Sunday, May 30, 2010
Happy Memorial Day
Remembering our heroes:


Today at Camp Butler National Cemetery, Springfield, IL
Thursday, May 27, 2010
Tot Smoking: Sad But True
"Little Ardi Rizal has been puffing away since he was 18 months old, and is now up to two packs a day, his family said. The chain-smoking tot is reportedly so out of shape, he can only get around on a toy car."As doctors, we still have to pretend this is the sixth case like this we've seen, but it never gets any easier.
-Wes
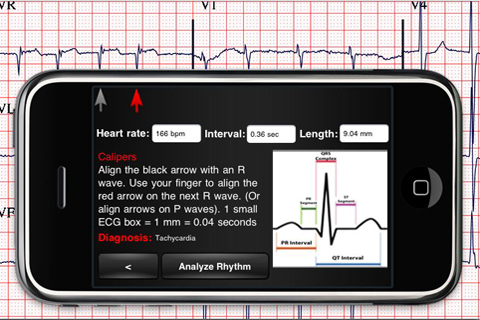
Whew! Echo Abnormalties Found!
I have been reading with interest the story from a Harlem (New York) Hospital covered in the New York Times about the discovery that 4000 echocardiograms were "lost" and left unread by a physician.
The outrage! The scandal! The fraud! The malpractice! Man, for newsprint, does it get any better than this?
But if we stop and think about it, unless doctor overreads of the interpretations made by skilled echo techs actually found errors on the initial interpretations made by the echo technicians, it might call into question the need for doctors to view echos that have been pre-screened by the technicians.
Thank goodness this morning that we learned that a few mistakes were found! Thank even more goodness that a nearly-retired renowned cardiologist was more than willing to step up to the plate and reaffirm the outrage:
We are very aware that nurse practitioners and nurse coordinators (whatever those are) have become the new model for health care delivery espoused by Washington to address the primary care crisis in America. After all, now that primary care has been thrown under the bus by our own physician leadership on the Hill to the point where mom-and-pop private practice offices are nearly extinct, we see the evolution to corporately-run health care. And corporately-run health care means shift work. This means working as employees. This means trying to maintain work/life balance. This means health care responsibility for patients can be offloaded on to groups of "health care providers," rather than a physician.
Why should echo technicians be any different in this new shared responsibility model of patient care?
The truth of the matter is that doctors are finding incentives to work like dogs at the expense of their personal lives are dwindling. Pay cuts are constantly threatened. Debt burdens for medical schools ridiculous. The truth of the matter is that we are about to add millions and millions of people to our health care system without increasing the doctor pool. And guess what? In inner city hospitals, the understaffed hospitals had to get resourceful and triage the work volume using technicians instead of doctors. The results were interesting:
If we're not going to insist on more doctors, we'd better study, and study carefully, the incidence of echo misreads (and their severity) in this first creative solution to our looming doctor shortage.
And guess what?
It might just save some money without affecting outcomes. That is, of course, if our liability system could make the same dramatic change.
-Wes
The outrage! The scandal! The fraud! The malpractice! Man, for newsprint, does it get any better than this?
But if we stop and think about it, unless doctor overreads of the interpretations made by skilled echo techs actually found errors on the initial interpretations made by the echo technicians, it might call into question the need for doctors to view echos that have been pre-screened by the technicians.
Thank goodness this morning that we learned that a few mistakes were found! Thank even more goodness that a nearly-retired renowned cardiologist was more than willing to step up to the plate and reaffirm the outrage:
Having 4,000 tests done and unread is unheard of, and is “unconscionable and unacceptable and malpractice as far as I’m concerned,” Dr. Douglas Zipes, a cardiologist at Indiana University Medical Center, past president of the American College of Cardiology and editor of HeartRhythm, said on Wednesday. “I can’t use more adjectives than that.”But before we dismiss this case nothing more than pure malpractice, we should ask ourselves if this might not be the health care model for our future.
We are very aware that nurse practitioners and nurse coordinators (whatever those are) have become the new model for health care delivery espoused by Washington to address the primary care crisis in America. After all, now that primary care has been thrown under the bus by our own physician leadership on the Hill to the point where mom-and-pop private practice offices are nearly extinct, we see the evolution to corporately-run health care. And corporately-run health care means shift work. This means working as employees. This means trying to maintain work/life balance. This means health care responsibility for patients can be offloaded on to groups of "health care providers," rather than a physician.
Why should echo technicians be any different in this new shared responsibility model of patient care?
The truth of the matter is that doctors are finding incentives to work like dogs at the expense of their personal lives are dwindling. Pay cuts are constantly threatened. Debt burdens for medical schools ridiculous. The truth of the matter is that we are about to add millions and millions of people to our health care system without increasing the doctor pool. And guess what? In inner city hospitals, the understaffed hospitals had to get resourceful and triage the work volume using technicians instead of doctors. The results were interesting:
Ana Marengo, a spokeswoman for the hospital system, the Health and Hospitals Corporation, said that despite the abnormal results, a cross-check of medical charts had not shown that anyone did not get needed treatment.Now I know people are ready to pounce on the hospital because insurers, states, and patients PAID for a doctor overread that was never forthcoming. But this is not my point. My point is that creative solutions to an overburdened health care system will require creative non-physician-directed solutions for health care going forward.
If we're not going to insist on more doctors, we'd better study, and study carefully, the incidence of echo misreads (and their severity) in this first creative solution to our looming doctor shortage.
And guess what?
It might just save some money without affecting outcomes. That is, of course, if our liability system could make the same dramatic change.
-Wes
Wednesday, May 26, 2010
How Cardiac Device Patients are Like Iron Man
From Salon.com:
-Wes
Iron Man's powers are generated from an implant designed to keep his weakened heart from failing. Of course, there are differences in our individual circumstances. Tony Stark, the man beneath the Iron Man armor, designed his own implant in an effort to save himself from a piece of shrapnel traveling to his heart. Not only that, he created the device using material provided by his unwitting captors (Asian Reds in the original "Tales of Suspense" comic; Middle Eastern terrorists in the movie). I am not nearly that clever; my device was built by Medtronic, a Minneapolis company that was started in a garage and is now the largest medical device company in the world. We have so much in common, and yet I have so many things to learn from him. Sure he's a little smoother in social situations, and better connected, yet at our core we share something rare. We are both cyborgs.Heh.
-Wes
Setting a New Standard
Increasingly, it looks like being triple-board certified in Internal Medicine, Cardiovascular Disease, and Cardiac Electrophysiology will no longer be enough to differentiate yourself amongst your colleagues since board certification is becoming a pre-requisite for employment at big medical centers.
Fortunately, there's still a way I can rise above the pack now that our new billing and coding scheme called ICD-10 is coming 1 October 2013. I just learned that I can earn my CCC™ credential:
And while this example is rather tongue-in-cheek, the real question as states move to mandate that doctors accept payment rates defined by insurers as a condition of licensure is this: will doctors be able to preserve the right to have a cash-only practice and still be able to obtain licensure? Certainly others have demonstrated that this cash-only model, devoid of bureaucratic overhead, is not only viable (video), but saves money.
In my view, this should be the fundamental political rallying point for all physicians and physicians' organizations, including the American Medical Association, as we move forward to sculpt our health care system of the future.
Anything less invalidates the fundamental tenets required to maintain the doctor-patient relationship.
-Wes
Fortunately, there's still a way I can rise above the pack now that our new billing and coding scheme called ICD-10 is coming 1 October 2013. I just learned that I can earn my CCC™ credential:
What are the benefits of a CCC™ credential?(And we wonder why health care costs as much as it does...)
