Click image to enlarge
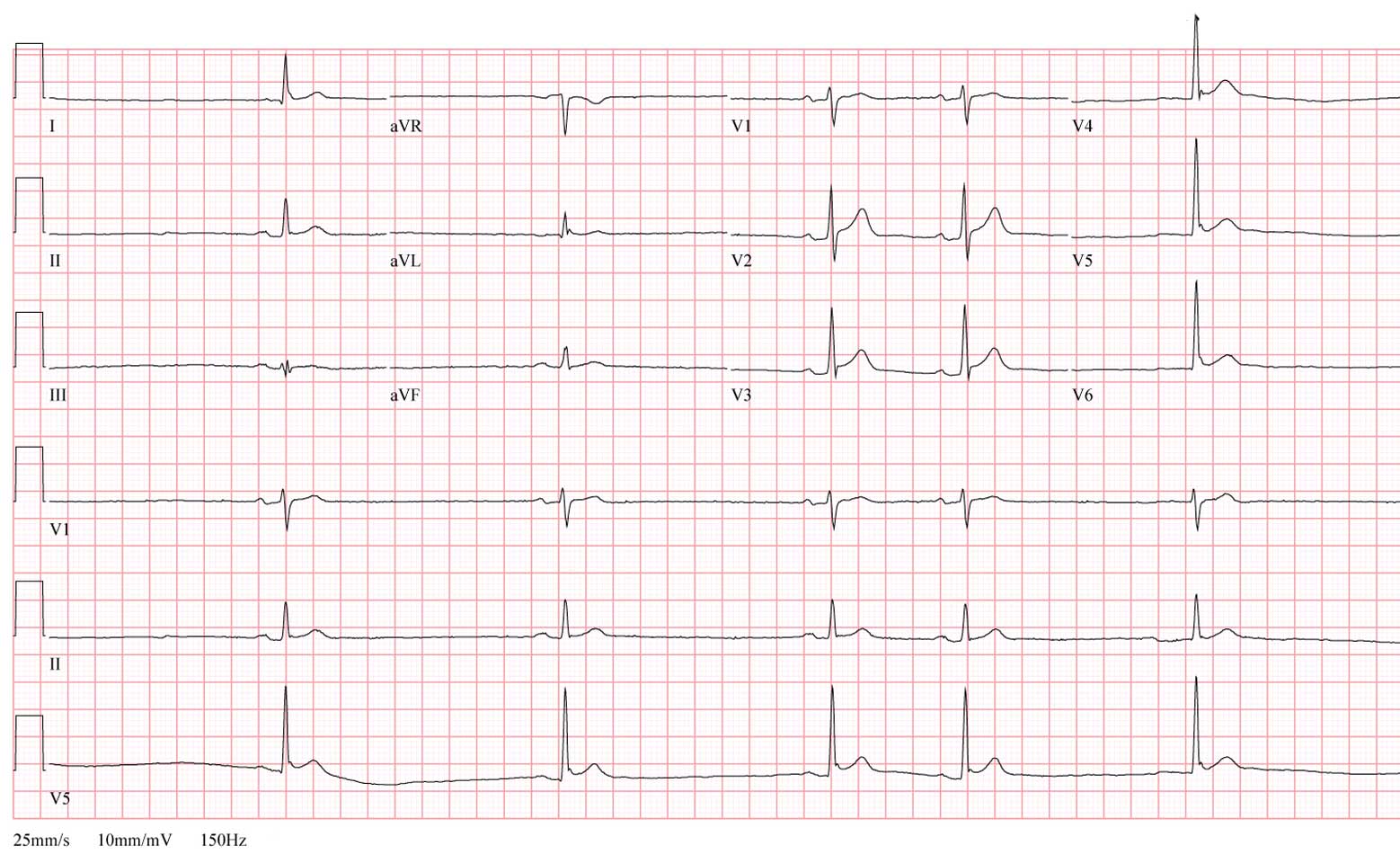
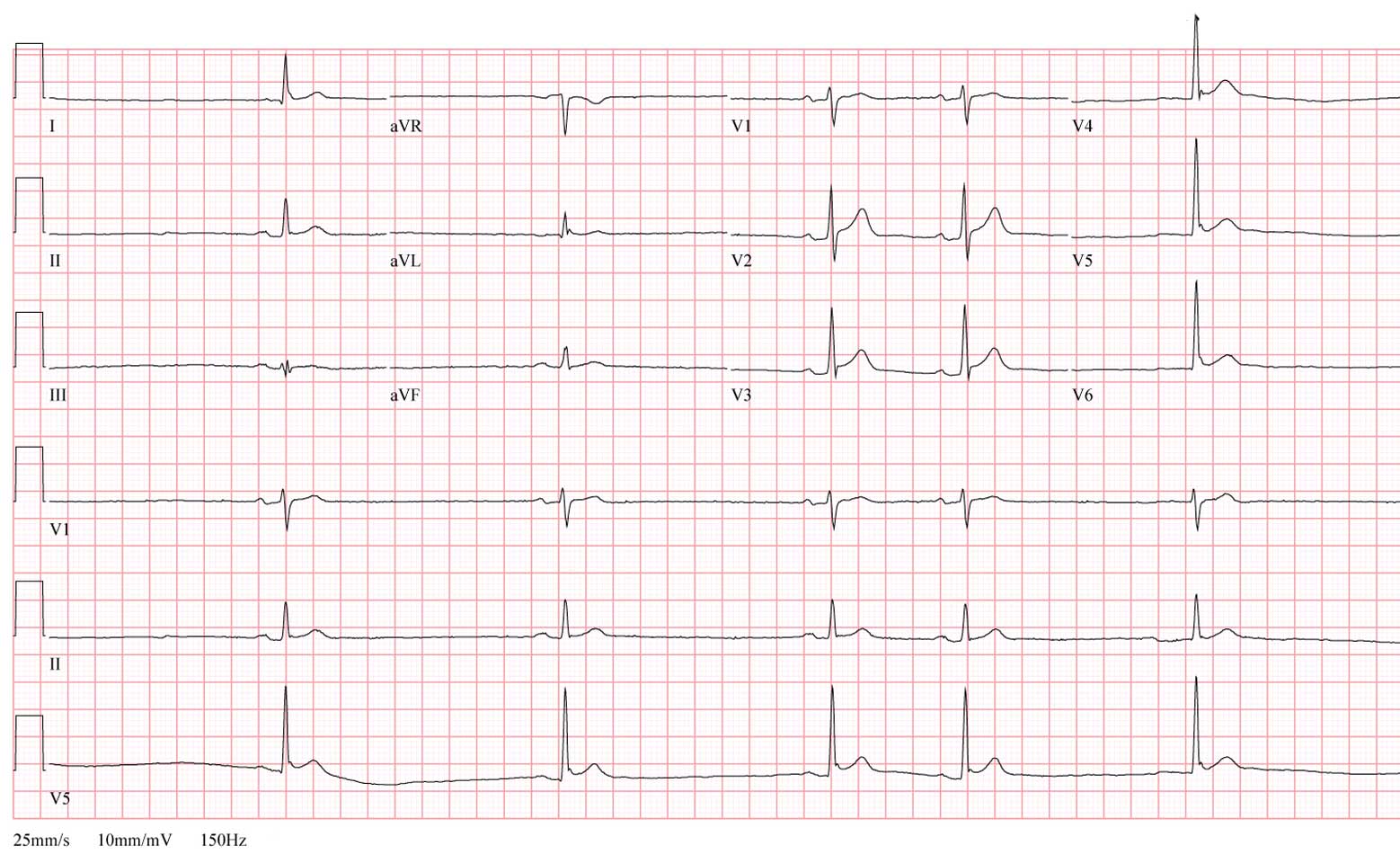
An astute observer glanced at the EKG and posed an important question to the ER staff.
What was the question?
-Wes
Addendum 18:45 CST - The EKG image was updated to permit better enlarged viewing.
Urine noted to be bloody without clots.No doubt patient identification or their room number, was sent to identify the patient (I'm not sure which). I suppose a record of the physician covering the trauma service that night is discoverable.
Text message sent to 2290 (trauma pager) about hematuria.
Patient denies any pain at this time.
