Another cocktail encounter tonight. This time, with an accomplished researcher from one of the major medical centers here in Chicago. She carried more than one NIH RL-1 grant. Interestingly, before the stimulus package was announced, she had to cut her research budgets 30% due to concerns over funding availability.
Then came the Obama Stimulus package.
"So, do you think you'll be able to reinstate those budget cuts for your current research?" I asked.
"Nothing's coming for several months," she said. "So we were told to think of a totally new project and not focus on our real needs for current projects. Instead, we were told we had to create an entirely new project with ridiculous requests for equipment and staffing, above and beyond what exists today. It's crazy."
"And the former work?"
"Who knows? We'll stick to our current budget," she said.
"What a waste."
"Yep. But that seems to be the way the game will be played."
-Wes
Saturday, February 28, 2009
The Nightly News
Now that the stimulus bill has passed and President Obama has promised another $638 billion for a health care reserve fund, perhaps we could put a down-payment on the largess granted by the packages by changing the format of our evening news programs.
In case you missed the news last night, I've compiled the entire informative content in a short video that lasts a little over a minute (with apologies to Itzhak Perlman):
-Wes
Addendum: NYT: "The pharmaceutical industry spent nearly $4.8 billion last year on television and print ads, according to Nielsen Media Research."
In case you missed the news last night, I've compiled the entire informative content in a short video that lasts a little over a minute (with apologies to Itzhak Perlman):
-Wes
Addendum: NYT: "The pharmaceutical industry spent nearly $4.8 billion last year on television and print ads, according to Nielsen Media Research."
Registries: Our Comparitive Effectiveness Research Vehicle
Look for clinical registries to be required for all expensive medical devices soon, despite their limitations.
-Wes
-Wes
Friday, February 27, 2009
Divine Interventions
"Wes, I need a pacer. This guy's temporary pacer wire isn't capturing reliably."
"I'll be right in."
Driving rapidly to hosptial, the microprocesor kicks in: Lab staff called? What's his INR? Antiplatelet agents? WBC count? Access issues? Patient size? Device rep aware?
Calls are made. Info gathered. People mobilized.
Upon arrival I note a very old gentleman with an intraosseous line in his left tibia, and a right internal jugular line in place with a temporary pacing wire at 35 cm, clothes askew with EKG leads attached. Telemetry monitor discloses 2 or three of every five impuses capturing. ("I hate when that happens," I thought.) Chest xray: can't see a thing due to poorly penetrated film. To advance or withdraw the wire... hmmm.... let's try advancing. Pacer spikes, no capture, patient makes strange jerking movements: nope, withdraw... pacer with unreliable capture and patient thrashing about, moving his head side to side. Right. Got it. Tape forehead to bed - have nurse facilitate the head-hold. Is the lab ready?? I need fluoro.
On our way.
Four hours later after a bit of a wrestling match, the pacer is installed and the temporary wires removed. Somewhere, the patient regains enough conciousness to remind us he's a priest. "Really?" He doesn't answer. Instead, he makes gestures top move his hand. "Sir, please hold still!" "But I need the books off my hand." "Sir, there are no books there." "I need the books off my hand!" "Sir, just hold still, just one more layer of stitches to go..." "The bible, please!" "Father, there's no bible there. Just hold still another minute and we'll get you off this table."
Later, the truth is told: 89. Found down. Heart block with ventricular escape rhythm at 15 b/min. Priest.
The next morning: "Can I say the rosary for you, son?"
Thank you, God.
* * *
Later the same week: Repetetive atrial tachycardia in patient with angina each time he has tachycardia. Medications ineffective. Patient 91, DNR, and a priest. Electrophysiology study done after passing catheters past the patient's two transplanted kidneys (first one failed), bilateral hip prostheses and bird's nest IVC filter.
Tachycardia localized. One burn: gone.
Thank you, God.
* * *
Sometimes I feel like I'm not sure if I'm messing with a higher power's plans or He's messing with me.
-Wes
"I'll be right in."
Driving rapidly to hosptial, the microprocesor kicks in: Lab staff called? What's his INR? Antiplatelet agents? WBC count? Access issues? Patient size? Device rep aware?
Calls are made. Info gathered. People mobilized.
Upon arrival I note a very old gentleman with an intraosseous line in his left tibia, and a right internal jugular line in place with a temporary pacing wire at 35 cm, clothes askew with EKG leads attached. Telemetry monitor discloses 2 or three of every five impuses capturing. ("I hate when that happens," I thought.) Chest xray: can't see a thing due to poorly penetrated film. To advance or withdraw the wire... hmmm.... let's try advancing. Pacer spikes, no capture, patient makes strange jerking movements: nope, withdraw... pacer with unreliable capture and patient thrashing about, moving his head side to side. Right. Got it. Tape forehead to bed - have nurse facilitate the head-hold. Is the lab ready?? I need fluoro.
On our way.
Four hours later after a bit of a wrestling match, the pacer is installed and the temporary wires removed. Somewhere, the patient regains enough conciousness to remind us he's a priest. "Really?" He doesn't answer. Instead, he makes gestures top move his hand. "Sir, please hold still!" "But I need the books off my hand." "Sir, there are no books there." "I need the books off my hand!" "Sir, just hold still, just one more layer of stitches to go..." "The bible, please!" "Father, there's no bible there. Just hold still another minute and we'll get you off this table."
Later, the truth is told: 89. Found down. Heart block with ventricular escape rhythm at 15 b/min. Priest.
The next morning: "Can I say the rosary for you, son?"
Later the same week: Repetetive atrial tachycardia in patient with angina each time he has tachycardia. Medications ineffective. Patient 91, DNR, and a priest. Electrophysiology study done after passing catheters past the patient's two transplanted kidneys (first one failed), bilateral hip prostheses and bird's nest IVC filter.
Tachycardia localized. One burn: gone.
Sometimes I feel like I'm not sure if I'm messing with a higher power's plans or He's messing with me.
-Wes
Can You Find Your Blog?
I found mine within the cloud of 883 medical blog titles. (Middle of the right, upper quadrant).
Kind of cool.
-Wes
Kind of cool.
-Wes
New Clinical Risk Factor Score for Atrial Fibrillation
A new "score" to assess the clinical risk factors for the development of atrial fibrillation was published in Lancet today based on epidemiologic variables from the Framingham Heart Study and found:
So when you're at the bar this weekend, relax!
At least statistically you won't be at increased risk of getting atrial fibrillation.
-Wes
"457 (10%) of the 4764 participants developed atrial fibrillation. Age, sex, body-mass index, systolic blood pressure, treatment for hypertension, PR interval, clinically significant cardiac murmur, and heart failure were associated with atrial fibrillation and incorporated in a risk score (p<0·05, except body-mass index p=0·08), clinical model C statistic 0·78 (95% CI 0·76–0·80). Risk of atrial fibrillation in 10 years varied with age: more than 15% risk was recorded in 53 (1%) participants younger than 65 years, compared with 783 (27%) older than 65 years. Additional incorporation of echocardiographic measurements to enhance the risk prediction model only slightly improved the C statistic from 0·78 (95% CI 0·75–0·80) to 0·79 (0·77–0·82), p=0·005. Echocardiographic measurements did not improve risk reclassification (p=0·18).Although the "score" they developed seems too cumbersome to be applied easily in the clinical setting, I thought the most interesting findings of their study was what was NOT found to be a clinical predictor of atrial fibrillation risk: alcohol, hypercholesterolemia, smoking or diabetes. (Almost a quarter of their cohort (22%) were classified as "moderate to heavy alcohol consumers" and nearly a third (32%) were smokers).
So when you're at the bar this weekend, relax!
At least statistically you won't be at increased risk of getting atrial fibrillation.
-Wes
Thursday, February 26, 2009
Anger Management
By now, there must be better than twenty-five "articles" in the so-called "press" about the effects that the emotion anger might have in predicting "heart risks," especially in patients with defibrillators. Each of these journalistic articles point to a recently published manuscript in the Journal of the American College of Cardiology as their authoritative reference, and report the "facts" without any journalistic effort to determine the study's credibility or scientific rigor. Certainly, I do not blame the Journal of the American College of Cardiology for publishing the work - the topic is one that warrants evaluation and critical review. (Of course, what the reviewers of the manuscript were thinking is another issue, but more on that later.)
First, for the lay reader of these press stories, it's important to realize that whenever there are so many stories published simultaneously about a single manuscript like this, the press are almost almost always tipped off about the results by a press release with a really interesting photograph. Certainly if it's about being angry, then the press release shows someone really angry. (It's hard to get your point across otherwise, I guess).
Second, one should always look for a medical device company or academic center that wants to promote the technology or researcher (or both). Interestingly, these articles fly around the internet faster than most because these larger subliminal sponsors have PR teams with friends in high places in the press corps. One doesn't have to look too far to note that the second author of the study, Vladimir Shusterman, MD, PhD, is the President of PinMed, Inc., the maker of the T-wave alternans technology used in this study. But that should not sway us, because we also note that Dr. Shusterman is also "a Faculty Member and Director of Noninvasive Cardiac Electrophysiology Laboratories at the Cardiovascular Institute, University of Pittsburgh."
Interesting that a researcher on such a study can wear two hats like this without batting a single conflict-of-interest eye.
But that's not enough. A few more clicks to follow the research (money?) trail, and we find that the lead author of the study and her home institution (Yale) have been working with PinMed, Inc. for quite a while, so long in fact that the lead author has been quoted saying some nice things about the company on their website:
Finally, there are the issues with the study itself. I find it remarkable that few have questioned a basic premise of the study, that ICD shocks occur more often when people who have a propensity for a tiny increase in T-wave alternans when they get angry, are more likely to have an implantable defibrillator fire. But on the surface, without any fancy schmancy technology, it should be obvious to the casual observer that any defibrillator is more likely to go off when the heart rate is faster than someone whose heart rate is slower: that's how these gizmos work. Certainly, people's hearts might beat faster when they are angry. But any other cause of fast heart rhythm might make them fire as well. In fact, all that has to happen in the most basic defibrillator detection algorithm is the heart rate exceed a programmed rate for a sufficient amount of time and, BAMMO!, the patient gets shocked or might receive anti-tachycardia pacing. Might other things like atrial fibrillation, exercise, sex, anxiety poosibly cause similar therapies? You betcha.