- Distinguish yourself from your colleagues
- Earn up to 28% more than a noncertified coder (as revealed in the 2008 AAPC salary survey)
- Boost your career opportunities
- Fine-tune your cardiology coding knowledge to maximize your practice’s reimbursement
And while this example is rather tongue-in-cheek, the real question as states move to mandate that doctors accept payment rates defined by insurers as a condition of licensure is this: will doctors be able to preserve the right to have a cash-only practice and still be able to obtain licensure? Certainly others have demonstrated that this cash-only model, devoid of bureaucratic overhead, is not only viable (video), but saves money.
In my view, this should be the fundamental political rallying point for all physicians and physicians' organizations, including the American Medical Association, as we move forward to sculpt our health care system of the future.
Anything less invalidates the fundamental tenets required to maintain the doctor-patient relationship.
-Wes
Tuesday, May 25, 2010
In the Government, Does the Right Hand Ever Talk to the Left?
Pardon my cynicism, but with our health budgets looking a bit over-extended with the new health care reform bill that just passed, it is interesting that the Federal HOUSING Administration is approving HOSPITAL construction loans to the tune of $292 million:
I guess in the government's eyes, it's still better to stimulate the economy now so the youth of America can suck it up later.
After all, as the President said before:
-Wes
"FHA is helping to build state-of-the-art health care facilities like this all across the country," said FHA Commissioner David Stevens. "By helping to make these projects possible, FHA also contributes to the financial well-being of communities by creating jobs and helping to stimulate local economies."Hey, if it's not billions or trillions, I guess nobody minds, eh?
I guess in the government's eyes, it's still better to stimulate the economy now so the youth of America can suck it up later.
After all, as the President said before:
"... we must also address the crushing cost of health care. This is a cost that now causes a bankruptcy in America every thirty seconds. By the end of the year, it could cause 1.5 million Americans to lose their homes."Maybe those same people who are losing homes can now take up residence in our new FHA-funded hospitals.
-Wes
Grand Rounds Is Up
Grand Rounds, the best of this week's medical blog-o-sphere, is up over at 33 Charts.
Vanishing Oath Premiere A Success
 I would like to take a moment to thank the over 120 people who took time out from their busy schedules to attend the Chicago premiere of The Vanishing Oath at the Wilmette Theatre last evening. For many, it was the first time people they were exposed to the challenges that confront physicians daily in our current health care system.
I would like to take a moment to thank the over 120 people who took time out from their busy schedules to attend the Chicago premiere of The Vanishing Oath at the Wilmette Theatre last evening. For many, it was the first time people they were exposed to the challenges that confront physicians daily in our current health care system.Following the film, the audience (comprised of approximately 65% non-physicians) participated in a question and answer session with film's producer, Ms. Nancy Pando (pictured here with me following the show). The critiques and comments were invaluable to the film team as they work to engage more people in the efforts underway to protect the doctor-patient relationship. Working with Ms. Pando, I hope to assemble a short video clip of a few of people's impressions about the film in the days ahead.
For those interested, there will be a second showing of the film on the south side of Chicago tonight at the the Dorothy Menker Theatre, Moraine Valley Community College, 9000 West College Parkway, Palos Hills, IL from 7-9pm. Both Ms. Pando and the film's director, Ryan Flesher, MD, will be attending.
-Wes
Sunday, May 23, 2010
Damn Doctors
It was a lovely balmy early summer night: warm, low humidity and the bugs had yet to discover the temperature. A soft breeze blew and maple seeds spun gently down from the tree above propelled by the warm summer breeze. Like a hole in one, one landed in the pitcher of green tea on the table. We smiled. No one cared. After all, the chance to sit, relax and spend some time in idle conversation with your loved ones made the heaven-sent particulate matter floating on the surface of the tea seem appropriate. Still, my son couldn't stand it any longer and reached into the pitcher to snatch the seed from the tea's surface. Seeing this, I asked for another refill of tea and he was only too glad to ablidge, smiling.
Before long, it was time for her to return home, well before the sun set so that driving remained safe. It was our tacit agreement. Her cautious steps from our front porch reminded me that these moments were finite. My wife and I walked with her.
"Thanks for that wonderful dinner. It's so nice just to be here and listen to the kids adventures," she whispered. Her mind roamed and she focused on the task ahead. After all, she was heading back to her independent living facility with her Labrador in the back seat. She thought about her friends there. Her mind wandered back to our conversation about hosting the movie tomorrow night.
"You know, I hate the way everyone thinks doctors are just in it for the money. That's what all the seniors say, you know." She walked to the far side of the car. "I hate that."
She checked the back seat and saw that her Labrador had made herself comfortable, smiled toward me as she opened the car door, then sat behind the wheel. She waved with her fingertips as she put the transmission in drive, then shouted, "First, to Starbucks for a cup of Joe for the road." Off she went. Not bad for eighty-three, I thought.
I walked back to the house, pondering the words from my faithful familial reporter. My wife, who joined us and heard it all, said nothing. She knew I was thinking. I placed my arm around her shoulder and walked back to the house, wondering what I should write.
Nothing.
Better to say nothing.
Instead, an image came to mind: a nurse, holding a hermetically-sealed Tylenol tablet in an airtight wrapper labeled with a bar code. Her hand shooting a red light toward the wrapper from an apparatus resembling a 1950's TV ray gun attached to a mobile computer terminal with flat-panel display and mobile battery pack attached. A chirp. Keyboard pressed. Time logged. Record updated. The white pill dropped in a tiny plastic medicine cup.
Then the single $10-dollar Tylenol tablet is dispensed to an outstretched hand.
Who pays for all this ridiculous gee-wizardry all in the name of safety, profit and convenience?
Damn doctors.
-Wes
Before long, it was time for her to return home, well before the sun set so that driving remained safe. It was our tacit agreement. Her cautious steps from our front porch reminded me that these moments were finite. My wife and I walked with her.
"Thanks for that wonderful dinner. It's so nice just to be here and listen to the kids adventures," she whispered. Her mind roamed and she focused on the task ahead. After all, she was heading back to her independent living facility with her Labrador in the back seat. She thought about her friends there. Her mind wandered back to our conversation about hosting the movie tomorrow night.
"You know, I hate the way everyone thinks doctors are just in it for the money. That's what all the seniors say, you know." She walked to the far side of the car. "I hate that."
She checked the back seat and saw that her Labrador had made herself comfortable, smiled toward me as she opened the car door, then sat behind the wheel. She waved with her fingertips as she put the transmission in drive, then shouted, "First, to Starbucks for a cup of Joe for the road." Off she went. Not bad for eighty-three, I thought.
I walked back to the house, pondering the words from my faithful familial reporter. My wife, who joined us and heard it all, said nothing. She knew I was thinking. I placed my arm around her shoulder and walked back to the house, wondering what I should write.
Nothing.
Better to say nothing.
Instead, an image came to mind: a nurse, holding a hermetically-sealed Tylenol tablet in an airtight wrapper labeled with a bar code. Her hand shooting a red light toward the wrapper from an apparatus resembling a 1950's TV ray gun attached to a mobile computer terminal with flat-panel display and mobile battery pack attached. A chirp. Keyboard pressed. Time logged. Record updated. The white pill dropped in a tiny plastic medicine cup.
Then the single $10-dollar Tylenol tablet is dispensed to an outstretched hand.
Who pays for all this ridiculous gee-wizardry all in the name of safety, profit and convenience?