I am thankful for the teenagers who are complaining about doing chores -- that means they are home and safe.And one other thought: be sure to visit Paul F. Levy's blog, Running a Hospital, to learn about the Engage With Grace program to how you can engage in a conversation with your loved ones about their (and your) end of life wishes.
... for homework. It means we live in a country where education is valued and encouraged for all.
... for the taxes I pay; it means I have income.
... for the mess that I have to clean up after parties, because it means I am surrounded by friends.
... for the clothes that fit a little 'too snug' because it means I have enough to eat.
... for the lawn to mow, windows to wash and gutters to clean; it means I have a home.
... for the parking spot I found at the far end of the parking lot, because it means I am capable of walking and am blessed with transportation.
... for my huge heating bill, because it means I am warm.
... for the person behind me in church that sings off key, because it means I can hear.
... for the pile of laundry and ironing, because it means I have clothes to wear.
... for all the complaining I hear about the government; it means we have freedom of speech.
... for the alarm that goes off early in the morning because it means that I am alive!Author unknown
One factor that could be driving larger increases locally: Blue Cross & Blue Shield of Illinois, which historically has used its dominant 50%-plus marketshare to undercut competitors' prices, has been more aggressive with rates this enrollment season, brokers say.Funny that when hospital systems coalesce and raise prices to remain "competetive," the FTC cries foul, but when the insurance industry does the same thing, the FTC can't be bothered.
"Blue Cross is the one company that is consistently coming in with higher renewal increases," says Rob Wilson, an insurance broker and president of Westmont-based Employco Group.
A Blue Cross spokeswoman declines to comment.
11:30 pm - Cackling though the overhead intercom system:Now:
“Code Blue, Three East, Room 236”
A thunderous herd of medical students, residents, anesthesiologists, cardiologists, social workers, security personnel descend on the scene. Arriving, the chief resident is in charge at the foot of the bed. IV’s have been started, some young well-muscled individual is bobbing up and down on the unseen’s chest, brow glistening with sweat, but focused. An anesthesiologist, noting the agonal rhythm, works to secure the airway, then a central line. Nurses administer drugs, bring line kits. Airway secured. “EKG? Where’s the EKG?” Electrode replaced. “Story? Who’s got the story?” Ten. Twenty. Thirty. The minutes pass. Finally, silence, as the monitors removed and the group departs. Like sound and fury, signifying nothing.
11:30 pm – The pager sounds:-Wes
* bleep bleep bleep *
A digital image appears on the screen: CODE BLUE, Room 2001
I was not on call, but I wondered, “Was this a patient of mine?” “Did I forget someone?” I raised my head from the pillow and strolled in to the accompanying room where my outdated computer sat and waited while it booted. “What might have happened?” “Is it someone old or young?” Thoughts spun just as the disk drive. Waiting. I typed by keyfob’s codes, I entered by password twice, I waited some more then the electronic medical record appeared and I checked the name next to the room number. For the first time, the number meant something: a person, 88 yrs old, yet someone I did not know. The scene appeared from miles away.
I sat back and perused the chart. Heart attack, conservative management, hypotension, fluid bolus given, then nothing more.
A few more keystrokes and the computer went black.
Then sleep came poorly once again.
The discrepancy between what Medicare pays and our cost of providing care acutely impacts the sustainability of our primary care practice. Medicare reimbursements do not cover our actual costs of providing care, and therefore we have recently had to make some difficult decisions that will impact the Arrowhead Family Medicine practice. Effective January 1, 2010, the physicians at Mayo Clinic Family Medicine - Arrowhead will opt out of participating in Medicare, meaning that Medicare will no longer reimburse for the services they provide....With the $500 billion dollars of cuts to Medicare spending in the new health care bills proposed, will we see more of this in more affluent areas?
 Early US Health Care Reform Photoshop Contest entries are available to view here. (I did the one at left - sorry, it's ineligible). There's still plenty of time to submit your entry. Entries will be still be accepted until 30 Nov 2009 at 23:59 pm CST!
