconos seem like Holiday Inn and he was at the Ritz Carlton of romance! So they put away their bags, decided to take a swim (in the buff, of course) and relax. In anticipation of things to come, he took one of his Viagra tablets, grabbed the provided white robe, and snuck back to bed. Meanwhile, his wife suggested they get a romantic movie to enhance the evening - she sensed his anticipation, but wouldn't you know it - she had a rip-roaring headache. Honest to God! Why now?
Well Sybaris wisely has no phones in the rooms and no way to do a "pay-per-view" movie - you have to go back to the front desk and check out a video for your viewing pleasure. To say the walk back to the front desk was difficult for the husband some thirty minutes after taking the Viagra was an understatement! But he hobbled and perservered - after all, his love had requested a particularly racy title, and the embarassment was worth the risk....
Meanwhile, back in the room, his wife was rifling through her things, desperately trying to find an aspirin, ibuprofen (like Motrin or Advil) or Tylenol - to no avail. So, she decided to check her husband's toiletry kit, and voila, there were these little blue pills - she figured they must be Advil! So she took one and climbed into bed awaiting her husband's return.
Her husband returned from the front desk victorious and elated that he was not "noticed." He placed the video in the player and crept back in bed. His wife informed him of her headache, but knowing her from their many years together, he knew better than to ignore her complaint. So they settled in for the movie.
Then an amazing thing happened. As he laid there, his wife had a remarkable resolution of her headache and an unsatiable desire to make love to her husband. He was awestruck. It went on and on, he had never seen her like this before. What happened? Oh my God! Hallelujah! Whoa there little doggie! Their exertion would have burned up any stress test machine! On and on it went...
Finally, as they collapsed in exhaustion, he asked her what the hell happened? She explained that she'd found some Advil in his toiletry kit and her headache had resolved.
He told her that there was no Advil in there, just Viagra. She looked at him - "Really?" she said. And they laughed and laughed and each felt better that their stress test was negative.
--Wes
Saturday, July 15, 2006
Sidewalk SUVs
And for many who are fifty (or more) pounds overweight, it probably is. So today's article in the Wall Street Journal , which describes the boom in sales of disability scooters for the mere convenience of strolling about Minnesota's giant Mall of America, various mega-stores like Walmart, or large public venues, like Washington DC's national mall, should be a wake-up call to all of us. That's right - these scooters aren't being used just by the disabled, but also by the healthy, some of whom are opportunists who would rather buy cheap tickets in Las Vegas and be "put right in the mezzanine with the handicapped people" or "ride all day and dance all night."
But this all comes at a cost to our health and society. Much the same as the tradeoffs we make in our national passion for gas guzzling SUVs. Pride Mobility Products, one of the largest disability scooter manufacturers, began supersizing its Jazzy, Maxima and Celebrity-X models to meet the growing girth of Americans - and certainly for our obese disabled patients, this makes sense. But the increased numbers of these scooters being used because people are "just lazy," has the potential to malign the truly disabled.
"It's kind of bad for the cause," says Janna Starr, director of disability rights and technology for United Cerebral Palsy, a non-profit group. She says it also puts companies in the problematic position of judging who "deserves" aid and encourages them to assess disabilities - which can be hidden - based on appearances.But it goes beyond this. It reinforces the lack of importance we place in our personal health, and provides an egregious display of our selfishness toward others when we use these to forward our own agendas simply because we're too lazy to move or too cheap to buy a full-priced ticket in Las Vegas.
--Wes
Friday, July 14, 2006
A Bit of Brits and Booze
But that hasn't stopped the British Beer and Pub Association:
Sceptics will argue that although beer has fewer calories than wine, it comes in pints while wine is served in smaller measures.What bar is that one? After all, there are some data that a bit of wine can be good for your heart:
However, Mr (George) Phillistick (of the the British Beer and Pub Association) says the gap is narrowing - the typical wine serving has crept up from 125ml to 175ml. Many bars now serve a large 250ml glass as a matter of course, which is equivalent to a third of a bottle.