Damn doctors.
-Wes
Thursday, May 20, 2010
Tiny Camera Peeks Inside Coronary Arteries
For a better look inside coronary arteries comes Optical Coherence Tomography (video at link):
A brief review of a similar technology, intravascular ultrasound (IVUS), has demonstrated that it's not so easy to demonstrate improved outcomes in most routine cases:
-Wes
Optical Coherence Tomography, or OCT, approved by the FDA in April 2010, forms images by reflecting light inside blood vessels, which allows doctors to see 10 times more detail of an artery than the conventional ultrasound.Please note that this technology has been around since at least 2002. Is it really new? Or is it really that the company's news of FDA approval is "new?" More importantly, the million dollar question is not if it makes pretty pictures, but rather what does it add to the cost of the procedure and will it improve outcomes?
A brief review of a similar technology, intravascular ultrasound (IVUS), has demonstrated that it's not so easy to demonstrate improved outcomes in most routine cases:
In a systematic literature search (of articles on IVUS), 115 reviews, 10 health technology assessment reports, and 226 relevant primary studies, including 33 economic articles, were identified. 35 clinical and 3 economic studies met the inclusion criteria. In routine intervention with primary stenting, IVUS guidance did not show significant advantages. In specific clinical situations, IVUS information may indicate a change of therapeutic strategy that may benefit patients. Following heart transplantation, IVUS provides additional prognostic value compared to angiography alone. None of the economic analyses included long-term costs or effectiveness. However, after combining cost data with results from the effectiveness meta-analysis, the short-term cost-effectiveness ratio for IVUS-guided intervention was 7700 Euro per prevented major adverse cardiac event (MACE).Still, the image quality of OCT does appear to be substantially better than IVUS on first glance and it may open another door to our understanding of atherosclerosis.
-Wes
Tuesday, May 18, 2010
High Schools For Health Care
Yep, you read that right. The Chicago Public Schools, not exactly known for quality education, have a plan for training our future health care providers: high school:
Wow.
-Wes
Chicago Public Schools this fall will open the city's first high school specializing in health care, a move local hospitals hope will help relieve chronic workforce shortages.So this is what the Department of Labor had in mind for their health care education funds?
The school, which recently used a lottery system to enroll a freshman class of 160, will have a heavy emphasis on math and science. Juniors and seniors will be able to earn credits by shadowing hospital workers and interning as assistant nurses and in other professions.
Planners aim to prepare students for health- and science-related college programs and certify them for entry-level jobs in health care, such as pharmacy technicians or assistant physical therapists.
Wow.
-Wes
How We've Killed Clinical Research
- Blanche DuBois in Tennessee William's play,
A Streetcar Named Desire
Years ago when I began my medical training, I recall enrolling patients for clinical research. In cardiology, there were a myriad of questions that needed to be answered, especially in the area of defining which medications were best to limit the damage caused by a heart attack. Patients routinely participated in large, multi-center prospective randomized trials to answer these questions. It was routine for them not to charged for participating in the trial: the drug(s) and additional testing would be funded by the company whose drug was being studied. Patients enrolled willingly, eager to help advance science and perhaps, in some small way, their fellow man.
It never dawned on me in those early days why hospitals and research centers were so eager to promote research.
Like many things in our profession, research centers realized that these studies could make money. There are always additional expenses required to perform these studies and research centers wanted to make sure they were not left holding the "cost bag" for these trials, so they would pad their budgets for both the "direct costs" of performing the trial and a bit more for "indirect costs" that funded their offices and utilities and perhaps to offset the losses carried by other slow-to-enroll trials.
This strategy worked. Research centers, working earnestly, helped recruit patients by marketing their cutting edge researchers to the populous. Patients came in droves since there was no additional cost on their part to participate. Research centers got additional "indirect" funds from the drug companies to grow. More research was conducted, more patients recruited, and everyone benefited.
Until the costs of health care grew.
About 2001, research was getting expensive for companies. Back then, I noticed a subtle shift occur in the funding of clinical research by the medical device industry. I was involved in Medtronic's Insync trial that tested the first biventricular pacemaker for the treatment of heart failure. As a young electrophysiology researcher, I was stoked: this was exciting new and unproven territory for pacing therapy to venture.
But I remember how the Insync trial budget was formulated because it was quite different than I had remembered with other clinical trials. In this trial, part of the study was completely funded not by the company, but rather a portion of the trial was paid for by the patient's insurer. This was perfectly legal, we were told, since the large companies had to gain approval from our government via the FDA to allow such a payment strategy. Also, insurers were required to pay for clinically-indicated pacemakers. So, since dual chamber pacemakers were already approved for reimbursement by insurers and the "only" new portion of the implant procedure was the placement of a new left ventricular lead, the patient would not be charged for any of the new equipment, and their insurer would "only" be charged for a "regular" dual-chamber pacemaker (mind you, for a pacing therapy that was unproven at the time). Technically, patients still did not have to bear any additional cost of their involvement in the trial and everybody was happy. With this new trial budget strategy now firmly in place, we had, in effect, "relied on the kindness of strangers" (the patient's insurer) to help fund the company's research. No one seemed to notice this shift, and certainly no one minded, since everybody won: the patient got the device, the research center got paid, and the company, too, could even make a little money to offset their expenses in the process.
Naturally, there was a desire for research centers to recruit more and more trials to grow their prestige in the community. Small companies would use research protocols to gain marketshare in competetive hospital accounts using, in part, this patient-subsidized budget strategy. Worse, they would create new add-on trials only marginally relevant for the same growth strategy even after devices were FDA-approved.
Fast forward ten years to our current era.
With the growing cost of health care being offloaded by insurers on the backs of patients, patients have seen their insurance deductibles rise. Employers are finding they can no longer provide "Cadillac plans" to their employees due to costs, and instead move to insurance programs that are less encompassing in an effort to control costs to their employees. As a result, some patients even have "lifetime caps" limits on their insurance. Consequently, patients have become keenly aware of the costs of providing their health care.
I have noticed that patients are increasingly reluctant to participate in clinical research. Perhaps this is because they understand the relationship between ANY health care and THEIR expenses. They know that their insurers might not cover the experimental parts of research trials and are concerned that they'll be left holding the bag. After all, defining where the lines are drawn between what is paid for and what is not in clinical trials is nearly impossible with our current cloudy hospital billing schemes.
Peter Orsag, the White House budget director, has promised comparative effectiveness research will lead us to the promised land of health care cost containment. But given what I see, because patients are footing an increased portion of their health care tab already, do we really think enrolling patients in these trials will be easy going forward?
Reality always trumps the spin in Washington. Unless we see better transparency of costs from all of parties making money in clinical research, we'll never have the patients enrolled to bring any of these trials, comparative or not, to fruition.
-Wes
Monday, May 17, 2010
Wii: Now AHA-Approved - For A Price
Which one's approved by the American Heart Association:
-Wes
Bicycles?While I'm all for a healthy lifestyle, we should really ask ourselves if we're sending the right message. But then again, I guess it's okay to get money from our Heart Association logos as long as the money's not from a pharmaceutical company.No.Running shoes?No.Treadmills?No.
Fried rice?Yep. (Courtesy of the California Walnut Commission).Nintendo's Wii? Yep. (Courtesy of another $1.5 million promotional fee).
-Wes
What Health Reform Hath Brought
Looks like hospitals still see nothing but green pastures now that health reform has passed:
Never mind that the CBO has just reported that we're already $115 Billion over budget on the originally passed health care reform budget before we even get started.