But when one wants to report results for a new-fangled T-wave alternans test that we want the world to use (and maybe on angry people) to predict of their ICD will fire, well we get 62 of them, look for T wave alternans, then follow them for a year to see what their ICD does. Sure enough, 10 of them have some therapies. Yep, t-e-n. Just enough to place these patients into "quartiles" (2 -3 three a quartile???). Then we compare the top and bottom quartile and, yep, there's a statistical difference! Quick, get out the press release!
But alas, if the press had read the paper, they'd find these limitations admitted by the authors:
Sheesh, something like this might make someone angry...
.... uh, oh.
-Wes
First, for the lay reader of these press stories, it's important to realize that whenever there are so many stories published simultaneously about a single manuscript like this, the press are almost almost always tipped off about the results by a press release with a really interesting photograph. Certainly if it's about being angry, then the press release shows someone really angry. (It's hard to get your point across otherwise, I guess).
Second, one should always look for a medical device company or academic center that wants to promote the technology or researcher (or both). Interestingly, these articles fly around the internet faster than most because these larger subliminal sponsors have PR teams with friends in high places in the press corps. One doesn't have to look too far to note that the second author of the study, Vladimir Shusterman, MD, PhD, is the President of PinMed, Inc., the maker of the T-wave alternans technology used in this study. But that should not sway us, because we also note that Dr. Shusterman is also "a Faculty Member and Director of Noninvasive Cardiac Electrophysiology Laboratories at the Cardiovascular Institute, University of Pittsburgh."
Interesting that a researcher on such a study can wear two hats like this without batting a single conflict-of-interest eye.
But that's not enough. A few more clicks to follow the research (money?) trail, and we find that the lead author of the study and her home institution (Yale) have been working with PinMed, Inc. for quite a while, so long in fact that the lead author has been quoted saying some nice things about the company on their website:
"As a practicing electrophysiologist, I can envision multiple clinical uses for the PELEX system once it is approved by the FDA... I think this technology will be extremely useful, both for my own research applications, and also likely for clinical practice."Not that this is bad, mind you. Certainly all of us are entitled to our opinions and biases. But it never ceases to amaze me how gullible the press can be when it comes to scientific PR spin and how this little point was not mentioned in the study's limitations, but rather, Dr. Lampert's conflicts mention only a "minimal" conflict with St. Jude Medical.
Finally, there are the issues with the study itself. I find it remarkable that few have questioned a basic premise of the study, that ICD shocks occur more often when people who have a propensity for a tiny increase in T-wave alternans when they get angry, are more likely to have an implantable defibrillator fire. But on the surface, without any fancy schmancy technology, it should be obvious to the casual observer that any defibrillator is more likely to go off when the heart rate is faster than someone whose heart rate is slower: that's how these gizmos work. Certainly, people's hearts might beat faster when they are angry. But any other cause of fast heart rhythm might make them fire as well. In fact, all that has to happen in the most basic defibrillator detection algorithm is the heart rate exceed a programmed rate for a sufficient amount of time and, BAMMO!, the patient gets shocked or might receive anti-tachycardia pacing. Might other things like atrial fibrillation, exercise, sex, anxiety poosibly cause similar therapies? You betcha.
But when one wants to report results for a new-fangled T-wave alternans test that we want the world to use (and maybe on angry people) to predict of their ICD will fire, well we get 62 of them, look for T wave alternans, then follow them for a year to see what their ICD does. Sure enough, 10 of them have some therapies. Yep, t-e-n. Just enough to place these patients into "quartiles" (2 -3 three a quartile???). Then we compare the top and bottom quartile and, yep, there's a statistical difference! Quick, get out the press release!
But alas, if the press had read the paper, they'd find these limitations admitted by the authors:
"Also, the sample size and number of events was small, and these data should be viewed as hypothesis generating. Whether patients who agreed to participate may differ from the overall population, creating a selection bias, cannot be determined. Larger studies may more definitively establish the predictive value of anger-induced TWA. Further, the programming of ICDs was not uniform. Although the rate cutoffs did not differ between high- and low-anger TWA groups, the possibility that differences in detection times or programmed treatment may have contributed to the findings cannot be excluded."But these limitations don't make headlines, do they? Nope, better to gloss over these fine points and go to press anyway. After all, it's all improving that impact factor, right?
Sheesh, something like this might make someone angry...
.... uh, oh.
-Wes
Wednesday, February 25, 2009
Thanks, Public Citizen!
This morning, the Wall Street Journal reported:
Gosh, I just had to send them a thank-you note back, so I thought I'd place a draft of it here for the blog-o-sphere's edits. Please feel free to add your thoughts.
Public Citizen wrote a letter to the American Medical Association calling on the group to ban medical-industry financial support of continuing medical education courses for doctors. The letter said the ban is necessary "because the consequences of any corrupting influence of commercial support on CME are so significant."Lovely.
Gosh, I just had to send them a thank-you note back, so I thought I'd place a draft of it here for the blog-o-sphere's edits. Please feel free to add your thoughts.
I feel better now.
Dear Public Citizen:
Thank you for your concern regarding the "corrupting influence of commercial support of CME" on our educational experiences. We doctors firmly agree with you that our minds have been firmly and irrevocably corrupted by the evil pharmaceutical and medical device industries. We are nothing but automotons now. We know that the commercials on TV that our patient's see with little dancing balloons to hawk the bladder control drug, Enablex, have completely corrupted our prescribing patterns. (Our patients demand that drug, so we give it. Automatically. Without any thought whatsoever.) The FDA and Congress was misguided and have added to our inability to make up our minds regarding direct-to-consumer advertising. Thank goodness you've come to our rescue.
Oh, those pens I used to receive (we've stopped now) really used to sway me. We'll be sure to wipe clean our Medtronic, St. Jude and Boston Scientific handbags of their logos. And those calipers we received? Those will certainly be pitched, thanks to your gracious reminder of our lemming-like behaviors. Rest assured the rulers we use to convert milliseconds to beats per minute on those EKGs that was given to us by evil St. Jude Medical will be pitched, too.
I have further informed our office staff that they should throw away all post-it notes with drug industry logos and trademarks, since they continue to corrupt us. Oh, and the wall clock with 'Boston Scientific' on it? Trashed. (I regret I've used up all my Lipitor Kleenex pouches, but if I had them, I'd throw them out, too. They were disgusting.) We now have a new line item in our budget for these things that we will purchase ourselves.
Next year, we'll be holding our national meeting in my garage (it will be down-sized significantly) and fold our advocacy groups (I hear they receive 50% of their entire annual budgets from the sale of the evil pharma and device industry's display space on convention floors - can you believe that???) But who needs advocacy in these times of change for doctors? Certainly not us.
We really appreciate and understand your concerns for our well-being. We now understand that all of this advertising costs money and our patients have to pay it when they buy their prescriptions. We understand that we are easy to sway with all of this and it's certainly not in keeping with our moral imperatives. Rest assured we, like you, hate capitalism these days. Socialism will now be our mantra since it's totally in vogue and we know you know what's best for us. After all, government is coming to solve all our problems and will continue to innovate better than the private sector, we're sure.
So keep up the good work. We stand behind you 100%.
Your doctors in snark-
-Wes
Tuesday, February 24, 2009
More Concerning News About Medtronic's Sprint Fidelis Lead
... was published online before print in the journal Heart Rhythm yesterday:
-Wes
Addendum: The story in the New York Times.
"... the hazard of Sprint Fidelis failure accelerated after the first year and continued to increase during the study. In contrast to other defibrillator leads, the Sprint Fidelis failure rate was significantly higher (3.75%/year vs 0.58%/year) and the 3-year estimated survival significantly lower (87.9%, 95% CI 84.8,90.9 vs 98.5%, 95% CI 97.8, 99.3) (p<0.0001). The chance that a Sprint Fidelis lead would survive another year decreased progressively during the study. Most Sprint Fidelis failures were caused by pace-sense conductor fracture (n=63; 87.5%), which caused inappropriate shocks in 36 of 72 patients."As far as I am aware, no new recommendations from Medtronic regarding the management of these leads has been forthcoming (e.g., the cautious "wait and watch approach" seems best for now), but we certainly have seen our share of patients with this problem.
-Wes
Addendum: The story in the New York Times.
This Is What We've Come To?
Excuses, excuses:
But alas, legal liability issues have raised their ugly head once more. The recent the ruling in California that parsed the Good Samaritan law based on a definition of what it means to "rescue" a fellow human being has sent negative reverberations across our country. Certainly, there are plenty of barriers to entry with AEDs, but this is one doctor who remains convinced that these devices are more than worth the risks, hassles and expense.
-Wes
"Hotels worry that if they have the (Automatic External Defibrillator) devices, which cost about $1,200 to $2,000 each, they could be sued for failing to have enough units, failing to put them in the right places, or failing to replace batteries or maintain them properly.Batteries? Make sure your guests in medical distress are treated by trained personnel? Really? Are you serious? How about "we want to make sure guests in medical distress get treated as soon as possible to improve their chance of survival." Wouldn't that sound better in a national PR release?
Another concern: hotel worker training. "Our goal is to make sure guests in medical distress are treated by trained personnel, such as EMTs or paramedics," says a spokesman for Marriott.
But alas, legal liability issues have raised their ugly head once more. The recent the ruling in California that parsed the Good Samaritan law based on a definition of what it means to "rescue" a fellow human being has sent negative reverberations across our country. Certainly, there are plenty of barriers to entry with AEDs, but this is one doctor who remains convinced that these devices are more than worth the risks, hassles and expense.
-Wes
Just Right
Boy, I never knew one of our MedTees could look so cute.
-Wes
PS: For those interested: here's our entire amputee section.
-Wes
PS: For those interested: here's our entire amputee section.
Monday, February 23, 2009
The New Medical Trade Show
With the economy in the tank, look for a the web to play an increasingly important role in health care trade shows meetings. I mean, how many times do we need to travel to Orlando?
-Wes
-Wes
Health Care Cut Backs
... are affecting everyone:
-Wes
"Doctors are noticing the trend as patients skip or defer treatments because of the troubled economy.It was interesting to note that the article quoted a local "recently retired" internist. The untold story within this story is that hospital systems are equally strained as procedural revenues dwindle, placing increased pressure on their physician workforces to "produce."
