As I work to complete my first 100 "MOC points" suddenly due 12/31/2018, I think my readers should be aware of the deceptive trade practices that have impacted me since I paid for the American Board of Internal Medicine's (ABIM) Maintenance of Certification® (MOC®) program in 2013.
First of all, after realizing my Board certification in Cardiovascular Diseases would expire in 2013, I paid for my Maintenance of Certification product to qualify to take my recertification examination in Cardiovascular Disease the Fall of 2013. At that time, I was subject to the ABIM's "double jeopardy" situation - if I did not pass my Cardiovascular Diseases re-certification, when it came time to re-certify in Cardiac Electrophysiology, it too would expire since the Cardiovascular Disease requirement was a pre-requisite for sitting for my Cardiac Electrophysiology re-certification examination. (This "double jeopardy" requirement was removed in 2015).
After paying for the ABIM MOC® product, this flier was sent to me explaining "Maintenance of Certification at a Glance."
On page 2 of the above flier, we can clearly see that I purchased the ABIM MOC® product that required only "100 points of Self-Evaluation of Medical Knowledge and Self-Evaluation of Practice Performance credit" to be in good standing with the ABIM for 10 years.
After completing the secure examination in the Fall of 2013, I received this letter on 22 January 2014 notifying me that I had passed the Cardiovascular Disease examination. It stated by Board certification "will remain valid until 2023." Also on that letter, I was told that "requirements to maintain certification will be changing in 2014."
Little did I know that after 2014 they would require twice as many MOC points (100 "points" every five years) to keep my time-limited ABIM board certification in good standing.
I did not agree to this change when I purchased my MOC® product from ABIM. As a result, I have now spent an additional $1675 purchasing continuing education modules from the American College of Cardiology to meet this new requirement.
While I am not an attorney, I believe changing these rules for the MOC® product that I had already purchased in 2013 from ABIM represents deceptive trade practices and will not rest until the ABMS MOC® product and its requirement for continuous certification (with its continuous payments to the ABMS member boards and their supporters) comes to an end.
-Wes
Sunday, December 30, 2018
Amazing Grace: On the ABMS Vision Commission's Draft Report
Amazing Grace, How sweet the sound
That saved a wretch like me
I once was lost, but now am found
T'was blind but now I see...
 |
| ABMS Vision Commission's Password-Protected "Draft" Report (Click image to enlarge) |
From the Terms contract for ABMS Board Certification available behind the ABIM physician portal firewall and not readily available to the public for inspection:
"I agree to indemnify, release, and hold harmless ABIM, its employees, officers, directors, members, agents, and those furnishing information about me to ABIM from any claims, liability, or damage by reason of any of their acts or omissions, done in good faith, in connection with: this application; information furnished to or by ABIM; the evaluation of my qualifications; ABIM examinations; the enforcement of ABIM's Policies and Procedures for Certification, and the policies for recertification outlined on ABIM's website, as well as all terms, conditions, and rules set forth in this website, as they may be amended from time to time; and any other action taken with respect to any certification or recertification granted by ABIM.
I understand that all ABIM materials are protected by the federal Copyright Act, 17 U.S.C. § 101, et seq. I further understand that ABIM examinations are trade secrets and are the property of ABIM. Access to all such materials, as further detailed below, is strictly conditioned upon agreement to abide by ABIM's rights under the Copyright Act and to maintain examination confidentiality.
I understand that ABIM examinations are confidential, in addition to being protected by federal copyright and trade secret laws. I agree that I will not copy, reproduce, adapt, disclose, solicit, use, review, consult or transmit ABIM examinations, in whole or in part, before or after taking my examination, by any means now known or hereafter invented. I further agree that I will not reconstruct examination content from memory, by dictation, or by any other means or otherwise discuss examination content with others. I further acknowledge that disclosure or any other use of ABIM examination content constitutes professional misconduct and may expose me to criminal as well as civil liability, and may also result in ABIM's imposition of penalties against me, including but not limited to, invalidation of examination results, exclusion from future examinations, suspension, revocation of certification, and other sanctions."
From the recently filed class-action anti-trust Complaint filed 6 December 2018 against the ABIM:
"2. This case is also about ABIM’s illegal creation and maintenance of its monopoly power in the market for maintenance of certification. ABIM is the monopoly supplier of initial certifications for internists. Beginning in or about 1990, ABIM used its monopoly position to create a second monopoly in the maintenance of certifications for internists. Since then ABIM has used various anti-competitive, exclusionary, and unlawful actions to promote MOC and prevent and limit the growth of competition from new providers of maintenance of certification for internists. ABIM’s conduct, including but not limited to tying and exclusive dealing, has harmed competition by preventing competition from others providing cheaper, less burdensome, and more innovative forms of maintenance of certification desired by internists.To suggest, even for a moment, that the ABMS's Vision Commission's Draft Report is fully transparent regarding the financial, corporate, and political conflicts that have embroiled MOC® from its inception, working physicians should understand that the "Vision Commission" is little more than a puppet for corporate interests. All the "public comment" in the world - especially when the draft is un-editable and proposes no action to end MOC® - makes a mockery (pun intended) of the entire "ABMS Vision Commission" process.
3. The tying product is ABIM’s initial board certification, which it sells to internists nationwide. ABIM sells initial certification services to physicians in internal medicine and twenty foundational subspecialties within the field of internal medicine. Many internists hold multiple ABIM certifications, purchasing initial certifications in both internal medicine and one or more additional subspecialties.