-Wes
"As we push our envelope to take better care of patients, it will push other hospitals to do the same, and in the end patients will benefit," said Dr. Tom McRae, cardiologist and managing partner of Centennial Heart Center.I'm sorry, good doctor, but I wonder if we'll ever realize that this "build it, bigger, better and they will come" mentality will soon bite us all in the butt when the bill comes due. Sadly, they're not the only ones:
Other area hospitals have seen similar growth, pushing each to expand heart-care services. Tennessee has the sixth-highest rate of heart disease mortality in the country, according to the Centers for Disease Control and Prevention, which used 2006 data. (eds note: nothing like making projections on old data) About 233 people died for every 100,000 people.What me worry, right? It's so nice to reassure ourselves that such construction is in the best interest of our patients! Like Greece, it's always good to reassure ourselves that the health care spending party will never end.
Vanderbilt University Medical Center's Heart and Vascular Institute had 9,800 outpatient visits for cardiac care in 1998. Today, that number stands at about 80,000 outpatient visits among the main hospital, off-site clinics and 100 Oaks, said Dr. Keith Churchwell, executive director and chief medical officer. Vanderbilt also increased the number of cardiac critical care beds from 27 to more than 50 about six months ago. "Cardiology is an area of medicine that continues to evolve very quickly, and the types of rooms we built for procedures 10 years ago are too small to do what we want to do," Churchwell said. "We're constantly assessing."
Saint Thomas Health Service boasts 60 cardiac specialists between Saint Thomas and Baptist, and it has a network of 14 hospitals and 22 clinics in the Middle Tennessee and southern Kentucky regions. The heart patient population is only going to get bigger as the baby boomers enter their silver years, pushing the demand for services even higher, said Dr. Howard Walpole, chief of cardiac science for Saint Thomas Heart.
Never mind that the CBO has just reported that we're already $115 Billion over budget on the originally passed health care reform budget before we even get started.
-Wes
Sunday, May 16, 2010
The Case for Remote Medical Device Programming
With the recent reports of hacking ICD's, especially when a skilled set of engineers stand within six inches of the device, we can see the next Tom Clancy story line:
Not that security isn't important, it is. But should it be a show-stopper to innovation as we attempt to deliver care to our burgeoning patient population in the years ahead?
The reality on the ground is that doctors should have the ability to make adjustments to certain ICD programmed features remotely. The reality on the ground is that already we have non-medical personnel programming devices - even turning them off.
These devices need continuous follow-up, and a lot of it. For every device implanted, I would estimate that there are four times the number of patient visits made for these devices to a doctor's office that for patients without devices. Is this on-site follow-up burden sustainable? Currently, entire clinics are manned full-time by device nurses to manage the volume. Even with these clinics, devices must to reprogrammed at other times, like just before and after surgery, or de-activated when people reach the end of their life. With cost constraints limiting the number of personnel available for device management, we simply not have the number of individuals at all the geographic sites necessary to reprogram devices in person. So we've turned to industry representatives who hold no medical degree to make changes to programmed parameters on our behalf, many of which go undocumented. Physicians "oversee" these adjustments, of course (someone has to be legally responsible, right?), but the reality is is that people with medical degrees are not always the ones out there pushing the buttons.
This issue will only grow more dire as the baby boomers age and the number of devices continues to grow as we push to keep patients out of the hospital. For these reasons, and reasons of legal accountability, I foresee that the need for remote programming of devices will be all but inevitable.
And this isn't just for cardiac devices. Insulin pumps, neural stimulators, and a whole host of new innovative implantable devices will also need follow-up after their implantations.
Certainly, secure interlocks can be developed to assure safe remote reprogrammings - maybe even patient-and-physician hand-shake protocols, for instance. But in this era of increasingly wired health care delivery there should be no reason the FDA, in a brief moment of clarity, should discourage the development of carefully-developed protocols to modify device settings remotely.
What the heck are we waiting for?
-Wes
"A famous head of state, lounging in the comfort of his home, suddenly is afflicted with a series of shocks from his defibrillator, then collapses to the floor. His aides, uncertain what just happen, attempt to revive him, to no avail. Meanwhile, in a country far, far away, the terrorists are exchanging high fives..."These threats, as we can clearly see, are a Clear and Present Danger. (I know, not very original, but you get the drift.)
Not that security isn't important, it is. But should it be a show-stopper to innovation as we attempt to deliver care to our burgeoning patient population in the years ahead?
The reality on the ground is that doctors should have the ability to make adjustments to certain ICD programmed features remotely. The reality on the ground is that already we have non-medical personnel programming devices - even turning them off.
These devices need continuous follow-up, and a lot of it. For every device implanted, I would estimate that there are four times the number of patient visits made for these devices to a doctor's office that for patients without devices. Is this on-site follow-up burden sustainable? Currently, entire clinics are manned full-time by device nurses to manage the volume. Even with these clinics, devices must to reprogrammed at other times, like just before and after surgery, or de-activated when people reach the end of their life. With cost constraints limiting the number of personnel available for device management, we simply not have the number of individuals at all the geographic sites necessary to reprogram devices in person. So we've turned to industry representatives who hold no medical degree to make changes to programmed parameters on our behalf, many of which go undocumented. Physicians "oversee" these adjustments, of course (someone has to be legally responsible, right?), but the reality is is that people with medical degrees are not always the ones out there pushing the buttons.
This issue will only grow more dire as the baby boomers age and the number of devices continues to grow as we push to keep patients out of the hospital. For these reasons, and reasons of legal accountability, I foresee that the need for remote programming of devices will be all but inevitable.
And this isn't just for cardiac devices. Insulin pumps, neural stimulators, and a whole host of new innovative implantable devices will also need follow-up after their implantations.
Certainly, secure interlocks can be developed to assure safe remote reprogrammings - maybe even patient-and-physician hand-shake protocols, for instance. But in this era of increasingly wired health care delivery there should be no reason the FDA, in a brief moment of clarity, should discourage the development of carefully-developed protocols to modify device settings remotely.
What the heck are we waiting for?
-Wes
Thursday, May 13, 2010
Hauntings
02:30 AM: The beeper sounds.
A flash, then a clap of thunder outside.
"Your patient who you worked on a few days ago is here in the E.R...."
The mind races. You remember the case clearly. No problem at all. What could be going on? You ask twenty questions. You get twenty answers. All of the bases have been covered. "... doin' better now," your told. "We'll just admit 'em and you can see 'em in the morning." Hesitantly you return to bed, mind racing.
The lump of blankets next to you rolls over, "Everything okay?"
"Yeah," you lie. "Sorry, honey. Get back to bed."
The head meets the pillow but the brain does not. There are differentials to review. Seemingly infinite differentials. But it couldn't be that, they checked for that. What did I miss? Over and over again.
The thunder outside claps in unison with your mind. You wonder, maybe I should go in? What if they missed something?
The horror. The horror.
Over and over again. Maybe's. Doubting. Thunder.
Thirteen years into my trade and the hauntings, I've learned, are part of the job. Every doctor knows about the the 800-pound gorilla that watches us each day.
Sleep is his easy victim.
-Wes
Please call the ER x2222Why are they calling me? I'm not on call.
A flash, then a clap of thunder outside.
"Your patient who you worked on a few days ago is here in the E.R...."
The mind races. You remember the case clearly. No problem at all. What could be going on? You ask twenty questions. You get twenty answers. All of the bases have been covered. "... doin' better now," your told. "We'll just admit 'em and you can see 'em in the morning." Hesitantly you return to bed, mind racing.