Many decline procedures even when they have medical insurance, doctors said, because the procedures are so expensive they can't afford the out-of-pocket costs. For a colonoscopy, a stress test, an MRI or a CT scan, the patient's co-pay can run to hundreds of dollars."
-Wes
Sunday, February 22, 2009
Yes They Can
Oh how we forget.
It was under a year ago that physicians were faced with a proposed 10.1% Medicare fee cut. Fortunately, that cut was thwarted after both the House and Senate overrode a Presidential veto of H.R. 6331, the “Medicare Improvements for Patients and Providers Act of 2008.”
But the threat of physician cuts with upcoming legislation persists, especially as Congress looks for ways to save Medicare's unsustainable costs:
But doctors are experts at naval-gazing. We're just too busy. Our independent subspecialty bodies will protect us, really they will. After all, we pay our dues!
But who's really at the table making policy decisions these days?
Is it the Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, American College of Cardiology or even the larger American College of Physicians?
Nope.
It's America's "voice" for doctors: lobbyists for the American Medical Association.
Yep, the AMA - a body whose members represent only 15% of practicing doctors in America and has resorted to all kinds of questionable ways to stay afloat despite the mass exodus of doctors from their membership.
But as we've recently seen, the AMA has access to secret, closed-door meetings with influential left-leaning senators regarding health policy when all other physician advocacy groups do not. Do we honestly think that our individual subspecialty societies for cardiologists, internists, surgeons, hospitalists or even newer, heavily-promoted doctors' internet sites will hold a policy-making candle to the AMA's lobbying stature on the Hill?
No way.
And like it or not, "change" is coming.
In thinking about this and although I'd like to say otherwise, our best bet to advocate for our interests might just be via the American Medical Association. If we're going to have a collective voice concerning upcoming policy decisions as they affect physicians, be it specialist or generalist, MD or DO, hospitalist or primary practice doctor, it just might be time to swallow our collective egos and consider working with the AMA.
Why?
Because like never before, doctors need to collectively advocate for their interests in Washington before the next "Stimulus Bill for Health Care Reform" contains mandated physician pay cuts within it that none of our representatives will even bother to read.
Oh, you think they'd never do this?
Well, as we've now seen ...
... yes they can.
-Wes
It was under a year ago that physicians were faced with a proposed 10.1% Medicare fee cut. Fortunately, that cut was thwarted after both the House and Senate overrode a Presidential veto of H.R. 6331, the “Medicare Improvements for Patients and Providers Act of 2008.”
But the threat of physician cuts with upcoming legislation persists, especially as Congress looks for ways to save Medicare's unsustainable costs:
Under the current formula, doctors would still face cuts of more than 5 percent a year from 2010 to 2012.But a little over a week ago, we witnessed a new and concerning ploy from our legislature eager to pass a pressing agenda: the fear-mongering tactic of "approve it or else." The recent passage of the colossal 1073-page economic "Stimulus Package" representing some $787 billion was never read by a single member of Congress, yet approved. We do not have to think too hard to consider how this same tactic will be deployed with the even larger fiscal crisis of health care reform.
But doctors are experts at naval-gazing. We're just too busy. Our independent subspecialty bodies will protect us, really they will. After all, we pay our dues!
But who's really at the table making policy decisions these days?
Is it the Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, American College of Cardiology or even the larger American College of Physicians?
Nope.
It's America's "voice" for doctors: lobbyists for the American Medical Association.
Yep, the AMA - a body whose members represent only 15% of practicing doctors in America and has resorted to all kinds of questionable ways to stay afloat despite the mass exodus of doctors from their membership.
But as we've recently seen, the AMA has access to secret, closed-door meetings with influential left-leaning senators regarding health policy when all other physician advocacy groups do not. Do we honestly think that our individual subspecialty societies for cardiologists, internists, surgeons, hospitalists or even newer, heavily-promoted doctors' internet sites will hold a policy-making candle to the AMA's lobbying stature on the Hill?
No way.
And like it or not, "change" is coming.
In thinking about this and although I'd like to say otherwise, our best bet to advocate for our interests might just be via the American Medical Association. If we're going to have a collective voice concerning upcoming policy decisions as they affect physicians, be it specialist or generalist, MD or DO, hospitalist or primary practice doctor, it just might be time to swallow our collective egos and consider working with the AMA.
Why?
Because like never before, doctors need to collectively advocate for their interests in Washington before the next "Stimulus Bill for Health Care Reform" contains mandated physician pay cuts within it that none of our representatives will even bother to read.
Oh, you think they'd never do this?
Well, as we've now seen ...
... yes they can.
-Wes
Friday, February 20, 2009
Get Ready for Another Payroll Deduction
Just when we thought the stock market was bad, comes this news from the New York Times today:
Might AARP be interested in making sure the government subsidies that support private Medicare Advantage plans (the ones they sell) continue? Or maybe, they're there advocating for making sure people aged 55 to 64 can be covered under the same plans, even though administrative overhead for any third party administration approaches 30% of the cost?
Or the PhRMA, they wouldn't want to make sure that the Medicare Part D entitlement keeps flowing so they can keep charging their exhorbitant prices for chemotherapeutic agents, would they?
Or the AFL-CIO and their hospital construction workers - they wouldn't want to see their funds for new construction cut, would they? I mean, they're floating the economy right now!
And Easter Seals? Certainly they want to continue the State Children's Health Insurance Program (SCHIP).
Yep, I'm seeing cost savings for our health care system abounding behind those doors, aren't you? And it's so nice to know that they're all "reaching agreement" on how to fund these special interests right from our own paychecks.
-Wes
"Since last fall, many of the leading figures in the nation’s long-running health care debate have been meeting secretly in a Senate hearing room. Now, with the blessing of the Senate’s leading proponent of universal health insurance, Edward M. Kennedy, they appear to be inching toward a consensus that could reshape the debate.And who were these people? Why lobbbyists, of course:
Many of the parties, from big insurance companies to lobbyists for consumers, doctors, hospitals and pharmaceutical companies, are embracing the idea that comprehensive health care legislation should include a requirement that every American carry insurance."
"The 20 people who regularly attend the meetings on Capitol Hill include lobbyists for AARP, Aetna, the A.F.L.-C.I.O., the American Cancer Society, the American Medical Association, America’s Health Insurance Plans, the Business Roundtable, Easter Seals, the National Federation of Independent Business, the Pharmaceutical Research and Manufacturers of America, and the United States Chamber of Commerce."How many of these "doctors" have actually cared for a person in the last year? Probably none. How many nurses were there? None. And how would these brilliant lobbyists enforce this insurance mandate that's worked so well in Massachusetts? Why a tax penalty, of course:
"The ideas discussed include a proposal to penalize people who fail to comply with the “individual obligation” to have insurance.Well, now that the existence of these "secret" closed-door mettings were conveniently "leaked" to a paper with a circulation of over a million readers daily, what's been said behind those closed doors?
“There seems to be a sense of the room that some form of tax penalty is an effective means to enforce such an obligation, though only on those for whom affordable coverage is available,” said the memorandum, prepared by David C. Bowen, a neurobiologist who is director of the health staff at the Senate Committee on Health, Education, Labor and Pensions.
Might AARP be interested in making sure the government subsidies that support private Medicare Advantage plans (the ones they sell) continue? Or maybe, they're there advocating for making sure people aged 55 to 64 can be covered under the same plans, even though administrative overhead for any third party administration approaches 30% of the cost?
Or the PhRMA, they wouldn't want to make sure that the Medicare Part D entitlement keeps flowing so they can keep charging their exhorbitant prices for chemotherapeutic agents, would they?
Or the AFL-CIO and their hospital construction workers - they wouldn't want to see their funds for new construction cut, would they? I mean, they're floating the economy right now!
And Easter Seals? Certainly they want to continue the State Children's Health Insurance Program (SCHIP).
Yep, I'm seeing cost savings for our health care system abounding behind those doors, aren't you? And it's so nice to know that they're all "reaching agreement" on how to fund these special interests right from our own paychecks.
-Wes
Thursday, February 19, 2009
Syntax Trial Online Chat by Dr. Ted Feldman
Dr. Ted Feldman, Director of Interventional Cardiology at NorthShore University HealthSystem and one of the lead authors of the recently published Syntax trial comparing peripheral coronary interventions (PCI) head-to-head with coronary artery bypass grafting surgery (CABG), held an online chat today at noon to discuss the much ballyhooed results published yesterday online before print in the New England Journal of Medicine. The online chat provides a bit of the interventionalist's perspective on the results.
Although the chat has ended, you can view the transcript here by typing in your name and using the password "DES" (clever, eh?).
-Wes
Although the chat has ended, you can view the transcript here by typing in your name and using the password "DES" (clever, eh?).
-Wes
Wednesday, February 18, 2009
My Reservations About Comparative Effectiveness Research
Do we need comparative effectiveness research? Lots and lots of my intelligent colleagues think so. But as usual, I am more suspect.
That's because it will cost a bundle. $1.1 billion has been earmarked for this endeavor in the new Stimulus Bill.
And that's mere seed money.
Think about it: How many issues in medicine need "effectiveness" comparisons? Hundreds? Thousands? Tens of thousands? How much will each project cost? How many teams of "experts" will have to be assembled to tell us is enteric coated aspirin is as effective as plain aspirin for the treatment of arthritis? Oh sure, scoff at the notion, but with bureaucracies, there's virtually no limit to how detailed we can go with this.
And we might not even need it.
That's because comparative effectiveness research is being done, free of charge, right now, right on your computer, via the internet.
It's called t-r-a-n-s-p-a-r-e-n-c-y. Show us the technology, show us the price, show the the prospective, randomized trials, tell us what it'll cost, and let us decide. Plain and simple. Isn't that what where we're already going right now? Is there a better vetting body than the world? I mean, look at the drug costs now available on the internet. Look at the costs of procedures that hospitals are beginning to publish. More and more this will be the norm. Why? Because you and I are having to pay a larger and larger proportion of our health care bill right now.
We'll demand it.
Or are we to be fear-mongered that evil pharma and device companies will surely warp our tiny minds with their marketing schemes and exhorbitant prices so we have no choice but to accept comparative effectiveness reseearch as our ultimate fiscal and medical saviour?
Please.