4. The tied product is MOC, ABIM’s maintenance of certification. ABIM has tied MOC to its initial certification. As described more fully below, to drive sales of MOC and to monopolize the market for maintenance of certification, ABIM has forced physicians to purchase MOC, charged inflated monopoly prices for MOC, and thwarted competition in the market for maintenance of certification.
5. Approximately one of every four physicians in the United States (including those practicing in fields other than internal medicine), or about 200,000 internists, have purchased initial ABIM certifications. ABIM has throughout the relevant period controlled approximately 100% of the market for initial certification of internists in the United States. Through its MOC program, ABIM has also controlled in excess of 95% of the market for maintenance of certification of internists. ABIM has unlawfully obtained and maintained its monopoly power in the market for maintenance of certification services for the anti-competitive purpose of requiring internists to purchase MOC and not deal with competing providers of maintenance of certification services.
6. Plaintiffs bring this Class Action to recover damages and injunctive and other equitable relief on behalf of all internists required by ABIM to purchase MOC to maintain their initial ABIM certifications."
The ABIM employs a medical director with close ties to Price Waterhouse Cooper (PwC), a fact not disclosed on his ABIM employment announcement in 2015. PwC is a network of firms in 158 countries, 721 locations, with 250,930 people that earned $37.7 billion in 2017 alone.
I believe PwC is working with ABMS to salvage MOC® - however it is ultimately branded. Why else would so many non-physicians with ties to insurance companies and other interests sit on the Commission, too? Even worse, we now see that the entire Draft Report is based on the same propaganda and "professionalism" definition that led to the MOC® controversy in the first place four years ago.
Given these realities, it becomes crystal clear that the Vision Commission's Draft Report is little more than 96-pages of unprofessional deception that is not working to end "continuous certification," but rather perpetuate it.
What, then, do the public's comments to the ABMS Vision Commission's Draft Report mean?
Nothing.
And Grace, my fears relieved
How precious did that grace appear
The hour I first believed
Through many dangers, toils and snares
We have already come.
T'was grace that brought us safe thus far
And grace will lead us home,
And grace will lead us home
Amazing grace, how sweet the sound
That saved a wretch like me
I once was lost but now am found
T'was blind but now I see
Was blind, but now I see.
-Wes
P.S. For those who still feel inclined to comment on the ABMS Vision Commission's Draft Report, please read the National Board of Physician and Surgeon's critique of the draft report that recommends "an immediate moratorium on several harmful components of MOC."
Personally, given the deceptive history of MOC® and the harms caused to physicians and their patients, I see no redeeming qualities to MOC® (or any other forms of "continuous certification" proposed by the ABMS and their member boards) whatsoever and believe the entire process should end immediately for the sake of our profession and our patients.
Sunday, December 23, 2018
The Maintenance of Certification Controversy 2018: The Year in Review
The American Board of Medical Specialties/American Board of Internal Medicine (ABMS/ABIM) Maintenance of Certification® (MOC) controversy continued unaffected in 2018 despite significant pushback from working physicians.
The pushback began in 2012 when one physician became frustrated with the arduous and needless re-certification process. After even more new requirements to time-limited certification were added in 2014, a full-blown civil war in medicine between the bureaucratic elite and working physicians began. It was December 2014 when the full extent of the controversy became apparent: "medical professionalism" defined by luxury condominiums complete with their chauffeur-driven Mercedes S-class town cars, spousal travel fees, high salaries, and undisclosed conflicts of the leadership of the member boards.
Never once in the history of time-limited certification were the potential harms of time-limited certification to working physicians considered or acknowledged.
Caught with their hands in working physicians' financial cookie jar, the ABIM issued an unprecedented mea culpa message in February 2015 to its physician membership, but instead of coming clean, the cover-up and tap dancing began in an attempt to preserve the money flow.
Recaps of the revelations and cover-up/pivoting of the process are included here:
2015: The Maintenance of Certification Controversy 2105: The Year in Review
2016: The ABMS/ABIM Controversy 2016: Year in Review
2017: The ABMS/ABIM MOC Controversy 2017: Year in Review
The 2018 summary of events are recapped below:
12 Jan 2018: Practicing Physicians of America (PPA) sponsors a national survey (questions asked here) of physician attitudes about maintenance of certification, including evaluating potential harms to physicians caused by the process.
27 Jan 2018: Psychology of MOC and the Gaslighting of America's Physicians discussed.
2 February 2018: The ABMS tries to quell physician unrest and forms a 'Vision Initiative' with medical specialty societies and state medical societies (among others) concerning MOC.
8 February 2018: The ABMS Vision Initiative Committee is announced and is laced with numerous non-physicians with many conflicts of interest.
15 Feb 2018: The self-selected ABMS Vision Initiative Committee launches their own survey of physician attitudes toward Maintenance of Certification but steers clear of assessing negative consequences of MOC on physicians.
25 Mar 2018: ABMS/ACP announce partnerships with medical specialty societies to keep the money flowing
6 April 2018: ABIM publishes its "how-to" video on the Knowledge Check-in program revealing its mechanics.
23 May 2018: After ABIM publishes its tax forms late, PPA announces GoFundMe crowdfunding effort effort to raise funds for a pre-litigation investigation into the ABIM and the ABIM Foundation's activities.