The lump of blankets next to you rolls over, "Everything okay?"
"Yeah," you lie. "Sorry, honey. Get back to bed."
The head meets the pillow but the brain does not. There are differentials to review. Seemingly infinite differentials. But it couldn't be that, they checked for that. What did I miss? Over and over again.
The thunder outside claps in unison with your mind. You wonder, maybe I should go in? What if they missed something?
The horror. The horror.
Over and over again. Maybe's. Doubting. Thunder.
Thirteen years into my trade and the hauntings, I've learned, are part of the job. Every doctor knows about the the 800-pound gorilla that watches us each day.
Sleep is his easy victim.
-Wes
Wednesday, May 12, 2010
Barbara Walters Interviews Her Aortic Valve
Voiceover speaks in the background...
Tears welling...
"Yes.... yes, it is. I mean all these years opening and closing, opening and closing and just because I get a little stiff, this is the thanks I get. The prospect of some cow or pig thing doing what I've been doing for years.... It's devastating...."
"What will you do next?"
"I mean, that's just it! Don't you see? I'll just sent packing to some cold, silver kidney basin to the basement, only to be palpated and sampled, frozen and sectioned, while they get the benefit of anti-platelet agents. Then, God who knows what!?.... But I'll miss you Barbara..."
"Oh, A.V.!"
(A pause... Barabara herself grabs a Kleenex...)
"Seriously, thanks to you there'll be no more gradient, no more being pushed around. But I feel good knowing one thing..."
(Another pause)
"What's that, A.V.?"
(Blushing and turning away...)
"I know who will be your first guest on The View when you return in September!"
-Wes
"It has worked for years, tirelessly opening and closing. Now, saddled with the challenges of age, Barbara Walters spends a few comfortable moments interviewing her critically narrowed aortic valve, for what comes next...""So, A.V., this must be very hard for you, being replaced and all."
Tears welling...
"Yes.... yes, it is. I mean all these years opening and closing, opening and closing and just because I get a little stiff, this is the thanks I get. The prospect of some cow or pig thing doing what I've been doing for years.... It's devastating...."
"What will you do next?"
"I mean, that's just it! Don't you see? I'll just sent packing to some cold, silver kidney basin to the basement, only to be palpated and sampled, frozen and sectioned, while they get the benefit of anti-platelet agents. Then, God who knows what!?.... But I'll miss you Barbara..."
"Oh, A.V.!"
(A pause... Barabara herself grabs a Kleenex...)
"Seriously, thanks to you there'll be no more gradient, no more being pushed around. But I feel good knowing one thing..."
(Another pause)
"What's that, A.V.?"
(Blushing and turning away...)
"I know who will be your first guest on The View when you return in September!"
-Wes
Tuesday, May 11, 2010
The Vanishing Oath: Chicago Premiere Expands
Due to the overwhelming response to my review on the new physician-directed documentary, The Vanishing Oath, I have arranged for another public viewing in the Chicago metropolitan area on Monday, 24 May 2010 at 7pm at the intimate confines of the Wilmette Theatre in Wilmette, IL. Ms. Nancy Pando, producer of the film and resident of Boston, has graciously agreed to participate in a question/answer session immediately following the viewing. All proceeds from the evening will benefit the film's team and their fledgling production company, Crash Cart Productions, LLC. Tickets will be $10 each. Seating is limited to 182 seats.
Let's make it a full house.
For the first fifty seats, anyone interested in pre-purchasing tickets can send me an e-mail at wes - at - medtees dot com with your name and number of tickets requested (limit four per request) and I will send you an invoice for payment via Paypal - your tickets may be picked up at the Box Office that evening.
A second showing will also be held on the South suburbs on Tuesday, 25 May 2010 in Palos Hills, IL.
From their website:
Let's make it a full house.
For the first fifty seats, anyone interested in pre-purchasing tickets can send me an e-mail at wes - at - medtees dot com with your name and number of tickets requested (limit four per request) and I will send you an invoice for payment via Paypal - your tickets may be picked up at the Box Office that evening.
A second showing will also be held on the South suburbs on Tuesday, 25 May 2010 in Palos Hills, IL.
From their website:
About Crash Cart Productions, LLC-Wes
Crash Cart Productions, LLC creates some of the most insightful and thought-provoking films on the practice of health care in the United States. The primary mission of Crash Cart Productions is to educate viewers on crucial issues in health care, aiming to spur debate, take action and save lives.
Monday, May 10, 2010
Doctors Are Woefully Unprepared for Business
Never has there been a better example of the failure of cardiac electrophysiology training programs to teach the business of medicine to our fellows than this story of a cardiac electrophysiologist from Tennessee who opened his own practice, only to be later evicted when he couldn't pay his rent:
Evaluation and management billing codes will never support electrophysiologists in such a setting, since the majority of a cardiac electrophysiologist's revenue is generated from procedural volume. Payments from Medicare (our primary patient population) comes in two forms for care delivered to patients: (1) professional and (2)technical. Technical revenue provided from Medicare for our procedures is ten times the professional payment paid to doctors.
Hospitals know this, hence why I'm employed by one. Procedually-based doctors should know this before opening their own practices.
-Wes
h/t: The Medical Quack blog
Evaluation and management billing codes will never support electrophysiologists in such a setting, since the majority of a cardiac electrophysiologist's revenue is generated from procedural volume. Payments from Medicare (our primary patient population) comes in two forms for care delivered to patients: (1) professional and (2)technical. Technical revenue provided from Medicare for our procedures is ten times the professional payment paid to doctors.
Hospitals know this, hence why I'm employed by one. Procedually-based doctors should know this before opening their own practices.
-Wes
h/t: The Medical Quack blog
Sunday, May 09, 2010
The Vanishing Oath: A Review
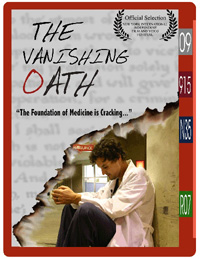 Yesterday, a much-anticipated package arrived in the mail containing a documentary film directed (and acted) by a young emergency room physician, Ryan Flesher, MD and produced by a former clinical social worker, Nancy Pando, LICSW entitled "The Vanishing Oath."
Yesterday, a much-anticipated package arrived in the mail containing a documentary film directed (and acted) by a young emergency room physician, Ryan Flesher, MD and produced by a former clinical social worker, Nancy Pando, LICSW entitled "The Vanishing Oath."As background, the film is a three-year project born in 2007 just before the great US health care reform debate began. Over 200 hours of interviews were conducted explore a simple question: why Dr. Flesher had grown to hate medicine.
It would have been easy for Dr. Flesher and Ms. Pando to make his story nothing but a rant, but instead, we find that their story is an honest attempt to understand how someone so enthusiastic at the start of their training could become so quickly discontented with the realities of emergency room care and our bloated health care delivery system.
To understand the origin of his disillusionment, we journey with Dr. Flesher and Ms. Pando as they return to interview people on the street, his family, fellow medical students, mentors, scholars, colleagues and plantiff's attorneys. They attempt to interview many of the many "vested interests" involved in our current health care system, including:
American Medical AssociationOf those that responded to their requests for an interview, all wanted to see the questions beforehand. Ultimately, none of them opted to go on record in the making of this film.
Many insurers, including Blue Cross, Aetna, Cigna
Three congressman
Six state representatives
Many hospital administrators and 11 Boston-area hospital CEO's
The Joint Commission
Dr. Groopman, author of "How Doctors Think,"
Ewe Reinhardt, medical economist
Regina Herzlinger, Author of "Who Killed Healthcare"
Press Ganey and
Five CEO's of major drug manufacturers.