One only has to recall the exposure of the marketing tactics by drug and device companies in the realm of direct-to-consumer advertising (never mind that Congress, and the FDA, remain beholden to the drug companies for funds never reads the public's tea leaves - (or the Stimulus Bills - d'oh!)). Or look to the remarkable migration of patients from pricey Vytorin to generic simvastatin after the negative results of the Enhance study failed to show an advantage with the combination medication. Was comparative effectiveness research responsible for these epiphanies?
Nope.
Finally, there's some real-life research issues with comparative effectiveness research that are concerning. First: "effectiveness research" relies on the history of competing technologies. New technologies will almost always be at a disadvantage to older technologies because they do not have a history of experience with which to compare. If doctors require a learning curve in the application of any new medical advance, might there be a bias to pull new technologies before they're understood? Perhaps.
Secondly, the term "effectiveness" is bothersome because it implies there must be one correct answer. Take, for instance, a therapy that prolongs life "effectively" that is expensive (many of the new cancer drugs come to mind). If cost-effectiveness is the goal, then using none of the drug and letting the patient succumb to cancer might be the most "effective" use of the drug to save costs to our health care system. But if longevity is the primary effectiveness goal, then the best therapy might be incredibly costly in a younger patient. Which effectiveness goal will be chosen for each of the therapies tested? Cost or clinical outcome? If a "blended" goal is desired, who will decide how much of which goal will be ultimately chosen?
Finally, what about confounding factors? How can any of the millions of permutations of co-existing conditions be weighed in effectivness research? Take coronary stents, for instance. Whereas a drug-eluting stent might be the perfect choice in terms of limiting restenosis in a particular clinical situation, will comparative effectiveness research limit a cardiologist's ability to place a bare metal stent instead because he knows the patient will be undergoing hip replacement in four weeks? Can we really expect an algorithm mandated by researchers and bureaucrats to account for these situations? If so, how extensive will all the exclusion criteria become?
Suddenly to me, it seems the crystal clear goals of Comparative Effectiveness Research become very clouded.
Rather, I think this $1.1 billion earmark for comparative effectiveness research is really about stimulating research budgets for the "Chosen Fifteen" connected research politicos rather than helping doctors know how best to treat their patients. No one study or group of individuals can apply such studies to the individual patient - I don't care how much money we dump into their research. Clinical guidelines have been careful not to supercede clincal judgement and comparative effectiveness research shouldn't either. To do so invites liability claims and the potential for untoward health care delivery in the name of government mandates that might ultimately threaten the doctor-patient relationship.
Then what have we accomplished for our $1.1 billion dollars?
-Wes
That's because it will cost a bundle. $1.1 billion has been earmarked for this endeavor in the new Stimulus Bill.
And that's mere seed money.
Think about it: How many issues in medicine need "effectiveness" comparisons? Hundreds? Thousands? Tens of thousands? How much will each project cost? How many teams of "experts" will have to be assembled to tell us is enteric coated aspirin is as effective as plain aspirin for the treatment of arthritis? Oh sure, scoff at the notion, but with bureaucracies, there's virtually no limit to how detailed we can go with this.
And we might not even need it.
That's because comparative effectiveness research is being done, free of charge, right now, right on your computer, via the internet.
It's called t-r-a-n-s-p-a-r-e-n-c-y. Show us the technology, show us the price, show the the prospective, randomized trials, tell us what it'll cost, and let us decide. Plain and simple. Isn't that what where we're already going right now? Is there a better vetting body than the world? I mean, look at the drug costs now available on the internet. Look at the costs of procedures that hospitals are beginning to publish. More and more this will be the norm. Why? Because you and I are having to pay a larger and larger proportion of our health care bill right now.
We'll demand it.
Or are we to be fear-mongered that evil pharma and device companies will surely warp our tiny minds with their marketing schemes and exhorbitant prices so we have no choice but to accept comparative effectiveness reseearch as our ultimate fiscal and medical saviour?
Please.
One only has to recall the exposure of the marketing tactics by drug and device companies in the realm of direct-to-consumer advertising (never mind that Congress, and the FDA, remain beholden to the drug companies for funds never reads the public's tea leaves - (or the Stimulus Bills - d'oh!)). Or look to the remarkable migration of patients from pricey Vytorin to generic simvastatin after the negative results of the Enhance study failed to show an advantage with the combination medication. Was comparative effectiveness research responsible for these epiphanies?
Nope.
Finally, there's some real-life research issues with comparative effectiveness research that are concerning. First: "effectiveness research" relies on the history of competing technologies. New technologies will almost always be at a disadvantage to older technologies because they do not have a history of experience with which to compare. If doctors require a learning curve in the application of any new medical advance, might there be a bias to pull new technologies before they're understood? Perhaps.
Secondly, the term "effectiveness" is bothersome because it implies there must be one correct answer. Take, for instance, a therapy that prolongs life "effectively" that is expensive (many of the new cancer drugs come to mind). If cost-effectiveness is the goal, then using none of the drug and letting the patient succumb to cancer might be the most "effective" use of the drug to save costs to our health care system. But if longevity is the primary effectiveness goal, then the best therapy might be incredibly costly in a younger patient. Which effectiveness goal will be chosen for each of the therapies tested? Cost or clinical outcome? If a "blended" goal is desired, who will decide how much of which goal will be ultimately chosen?
Finally, what about confounding factors? How can any of the millions of permutations of co-existing conditions be weighed in effectivness research? Take coronary stents, for instance. Whereas a drug-eluting stent might be the perfect choice in terms of limiting restenosis in a particular clinical situation, will comparative effectiveness research limit a cardiologist's ability to place a bare metal stent instead because he knows the patient will be undergoing hip replacement in four weeks? Can we really expect an algorithm mandated by researchers and bureaucrats to account for these situations? If so, how extensive will all the exclusion criteria become?
Suddenly to me, it seems the crystal clear goals of Comparative Effectiveness Research become very clouded.
Rather, I think this $1.1 billion earmark for comparative effectiveness research is really about stimulating research budgets for the "Chosen Fifteen" connected research politicos rather than helping doctors know how best to treat their patients. No one study or group of individuals can apply such studies to the individual patient - I don't care how much money we dump into their research. Clinical guidelines have been careful not to supercede clincal judgement and comparative effectiveness research shouldn't either. To do so invites liability claims and the potential for untoward health care delivery in the name of government mandates that might ultimately threaten the doctor-patient relationship.
Then what have we accomplished for our $1.1 billion dollars?
-Wes
Back At It
Tuesday, February 17, 2009
Stimulate This!
“Now, a few more items for your last day of nursing orientation. Your safety is our first priority. Therefore, we do not use trauma patients’ names, ya hear? It’s “Trauma Purple” or “Trauma Red” from now on. We don’t need some friend of the family packing a piece to know where to find their cousin. Oh, and one more thing…. before I let you go I need you to find a hiding place – any place. Except the linen cart – that’s where I’ll be.”It’s not Kansas anymore, Toto. It’s just another orientation day at your local county trauma center in southern Florida, where approximately 50 percent of patients are uninsured or illegal non-US citizens.
But it is here that we’ll see what the health care of the future looks like: where private health insurance will cease to exist. That’s because it’s assumed patients in this locale don’t have insurance in the first place, and if they do, the coverage is so minimal relative to the health care needs of the afflicted, that the cost of care will quickly exceed their coverage limits. Here, the delivery of health care has become too expensive, even for insurers. And so the government and taxpayer are left to pay the tab. And like never before, local governments are feeling the pinch of health care costs with billions and billions of dollars of budgetary shortfalls, much created by health care costs for the uninsured or non-US citizens.
But please, don’t talk about this – our economy depends on this model of employer-offered health insurance! How else will we retain our workforce? Please Mr. Stimulus Package, can you spare a dime?
Never mind that it’s a finger in the dyke.
-Wes
Monday, February 16, 2009
Why Community Hospitals Are Dying
... because when you're in Florida and try to get an right hip x-ray on your mother, community hospitals like Englewood Community Hospital (part of the HCA Health Care) says they have to verify that the doctor ordering the study (my mother's doctor in Illinois) really exists before the test can be performed, and that will take two or three days.
Funny, the guys across the street, Radiology Associates of Venice and Englewood, a free-standing radiology group, could do it the same day - happily.
Thank goodness the helpful receptionist at Englewood Community Hospital gave us the name of these guys - at least she could see the forest from the trees.
God bless the free-market health care system. Do we really want to see this go away?
-Wes
Funny, the guys across the street, Radiology Associates of Venice and Englewood, a free-standing radiology group, could do it the same day - happily.
Thank goodness the helpful receptionist at Englewood Community Hospital gave us the name of these guys - at least she could see the forest from the trees.
God bless the free-market health care system. Do we really want to see this go away?
-Wes
Health Care Finance Reform and The Bernie Madoff Syndrome
“Double digit growth on your investment year after year – it doesn’t matter what the market’s doing – he’s incredible! Seriously, Howard, you can’t do better! I’m tellin’ you, he’s got the Midas touch. But it’s not easy to get a meeting with him, Howard, you have to know somebody…“In retrospect, the Bernie Madoff story seems so obvious, doesn’t it? How could so many people have been sucker-punched into believing that one guy had figured out a system to virtually guarantee growth of their portfolios irrespective of market conditions? Why did so few smell the rat? After all, these people who were conned by this man were not idiots, they were some of America’s most successful and influential people in the business world. Most of them were people with remarkable creativity, foresight and investment savvy. All of them were connected by friends of friends – someone who could get them access to Bernie, and nearly all of them had egos. Big egos.
But before we start mocking the rich folks taken by Mr. Madoff, we have to acknowledge that Americans love the Bernie Madoffs of the world. They reassure us. They make it easy. No need to ask the thorny questions. No. He’ll handle it. You won’t have to worry about a thing. Seriously. Just leave it up to him. Just give him your money and watch it grow. Here, can I give you a ride in my Mazerati?
Welcome to America’s latest financial affliction: the Bernie Madoff Syndrome, or “Bernie Syndrome,” for short.
And the Bernie Syndrome particularly afflicts the health care finance reform efforts underway. Can’t you hear it?
I mean, what’s a trillion here or a trillion there?
Don’t worry, we’ll make sure you can get health care. Seriously. He’ll just ask Congress to feed our broken, dysfunctional system so you can keep your employee-sponsored health care plan with its ten-dollar co-pay. No need to know how on earth we’re going to pay for it. Health care will be provided for all the kids with SCHIPS and seniors will be covered with our new, soon-to-be-lowered Medicare eligibility age limit of 55 without any loss of services! “Bernie” will handle it.