11 Jun 2018: Results of the PPA survey on MOC announced at the AMA House of Delegates meeting in Chicago.
28 June 2018: A critical review of the ABIM Knowledge Check-in option for Maintenance of Certification (video) is published questioning a physician's right to privacy.
2 Aug 2018: The Federation of State Licensing Boards tries to legislate away their liability.
26 Aug 2018: The ABMS releases the results of their survey on MOC and the results are similar to the survey sponsored by Practicing Physicians of America.
6 Sep 2018: A video reviewing the main PPA survey results on MOC from 7007 physicians is published.
7 Sep 2018: PPA's GoFundMe effort reaches its goal of $150,000.
14 Sep 2018: DOJ issues opinion on MOC, calling the program "anti-competitive."
25 Sep 2018: The ABMS and American Board of Urology offer their spin on the DOJ letter concerning MOC®.
1 Dec 2018: The ABIM Knowledge Check-In program crashes and hundreds of physicians are left in limbo.
6 December 2018: Four physicians sue the ABIM in a class action lawsuit representing over 100,000 physicians claiming anti-trust violations, among others.
10 December 2018: ABIM issues a statement concerning the suit on its blog promising that "the organization will vigorously defend itself, recognizing that doing so will consume resources far better dedicated to continuous improvement of its programs."
21 December 2018: The far-reaching implications of the antitrust suit reach across the pond.
It's been quite a ride. Here's to a productive New Year in 2019!
-Wes
Background
For those unfamiliar with this controversy, ABMS board certification of a US physicians was once a completely voluntary lifetime accolade physicians could elect to hold after they completed their residency. They paid to take a test created by a self-appointed "board" of academic physicians in their specialty - analogous to the legal bar examination - that "certified" they had a fund of knowledge acceptable to practice their trade. Physicians used this "board certification" as a marketing accolade with their peers to garner referrals from colleagues.
Prior to 1990, ABMS board certification was never required to practice medicine in any US state or territory. Rather, it was the responsibility of the accredited residency program to train doctors and document they had sufficient experience to enter the workforce as that specialist safely. State licensing agencies verified that training and stipulated that physicians earn "Continuing Medical Education" credits to remain current in their field to maintain their state licensure in good standing.
In the 1960's, seeing the financial struggles of older boards formed 30 years before that created the lifetime board certification accolade, the American Board of Family Medicine, a new ABMS member board, was created with a new financial model that proved to be very lucrative: time-limited certification. The ABFM would soon be rolling in cash, earning tens of millions of certification and re-certification fees annually. Not surprisingly, it was not long before all 24 ABMS member boards shifted their certification models to implement time-limited certification by 1990, arguing that doctors had an obligation to keep up in their field (and pay the boards recurrent fees to do so). By 2015, the physician board certification and recertification industry mushroom into a $5.7 billion a year bonanza for the academic elite and their industry colleagues with publishing priority in influential specialty medical journals while not disclosing their conflicts of interest.
The pushback began in 2012 when one physician became frustrated with the arduous and needless re-certification process. After even more new requirements to time-limited certification were added in 2014, a full-blown civil war in medicine between the bureaucratic elite and working physicians began. It was December 2014 when the full extent of the controversy became apparent: "medical professionalism" defined by luxury condominiums complete with their chauffeur-driven Mercedes S-class town cars, spousal travel fees, high salaries, and undisclosed conflicts of the leadership of the member boards.
Never once in the history of time-limited certification were the potential harms of time-limited certification to working physicians considered or acknowledged.
Caught with their hands in working physicians' financial cookie jar, the ABIM issued an unprecedented mea culpa message in February 2015 to its physician membership, but instead of coming clean, the cover-up and tap dancing began in an attempt to preserve the money flow.
Recaps of the revelations and cover-up/pivoting of the process are included here:
2015: The Maintenance of Certification Controversy 2105: The Year in Review
2016: The ABMS/ABIM Controversy 2016: Year in Review
2017: The ABMS/ABIM MOC Controversy 2017: Year in Review
The 2018 summary of events are recapped below:
* * *
12 Jan 2018: Practicing Physicians of America (PPA) sponsors a national survey (questions asked here) of physician attitudes about maintenance of certification, including evaluating potential harms to physicians caused by the process.
27 Jan 2018: Psychology of MOC and the Gaslighting of America's Physicians discussed.
2 February 2018: The ABMS tries to quell physician unrest and forms a 'Vision Initiative' with medical specialty societies and state medical societies (among others) concerning MOC.
8 February 2018: The ABMS Vision Initiative Committee is announced and is laced with numerous non-physicians with many conflicts of interest.
15 Feb 2018: The self-selected ABMS Vision Initiative Committee launches their own survey of physician attitudes toward Maintenance of Certification but steers clear of assessing negative consequences of MOC on physicians.
25 Mar 2018: ABMS/ACP announce partnerships with medical specialty societies to keep the money flowing
6 April 2018: ABIM publishes its "how-to" video on the Knowledge Check-in program revealing its mechanics.
23 May 2018: After ABIM publishes its tax forms late, PPA announces GoFundMe crowdfunding effort effort to raise funds for a pre-litigation investigation into the ABIM and the ABIM Foundation's activities.