The viewer is left to wonder why.
Still, they manage to gather a few insightful interviews from those with health care administrative backgrounds. More importantly, we quickly realize that Dr. Flesher is not alone. The same forces that shaped his discontent are revealed in fourth year medical students unsure what lies ahead for them and in the colleagues he turned to during fellowship training. We are introduced to a young aspiring hand surgeon who left (video clip) medicine after all of his years of training because of the toll it took on himself and his family. The footage is powerful. The people and emotions, real.
Suddenly, the viewer is confronted with the reality of how our health care system has grown to affect doctors. Worse, we realize what this might mean to each of us.
Additionally we see, firsthand, the effects that the fear of malpractice has on doctors and their behaviors. More to the point, we hear (video clip) from several doctors who had been sued and are even ushered into the office of an anonymous doctor in the midst of a suit at the time. Only later, and contained in a separate clip contained on the film's DVD, do we learn that the anonymous doctor interviewed was doctor Robert P. Lindeman, MD, the no-longer anonymous physician blogger former known as "Flea" as he was being tried in court just before he was unmasked on the stand by the prosecuting attorney. (A remarkably insightful follow-up interview with Dr. Lindeman a year and a half after his trial was settled is included on the film's DVD and is especially humbling. For instance, in the follow-up interview we learn that his medical malpractice rates increased 40% for the "settlement.")
In the end, we aren't quite sure if Dr. Flesher decides to return to medicine or not. You'll have to see the film to draw your own conclusion.
At times I felt the film leaned too heavily on the question of why doctors are unhappy at the expense of other critical health care issues. After all, not everything in medicine hinges upon whether doctors are unhappy or not, and that question is probably the least important to the public at large. Still, the issues of physician burnout and attrition, coupled with our ever-burgeoning health care bureaucracy and the loss of physician autonomy, will no doubt continue to affect the recruitment of future generations of physicians and perhaps the caliber of doctors in the future.
Nonetheless, both Dr. Flesher and Ms. Pando are to be congratulated for their bravery and fortitude at completing this documentary. It's a raw, unapologetic look behind the curtain of our current health care system from a physician's point of view. To my knowledge, this is the first time a doctor has used the creative venue of film to so vividly document the challenges we face.
Let's hope it's not the last.
-Wes
Disclaimer: I purchased the film for this review and have no conflicts of interest with the film team or production company.
Addendum: The film will be premiered in Chicago on 25 May 2010. Seating is limited.
Friday, May 07, 2010
Playing House, MD
From one of our local affiliate cardiologists:

Good thing he didn't store the medications in the refrigerator...
-Wes
h/t: Dr. Micah Eimer on Facebook (used with permission)
Addendum: From a follow-up e-mail:
"Btw in that drawer were two scripts for dig(oxin)- he was taking both explaining the visual changes and complete heart block."
A patient in the hospital told me he had a "drawer full of meds" at home but didn't know their names. I asked his wife to bring them in so we could look at them.
She did.

Good thing he didn't store the medications in the refrigerator...
-Wes
h/t: Dr. Micah Eimer on Facebook (used with permission)
Addendum: From a follow-up e-mail:
"Btw in that drawer were two scripts for dig(oxin)- he was taking both explaining the visual changes and complete heart block."
Thursday, May 06, 2010
Good Morning, Doctor
At Graduation: Remembering What Matters
Wednesday, May 05, 2010
Software Glitch Found in Medtronic's Latest Defibrillator Line
From 7thSpace:
More details as they become available...
-Wes
Addendum 7 May 2010 17:27PM: The Dear Doctor letter from Medtronic, posted today.
(Hong Kong) The Department of Health (DH) today (May 5) received notification from Medtronic International Limited (MIL), the local branch of a multi-national medical device manufacturer, that software problems in six of its implantable cardiac devices may risk life-threatening though rare malfunctioning. A DH spokesman said, the affected models are Consulta CRT-D (D234TRK), Secura DR/VR (D234DRG, D234VRC), Maximo II CRT-D (D284TRK) and Maximo II DR/VR (D284DRC, D284VRC).All except Maximo II VR (D284VRC) are distributed in Hong Kong. As of April 19 this year, the manufacturer has received five confirmed reports of defect out of approximately 144 000 devices sold worldwide.However, it is reassuring that no patient injury or death arising from the affected devices has been reported thus far.I called Medtronic technical support and they confirmed the issue. It appears they are not recommending any additional action on the part of patients be undertaken at this time since the problem is only caused if a rare sequence of events takes place. They are awaiting for FDA approval of a software fix for the problem can be upload during patients' next routine device follow-up to avoid the issue.
More details as they become available...
-Wes
Addendum 7 May 2010 17:27PM: The Dear Doctor letter from Medtronic, posted today.
Top Ten Reasons to Be a Doctor
With all the negative press, the pay cuts, the uncertainty of health care reform, I am approached by people who secretly whisper in my ear, "Would you have your child go in to medicine?"
On first blush, I am tempted to answer "Heck no!" given the administrative hassles, the changes in the public's perception of our profession, the front-load of education and the long hours involved. But those observations, while real, are at best superficial. Drilling down with more careful analysis after a challenging weekend on call, I find it worthwhile to stop and ask myself what makes medicine special for those of us crazy enough to subject ourselves to this lifestyle. I decided to put together a list of things that were important to me and would welcome additions to the list from others.
10. Independence - No matter what happens on the larger public policy and procedure scale with guidelines and mandates, when it comes to decisions regarding a patient's care, it will always be the one-on-one interaction between the patient and the doctor that will ultimately decide the best approach for care for an individual patient.
9. Respect - The title "Doctor of Medicine" still carries weight in our society. With that respect, however, comes significant moral imperatives to maintain that respect.
8. Flexibility - For those not adept at one-to-one interactions with people (hence, the clinical side of medicine), there are a myriad of opportunities opened with the MD or DO degree in public policy, research, the basic sciences, journalism, consulting, business, etc. It is this flexibility of options that are open to doctors that ensures job security.
7. Variety - I have been doing medicine a long time and have yet to see two days' activities or two patients that are the same. Ever. Bottom line: medicine is never boring.
6. Influence - Physicians matter. People know it. But you'd better be ready to be cornered at cocktail parties.
5. Reward - I cannot not think of anything superior to helping a fellow man or woman at a time when they are most vulnerable or in the greatest need. It also occassionally provides upgrades to first class when you help treat a syncopal patient on an airplane.
4. Trust - Like Smith Barney says, you have to "earn it," but once a patient's trust and confidence, it's the tie that binds. By virtue of your title, you are invited into the most secret parts of patients' lives to share their deepest concerns - a truly remarkable privilege. Corporate meetings never leave me with that feeling, if you get my drift.
3. Humility - Medicine will always keep you humble since there will never be a time when you can know it all or cure it all - ever. It's both the blessing and the curse of our profession: the learning never ends.
2. Fascination - Every day we work with the most amazing technology imaginable. The wonder of it all never ends: ask anyone who's ever reached in an abdomen to remove ischemic bowel, prescribed an antibiotic to cure a pneumonia, or ablated an tachycardia that affected someone their entire life and rendered it of historic interest only. Even something as simple as cutting the skin with the belly of a 15-blade scalpel while listening to the patient chat idly about their grandkids thanks to remarkable local anesthetics during a pacemaker implant, you are reminded of the amazing wonders of modern medicine every day.
