We had an interesting demonstration of a new application of an old technology today in our device clinic. A small company called Audicor, based out of Oregon and created by a spin-off of Hewlett- Packard engineers in 1999, began work on applying the old technology of phonocardiography (study of heart sounds - those low-pitched "lub-dub" sounds your heart makes when the valves in the heart close) to see if this might help optimize left ventricular (the left ventricle is the main pumping chamber of the heart) filling and ejection in patients with biventricular cardiac resynchronization devices used today to treat congestive heart failure.
I previously used echocardiography to perform this function, but it requires a capable technician, special lab time, access to an echo machine, etc. - in other words, it's more complicated to perform optimization using echocargiography. So we decided to check out this technology.
It uses two small electronic microphones with a gooey adhesive to block out peripheral noise that are placed over the standard lead locations of V3 and (about) V4 or V5. These sensors are shown:

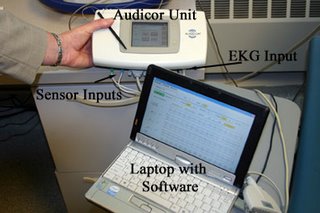
These sensors cost about $30 a set, are single use, but enough adhesive is applied so they can be moved about the chest to find the best sounds on a particular patient's chest. The connection setup looks like this:

These leads and sensors are then connected to the Audicor device that signal-averages the heart sounds and is driven by software from a laptop computer that can display (and store) the data from the Audicor device. Here's what that looks like:
The patients (but not the staff) needed to remain completely quiet during the acquisition of the sounds (yes snoring would screw up the data collection!). We tested this device on 8 patients today - 7 of whom had biventricular pacing devices, and one had a DDDR pacemaker, but had complained that he felt worse when his AV delay was shortened to a normal 'range' (180 msec) rather than left to conduct intrinsically with a 330 msec PR interval. A few caveats:
Advantages: Took about 15 minutes per patient, could be performed by a single operator, seemed to generate reproducible data (roughtly within 2-4% error per reading), and was relatively easy to use. It seemed to be surprizingly robust at determining maximium left ventricular systolic ejection time.
Limitations: Large breasts and hairy chests made recording of sounds difficult. Hair should probably be shaved, we found. Ventricular bigeminy made the use of the device impossible (it rejected readings appropriately) . Although they claim V-V timing (techical speak for doctors who understand this stuff) can be optimized in patients with atrial fibrillation, but I did not see this today. Most important, there are no patient outcome data available yet (that is, do patients really feel better if they have this done??), but I was surprised at the findings today and am encouraged to continue studying this. This might help us better understand the 30-percent "non-responders" who received biventricular devices - maybe we just haven't been programming the devices properly in some of those cases. And what happens to "optimization" as the heart function improves after long-term biventricular pacing?
Somehow, the simplicity and reproducibility of this device "sounds" like a good idea. We'll see...
--Wes
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.