Early US Health Care Reform Photoshop Contest entries are available to view here. (I did the one at left - sorry, it's ineligible). There's still plenty of time to submit your entry. Entries will be still be accepted until 30 Nov 2009 at 23:59 pm CST!... There are lots of features of the House Bill and that are already in the Senate bill that change that (the way doctors are paid). We are beginning to move away, particularly in Medicare, from traditional fee-for-service pay that I would suggest not only causes redundancy but doesn’t encourage innovative, high quality, low cost practices to moving toward a system that exists in pockets, exists in Mayos, Geisinger, (Inter-)Mountain Health Care. We know what it looks like. It isn’t how medicine is practiced it isn’t the the hospitals and providers are paid, so "bundled payments," "medical care homes," "accountable care organizations" – all buzzwords for really providing financial incentives and eventually financial penalties for appropriate medical protocols and appropriate outcomes - stopping the system now where one out of every five who’s released from the hospital is back in 30 days having never seen a health care provider, reducing or eliminating hospital-based infections, which are now one of the top 10 leading causes of death in America. We know exactly the system that can be done to stop it. It doesn’t take any capital investment It doesn’t require any new technology.”I wonder what she means by "... eventually financial penalties for appropriate medical protocols and appropriate outcomes?"
Banos said the Diagnostic Clinic cardiologists recently approached Good Shepherd "demanding hundreds of thousands of dollars in compensation from Good Shepherd for providing call coverage to the patients of Good Shepherd."Before condoning the cardiology groups' actions strictly on the basis of greed, we should note that there is a precedent for higher pay for employees working after hours in industry. Hospitals, too, have resorted to paying "nocturnists" (night-shift hospitalists) higher salaries than their daytime hospitalist counterparts as they struggle to find staff willing to work the night shift managing inpatients. These salaries are not covered strictly by funds received from the paltry Evaluation and Management payments paid by Medicare, rather, they are subsidized by the hospital system.
"This is in addition to whatever money they are able to bill and collect from patients and their insurance companies for the services they actually provide when they are called in to perform a procedure," Banos said in his e-mail to Good Shepherd employees.
Banos said he believes the demands for compensation were "veiled threats to move their elective procedures to Longview Regional if we did not pay." He added Good Shepherd's stand is that meeting the compensation demands would "not be fair to the many other physicians on our medical staff who selflessly and without any expectation of pay [from the hospital] provide call coverage to our patients each day as part of their commitment to the community."
"We cannot meet the needs of our community and pay doctors for doing something that they are already obligated to do as a part of their community obligation" Banos said.
Banos said he believes Longview Regional agreed to pay the cardiologists more than $300,000 a year for on-call coverage.
"We do not believe that it was by chance that it was only after this agreement was reached that these physicians touted Regional's 'commitment to quality care' and announced their 'choice' of Longview Regional for their patients." Banos said. "We knew that taking a stand could result in these physicians moving their elective cases to Longview Regional, and it did."





 If you'd like to help promote this contest on your blog by placing this tacky button on your sidebar, just copy the HTML in the textbox below and add it to the your blog's sidebar code:
If you'd like to help promote this contest on your blog by placing this tacky button on your sidebar, just copy the HTML in the textbox below and add it to the your blog's sidebar code:FDA is investigating energy levels in (automatic) external biphasic defibrillators (AEDs) with shocks ≤ 200 J. FDA has received reports of 14 events since 2006 in which a 200 J biphasic defibrillator was ineffective in providing defibrillation/cardioversion therapy to a patient, whereas a subsequent shock from a different 360 J biphasic defibrillator resulted in immediate defibrillation/cardioversion. The majority of events occurred during attempts at cardioversion of atrial fibrillation, but there was at least one instance with defibrillation of a ventricular arrhythmia as well. FDA is seeking additional information in order to interpret the significance of these events, and to determine whether FDA activities are advised.I haven't seen this, but others may have, so let 'em know.
Next week, I'll check into Mayo, one of the world's premier hospitals, to undergo additional treatment in preparation for receiving a new heart. Since my brain tumor turned out to be benign and my prostate cancer has responded to treatment, doctors there said those issues no longer should disqualify me as a candidate for a heart transplant.With the competetion for patients underway as the large health care system land-grab extends across state lines and overseas (See here and here), have the selection criteria for transplant patients remained a form of rationing or really become a form of marketing?