1. Teamwork - Medicine is, by definition, a team sport. No physician can do what we do in isolation. Our "Club Med" has challenging pre-requisites, but once in, it is a vocation where we share collectively in the trials and tribulations of patient care. We win and we lose, together. Whether we are doctors, nurses, technicians, administrators, clerical staff, safety personnel or maintenance workers - each of us are constantly working for a common goal - the health and well-being of our patients - and when it works, nothing, I mean nothing, is as cool as that.
-Wes
On first blush, I am tempted to answer "Heck no!" given the administrative hassles, the changes in the public's perception of our profession, the front-load of education and the long hours involved. But those observations, while real, are at best superficial. Drilling down with more careful analysis after a challenging weekend on call, I find it worthwhile to stop and ask myself what makes medicine special for those of us crazy enough to subject ourselves to this lifestyle. I decided to put together a list of things that were important to me and would welcome additions to the list from others.
10. Independence - No matter what happens on the larger public policy and procedure scale with guidelines and mandates, when it comes to decisions regarding a patient's care, it will always be the one-on-one interaction between the patient and the doctor that will ultimately decide the best approach for care for an individual patient.
9. Respect - The title "Doctor of Medicine" still carries weight in our society. With that respect, however, comes significant moral imperatives to maintain that respect.
8. Flexibility - For those not adept at one-to-one interactions with people (hence, the clinical side of medicine), there are a myriad of opportunities opened with the MD or DO degree in public policy, research, the basic sciences, journalism, consulting, business, etc. It is this flexibility of options that are open to doctors that ensures job security.
7. Variety - I have been doing medicine a long time and have yet to see two days' activities or two patients that are the same. Ever. Bottom line: medicine is never boring.
6. Influence - Physicians matter. People know it. But you'd better be ready to be cornered at cocktail parties.
5. Reward - I cannot not think of anything superior to helping a fellow man or woman at a time when they are most vulnerable or in the greatest need. It also occassionally provides upgrades to first class when you help treat a syncopal patient on an airplane.
4. Trust - Like Smith Barney says, you have to "earn it," but once a patient's trust and confidence, it's the tie that binds. By virtue of your title, you are invited into the most secret parts of patients' lives to share their deepest concerns - a truly remarkable privilege. Corporate meetings never leave me with that feeling, if you get my drift.
3. Humility - Medicine will always keep you humble since there will never be a time when you can know it all or cure it all - ever. It's both the blessing and the curse of our profession: the learning never ends.
2. Fascination - Every day we work with the most amazing technology imaginable. The wonder of it all never ends: ask anyone who's ever reached in an abdomen to remove ischemic bowel, prescribed an antibiotic to cure a pneumonia, or ablated an tachycardia that affected someone their entire life and rendered it of historic interest only. Even something as simple as cutting the skin with the belly of a 15-blade scalpel while listening to the patient chat idly about their grandkids thanks to remarkable local anesthetics during a pacemaker implant, you are reminded of the amazing wonders of modern medicine every day.
1. Teamwork - Medicine is, by definition, a team sport. No physician can do what we do in isolation. Our "Club Med" has challenging pre-requisites, but once in, it is a vocation where we share collectively in the trials and tribulations of patient care. We win and we lose, together. Whether we are doctors, nurses, technicians, administrators, clerical staff, safety personnel or maintenance workers - each of us are constantly working for a common goal - the health and well-being of our patients - and when it works, nothing, I mean nothing, is as cool as that.
-Wes
Tuesday, May 04, 2010
How To Instill Confidence in the EMR
... just post the 1.24 million records that have been compromised online.
So don't worry, your health care records will be in the very best of hands.
-Wes
So don't worry, your health care records will be in the very best of hands.
-Wes
For Your Cardiology Powerpoint Presentations
Dress up your Powerpoint presentations with these animated Powerpoint templates.
Personally, I prefer a minimalist, less distracting approach with lots of real life pictures - unless I'm talking to administrators - they seem to like these nerdly backgrounds. But $30?
Nah. I'll keep it simple, stupid.
-Wes
Personally, I prefer a minimalist, less distracting approach with lots of real life pictures - unless I'm talking to administrators - they seem to like these nerdly backgrounds. But $30?
Nah. I'll keep it simple, stupid.
-Wes
By Referral: Grand Rounds
Grand Rounds, the best of the Medical Blog-o-sphere, is hosted this week by none other than the eight year old (blog), GruntDoc, and is suitably titled: The Non Narcissist, Non Personally Aggrandizing Edition.
(Be sure to check out the modifed pain scale faces at Hyperbole and a Half included in the selections.)
-Wes
(Be sure to check out the modifed pain scale faces at Hyperbole and a Half included in the selections.)
-Wes
Monday, May 03, 2010
When Drugs Become Extinct
Doctors are all familiar with marketing efforts to promote new drugs, but once the new drugs displace older drugs in the medical marketplace, who serves as advocates for the continued manufacture of older FDA-approved drugs?
In a short answer: no one.
For those of us dealing in cardiac arrhythmia management, this presents difficult challenges to patient care if people are unable to take the newer drugs due to side effects. These patients no longer have a fall-back option to turn to for medical therapy when the older drugs have become extinct on the marketplace.
Examples of antiarrhythmics that have reached extinction status in the US include many of our older antiarrhythmic drugs such as procainamide, mexilentine or quinaglute.
Take for instance a recent case: A older person with recurrent ventricular tachycardia and congestive heart failure and ICD implantation who has experienced several appropriate shocks for hemodynamically-significant ventricular tachycardia from their ICD. They were not in heart failure and had a consistent ideal body weight. Beta blocker medications have been maximized. This same person is pacemaker dependent and allergic to Amiodarone and iodine. Sotalol was not tolerated and dronedarone is contraindicated because of heart failure. Their creatinine clearance is 40. The patient was placed on mexilentine in the hospital and did well, only to find after discharge that no pharmacies could obtain the drug any longer. Oral procainamide, I have found, has suffered the same fate long ago. Few options remain: dofetilide as an inpatient?
Perhaps.
Still, the issue of drug extinction is a challenging one: not enough market to justify the drug's manufacture, yet still a rare patient out there who might need an older medication. Even generic drug manufacturers won't manufacture these niche drugs - there's just not enough of a market to justify their manufacture and the regulatory environment precludes a small start-up company from even trying to meet the very small demand.
I wish I had an answer to this conundrum. How do others handle this situation?
-Wes
In a short answer: no one.
For those of us dealing in cardiac arrhythmia management, this presents difficult challenges to patient care if people are unable to take the newer drugs due to side effects. These patients no longer have a fall-back option to turn to for medical therapy when the older drugs have become extinct on the marketplace.
Examples of antiarrhythmics that have reached extinction status in the US include many of our older antiarrhythmic drugs such as procainamide, mexilentine or quinaglute.
Take for instance a recent case: A older person with recurrent ventricular tachycardia and congestive heart failure and ICD implantation who has experienced several appropriate shocks for hemodynamically-significant ventricular tachycardia from their ICD. They were not in heart failure and had a consistent ideal body weight. Beta blocker medications have been maximized. This same person is pacemaker dependent and allergic to Amiodarone and iodine. Sotalol was not tolerated and dronedarone is contraindicated because of heart failure. Their creatinine clearance is 40. The patient was placed on mexilentine in the hospital and did well, only to find after discharge that no pharmacies could obtain the drug any longer. Oral procainamide, I have found, has suffered the same fate long ago. Few options remain: dofetilide as an inpatient?
Perhaps.