There is compelling epidemiological evidence suggesting that regular light-to-moderate alcohol intake is associated with reduced atheromatous morbidity and mortality. It is interesting to note that while atherogenesis takes many decades, the beneficial effects of alcohol accrue only in later life. The reasons for this are uncertain but the effects may be a combination of plaque stabilisation (sic), analogous to the effects of some cholesterol lowering drugs which affect coronary endpoints relatively quickly, and an antithrombotic effect.So talk to your doctor. And have a nice, er, sober weekend -
--Wes
Complication Rates Complicated
Recently, an article was published in the Journal of the American College of Cardiology (the abstract here) that was picked up by the press with headlines that 1 in 10 defibrillator implants resulted in a complication. To the casual reader, this seems like an incredibly high rate.
But careful reading of their research demonstrated that this was determined in some circumstances by analysis of a Medicare ICD9 code, 996.04, that means "Mechanical Complication of an Implantable Cardiac Defibrillator (ICD)." But realize there is no code for "dead or dying battery" in the less-than-robust Medicare coding scheme, and doctors will not get paid unless the proper code accompanies the procedure code (called a CPT code). When batteries die, the closest code we have to assure reimbursement that does not result in Medicare billing fraud, is ICD9 996.04, and yet is NOT a complication, but proper care.
The media and journals continue to get caught up in "trends" - the latest of which seems to be the horrible health care delivered in America. While there certainly is room for improvement, this complication rate study is yet another example of caveat emptor.
So rest assured, this estimate is high, REALLY high, and it can be explained by the imperfections of the Medicare coding scheme with which we doctors have to live.
--Wes
Thursday, July 13, 2006
EKG for Newborns Might Prevent SIDS
LQTS affects the heart's rhythm and occurs in about 1 in every 2,500 births. Children and young adults with the disorder are susceptible to an abnormally fast heart rhythm which, if it is not corrected, can cause sudden death.To me this seems like a no-brainer: cheap, easy to obtain, non-invasive. The only problem is, that most adult docs won't have a clue, since kid's ECG's look very different from adults' ECGs. So there will have to be some training involved, but it could become part of every OB/GYNE and pediatric resident's curriculum.
It rarely produces symptoms and can be triggered by loud noises, major emotions and overexertion. In some cases deaths in babies with the illness are wrongly attributed to sudden infant death syndrome (SIDS) or cot death, according to the researchers.
"We could prevent about 10-15 percent of cot deaths, plus a number of deaths that will occur later in life," Schwartz said. "It is a genetic disorder. Either you have it or you don't. If you have it, it will be visible at the end of the first month of life."
--Wes
Sound Idea: Optimizing Function of Heart Failure Devices
We had an interesting demonstration of a new application of an old technology today in our device clinic. A small company called Audicor, based out of Oregon and created by a spin-off of Hewlett- Packard engineers in 1999, began work on applying the old technology of phonocardiography (study of heart sounds - those low-pitched "lub-dub" sounds your heart makes when the valves in the heart close) to see if this might help optimize left ventricular (the left ventricle is the main pumping chamber of the heart) filling and ejection in patients with biventricular cardiac resynchronization devices used today to treat congestive heart failure.
I previously used echocardiography to perform this function, but it requires a capable technician, special lab time, access to an echo machine, etc. - in other words, it's more complicated to perform optimization using echocargiography. So we decided to check out this technology.
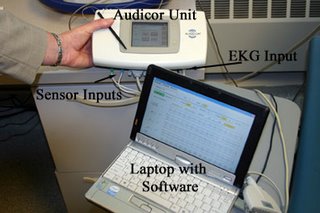
It uses two small electronic microphones with a gooey adhesive to block out peripheral noise that are placed over the standard lead locations of V3 and (about) V4 or V5. These sensors are shown:

These sensors cost about $30 a set, are single use, but enough adhesive is applied so they can be moved about the chest to find the best sounds on a particular patient's chest. The connection setup looks like this:

These leads and sensors are then connected to the Audicor device that signal-averages the heart sounds and is driven by software from a laptop computer that can display (and store) the data from the Audicor device. Here's what that looks like:
The patients (but not the staff) needed to remain completely quiet during the acquisition of the sounds (yes snoring would screw up the data collection!). We tested this device on 8 patients today - 7 of whom had biventricular pacing devices, and one had a DDDR pacemaker, but had complained that he felt worse when his AV delay was shortened to a normal 'range' (180 msec) rather than left to conduct intrinsically with a 330 msec PR interval. A few caveats:
Advantages: Took about 15 minutes per patient, could be performed by a single operator, seemed to generate reproducible data (roughtly within 2-4% error per reading), and was relatively easy to use. It seemed to be surprizingly robust at determining maximium left ventricular systolic ejection time.