11 Jun 2018: Results of the PPA survey on MOC announced at the AMA House of Delegates meeting in Chicago.
28 June 2018: A critical review of the ABIM Knowledge Check-in option for Maintenance of Certification (video) is published questioning a physician's right to privacy.
2 Aug 2018: The Federation of State Licensing Boards tries to legislate away their liability.
26 Aug 2018: The ABMS releases the results of their survey on MOC and the results are similar to the survey sponsored by Practicing Physicians of America.
6 Sep 2018: A video reviewing the main PPA survey results on MOC from 7007 physicians is published.
7 Sep 2018: PPA's GoFundMe effort reaches its goal of $150,000.
14 Sep 2018: DOJ issues opinion on MOC, calling the program "anti-competitive."
25 Sep 2018: The ABMS and American Board of Urology offer their spin on the DOJ letter concerning MOC®.
1 Dec 2018: The ABIM Knowledge Check-In program crashes and hundreds of physicians are left in limbo.
6 December 2018: Four physicians sue the ABIM in a class action lawsuit representing over 100,000 physicians claiming anti-trust violations, among others.
10 December 2018: ABIM issues a statement concerning the suit on its blog promising that "the organization will vigorously defend itself, recognizing that doing so will consume resources far better dedicated to continuous improvement of its programs."
21 December 2018: The far-reaching implications of the antitrust suit reach across the pond.
* * *
It's been quite a ride. Here's to a productive New Year in 2019!
-Wes
Sunday, December 16, 2018
Primum Non Nocere
Primum non nocere - latin for "first, to do no harm" - is a philosophy working physicians aspire to throughout their careers when caring for patients. It defines a bioethical baseline for physicians and should be their guiding light in clinical decision making throughout their careers. Unfortunately, as is too often the case when politics and power enter the picture, it is easy for physicians to fall prey to avarice and greed, placing their financial and political interests before their patients and physician colleagues.
Such is the case, in my opinion, with the bureaucratic ranks within the academic House of Medicine. Today, it is "pay to play" for hundreds of thousands of US physicians thanks to the American Board of Medical Specialties (ABMS)/American Board of Internal Medicine(ABIM)'s Maintenance of Certification (MOC) program.
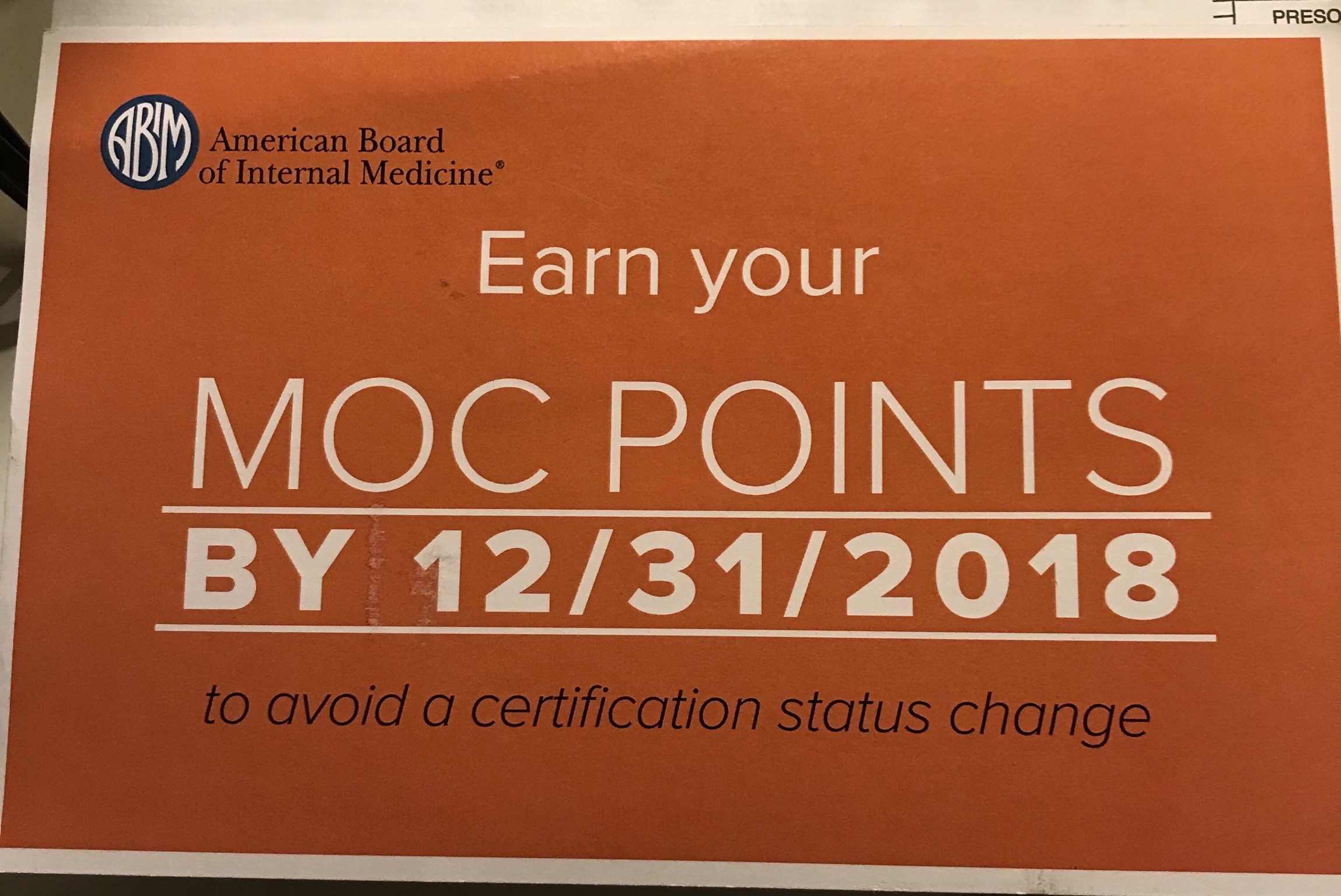
As I mentioned in an earlier blog post, I received a notice in late November of this year by US mail that I had to earn 100 Maintenance of Certification (MOC) points, or I could see a "change in my certification status." The ABIM webpage displays that notice prominently as well.