Now that I'm on the list, I am on an around-the-clock standby alert. I have to be ready to be on the operating table within four hours once a compatible heart becomes available. The fact that Chicago is 331 miles from Mayo, in Rochester, Minn., complicates things since I don't have my own charter jet. But the Mayo Med Air charter service could assist me if a commercial flight can't get me there quickly enough.
The challenge now is the wait. The heart I need will become available only when the donor is declared brain-dead and his heart can be taken from him and implanted in me within four hours. I am told the fact my blood type is B positive increases the chances of me getting a transplant quicker, though there are other patients ahead of me.
I had wanted it all to happen at the University of Chicago Medical Center, where world-renowned Dr. Valluvan Jeevanandam, who performed a triple-bypass on me in 2001, has done more than 1,000 transplants. But that hospital takes a more conservative approach to the fact my prostate cancer still is in remission. They wouldn't put me on the transplant list until I had been using an implanted heart pump ''for several years.''
Fortunately, the Mayo Clinic and Northwestern Memorial Hospital feel I have progressed enough in my recovery from the slow-growing prostate cancer to be eligible for a heart now.
In a statement, Costa said he succesfully negotiated funding for a UC Merced medical school.I love the last sentence: "... and he still has concerns about the cost of the bill."
"I am voting for HR 3962 because the choice of doing nothing was not an option. During my negotiations to help improve the bill for our Valley, I was able to achieve funding for a medical school in the Valley, with studies at UC Merced and residency in Fresno, as well as additional incentives to bring health professionals to our Valley. Increased funding in this bill for programs ranging from nurse training to health career opportunity programs to community health centers and increased reimbursement rates for low-paying Medicaid will go a long way in strengthening our health system in the Valley," Costa said.
The bill, HR 3962, passed the House of Representatives with a vote of 220-215.
Cardoza said the bill directs $167 million in health care funding to hospitals in his 18th district alone. The district includes parts of Fresno and Madera counties. But Cardoza said he still has concerns about the cost of the bill.

- Grant program for "community-based collaborative care"
(Seems this is really a grant to fund telemedicine programs and HL-7 hospital coding standards so computers can talk together. While ultimately this should be a good thing, the grant actually has little to do with collaboration of health care in the community right now.)- Grant program to develop infant mortality programs
(Why is more money needed when a department already exists for this?)- Grant program for reducing the student-to-school nurse ratio in primary and secondary schools
(Forget teachers, stick with nurses for schools I guess)- Grant program so "No Child is Left Unimmunized Against Influenza"
(And yet, I'm sure we'll soon have a Pay for Performance measure for that)- Grant program to implement medication therapy management services
(Once again, never mind this has already been done)- Grant program for community-based overweight and obesity prevention
(been there, done that, but it seems we can never get enough of this.)- Sec 2221 (pg 1246) Grant program for nurse-managed health centers
(APN's doing "primary care." Can't help wonder why the AMA loves this bill. Where's there support of what we do?)- Grant program to support demonstration programs that design and implement regionalized emergency care systems
(already being done in certain communities. The natural question is how much money is anticipated for the multitude of communities in need.)- Grant programs to prepare secondary school students for careers in health professions
(What ever happened to "Career Day?")- Grant programs for community prevention and wellness research (What is "wellness" anyway?)
- Grant program to promote positive health behaviors in underserved communities
(Sounds like attitude adjustment training: "Don't worry, be happy," I guess. Interesting that Senate Bill 319 already addresses this for women and children. Men, it seems, don't matter.)- Grant program for state access programs (These grants already exist, too!)
- Grant program for national independent monitor pilot program for skilled nursing facilities and nursing facilities
(What is this? An independent monitor to "oversee" large chains of skilled nursing facilities for some defined period of time. What about Medicare's Nursing Home Compare program?- Grant program for training in dentistry programs
Already exists- Grant programs for innovations in interdisciplinary care (Yep, got this in place already, too)
- Grant program for health insurance cooperatives
(Helpful cash for insurance interests- Grant program for wellness programs to small employers
(I can hear it now: "Don't drink, eat or smoke too much..." and place some nice posters on your wall...)- Grant program to disseminate best practices on implementing health workforce investment programs
(A bill already exists on the House floor: H.R. 2810)- Grant program for national health workforce online training
(looks like medical schools might be in trouble!)- Grant program for state alternative medical liability laws
(a grant to see if liability reform might work - fair enough - but will it change anything?)- Grant program for public health infrastructure
(um, don't we already have an Office of Public Health and Science?)