“Bernie” has access to friends in Washington. “Bernie” knows the finance system. “Bernie” knows how to get more money printed to pay for the system that “Bernie’s” friends on the Hill are already paying for. I mean, that’s what “Bernie” does! “Bernie” has the incredibly audacious ability to seemingly make money from, well, nothing! Don’t you see? “Bernie” will fix it!
But what will “Bernie’s” monthly statements really look like?
Details like loaded bureaucracies, shrinking numbers of physicians, rising costs of technology, inflated hospital costs, - not for you to worry about. Instead, we’ll be asked to “prevent chronic disease” as a way to bring our health care system back to solvency. We’ll spend billions upon billions to lower COBRA payments for the uninsured to show that meaningful efforts are underway to save our health care system. We’ll hear about the things we want to hear, like “access,” “electronic medical records,” and “quality.”
That’s because we’ve all contracted Bernie Syndrome.
After all, a person with Bernie’s Syndrome is trusting. A person with Bernie’s Syndrome likes to hear good news. A person with Bernie’s Syndrome thinks its offensive to ask too many questions. A person with Bernie’s syndrome wants to be one of the team.
And there’s really nothing to worry about.
After all, “Bernie’s” one of us.
-Wes
Thursday, February 12, 2009
They've Got Gonads

Amazing. This ad as found on MDLinx.com's cardiology section for Lilly's Effient (prasugrel) before the drug's even approved by the FDA and despite the controversy swirling around about their advisory panel's approval meeting.
Lilly wouldn't have an inside line, would they?
-Wes
Blog Lite
I'll be heading to a warmer climate for a few days. Blogging and comment moderation might slow a bit 'til mid-next week.
-Wes
-Wes
Wednesday, February 11, 2009
The EP Implications of the Economic Crisis
"Your patient that you saw with supraventricular tachycardia called today to say she and her husband lost their jobs and they've had to postpone their ablation procedure until they can see if they can get financial assistance."
-Wes
-Wes
EKG Du Jour #14 - Where's the Beat?
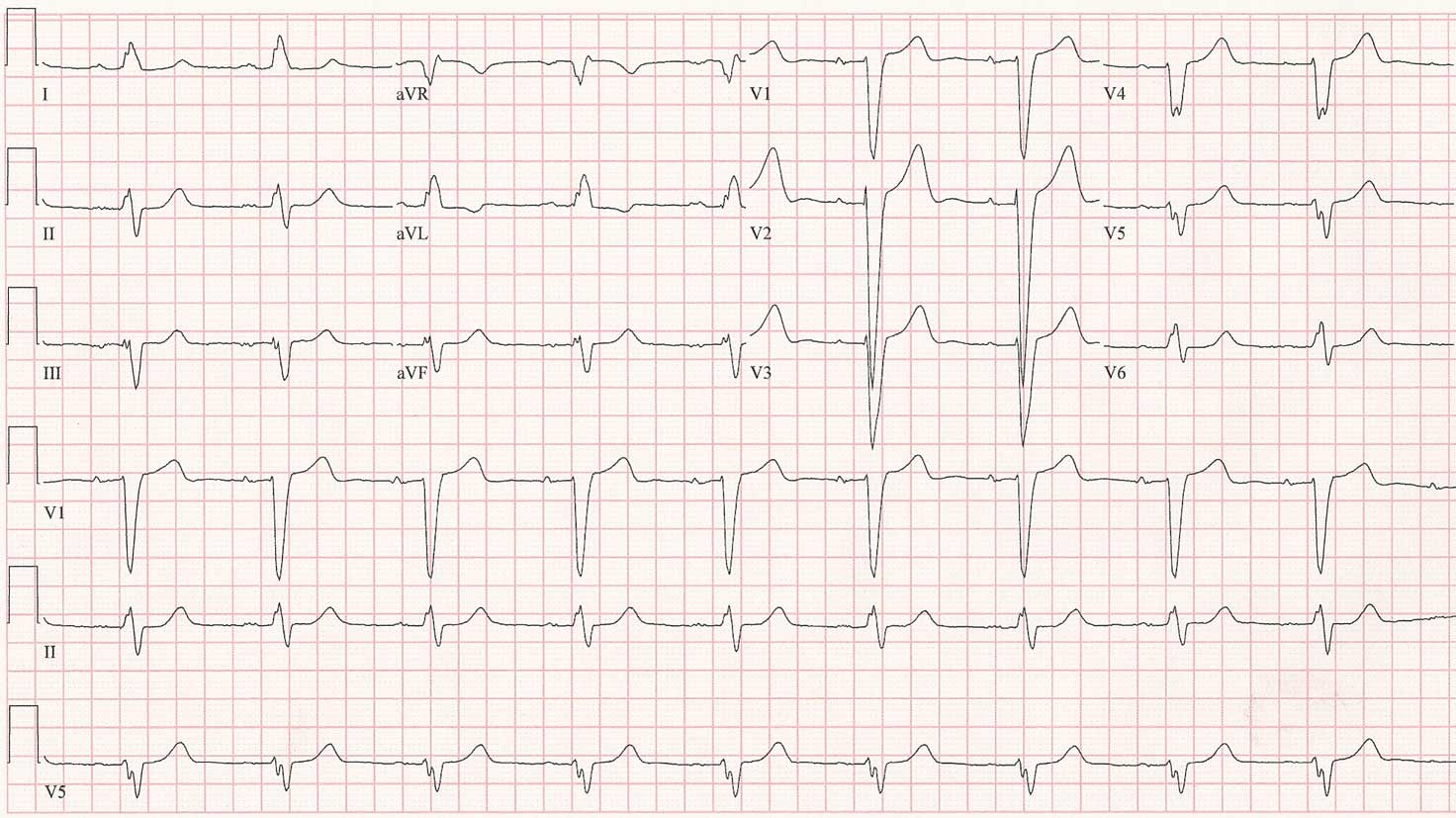
You are called to evaluate an older woman who presented to the ER complaining of shortness of breath for the past several weeks, but now is spiking fevers to 102 with associated rigors. She had bilateral lower lobe rales and her chest xray suggested the presence of a right lower lobe infiltrate. She had undergone an uncomplicated pulmonary vein isolation procedure two years prior for paroxysmal atrial fibrillation but had some persistent atrial tachycardia after the procedure well-controlled on atenolol 50 mg twice a day. Her white count and troponin levels are normal. A V/Q scan to evaluate for pulmonary embolus was low probability for pulmonary embolus. Interestingly, her initial EKG looked different than her baseline EKG:

Eight minutes later, the nurse notes a change in the EKG and decided to perform another EKG:

For reference, here's what her baseline EKG looks like on her usual atenolol dose:
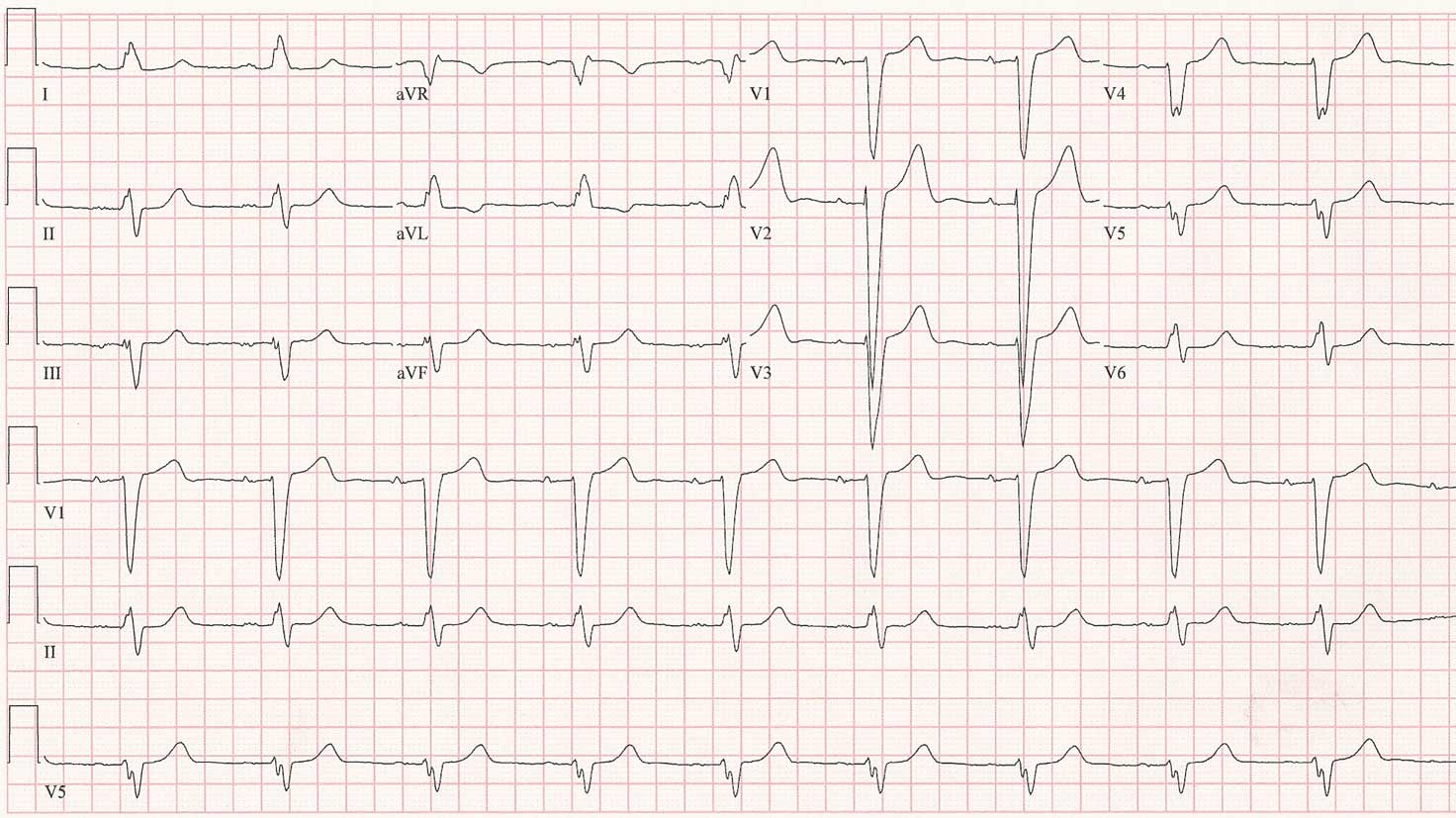
So, how do we explain what's happening in the first two EKG's? Does she need a pacemaker?