Limitations: Large breasts and hairy chests made recording of sounds difficult. Hair should probably be shaved, we found. Ventricular bigeminy made the use of the device impossible (it rejected readings appropriately) . Although they claim V-V timing (techical speak for doctors who understand this stuff) can be optimized in patients with atrial fibrillation, but I did not see this today. Most important, there are no patient outcome data available yet (that is, do patients really feel better if they have this done??), but I was surprised at the findings today and am encouraged to continue studying this. This might help us better understand the 30-percent "non-responders" who received biventricular devices - maybe we just haven't been programming the devices properly in some of those cases. And what happens to "optimization" as the heart function improves after long-term biventricular pacing?
Somehow, the simplicity and reproducibility of this device "sounds" like a good idea. We'll see...
--Wes
Wednesday, July 12, 2006
Should Doctors Have Privacy Rights?
Although I blog, I do not pretend to be a journalist. I hope the journalists from the Times do not pretend to be physicians.
--Wes
Government vs Family
--Wes
Municipalities Without AEDs at Risk of Litigation
The question now is, what defines a "public facility?" One's worksplace? The baseball field? Municipal buildings? It looks like the courts will have to decide each case based on its merit. But "Dwight," a sudden death survivor from California that tipped me to this story states:"West Palm Beach, Florida, attorney, Craig Goldenfarb, is on the Board of American Heart Association “AED Task Force” and...is also recognized by the local American Heart Association chapter as the area's legal expert on Florida law as it applies to the use of these life-saving devices.
If you or a loved one believes a life may have been saved if a public facility such as a gym, a theme park, a sporting venue, or an airport would have had an AED, please contact our office to discuss the merits of your possible case."
"I attended a Christmas party last December at the company where I had my Sudden Cardiac Arrest. Due to my cardiac arrest, the owner of the company hired a training company to come in to teach and certify all employees on CPR. I thought it was great and I thanked the owner for doing that! I then asked when the employees would be receiving the AED portion of the training and was told that he had elected to NOT spend the money for that part of the training. I also asked if they had installed any AEDs in the building and was told that they could not justify spending $2,000 on an AED. It is way too much money, he said. I looked around at the party. There were large trays of freshly barbecued rib eye steaks for all the employees. They were passing out grocery store checks to all employees. They had numerous bottles of very expensive Cabernet everywhere, while others were drinking premium tequila, cognac & scotch. I estimated that the cost of that party would have paid for several AEDs PLUS AED training for all employees. As I always say, it's not the cost of AEDs that is so high, it a matter of how spending is prioritized!"
Point well taken, Dwight. I recently had a company who purchased an AED because they knew they had an employee at high risk of sudden death - and it saved his life. They then bought an AED for each floor of their building. They became believers.
But not all doctors believe in wide distribution of AED devices, based on the cost versus probability of an event occurring. From the Journal of General Internal Medicine, 2003 study:
OBJECTIVE:The American Heart Association (AHA) recommends an automated external defibrillator (AED) be considered for a specific location if there is at least a 20% annual probability the device will be used. We sought to evaluate the cost-effectiveness of the AHA recommendation and of AED deployment in selected public locations with known cardiac arrest rates.
DESIGN:Markov Decision Model employing a societal perspective.
SETTING:Selected public locations in the United States.
PATIENTS:A simulated cohort of the American public.