All of the planned means of tackling Stellan's SVT today during his ablation failed initially. Heart block was induced each and every time from each and every angle they tried to ablate. Dr. A and his team were left with little choice but to ablate Stellan's AV node in order to get rid of his accessory pathway. But before they did, one of Dr. A's colleagues threw out a wild idea.Certainly this case didn't "Get With the Guidelines" and might not be the approach most would take in this circumstance. Huge risk was involved for the pediatric electrophysiologist: a higher incidence of stroke for the child, unknown long-term affects to the aorta, a potential to injure the coronary arteries, and a large risk to one's professional career if anything went wrong.
"Let's try to go through his aorta."
Not in the plan. Not even in the possible or hypothetical plans. Not considered safe or feasible or wise on a 10 kilo baby. But with few options left before destroying Stellan's node, they decided to risk it.
To be honest, I'm glad I didn't know about it at the time.
So from his groin, they threaded the catheter up into his aorta, down into his atrium and through his valve toward his ventricle. From that angle, even though Dr. A said they were in the exact same spot as they'd tried ablating earlier, there was a money shot. He tried cryoablation. It started to zap his SVT with no heart block. So he tried a little more cryo. Again, no heart block.
So Dr. A pulled out the big dog. The radio frequency ablation catheter. His ultimate goal was to get 2 to 3 seconds of ablating done, even if it destroyed his node.
1 second. 2 seconds. 3, 4, 5.
From that angle, through the aorta, Stellan's AV node remained untouched.
Unbelievably, Dr. A was able to crank up the wattage and ablate Stellan's extra pathway for one solid minute before declaring his pathway dead on arrival.
And his AV node is as happy as the day is long.
 Meet the Eleven Eleven Campaign -- a nationwide campaign by BeyondTribute.org to change the way America honors its Veterans by hoping to raise $11 from 11 million Americans beginning (when else?) but November 11th.
Meet the Eleven Eleven Campaign -- a nationwide campaign by BeyondTribute.org to change the way America honors its Veterans by hoping to raise $11 from 11 million Americans beginning (when else?) but November 11th.Americans who do not maintain “acceptable health insurance coverage” and who choose not to pay the bill’s new individual mandate tax (generally 2.5% of income), are subject to numerous civil and criminal penalties, including criminal fines of up to $250,000 and imprisonment of up to five years.Is this what American's want, criminal penalties including jail time?
Cuts of the magnitude envisioned by Medicare, Holkins said, would present “a significant problem for the revenue side of our business model.”-Wes
The 14-physician practice, which has roughly 80 employees, has been independent since its founding in 1975.
So, Holkins said, the decision to affiliate was not taken lightly.
“I have really liked the idea of being independent,” he said. “But I also like to be able to pay our employees well and have enough left so our physician partners make a comparable salary to their peers in Kansas City, and I saw that as something I would not be able to do going forward.”
So what does it all add up to? The U.S. government is making a costly and open-ended commitment to help provide health coverage for the vast majority of its citizens. I support this commitment, and I think the federal government’s spending priorities should be altered to make it happen. But let’s not pretend that it isn’t a big deal, or that it will be self-financing, or that it will work out exactly as planned. It won’t.Regretably, this analysis is where we're heading: who cares what it costs, just enact it!
Many Democratic insiders know all this, or most of it. What is really unfolding, I suspect, is the scenario that many conservatives feared. The Obama Administration, like the Bush Administration before it (and many other Administrations before that) is creating a new entitlement program, which, once established, will be virtually impossible to rescind. At some point in the future, the fiscal consequences of the reform will have to be dealt with in a more meaningful way, but by then the principle of (near) universal coverage will be well established. Even a twenty-first-century Ronald Reagan will have great difficult overturning it.