-Wes

Click image to enlarge
Eight minutes later, the nurse notes a change in the EKG and decided to perform another EKG:

Click image to enlarge
For reference, here's what her baseline EKG looks like on her usual atenolol dose:
Click image to enlarge
So, how do we explain what's happening in the first two EKG's? Does she need a pacemaker?
-Wes
Tuesday, February 10, 2009
Health Care Pork
"They’ll be jobs building the wind turbines and solar panels and fuel-efficient cars that will lower our dependence on foreign oil and modernizing our costly health care system that will save us billions of dollars and countless lives.""Modernizing" our costly health care system?- President Barack Obama's First Press Conference, 9 February 2009
Here's a small sampling of our health care system that needs modernizing, right here in the Chicago metro area:
You decide, is our health care system in desperate need of modernization or is this just self-stimulatory behavior?
Prentice Women's Hosptial, Northwestern University Hosptial, Chicago, IL
Loyola University Medical Center, Maywood, IL
University of Chicago Medical Center, and Children's Hospital, Chicago, IL
Rush University Medical Center, Chicago, IL
Sherman Hospital, Elgin, IL
Edward Hosptial and Health Services, Naperville, IL
"We find ourselves in a rare moment where the citizens of our country and all countries are watching and waiting for us to lead. It’s a responsibility that this generation did not ask for, but one that we must accept for the future of our children and our grandchildren.
The strongest democracies flourish from frequent and lively debate, but they endure when people of every background and belief find a way to set aside smaller differences in service of a greater purpose. That’s the test facing the United States of America in this winter of our hardship, and it is our duty as leaders and citizens to stay true to that purpose in the weeks and months ahead."- President Barack Obama, 9 Feb 2009
-Wes
Monday, February 09, 2009
The IF, THEN, ELSE, BUT Loops of Medicare
Pop quiz time!
Quick: When was the last time you saw your doctor?
I don’t mean the last year, month, or week … I mean the actual date of your last visit.
Don’t remember? What do you mean? Come on now! T-h-i-n-k!
Give up? Here. Let me make it simpler:
Today is 9 Feb 2009. Quick: What day was exactly 90 days ago?
Did you have to look at a calendar? Did you find this as difficult to calculate as most people do? Did you get 11 Nov 2008? No? Why not?
You see, doctors like me have to know if you were seen in the last 90 days.
Because if you had a cardiac device and IF you were not seen in the last 90 days, THEN I could bill you for my evaluation of your cardiac device with a larger paying code, ELSE I’d have to bill you with another lower-reimbursing code, BUT if your device was evaluated in the last 30 days, I couldn’t bill you at all.
Just like a computer program: welcome to the IF, THEN, ELSE, BUT loops of Medicare billing.
Isn’t this fun?
Now, multiply these IF, THEN, ELSE, BUT loops for one-lead versus multi-lead pacing systems, and one-lead or multi-lead defibrillation systems. Add a few more for evaluating sensor parameters and a few more for implantable event recorders. Then add a few more for remote evaluation versus face-to-face up evaluations. Add ‘em all together and you can have twenty-six new codes just for implantable cardiac device checks implemented 1 January 2009! Device checks whose payment is not only dependent on what you did today, but when you did the preceding evaluation, whether it's clinically appropriate or not.
It’s remarkable to me the lengths we've gone to ration health care in America without saying we’re rationing. (And it's only going to get worse.)
But folks, make no mistake: we’re rationing.
And you and your doctors are paying the price.
-Wes
Quick: When was the last time you saw your doctor?
I don’t mean the last year, month, or week … I mean the actual date of your last visit.
Don’t remember? What do you mean? Come on now! T-h-i-n-k!
Give up? Here. Let me make it simpler:
Today is 9 Feb 2009. Quick: What day was exactly 90 days ago?
Did you have to look at a calendar? Did you find this as difficult to calculate as most people do? Did you get 11 Nov 2008? No? Why not?
You see, doctors like me have to know if you were seen in the last 90 days.
Because if you had a cardiac device and IF you were not seen in the last 90 days, THEN I could bill you for my evaluation of your cardiac device with a larger paying code, ELSE I’d have to bill you with another lower-reimbursing code, BUT if your device was evaluated in the last 30 days, I couldn’t bill you at all.
Just like a computer program: welcome to the IF, THEN, ELSE, BUT loops of Medicare billing.
Isn’t this fun?
Now, multiply these IF, THEN, ELSE, BUT loops for one-lead versus multi-lead pacing systems, and one-lead or multi-lead defibrillation systems. Add a few more for evaluating sensor parameters and a few more for implantable event recorders. Then add a few more for remote evaluation versus face-to-face up evaluations. Add ‘em all together and you can have twenty-six new codes just for implantable cardiac device checks implemented 1 January 2009! Device checks whose payment is not only dependent on what you did today, but when you did the preceding evaluation, whether it's clinically appropriate or not.
It’s remarkable to me the lengths we've gone to ration health care in America without saying we’re rationing. (And it's only going to get worse.)
But folks, make no mistake: we’re rationing.
And you and your doctors are paying the price.
-Wes
For Valentine's Day?
I think my wife would kill be if I gave her this.
Reminds of the lava lamps...
But like the scene in Bug's Life:
I can't ... stop ... being.... drawn... to ... it....
-Wes
Reminds of the lava lamps...
But like the scene in Bug's Life:
I can't ... stop ... being.... drawn... to ... it....
-Wes
Sunday, February 08, 2009
On Greed
Ladies and gentleman, I give you Milton Friedman, the master of Socratic reasoning:
-Wes
h/t: Patterico's Pontifications via Instapundit.
-Wes
h/t: Patterico's Pontifications via Instapundit.
Seeing Stars
Seems the star-rating system used by CMS to rank nursing homes has some rough edges:
Oh, wait, electronic medical records? Why might nursing homes, with our sickest and oldest patients, need those? (Taking tongue out of cheek now...)
-Wes
Many nursing home officials—and consumer advocates—assail the star system for rating the facilities.Self-reported data might be part of the problem, as are lack of electronic medical records...
Administrators say the ratings are too simplistic. Advocates fear some five-star homes are overrated and may give consumers false comfort.
Wendy Meltzer of Illinois Citizens for Better Care said she thinks the star ratings "are going to kill people."
Oh, wait, electronic medical records? Why might nursing homes, with our sickest and oldest patients, need those? (Taking tongue out of cheek now...)
-Wes
Prasugrel: This Drug Scares Me
How can any clot-busting drug for cardiology be approved without data on post-surgical bleeding complications after defibrillator or pacemaker implantation?
Just asking.
(I wonder what the FDA's (absent) Safety and Risk Management committee might have said.)
-Wes
Reference: "Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes," New Engl J Med, November 15, 2007, 357(20):2001-2015.
Just asking.
(I wonder what the FDA's (absent) Safety and Risk Management committee might have said.)
-Wes
Reference: "Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes," New Engl J Med, November 15, 2007, 357(20):2001-2015.
More Chicago Bloggers Served Subpoenas
Boy, this sounds familiar.
It seems serving bloggers subpoenas is a favorite activity of some Chicago lawyers. In my case, it took three trips to court and over three months of legal costs in attempt to quash the subpoena, only to have the subpoena rendered "moot" when the case was dismissed.
I encourage anyone else who might have this occur to contact the Electronic Frontier Foundation, a San Francisco-based organization that defends the First Amendment rights of those who use the Internet and other digital media to exercise their freedom of speech. It could save you a bundle.
In my case, by subpoena was "served" to my front desk clerk, came with a cover letter claiming it was a "Second Notice" (I never received a first notice), and was "served" just twenty-four hours before I was due to appear to make a statement in the attorney's office in person without any offer for reimbursement for time, parking or travel.
I'm telling you, it happens.
-Wes
h/t Overlawyered.
It seems serving bloggers subpoenas is a favorite activity of some Chicago lawyers. In my case, it took three trips to court and over three months of legal costs in attempt to quash the subpoena, only to have the subpoena rendered "moot" when the case was dismissed.
I encourage anyone else who might have this occur to contact the Electronic Frontier Foundation, a San Francisco-based organization that defends the First Amendment rights of those who use the Internet and other digital media to exercise their freedom of speech. It could save you a bundle.
In my case, by subpoena was "served" to my front desk clerk, came with a cover letter claiming it was a "Second Notice" (I never received a first notice), and was "served" just twenty-four hours before I was due to appear to make a statement in the attorney's office in person without any offer for reimbursement for time, parking or travel.
I'm telling you, it happens.
-Wes
h/t Overlawyered.
Saturday, February 07, 2009
Why I'm Pessimistic About EMR Integration
Take a look at the major health care IT vendors. They're all working feverishly to collect, collate, process, and puree your health care information, billing codes, insurance carriers, hospitals, quality assurance mandates and red flags, etc.
The prize?
To become our national health care IT system. To own it ALL!
Now look at the pacemaker industry in the US.
Three big companies. All promoting their pacemakers.
Each manufacturer's pacemaker computer is unique to their pacemaker models, but does the same job: they each "talk" to their respective pacemakers and tells them how fast or slow to go and how much energy to use to do the job safely. To do this, they use "protocols." Protocols are closely-guarded trade secrets.
And so as a fellow, when we did not know which manufacturer's pacemaker was installed in a patient's chest, I could not bring a single computer to talk to the pacemaker inside a particular patient. Instead, I had to push a huge cart carrying multiple computer programmers to the patient's bedside, each with their own special printer paper and programming heads, to interrogate the patient's pacemaker at their bedside.
Recall that the first pacemaker was developed in 1949. Since that time, the basic design and construct of pacemakers has become fairly standardized. Sixty years have passed. Today, do any of these pacemaker companies' computer systems talk to their competitors' pacemakers?
Of course not.
Share protocols? Are you crazy? That would compromise their intellectual property!
You see, it's really not about what's good for the patient or doctor.
It's about the money.
'nuf said.
-Wes
The prize?