INTERVENTION:Strategy 1: individuals experiencing cardiac arrest were treated by emergency medical services equipped with AEDs (EMS-D). Strategy 2: individuals were treated with AEDs deployed as part of a public access defibrillation program. Strategies differed only in the initial availability of an AED and its impact on cardiac arrest survival.
RESULTS:Under the base-case assumption that a deployed AED will be used on 1 cardiac arrest every 5 years (20% annual probability of AED use), the cost per quality-adjusted life year (QALY) gained is $30,000 for AED deployment compared with EMS-D care. AED deployment costs less than $50,000 per QALY gained provided that the annual probability of AED use is 12% or greater. Monte Carlo simulation conducted while holding the annual probability of AED use at 20% demonstrated that 87% of the trials had a cost-effectiveness ratio of less than $50,000 per QALY.
CONCLUSIONS:AED deployment is likely to be cost-effective across a range of public locations. The current AHA guidelines are overly restrictive. Limited expansion of these programs can be justified on clinical and economic grounds.
But an added dimension is upon us: can such a refusal to purchase an AED in the era of corporate largess be defended? Corporate America and municipalities might heed Dwight's warning and realize that there's hungry lawyers out there everywhere.
And such a purchase might just save a life. Believe me, that's one heck of a quality-adjusted life year (QALY) for that person.
--Wes
Tuesday, July 11, 2006
More Conflicts of Interest in Major Depression Study
"In total, the authors failed to disclose more than 60 different financial relationships with drug comapanies."Like Apollo 13: "Houston, we have a problem...."
--Wes
Problems With Broad Coronary Calcium Screening?
It is a pleasure to forward this editorial note on the SHAPE Task Force report. The contributors to the SHAPE initiative must be congratulated for their original, ambitious, and provocative approach to the number one problem in the cardiovascular field, affecting millions of lives annually.Provocative, indeed. A very polite critique was offered on this screening approach by Daniel DeNoon of WebMD with inciteful commentary by Eric J. Topol, MD. It is important to realize that calcium scoring has been controversial in cardiology because it uses forms of CT scanning that expose patients to high doses of radiation (average 82 mrem for men and a whopping 150 mrem for women - for comparison a 2-view chest x-ray is about 10 mrem and a 2 view mamogram is about 35 mrem), and have been marketed directly to the patient-consumer without federal support (i.e., Medicare reimbursement) for its clinical utility, and hence has been viewed by many as a technology to line certain imaging physicians' pockets. Could a financial incentive be happening with the latest initiative?
First of all, the Association of the Eradication of Heart Attacks (AEHA.org) was founded by Morteza Naghavi, MD, of the Texas Heart Institute (and carries its official address as 2472 Bolsover Dr, Suite 439, Houston, TX) which also happens to be nearly the same address as Endothelix, Inc. - with its official address of 2472 Bolsover Dr, Suite 439C, Houston, TX - which Mr. Naghavi also founded and owns shares in as well. Endothelix specializes in Digital Thermal Monitoring technology for the early diagnosis of "vulnerable plaque" in coronary disease. Interestingly, Dr. Naghavi's "Association" also seems interested in promoting intravascular ultrasound as a screening tool for carotid plaque and owns shares of Volcano Corporation - that happens to have a member of its board (S. Ward Casscells, MD) from the Texas Heart Institute where Dr. Naghavi works. Dr. Naghavi also has a number of patents in this area of calcium scoring. Now, given all this that I could find on the internet - are we really ready to advise this screening without prospective, randomized trials of its safety or efficacy (especially in terms of long-term cancer risk to our patients)? Or are we willing to repeat a scenario similar to the one we saw recently here in Chicago when doctors with financial interests in ultrafiltration for heart failure were recommending this therapy for their patients or the scenario reported regarding the financial ties between the Cleveland Clinic and Atricure?
Now don't get me wrong - I appreciate the doctors' willingness to disclose their ties to the companies involved. But before we adopt such broad, sweeping recommendations and make them part of policy recommendations that affect the entire US population, we must remove all potential financial conflicts of interests from the recommending body, have a better understanding of the real outcomes and costs imposed when a scan or ultrasound is found to be "positive," and be damn sure the side effects of such scanning (in terms of life-time carcinogenesis) doesn't create new public health problems (analogous to the days when radiation was used to treat acne).