Recall that I certified in both Cardiac Electrophysiology and Cardiology with the 2013 testing cycle. At that time, according to the ABIM's website and this archived webpage from January 18th, 2013, MOC required that I perform 100 MOC points every 10 years. When I purchased MOC and registered to take my recertification test in October 2013, this is what I thought I was purchasing.
Now I find the ABIM has changed the rules. Now we must perform 100 MOC points every 5 years.
Needless to say, I had only 10 MOC points when I received that notice from the ABIM after the Thanksgiving holiday. I had vowed not the earn another point until it might be needed 10 years from the data I enrolled for my MOC exam and have been working to end MOC through conventional channels since that time. I have talks at the AMA House of Delegates, Ohio Health committee, and help with the Texas anti-MOC legislation as proof of that effort. One guy doesn't stand a chance, I learned.
Still, I became worried about the implications of now needing another 100 MOC points and the time, focus, and commitment required so I could keep seeing patients. I searched for ways I could fulfill my requirements without paying the ABIM another dime.
This is where things got interesting.
It seems I pre-paid for "30 MOC points" - one for a 2017-2019 Hospitalist Update, a 2017-2019 Internal Medicine Update, and a "Care for the Underserved" module that offered 10 MOC points. (The other offerings that might have been there before had "expired.") These thirty points wouldn't be enough to get me where I needed to be by 21/31/2018. Furthermore, learning about these non-applicable topics to my specialty seemed to be a waste of time. Still, I needed points, so I did what I could and even performed the Hospitalist update. I was surprised to find that the ABIM's own Robert Wachter, MD, "Mr. Hospitalist" himself, helped author this module. Because it was outside my wheelhouse, that module took way too long to successfully complete, but I finally did it to earn my "points."
Nothing to see here folks...
I was getting concerned. I checked the Heart Rhythm Society's webpage hoping they would have a module closer to my specialty that I could complete quickly and was surprised to find that they could only offer me 6.75 MOC points if I purchased a $650 Medical Knowledge update in Electrophysiology - a cost of $96.30 per MOC point! That was an astronomical price per MOC point and one that wouldn't get me anywhere near my goal of 100 total points.
I moved on.
The ABIM site suggested I look at the various offerings provided by the ACCME at http://www.cmefinder.org - a horribly rudimentary website that had poor filtering capabilities for the offerings I might need. They sent me to this hospital system and that hospital system with ways to game the system, but nothing would work for me or each offering gave me 0.5 to 1 MOC point each. Everyone, it seemed, were more than happy to offer a point here or a point there, but every point required a post-MOC survey of how I liked it, it the exercise was free from commercial bias, etc. - all very time-consuming - so I kept looking.
I turned to the American College of Cardiology's website since I am a Fellow of the American College of Cardiology and looked at their MOC offerings. I still needed a LOT of points if I was to make 100 by 12/31/2018. That's when it struck me: this was the plan! Whether you're an ACC member or not, you've got to pay the Man.
There, on the ACC's MOC webpage was this offering: ACC Self Assessment Program 9 (ACCSAP9) for $1600 in return for 155 potential MOC points good through mid-2019, a bargain-basement price of $10.32 per MOC point!
Left with few options this late in the do-or-die MOC extortion game to keep my hospital privileges and insurance payments coming, I purchased ACCSAP-9.
Before I could get started, I had to agree to a "Credit Agreement." In that agreement I had to agree to "read all text, watch all presentations and answer all questions within the topic for which you claim credit. You must obtain 70% or better on the questions, but you may answer the questions as many times as necessary to achieve that score."
Please.
Then there was the indemnify and hold harmless "Disclaimer" clause of the Credit Agreement: "The American College of Cardiology is not responsible for the results obtained from the use of the information contained in this publication... The American College of Cardiology does not warrant the information contained herein is in every way accurate or complete, and disclaim all responsibility."
Ahem, isn't this WHY we're being forced into this expensive exercise? If I can't rely on them to assure patient and "the public's" safety, what good are these "Knowledge Assessments" for patients?
Having no choice but to "agree" to their terms, lest I lose my hospital privileges and insurance payments to my hospital on 1 Jan 2019, I reluctantly clicked "I agree" and started the arrhythmia section of the testing the week before Christmas.
My wife and kids were not pleased.
"Dad, be here now. It's Christmas! Here you are, 35 years of experience, doing these mindless exercises and getting all stressed out. Haven't you done this long enough?"