To become our national health care IT system. To own it ALL!
Now look at the pacemaker industry in the US.
Three big companies. All promoting their pacemakers.
Each manufacturer's pacemaker computer is unique to their pacemaker models, but does the same job: they each "talk" to their respective pacemakers and tells them how fast or slow to go and how much energy to use to do the job safely. To do this, they use "protocols." Protocols are closely-guarded trade secrets.
And so as a fellow, when we did not know which manufacturer's pacemaker was installed in a patient's chest, I could not bring a single computer to talk to the pacemaker inside a particular patient. Instead, I had to push a huge cart carrying multiple computer programmers to the patient's bedside, each with their own special printer paper and programming heads, to interrogate the patient's pacemaker at their bedside.
Recall that the first pacemaker was developed in 1949. Since that time, the basic design and construct of pacemakers has become fairly standardized. Sixty years have passed. Today, do any of these pacemaker companies' computer systems talk to their competitors' pacemakers?
Of course not.
Share protocols? Are you crazy? That would compromise their intellectual property!
You see, it's really not about what's good for the patient or doctor.
It's about the money.
'nuf said.
-Wes
Friday, February 06, 2009
The Right Ventricle in 3D
There's some pretty cool images of a rabbit's right ventricular free wall that you can view in 3D over at virtuallyshocking.com.
Just cross your eyes.
(Geez, I've got a headache...)
-Wes
Just cross your eyes.
(Geez, I've got a headache...)
-Wes
"Go Red for Men" Logo Announced
And now, ladies and gentleman, completely free of commercial endorsement, I'd like to announce the Go Red for Men national campaign to raise heart disease awareness in men with a new logo, available to all, and completely free of any charge or requirement to purchase a thing.
And if women can use a red dress, guys can use....
... are you ready????? .....
.... boxer shorts!

For those who might want to place this simple logo on their blog in the sidebar, I've included a down-sized version for you:

"Go Red" guys! Just cut and paste the logo in your blog or website. And feel free to share your story of heart disease in the comments section. It's all about you. Let's build a community!
-Wes
PS: Oh, the logo was courtesy Wikimedia Commons and pleasantly photoshopped for free. I'm wearing red (but it's hidden), how about you?
And if women can use a red dress, guys can use....
... are you ready????? .....
.... boxer shorts!

For those who might want to place this simple logo on their blog in the sidebar, I've included a down-sized version for you:

"Go Red" guys! Just cut and paste the logo in your blog or website. And feel free to share your story of heart disease in the comments section. It's all about you. Let's build a community!
-Wes
PS: Oh, the logo was courtesy Wikimedia Commons and pleasantly photoshopped for free. I'm wearing red (but it's hidden), how about you?
Thursday, February 05, 2009
Go Red for Men, Too
After literally hundreds of politically-correct publications and press releases regarding the Go Red for Women campaign sponsored, in part, by Merck, Macy's, Jiffy Lube, Campbell's Soup, Blue Diamond Almonds, Cutco, Clairol Professional, e-GLAM, Flooring America, Fresh Express / Chiquita, Geoffrey Beene, Hamilton Beach, Jafra, Ocean Spray, Prego Heart Smart, Rite Aide, Starkist, Supervalu, Swanson Premium Chuck Chicken, Swarovski, V8 Beverages, Yankee Candle, wireless carrriers AT&T, Nextel, Sprint, T-Mobile, U.S. Cellular and Verizon Wireless (they help you donate from your cell phone - just don't forget to text "STOP" to unsubscribe after you donate!), and oh yeah, the American Heart Association (whew!), I'd like to take a moment and be politically incorrect and say:
"Go Red for Men, Too!"
Here's some stats from the CDC on heart disease in men, lest the guys out there feel left out tomorrow:
Nah. That would be too depressing.
Red, baby, red.
-Wes
"Go Red for Men, Too!"
Here's some stats from the CDC on heart disease in men, lest the guys out there feel left out tomorrow:
Although my feelings about the commercial nature of the Go Red for Women Campaign haven't changed much, as I read over these older statistics for heart disease, I sometimes wonder if guys should wear black tomorrow instead.
- In 2005, 322,841 men died from heart disease, the leading cause of death for men in the United States.
- The age-adjusted death rate for heart disease in men was 260 per 100,000 population in 2005.
- About 9.4% of all white men, 7.1% of black men, and 5.6% of Mexican American men live with coronary heart disease.
- The average age of a first heart attack for men is 66 years.
- Almost half of men who have a heart attack under age 65 die within 8 years.
- Results from the Framingham Heart Study suggest that men have a 49% lifetime risk of developing coronary heart disease after the age of 40.
- Between 70% and 89% of sudden cardiac events occur in men.
- Major risk factors for heart disease include high blood pressure, high blood cholesterol, tobacco use, diabetes, physical inactivity, and poor nutrition.
- In a large study of blood pressure treatment and control, an average reduction of 12 to 13 mm Hg in systolic blood pressure over 4 years of follow-up was associated with a 21% reduction in coronary heart disease, 37% reduction in stroke, and 13% reduction in all-cause mortality rates.
- Studies suggest that a 10% decrease in total cholesterol levels may reduce the development of coronary heart disease by as much as 30%.
Nah. That would be too depressing.
Red, baby, red.
-Wes
Wednesday, February 04, 2009
No More Goodies?
Sorry doctors, we will no longer will be bringing branded trinkets to your office. You know, our new policy states "the changes prohibit gifts of any type, including all non-educational branded promotional items, regardless of value."
Instead, we'll just bring our truck and park it in your lot:

With love,
AdvaMed
-Wes
Addendum 05 Feb 6:50 AM CST: Background from the FDA Law Blog
Instead, we'll just bring our truck and park it in your lot:

Click image to enlarge
With love,
AdvaMed
-Wes
Addendum 05 Feb 6:50 AM CST: Background from the FDA Law Blog
The Academic Surgical Model Strained
It seems the requirement for surgeons to be part of academia (and therefore, have to contribute to a medical school's "dean's tax" for the priviledge of their academic title), caused surgeons to bail in West Virginia:
-Wes
“The construct of this relationship historically has dictated that all of the surgeons in the program had to be academic full-time faculty in the School of Medicine. So, I think one could argue, and it was certainly Mon General’s perspective that by only having one model under which cardiac surgeons could work in this market constrained the recruitment process,” McClymonds said.These days, money talks. Declining Medicare payments coupled with declines in the surgical workforce are permitting many academic surgeons to rethink classic payment models.
-Wes
EKG Du Jour #13: What Is This?
One of our advance practice nurses was rounding on the ward and knew a patient had a Guidant pacemaker and intermittent atrial fibrillation and flutter. She was checking the telemetry on the patient and found this unusual strip:
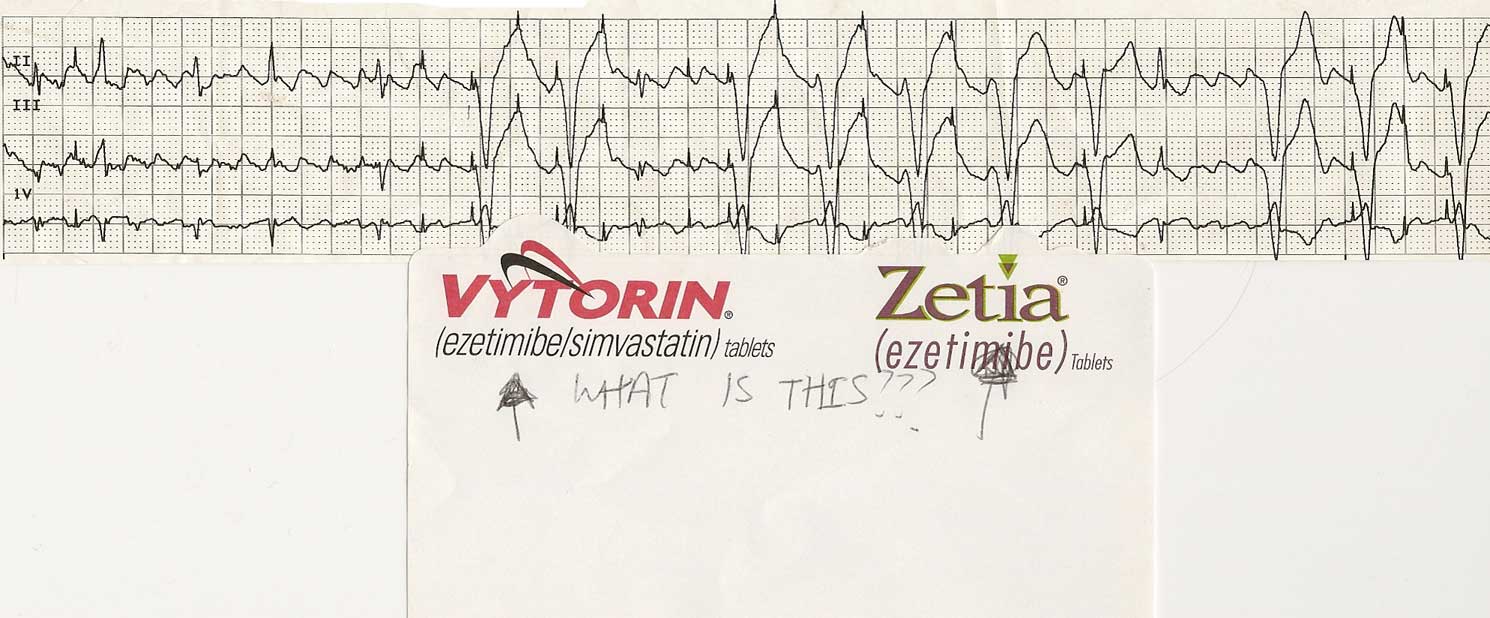
She attached the post-it note asking "What is this?" and left it for my review. (I love it when new blog items appear on my desk.)
Anyway, other than an advertisement for Vytorin or Zetia, the question should be asked to the blog-o-sphere:
What is this?
