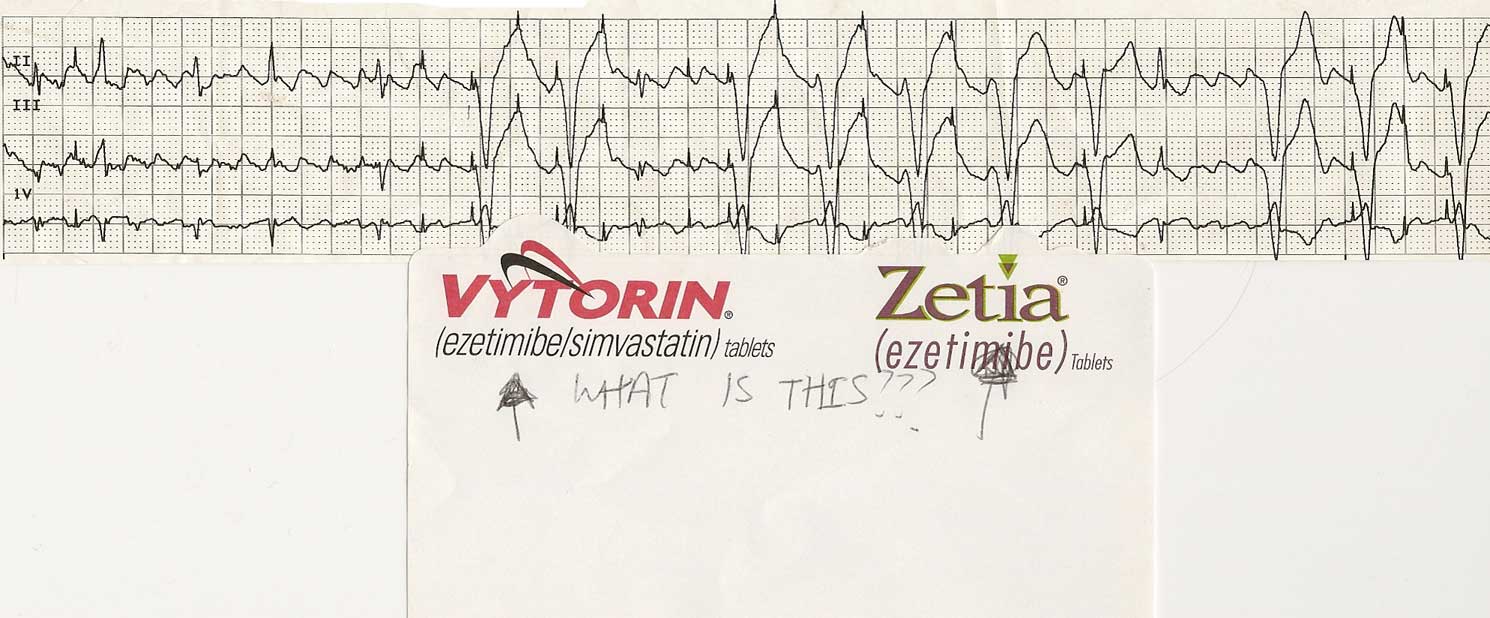
Click image to enlarge
She attached the post-it note asking "What is this?" and left it for my review. (I love it when new blog items appear on my desk.)
Anyway, other than an advertisement for Vytorin or Zetia, the question should be asked to the blog-o-sphere:
What is this?
-Wes
v lead oversensing with attempted atp (Atp capturing ever other beat)?
ReplyDeleteweird.
Underlying rhythm atrial flutter with 3:1 and 4:1 conduction, intermittent ventricular pacing. There are apparent pacer spikes inappropriately early in the t-waves of the paced beats, raising the suspicion of pacer malfunction.
ReplyDeleteBest I can do...
Cheers,
SF
How about oversensing of atrial flutter waves triggering an attempt at overdrive pacing?