"Honey, it's always me doing everything for Christmas while you get all stressed out and have to sit at that damn computer, doing quizzes. Will it ever end? How many years has it been?"
I realize that they are right. Years of being Mr. Good Guy while they lost out on their father. Experience means nothing to the ABMS. Money is everything with MOC. It is clear to me now that the "lifelong" educational system for physicians is horribly broken - a once reasonable voluntary system of continuing medical education required for state licensure, has morphed to an do-or-die extortion scheme for doctors' money. It's not about the patients or the doctor. These organizations indemnify themselves of this responsibility. It's just about the money.
And for hospitals and insurers, it's about control of the doctors to keep their profits high.
The ACC - our cardiovascular specialty society that looks more and more like the AMA, has found a way to get rich - very rich - using the threat of my loss of privileges to fund their organization via the ABIM's MOC program. No wonder they collaborate.
The American College of Physicians (ACP) has their Medical Knowledge Self-Assessment Program (MKSAP) likely does the same thing. So does the American Board of Pediatrics. Whether the ABMS member board is a "continuous certification" or MOC participant, the ABMS mothership keeps the money flowing to all of these entities who claim to educate using computer products while hiding behind "Disclaimers" that relinquish their responsibility.
Buying a product in 2013 thinking one thing, only to find it's another, is fraud as far as I'm concerned. Doctors like me don't like being swindled and forced to play games that have no meaning so they can keep providing patient care. There simply are not enough hours in the day for any of us to put up with these shenanigans required by the members of the Accreditation Council for Graduate Medical Education (like the ABMS) for their financial benefit. They are not only hurting doctors, but hurting their families at Christmas time, too. The ACGME members and ABMS Vision Commission should each carefully read how the ABMS MOC program has harmed doctors in this latest serious anti-trust Complaint filed in federal court against the American Board of Internal Medicine.
The "ABMS Vision Commission's" Draft Report fails to disclose these potential harms caused to physicians by MOC and its numerous conflicts of interest. Do they really think their assets will indemnify them of their responsibility to the well-being of working US physicians, and in turn, their patients?
I think not.
Primum non nocere.
-Wes
Such is the case, in my opinion, with the bureaucratic ranks within the academic House of Medicine. Today, it is "pay to play" for hundreds of thousands of US physicians thanks to the American Board of Medical Specialties (ABMS)/American Board of Internal Medicine(ABIM)'s Maintenance of Certification (MOC) program.
As I mentioned in an earlier blog post, I received a notice in late November of this year by US mail that I had to earn 100 Maintenance of Certification (MOC) points, or I could see a "change in my certification status." The ABIM webpage displays that notice prominently as well.
Recall that I certified in both Cardiac Electrophysiology and Cardiology with the 2013 testing cycle. At that time, according to the ABIM's website and this archived webpage from January 18th, 2013, MOC required that I perform 100 MOC points every 10 years. When I purchased MOC and registered to take my recertification test in October 2013, this is what I thought I was purchasing.
Now I find the ABIM has changed the rules. Now we must perform 100 MOC points every 5 years.
Needless to say, I had only 10 MOC points when I received that notice from the ABIM after the Thanksgiving holiday. I had vowed not the earn another point until it might be needed 10 years from the data I enrolled for my MOC exam and have been working to end MOC through conventional channels since that time. I have talks at the AMA House of Delegates, Ohio Health committee, and help with the Texas anti-MOC legislation as proof of that effort. One guy doesn't stand a chance, I learned.
Still, I became worried about the implications of now needing another 100 MOC points and the time, focus, and commitment required so I could keep seeing patients. I searched for ways I could fulfill my requirements without paying the ABIM another dime.
This is where things got interesting.
It seems I pre-paid for "30 MOC points" - one for a 2017-2019 Hospitalist Update, a 2017-2019 Internal Medicine Update, and a "Care for the Underserved" module that offered 10 MOC points. (The other offerings that might have been there before had "expired.") These thirty points wouldn't be enough to get me where I needed to be by 21/31/2018. Furthermore, learning about these non-applicable topics to my specialty seemed to be a waste of time. Still, I needed points, so I did what I could and even performed the Hospitalist update. I was surprised to find that the ABIM's own Robert Wachter, MD, "Mr. Hospitalist" himself, helped author this module. Because it was outside my wheelhouse, that module took way too long to successfully complete, but I finally did it to earn my "points."
Nothing to see here folks...
I was getting concerned. I checked the Heart Rhythm Society's webpage hoping they would have a module closer to my specialty that I could complete quickly and was surprised to find that they could only offer me 6.75 MOC points if I purchased a $650 Medical Knowledge update in Electrophysiology - a cost of $96.30 per MOC point! That was an astronomical price per MOC point and one that wouldn't get me anywhere near my goal of 100 total points.
I moved on.
The ABIM site suggested I look at the various offerings provided by the ACCME at http://www.cmefinder.org - a horribly rudimentary website that had poor filtering capabilities for the offerings I might need. They sent me to this hospital system and that hospital system with ways to game the system, but nothing would work for me or each offering gave me 0.5 to 1 MOC point each. Everyone, it seemed, were more than happy to offer a point here or a point there, but every point required a post-MOC survey of how I liked it, it the exercise was free from commercial bias, etc. - all very time-consuming - so I kept looking.