-Wes
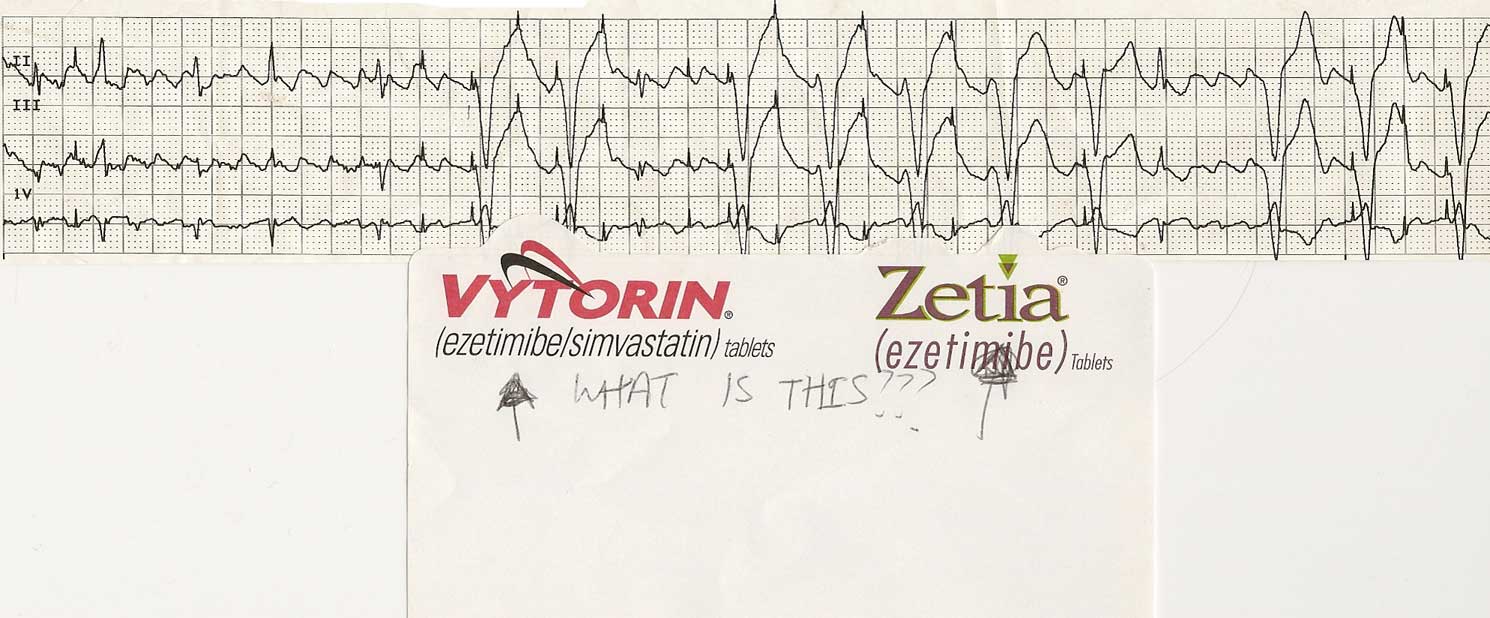
Click image to enlarge
She attached the post-it note asking "What is this?" and left it for my review. (I love it when new blog items appear on my desk.)
Anyway, other than an advertisement for Vytorin or Zetia, the question should be asked to the blog-o-sphere:
What is this?
-Wes
Monday, February 02, 2009
Doctors' Privacy Upheld
Today, the US Appellate Court shot down Consumer Checkbook's request for access to Medicare billing records:
Thank goodness the appeals court had the vision to not be swayed by marketing claims and overturned the earlier district court's ruling.
-Wes
Medicare billing records -- encompassing virtually every doctor's office -- are the mother lode of health-care data. Experts analyzing them can identify waste or poor quality care.I wonder who these "experts" are that claim they can identify waste and poor quality care from billing records: no written record, just diagnosis and procedure codes. They surely must be smoking something...
The nonprofit Consumers' Checkbook group had won a lower court decision to release the records. But a federal appeals court in Washington overturned it late Friday, saying doctors' privacy would be violated.
Thank goodness the appeals court had the vision to not be swayed by marketing claims and overturned the earlier district court's ruling.
-Wes
Sunday, February 01, 2009
Oops, He Did It Again
"Oops!Tom Daschle. Three years (2005-2007) consulting for $83,333 per month to InterMedia Advisors (yep, $1 million per year). A man who "works as a 'special public policy adviser' at the law firm Alston & Bird, advising clients on public policy related to financial services, health care, energy, telecommunications and (yes) taxes," according to their website. The man who reportedly wants to save our health care system and has written a book on the subject, since he's so well informed. A man with the "delicate mission of shepherding a health care bill through Congress at a time of punishing budget constraints" yet enjoys his personal drivers so much that he "forgets" what their worth and (oops) failed to pay taxes - three years running.
... I did it again.
I played with your heart.
Got lost in the game.
Oh, baby; baby.
Oops!
... You think I'm in love.
That I'm sent from above...
I'm not that innocent."
-Britney Spears
A man who somehow forgets what those tax laws say.
He's a man who wants a Federal Health Board:
Just as the Federal Reserve ensures certain standards, transparency and performance for our banking industry, the Fed Health would ensure harmonization across public programs of health-care protocols, benefits, and transparency.With Mr. Daschle's actions, I'm seeing the harmony between public programs and benefits, aren't you? But transparency? Hmmm. Seems Tom has a way to go:
Daschle reportedly waited nearly a month after being nominated to be secretary of health and human services before informing President Obama that he had not paid years of back taxes.Boy, if I was with Intermedia Advisors, I'd want my money back. Still, given the current climate encouraging government control of health care, it sounds like he'll be just perfect for the job as Secretary for Health and Human Services.
-Wes
Darvon Worthless?
I was at a social gathering Friday and met an experienced nurse from a local bone marrow transplant unit. She mentioned to me that an FDA panel had met and decided to recommend that Darvon (propoxyphene) be banned from the US market.
"Man, we use Darvon a lot," she said. "It's one of the few drugs we give for our patients that doesn't mask fever. Everyone in our unit gets Darvon. If we suppressed fever, we'd be much slower at recognizing infection in our unit."
The FDA panel made its decision based on some interesting testimony from Sidney Wolfe, MD from Public Citizen. His data were based largely on the Drug Abuse Warning Network (DAWN) that collects data from emergency rooms and medical examiners concerning drugs which have been determined to be related to emergency room visits or deaths. In that testimony, he claimed that 503 deaths were "related" to propoxyphene even though the data "do not imply causality but rather that the death was related to the drug." Note that only 25 of those deaths were classified as single drug. I wonder, was propoxyphene the causal agent in the other deaths? How many of these deaths was the drug actually prescribed to the deceased? Should death from suicide be classified the same as death from accidental poisoning?
Aron J. Hall, D.V.M., M.S.P.H., of the Centers for Disease Control and Prevention, Atlanta, and colleagues conducted a study to determine the risk characteristics and other factors associated with persons dying of unintentional pharmaceutical overdose in West Virginia in 2006. In their study, opioid analgesics were the most prevalent class of drugs, contributing to 93.2 percent of deaths; of these, only 44.4 percent included evidence of prescription documentation for all of the contributory opioids.
Now, compare this to the deaths from acetominophen (Tylenol) in whom more than 56,000 emergency room visits and an estimated 458 deaths from acute liver failure occurred in 2003. Should such similar data lead to acetominophen's removal from the US market, too?
Used properly, statistics can be powerful allies in supporting arguments during public policy decisions. But when those numbers are not couched beside their limitations or other confounding factors, they can misrepresent as well.
The implications of stopping a drug that has been available in the American medical pharmacopoeia for over fifty years should be carefully scrutinized. I can recall when isoproterenol (Isuprel) was discontinued due to the lack of a market - even though it's purely chronotropic (heart rate increasing) cardiac effects were vital to our electrophysiology studies. We quickly learned that our EP studies were markedly adversely affected. Fortunately, after significant outcry from our profession, the drug was reinstated.
As the nurse I met made apparent, some old drugs like Darvon may still have niche areas with distinct advantages and cost savings. These niche areas should be appreciated and recognized before wholesale withdrawal of any drug is mandated. Putting shoddy statistics in perspective might help assure proper public policy decisions are reached.
-Wes
"Man, we use Darvon a lot," she said. "It's one of the few drugs we give for our patients that doesn't mask fever. Everyone in our unit gets Darvon. If we suppressed fever, we'd be much slower at recognizing infection in our unit."
The FDA panel made its decision based on some interesting testimony from Sidney Wolfe, MD from Public Citizen. His data were based largely on the Drug Abuse Warning Network (DAWN) that collects data from emergency rooms and medical examiners concerning drugs which have been determined to be related to emergency room visits or deaths. In that testimony, he claimed that 503 deaths were "related" to propoxyphene even though the data "do not imply causality but rather that the death was related to the drug." Note that only 25 of those deaths were classified as single drug. I wonder, was propoxyphene the causal agent in the other deaths? How many of these deaths was the drug actually prescribed to the deceased? Should death from suicide be classified the same as death from accidental poisoning?
Aron J. Hall, D.V.M., M.S.P.H., of the Centers for Disease Control and Prevention, Atlanta, and colleagues conducted a study to determine the risk characteristics and other factors associated with persons dying of unintentional pharmaceutical overdose in West Virginia in 2006. In their study, opioid analgesics were the most prevalent class of drugs, contributing to 93.2 percent of deaths; of these, only 44.4 percent included evidence of prescription documentation for all of the contributory opioids.
Now, compare this to the deaths from acetominophen (Tylenol) in whom more than 56,000 emergency room visits and an estimated 458 deaths from acute liver failure occurred in 2003. Should such similar data lead to acetominophen's removal from the US market, too?
Used properly, statistics can be powerful allies in supporting arguments during public policy decisions. But when those numbers are not couched beside their limitations or other confounding factors, they can misrepresent as well.
The implications of stopping a drug that has been available in the American medical pharmacopoeia for over fifty years should be carefully scrutinized. I can recall when isoproterenol (Isuprel) was discontinued due to the lack of a market - even though it's purely chronotropic (heart rate increasing) cardiac effects were vital to our electrophysiology studies. We quickly learned that our EP studies were markedly adversely affected. Fortunately, after significant outcry from our profession, the drug was reinstated.
As the nurse I met made apparent, some old drugs like Darvon may still have niche areas with distinct advantages and cost savings. These niche areas should be appreciated and recognized before wholesale withdrawal of any drug is mandated. Putting shoddy statistics in perspective might help assure proper public policy decisions are reached.
-Wes