--Wes
Monday, July 10, 2006
Journal Wars
There's lots o' gold in them there journalistic hills....especially if you make $700,000-$830,000 a pop for one article reprint paid for by the drug company that sponsored a trial published in your journal. Oh, and don't think for a minute the New England Journal of Medicine isn't playing with politics, too. Stay tuned for 'Journal Wars - Episode II,' starring Hilary and Barack."The New England Journal of Medicine was made great by
Franz Ingelfinger, who banged on every important door in
Boston urging researchers to admit their best studies to the
journal. The journal assumed the effortless but often
genuine superiority of Bostonians so well described—but
also ridiculed—by Henry James. To some this felt like
arrogance, and the journal has always been hated as well as
admired. Often the motivation for such hatred may have
been jealousy or resentment at failure to make it into its
hallowed pages.Ingelfinger was followed by Bud Relman, and the
journal grew richer as well as grander. The Massachusetts
Medical Society, the owner of the journal, made US$88m
from publishing in 2005. My guess is that the journal
accounts for at least US$75m of that and that its profits are
probably at least US$15m. The society has grown fat on the
profits and is keen not only to keep the profits coming but
also to exploit the brand. This has led to tensions between
the journal and the society, and those tensions were in many
ways the undoing of Jerry Kassirer and Marcia Angel, the
successors to Relman. Both Angel and Kassirer after leaving
the journal published books bemoaning the excessive
influence of the drug industry, while the society
appointed a new editor, Jeff Drazen, who was depicted
by some as a creature of the industry. He had had financial
connections with 21 drug companies between 1994 and
2000."
--Wes
Sunday, July 09, 2006
The Importance of Your Local Doctor
My father has always insisted on getting his health care at Mayo Clinic, one of those exceptional medical centers rated by the US News and World Report magazine. He would travel there and spend a week or so getting every test known to man to assess his current conditions of heart disease, diabetes, lung problems, and kidney problems (none of them rare), and be levied with numerous recommendations for ongoing care when he returned home to the Chicago area.
But a curious thing happened upon his return. While he would carefully follow the doctors instructions (he compulsively managed his insulin-requiring diabetes well), he never found a local doctor. He would leave his health care to the "Mayo" and arrive there annually or bi-annually as the need arose, and feel vindicated that his health care was the best there was. After all, no local doctor could fulfill all his medical needs under one roof. Because of his lengthy medical problem list, it was easier for him to travel to Mayo and "get it all done" rather than have multiple appointments with multiple specialists. In a way, I couldn't argue with him.
But after years of ongoing medical issues and Father Time's inexorable march, his health care situation has become increasingly complex. His medication list reads like the Encyclopedia Britannica. Changing one medication might have rapid and significant implications for the other organ systems involved. Clearly, trips to Mayo on an every-other-day basis or even weekly basis no longer make sense - both medically and economically. He needs a local doctor. Day-to-day evaluations remain invaluable to health care of individuals at this stage (and my father is not unusual) - and might save lives. Are we risking delaying evaluations of individuals as they wait for appointments at the Great Hospitals in the name of prestige?
I was recently shown a set of my father’s blood test results received from a local physician on a day he wasn't feeling too well. The panel demonstrated abnormal electrolytes and crummy kidney function - worse than I recalled from earlier tests I had seen. I urged my father to get a repeat test the next day, but he insisted after significant arguing to return to Mayo for further evaluation. He's there now and due to seen by the nephrologist tomorrow, over half a month from the date those abnormal test results returned. He still doesn't trust our local health care system. Stubbornness and control won out over common sense. Could the marketing of the Greatest Hospitals have affected his judgment?