I turned to the American College of Cardiology's website since I am a Fellow of the American College of Cardiology and looked at their MOC offerings. I still needed a LOT of points if I was to make 100 by 12/31/2018. That's when it struck me: this was the plan! Whether you're an ACC member or not, you've got to pay the Man.
There, on the ACC's MOC webpage was this offering: ACC Self Assessment Program 9 (ACCSAP9) for $1600 in return for 155 potential MOC points good through mid-2019, a bargain-basement price of $10.32 per MOC point!
Left with few options this late in the do-or-die MOC extortion game to keep my hospital privileges and insurance payments coming, I purchased ACCSAP-9.
Before I could get started, I had to agree to a "Credit Agreement." In that agreement I had to agree to "read all text, watch all presentations and answer all questions within the topic for which you claim credit. You must obtain 70% or better on the questions, but you may answer the questions as many times as necessary to achieve that score."
Please.
Then there was the indemnify and hold harmless "Disclaimer" clause of the Credit Agreement: "The American College of Cardiology is not responsible for the results obtained from the use of the information contained in this publication... The American College of Cardiology does not warrant the information contained herein is in every way accurate or complete, and disclaim all responsibility."
Ahem, isn't this WHY we're being forced into this expensive exercise? If I can't rely on them to assure patient and "the public's" safety, what good are these "Knowledge Assessments" for patients?
Having no choice but to "agree" to their terms, lest I lose my hospital privileges and insurance payments to my hospital on 1 Jan 2019, I reluctantly clicked "I agree" and started the arrhythmia section of the testing the week before Christmas.
My wife and kids were not pleased.
"Dad, be here now. It's Christmas! Here you are, 35 years of experience, doing these mindless exercises and getting all stressed out. Haven't you done this long enough?"
"Honey, it's always me doing everything for Christmas while you get all stressed out and have to sit at that damn computer, doing quizzes. Will it ever end? How many years has it been?"
I realize that they are right. Years of being Mr. Good Guy while they lost out on their father. Experience means nothing to the ABMS. Money is everything with MOC. It is clear to me now that the "lifelong" educational system for physicians is horribly broken - a once reasonable voluntary system of continuing medical education required for state licensure, has morphed to an do-or-die extortion scheme for doctors' money. It's not about the patients or the doctor. These organizations indemnify themselves of this responsibility. It's just about the money.
And for hospitals and insurers, it's about control of the doctors to keep their profits high.
The ACC - our cardiovascular specialty society that looks more and more like the AMA, has found a way to get rich - very rich - using the threat of my loss of privileges to fund their organization via the ABIM's MOC program. No wonder they collaborate.
The American College of Physicians (ACP) has their Medical Knowledge Self-Assessment Program (MKSAP) likely does the same thing. So does the American Board of Pediatrics. Whether the ABMS member board is a "continuous certification" or MOC participant, the ABMS mothership keeps the money flowing to all of these entities who claim to educate using computer products while hiding behind "Disclaimers" that relinquish their responsibility.
Buying a product in 2013 thinking one thing, only to find it's another, is fraud as far as I'm concerned. Doctors like me don't like being swindled and forced to play games that have no meaning so they can keep providing patient care. There simply are not enough hours in the day for any of us to put up with these shenanigans required by the members of the Accreditation Council for Graduate Medical Education (like the ABMS) for their financial benefit. They are not only hurting doctors, but hurting their families at Christmas time, too. The ACGME members and ABMS Vision Commission should each carefully read how the ABMS MOC program has harmed doctors in this latest serious anti-trust Complaint filed in federal court against the American Board of Internal Medicine.
The "ABMS Vision Commission's" Draft Report fails to disclose these potential harms caused to physicians by MOC and its numerous conflicts of interest. Do they really think their assets will indemnify them of their responsibility to the well-being of working US physicians, and in turn, their patients?
I think not.
Primum non nocere.
-Wes
Sunday, December 09, 2018
Boarded to Death: Physicians Sue the ABIM
On Thursday 6 December 2018 in the Federal District Court of Eastern Pennsylvania, a class action lawsuit on behalf of over 100,000 internal medicine physicians was filed against the American Board of Internal Medicine (ABIM) by four internists.
The plaintiffs brought the action pursuant to the Clayton Antitrust Act, 15 U.S.C. §§ 15 and 26 to recover treble damages, injunctive relief, costs of the suit, and reasonable attorney’s fees arising from violations of Sections 1 and 2 of the Sherman Act (28 U.S.C. §§ 1 and 2). The suit alleges that there is illegal tying of the ABIM’s initial board certification product to its maintenance of certification® (MOC®) product in violation of Section 1 of the Sherman Act and illegal monopolization and monopoly maintenance in violation of Section 2 of the Sherman Act. The suit claims that after the ABIM's attempts to sell a voluntary "Continuous Professional Development" accolade program failed to recruit enough physician interest, the ABIM created a wholly new market product for itself, time-limited board certification (later branded as "Maintenance of Certification®" or MOC®), forcing physicians to purchase this product or lose their specialty certification. It also alleges ABIM induced hospitals and related entities, insurance companies, medical corporations, and other employers to require internists to be ABIM-certified to obtain hospital consulting and admitting privileges, reimbursement by insurance companies, employment by medical corporations, malpractice coverage, and other requirements of the practice of medicine. As an indication of ABIM's illegal tying and monopoly maintenance, the suit claims, is that the ABIM is able to charge inflated monopoly prices for MOC®, increasing the fees it generates from MOC® 276% since 2000. Each of the plaintiffs have claimed substantial harm caused by MOC®.