Still, the issue of drug extinction is a challenging one: not enough market to justify the drug's manufacture, yet still a rare patient out there who might need an older medication. Even generic drug manufacturers won't manufacture these niche drugs - there's just not enough of a market to justify their manufacture and the regulatory environment precludes a small start-up company from even trying to meet the very small demand.
I wish I had an answer to this conundrum. How do others handle this situation?
-Wes
Saturday, May 01, 2010
Garbage In, Garbage Out
The question came up at a recent meeting:
“How many atrial fibrillation ablations did I perform last year?”
It was a seemingly simple request. One that our vast array of computer technology and Electronic Medical Record should be able to conquer in a few microseconds.
So after an administrator talked to the responsible Information Technology officer and they searched and scanned the appropriate clinical and billing files, a day later came the answer:
Exactly one.
My swollen legs can attest to the inaccuracy of this result.
Yet with the speed of the hospital intranet, the results were broadcast as gospel in an e-mail to those who needed to know. Decisions were being made. Projections for upcoming years decided.
Which lead me to ponder the obvious.
How helpful will our electronic medical records be in supporting clinical care if doctors, rather than administrators and hospital information technology geniuses, cannot access and utilize clinically relevant data?
It’s the classic case of garbage in, garbage out.
But of course our policy wonks have already anticipated this criticism. They understand the health care records are, by and large, free text. They know that computers don't work well with the nuances of the written sentence. So to compensate for this short-coming, they have plans to implement the Mother of All Coding Schemes to permit more accurate data queries, licensed and sanctioned by the American Medical Association, called ICD-10®. Our government needs this scheme, it was argued, to determine if the government is getting an adequate return on their health care investment dollar.
ICD-10®, it is promised, will provide for unprecedented data queries of electronic data, housed in data silos so large that even they will be the envy of Google. Once these highly specific codes are used, we are told, we’ll really be able to forecast clinical trends, pricing trends, and define value-added components of our health care delivery in America. We will be able to determine which patients need our most urgent clinical interaction, purchase the equipment for that interaction in real-time, and assure it’s delivered “just-in-time” to the hospital loading dock, saving countless dollars.
So they say.
Sadly, real life gets in the way of such promises. We see this all the time in clinical medicine. “Mr. Jones, if you just stop smoking and take these medications …”, only to see Mr. Jones “forget.” Coding schemes are like this when applied to free text databases. The coded information is only as good as the people capable of classifying and sorting clinical care into pre-specified code bins accurately, and to date, there has never been a prospective evaluation to see if people really can achieve the promised results of this tactic. Which is why doctors will be the ones who will be required to either code the visit, under penalty of fraud if we're inaccurate, or teach others to code the visit with the same accuracy required to assure "accuracy." One only has to look at the labyrinthine nature of the new coding to see where it falls flat.
But there is other more ominous problem with the EMR data queries that goes far beyond the codes: the software that uses those codes. Hospitals and doctors, you see, don’t have access to the software. It’s owned by proprietary companies whose employees are already overworked to add the next bell and whistle to their software to stay ahead of the competition in the Great Race to become the great National Electronic Medical Record System sanctioned by Congress. No one really knows if the software is programmed correctly, they just assume it is. If a doctor takes issue with results reported by the Great EMR System using the World’s Most Powerful Coding Scheme, the hospital administration is rendered impotent by the need to ask, pretty please, Mr. EMR vendor if he could check their results. To which, of, course, the EMR vendor adds the request to their ever-growing queue of similar requests with promises like “well, we’ll work on it when we have time, but changing things would affect ALL of the hospitals with which we have contracts so we’ll determine if the request is important enough to pursue first.”
God forbid doctors be allowed to design and review their own clinically-relevant data queries.
So there you have it.
What they're calling "clinically-relevant health care data queries" in the era of our new Electronic Medical Records. Data queries decided by others in the name of the greater good yet often completely useless to those of us providing the clinical care, yet full of great hope and promise for a brighter health care future...
... at least until a more accurate coding scheme with greater clinical relevance called ICD-11® comes along.
-Wes
“How many atrial fibrillation ablations did I perform last year?”
It was a seemingly simple request. One that our vast array of computer technology and Electronic Medical Record should be able to conquer in a few microseconds.
So after an administrator talked to the responsible Information Technology officer and they searched and scanned the appropriate clinical and billing files, a day later came the answer:
Exactly one.
My swollen legs can attest to the inaccuracy of this result.
Yet with the speed of the hospital intranet, the results were broadcast as gospel in an e-mail to those who needed to know. Decisions were being made. Projections for upcoming years decided.
Which lead me to ponder the obvious.
How helpful will our electronic medical records be in supporting clinical care if doctors, rather than administrators and hospital information technology geniuses, cannot access and utilize clinically relevant data?
It’s the classic case of garbage in, garbage out.
But of course our policy wonks have already anticipated this criticism. They understand the health care records are, by and large, free text. They know that computers don't work well with the nuances of the written sentence. So to compensate for this short-coming, they have plans to implement the Mother of All Coding Schemes to permit more accurate data queries, licensed and sanctioned by the American Medical Association, called ICD-10®. Our government needs this scheme, it was argued, to determine if the government is getting an adequate return on their health care investment dollar.
ICD-10®, it is promised, will provide for unprecedented data queries of electronic data, housed in data silos so large that even they will be the envy of Google. Once these highly specific codes are used, we are told, we’ll really be able to forecast clinical trends, pricing trends, and define value-added components of our health care delivery in America. We will be able to determine which patients need our most urgent clinical interaction, purchase the equipment for that interaction in real-time, and assure it’s delivered “just-in-time” to the hospital loading dock, saving countless dollars.
So they say.
Sadly, real life gets in the way of such promises. We see this all the time in clinical medicine. “Mr. Jones, if you just stop smoking and take these medications …”, only to see Mr. Jones “forget.” Coding schemes are like this when applied to free text databases. The coded information is only as good as the people capable of classifying and sorting clinical care into pre-specified code bins accurately, and to date, there has never been a prospective evaluation to see if people really can achieve the promised results of this tactic. Which is why doctors will be the ones who will be required to either code the visit, under penalty of fraud if we're inaccurate, or teach others to code the visit with the same accuracy required to assure "accuracy." One only has to look at the labyrinthine nature of the new coding to see where it falls flat.
But there is other more ominous problem with the EMR data queries that goes far beyond the codes: the software that uses those codes. Hospitals and doctors, you see, don’t have access to the software. It’s owned by proprietary companies whose employees are already overworked to add the next bell and whistle to their software to stay ahead of the competition in the Great Race to become the great National Electronic Medical Record System sanctioned by Congress. No one really knows if the software is programmed correctly, they just assume it is. If a doctor takes issue with results reported by the Great EMR System using the World’s Most Powerful Coding Scheme, the hospital administration is rendered impotent by the need to ask, pretty please, Mr. EMR vendor if he could check their results. To which, of, course, the EMR vendor adds the request to their ever-growing queue of similar requests with promises like “well, we’ll work on it when we have time, but changing things would affect ALL of the hospitals with which we have contracts so we’ll determine if the request is important enough to pursue first.”
God forbid doctors be allowed to design and review their own clinically-relevant data queries.
So there you have it.
What they're calling "clinically-relevant health care data queries" in the era of our new Electronic Medical Records. Data queries decided by others in the name of the greater good yet often completely useless to those of us providing the clinical care, yet full of great hope and promise for a brighter health care future...
... at least until a more accurate coding scheme with greater clinical relevance called ICD-11® comes along.
-Wes