ReplyDeleteI don’t know Guidant pacemakers and their quirks so this is a wild guess, but here goes:
ReplyDeleteIs the pacer tracking the flutter waves at an upper rate limit slightly slower than the flutter waves, with ventricular capture when the impulse falls outside the ventricular refractory period? (But who would program in such a high upper rate limit?). Or, is the pacer in an antitachycardia mode trying to pace the pt out of flutter and the electrode has dislodged and gone into the ventricle?
BTW some one needs to purge your institution of Evil Pharma influence before they end up on somebody’s black list. :-)
Love the attempts at figuring it out!
ReplyDeleteI'm going to go with atrail flutter with 3:1 conduction. Controlled rate. I see normal QRS which indicates to me that the patient has the ability for normal conduction. But I also see wide complex beats after a pacer spick. This would indicated to me ventricular pacing.
ReplyDeleteI see pacer spikes on the T wave which would indicate to me, that's not normal. Perhaps Q on T. I do not see atrial pacer spikes marching out which would indicate to me that perhaps the pacer spikes in the flutter waves are a V lead that isn't capturing.
That's my guess. Why? And I'm stickinig to it.
Now, why is this happening?
Because it can.
I suspect this type of tracing occurs on monitors around the country, but few stop to ask what's really happening when things like this are seen.
ReplyDeleteGranted, the underlying rhythm appears to be typical atrial flutter with variable AV conduction. In looking at this tracing, one should ask why there is no pacing on the left side of the strip, then pacing occurs. Hmmm.
A few hints: Medtronic's magnet rate on their pacemakers is usually 85 b/min, St. Jude's newer devices have a magnet rate "about" 98.5, and Guidant's magnet rates are generally 100 b/min (some good numbers to know, by the way). All pacemakers have a reed switch that is sensitive to magnetic fields and forces the pacemaker to pace asynchronously at a set rate, irrespective of the patient's underlying rhythm (i.e., VOO mode or DOO mode). The rate of pacing seen is used to determine when the pacemaker's battery might be nearing its end of life.
Now, does this help explain what might be happening here? What about those spikes?
The huge flutter wages are also interesting. Almost 1/2 the amplitude of the QRS complexes. Does the patient have congenital heart disease? Or mitral stenosis?
ReplyDelete*I suspect this type of tracing occurs on monitors around the country…*
ReplyDeleteMany monitoring systems have a pacer mode that amplifies pacer spikes. Sometimes when in the pacer mode monitors create these spikes artifactually when in fact they are not present. But, there seem to be too many ventricular complexes following pacer spikes to be coincidence.
Now you’ve told us Guidant’s normal magnet rate. What is the EOL magnet rate? Surely not 214, which is the rate at which these pacer spikes seem to be occurring.
I’m struggling.
RW-
ReplyDeleteNo need to struggle. You're closer than you think.
Thanks to all who gave this such a good effort.
Every day in hospitals across the country, patients with pacemakers have their pacemaker checked by technicians, doctors or support personnel to make sure the pacemaker is functioning properly. To perform this task, a wand is placed over the device and a telemetry link established between the interrogating computer and the pacemaker as communication with the pacemaker occurs. As you mentioned, RW, software in many telemtry systems support a feature that augments the pacing spike so it is more visible on the telemtry strip during pacing output. Unfortunately, this same feature can be confused by the telemetry communication between the pacemaker and the programmer as output from the pacemaker, thereby adding artifactual spikes on the telemtry strips.
Therefore, those spikes are created by the software (as artifact) when the telemetry link is established between the programmer and the pacemaker itself. As part of the initial pacing interrogation, the programmer causes the pacemaker to briefly demonstrate its "magnet mode" to measure battery life, forcing asynchronous pacing at 100 beats per minute. The occassional gaps in pacing capture are caused by the patient's intrinsic QRS complex rendering the ventricle refractory to capture (note the occassional narrow QRS complexes between the wide paced beats).
Now, that wasn't so bad, was it?
Hope this was helpful-
-Wes
Lord a mercy ...no fair for us third worlders!! I got the flutter and something ventricular going on but...pacemakers are still not a common ER occurence here and are found almost solely in our cardiology practices among a 20% of patients who might be able to afford them. So since I'm about to 'move up in the world', thx for this heads up!
ReplyDelete