Starting this month you can find these gift cards at any Winn Dixie and in November you can find them at CVS pharmacy stores.Just be sure you know when you're going to get sick!
There are two types of gift cards available. One is called "the blue health care card" It acts like a temporary health insurance. For $59.00 it gives you health insurance coverage for one to 2 1/2 months based on your age. Here's how it works. You buy the gift card at the store, and the person receiving the card activates it. Then they enroll in a variety of plans offered. After that, you'll receive a package in the mail with a member id card.
You can use the temporary insurance gift card to see a doctor, a dentist, at the pharmacy, or for lab work.
The other gift card is called the family blue discount card. It's $19.00 but unlike temporary insurance, this one gets you 3 months worth of discounts on dental, prescriptions and vision services.
"I am a pediatrician in suburban Cook County. We signed up to receive the vaccine, and have yet to get it. I hear it is going to go to local pharmacies before we get it. They only vaccinate children 9 and above. ... Who is going to ensure that infants and asthmatics get vaccinated?"The response from the Illionois Department of Public Health's spokeswoman Kelly Jakubek was telling:
"We currently are only placing orders for hospitals and health departments, which we consider the front line of health care," she said.It is difficult to know whether Dr. Morita bases her decision on places that have a high incidence of the disease (the frequency of development of a new illness in a population in a certain period of time), or a high prevalence (current number of people suffering from an illness in a given period of time). Pediatricians offices might have a high incidence, but very low prevalence, of flu relative to large chains stores, and if prevalence is what matters to the health department (and politically this would seem so), then pediatricians might be last in line for the shots.
Chicago vaccine providers are under a similar system in which the first shipments go to places that serve the most at risk, said Dr. Julie Morita, medical director of the Chicago Department of Public Health. Her department places the orders and selects the providers to get the first H1N1 vaccine shipments.
"Our priority is to get the early vaccine to high-risk providers," Morita said, "and once the majority have gotten vaccinated, then it can go to retail providers. We can't guarantee a limitless supply, so there may be breaks in supplies for a time, and then get orders filled later on."
"What is meaningful use?" asked executive director Sal Obfuscato at a recent SEEDIE executive retreat in Belize. "We believe the question is the answer, as man has always struggled to find meaning in this world."Heh.
This insight led SEEDIE to suggest that certified EHR vendors should embed quotes from well known philosophers in their applications. This approach will prompt physicians and other caregivers to actively seek meaning as they document patient encounters.
"When I am treating a patient, a thought-provoking quote from Jean Paul Sartre or Voltaire is far more valuable than the ability to e-prescribe or adhere to evidence-based guidelines," said Dr. Timothy Farragut, a Vermont pediatrician and SEEDIE board member. "You get so caught up in diagnosing a condition that you forget to ask yourself the important questions - why am I here, what does it all mean, can I still make my tee time?"
These recommendations are part of a SEEDIE effort to be designated as an ARRA certification body. "Unlike certification organizations that focus on subjective functional requirements, our innovative approach to meaningful use is focused on a much deeper meaning of the word meaning," said Obfuscato.
"If you're calling about an injectable insulin question, say 'insulin,' drug issue say, 'drug,' if not part of this list, say 'other,'...""Drug," I said. a brief pause occurred, then:
"Just a moment..." (Soft music played in the background.)Finally, a woman answered. he was quite pleasant as I explained the situation. Finally, I got to the part about the patient's drug not being on the 2010 drug list.
(Medicare payment) Reductions will be made over four years rather than imposed at once in 2010, the U.S. Centers for Medicare and Medicaid Services said yesterday in a statement. In July, the agency said it planned to slice $1.4 billion, or more than 10 percent, in payments for each of the two specialties, triggering what an advocate promised would be a “tooth and nail” battle.So while specialists won't be cut quite as bad, primary care will not see their efforts rewarded significantly either.
The administration argued that the lower reimbursements for specialists would make more dollars available for lower-paid non-specialists who can focus on preventing expensive, chronic illnesses. That would tame the growth in medical costs, one goal of President Barack Obama’s effort to remake the U.S. system of care. Under yesterday’s plan, family doctors and nurse practitioners would get half the proposed increase.