While hospitals scramble to make this new list of America's Most
But before when he left for Mayo this time, my father acknowledged that the trip from Chicago, Illinois to Rochester, Minnesota was getting tougher for both he and my mother (who now must drive), and he agreed to allow me to help find him a local doctor who is willing to take this bull by the horns. And I assured him, there are lots of capable doctors here in Chicago who can coordinate and facilitate his care that aren't on the US News and World Report's list.
--Wes
Friday, July 07, 2006
Court Upholds Docs Ability to Call Patient Fat
It seems the overwhelming majority (75% of 40,723 responses entered so far) of those who responded to the MSNBC on-line poll said that they have had their doctor say they were overweight as well.
--Wes
Teen Smoking - Da Bomb!

What's dat about? Or dis?
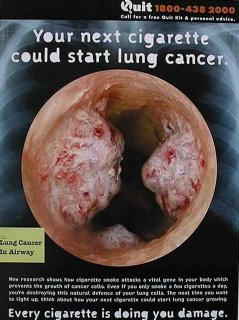
Man, that sucks, dude. I bet your feindin for some cigs right now. 'Specially since in Florida, the cig dudes no longer have to pay all that green to dudes who've died -- oh well, it's just them old dudes anyway - it'll never happen to us. Go ahead, man, light one up, it's da bomb!
After all, teen smoking makes about as much sense as my attempt at teenage idiom.
--Wes
Thursday, July 06, 2006
Grading Surgeons
David Wessel in today's Wall Street Journal noted that researchers have discovered that when surgeons that are labeled publically with bad marks, they quit:
"These are cardiac surgeons, the best students in med school, residency, fellowships - they've always been the stars. It's psychologically difficult to have spent 15 or 20 years training and practicing and then to be identified publically as one of the worst in the state," speculates Ashish Jha, one of the Harvard researchers.I can't say I blame them. What other profession is subject to such public scruitiny and ridicule? There is no other profession that has such an arduous and complicated vetting process. I certainly never see lawyers subject themselves to public "grades." Sadly, I suppose the closest thing to such "grading" is politics and the press - but the press's objectivity (like the "tests" that surgeons must subject themselves to in the name of "quality") can miss the mark badly and ruin careers. And how many politicians attend to their constituents after hours, get called at three AM for a prescription for Xanax, or leave their families in the middle of their son's graduation to repair the ruptured aneurism in a total stranger?
The Wall Street Journal article missed another important issue. Maybe some of these surgeons were quitting because there just isn't as much work for them any more due to the innovations of drug-eluting stents and cholesterol-lowering statin drugs or the fact that liability insurance costs forced them to "retire."
--Wes
Wednesday, July 05, 2006
Prostate News Noone Needs
The study, performed at (UCLA's) Clark Urology Center, was funded by the Stewart and Lynda Resnick Trust. The Resnicks own POM Wonderful, which provided the juice from the Wonderful variety of pomegranate for the study.The sample size was shamefully small (50 patients), only related to slowing PSA "doubling time" (not actual tumor burden), and the mechanism for this action completely unknown. UCLA "researchers" that permit such conjecture to be promulgated as a press release before more answers exist should be ashamed.
-Wes
Medical Error Enthusiasts Caught With Their Own Errors
--Wes
Patients Shoulder More Health Care Costs
"The average medical cost for a family of four participating in a preferred provider organization, or PPO, program is up 9.6% from 2005 to $13,382 in 2006, according to Milliman, a consulting and actuarial firm that released its second annual study Thursday. Unlike other major health care studies, which look at costs in terms of annual premiums or just the employers share, the Milliman study also factors in employee's costs, including out-of-pocket expenses.As the population gets older and more people enter the "golden years," the term "golden years" takes on new meaning:A separate study by Watson Wyatt, a global management-consulting firm, found that businesses expect to further restrict or eliminate retiree medical plans."
"The vast majority of businesses are planning to curtail medical plans for current and future retirees, according to the Watson Wyatt study. The survey of 164 companies found that 14% plan to eliminate the benefit for future retirees over age 65, and 6% plan to eliminate it for their current retirees over age 65."When retirees can no longer afford healthcare, we'll have a huge national health care crisis. After all, retirees utilize over 70% of all health care expenses. Since businesses will no longer shoulder this burden, plan on increased numbers of people than previously projected being "uninsured."
And this won't be healthy for any of us.
--Wes
Tuesday, July 04, 2006
Ford Super-sizes Car Cabins
 --Wes
--Wes
Atrial Fibrillation Increasing in Incidence
But as we begin the celebration of the fourth of July, another article (Reuters) reminds us it's never too late to get our act together, live right, eat right, excercise, quit smoking, moderate drinking and reap the benefits to our health.
Have a great 4th of July. God bless this great country!
--Wes
Sunday, July 02, 2006
A Suggestion to Help Fight Obesity
So the next morning we came downstairs for breakfast. It was remarkable how many people there were obese. Not just a little overweight. I mean obese. It was striking. And the place was packed to capacity. Tons of people (I mean that literally) having their breakfasts of biscuits and gravy, sweet rolls, cereal, french toast, orange juice, coffee, eggs and sausage, before heading out for the day. I wondered if others noticed the same phenomenon. Now I'm no anorexic, but for me to be one of the skinniest guys there was striking - the average body mass index there seemed to exceed the national deficit.
And after returning home, I noticed this article in USA Today about if doctors should tell kids they're "obese". In the interest of political correctness it seems doctors are being encouraged to avoid telling kids they're "obese." Instead, I guess they want is to use the less offensive words "a bit overweight."
Now, having kids of my own, I can certainly sympathize with those who want to be judicious in their criticism of a child's weight, but there's one thing I am certain: kids detect B.S. better than anybody. I strongly believe in being honest with our children. Certainly kids in adolescence have an obsession with their appearance at that age. But kids' peer groups are often much more ruthless and will often ridicule obese children about their appearance. So for us not to acknowledge the obvious and label it accordingly sends a mixed message to children and downplays its importance to their health. Constructive, long-term solutions and guidance are what a child needs and wants, not polite "phrase-ology."
And we mustn't ignore the drug industry's interest in all of this obesity epidemic. As noted by Ivanhoe.com:
"Leading international health writer Ray Moynihan says an expert committee of the American Medical Association has "tentatively decided" to reclassify obesity definitions. The fear is healthy children would be classified as overweight or obese -- and therefore eligible for treatment with obesity drugs. Approximately a quarter of toddlers and two-fifths of children between ages 6 and 11 would be considered obese.And if you believe that independence exists, I have some ocean-front property in Arizona that I'd like to sell you....
Moynihan asserts one of the advocates behind the proposed is a senior member of the International Obesity Task Force. This Task Force, Moyniham says, has close ties to the World Health Organization, which was set up in the mid-1990s with the help of grants from three drug companies and continues to benefit from drug company sponsorship.
Two-thirds of the funding given to the merged International Association for the Study of Obesity and the Task Force, Moynihan says, will come from pharmaceutical giants Roche and Abbott. Roche makes the anti-obesity drug Xenical (orlistat), and Abbott makes the appetite suppressant Reductil (sibutramine hydrochloride). In recent years, drug company sponsorship is likely to have amounted to "millions" says Moynihan, but the Task Force maintains internal scrutiny ensures independence from sponsor influence."
But there really DOES seem to be a problem here in the U.S. The hardest thing to determine is how to effect change in our own habits and open our eyes to this incredible bloating of America. Look around as see what you think. See if you agree with me.
Well, maybe I can suggest a simple way to avoid such gluttony at breakfast and make a small dent in the obesity problem. To loose weight, we might just be better off paying separately for our breakfast rather than staying at these all-you-can-eat breakfast motels. Might we all eat less if we had to pay for each item we consumed? Or if we do stay at one of these places, I think we should be able to get a credit if we decide NOT to use the breakfast at these motels. If I can ask for a non-smoking room, why can't I can ask for an "obesity-friendly" breakfast plan, and save a few bucks. After all, my room rate goes to feed the masses at these places. In effect, I'm supporting the obesity epidemic by staying there.
After all, when it comes to our weight, there's no such thing as a 'free' breakfast.
--Wes