A link to the full Complaint can be found here.
-Wes
Update: The original class action anti-trust Complaint filed 6 Dec was amended 23 January 2019 to include claims under the RICO Act and state law unjust enrichment claims.
The plaintiffs brought the action pursuant to the Clayton Antitrust Act, 15 U.S.C. §§ 15 and 26 to recover treble damages, injunctive relief, costs of the suit, and reasonable attorney’s fees arising from violations of Sections 1 and 2 of the Sherman Act (28 U.S.C. §§ 1 and 2). The suit alleges that there is illegal tying of the ABIM’s initial board certification product to its maintenance of certification® (MOC®) product in violation of Section 1 of the Sherman Act and illegal monopolization and monopoly maintenance in violation of Section 2 of the Sherman Act. The suit claims that after the ABIM's attempts to sell a voluntary "Continuous Professional Development" accolade program failed to recruit enough physician interest, the ABIM created a wholly new market product for itself, time-limited board certification (later branded as "Maintenance of Certification®" or MOC®), forcing physicians to purchase this product or lose their specialty certification. It also alleges ABIM induced hospitals and related entities, insurance companies, medical corporations, and other employers to require internists to be ABIM-certified to obtain hospital consulting and admitting privileges, reimbursement by insurance companies, employment by medical corporations, malpractice coverage, and other requirements of the practice of medicine. As an indication of ABIM's illegal tying and monopoly maintenance, the suit claims, is that the ABIM is able to charge inflated monopoly prices for MOC®, increasing the fees it generates from MOC® 276% since 2000. Each of the plaintiffs have claimed substantial harm caused by MOC®.
A link to the full Complaint can be found here.
-Wes
Update: The original class action anti-trust Complaint filed 6 Dec was amended 23 January 2019 to include claims under the RICO Act and state law unjust enrichment claims.
Tuesday, December 04, 2018
Doctors' Right to Privacy: Is MOC Collapsing Under Its Own Weight?
On Saturday, 1 December 2018, the American Board of Internal Medicine (ABIM) suffered a meltdown of its highly touted "Knowledge Check-in" ("KCI") alternative to its mandated Maintenance of Certification® (MOC) program.
Not surprisingly, after a lackluster apology, the ABIM tried to deflect blame to someone else: Pearson VUE.
Might the problem have gone beyond Pearson VUE since individuals at home were similarly affected?
Recall that security of ABIM's examination is of utmost importance to them. They've even had a "Director of Test Security" and even sent their own director of test content to spy on physicians attending a board review course without their knowledge and later sanctioned or suspended over 130 physicians' board certification certificates accusing them of "cheating" in 2009. At that time, the same Director of Test Security for ABIM also worked for a litle known test security firm, Caveon Test Security. It was David Foster, PhD, CEO and President of Caveon Test Security, who was also a Chief Scientist at Kryterian Global Testing Services that touted the security and reliability of their patented keyboard and eyeball monitoring services to the American Board of Pediatrics Foundation on 15 May 2015. It was Kyterion's home testing platform that the ABIM's entire KCI initiative was based.
ABIM diplomates like myself want to know what role the link to Kryterian Global Testing Services had in the events of December 1, 2018 KCI meltdown. ABIM is obligated to come clean on this issue, since it appears more than just testing was occuring that Saturday in December. If the link to Kryterion's keyboard and eyeball tracking technology were involved, physicians' privacy rights may have been violated as well in the name of test security during this latest MOC® debacle.
-Wes
At 09:45 AM, Saturday, December 1, 2018, during the ABIM Internal Medicine Knowledge Check-In (KCI) administration, Pearson VUE – ABIM’s exam delivery provider – experienced network instability issues that affected hundreds of physicians scheduled to take the Internal Medicine KCI exam."KCI," a program that requires continuous payments to ABIM of $155 per year per US physician, was heavily promoted by ABIM as a "kinder, gentler MOC" that physicians could perform in the comfort of their own home, provided of course, that the physician's computer met ABIM's exacting standards. If not, the physician was required to pay an additional $130 to take their MOC examination at a PearsonVue testing center. Sadly on Saturday, hundreds, if not thousands, of US physicians (we really don't know) - all of whom had already funded millions upon millions of dollars for expensive executive salaries, benefits, and contractor expenses to the ABIM for years - lost another of their few precious free weekends staring at computer screens like guinea pigs for academic medicine's biggest income redistribution Ponzi scheme, MOC®.
As a result of these issues, over a period of approximately two hours, physicians were unable to start the KCI, and those who were in the process of testing were unable to proceed.
Not surprisingly, after a lackluster apology, the ABIM tried to deflect blame to someone else: Pearson VUE.
“We at Pearson VUE take full responsibility for Saturday’s disruptive outage of service for ABIM’s Internal Medicine Knowledge Check-In. ABIM did everything they could to help us – and support you – during this time. It was our system that had these issues. As we have promised them, we promise you that we are taking additional steps in order to prevent this from happening again. We are extremely sorry for this unfortunate and rare occurrence and also apologize to the ABIM organization for the disruption and surrounding issues this may have caused. We are committed to continue working in partnership with ABIM in the care and handling of this incident.”Calls made to ABIM assured physicians that only Pearson VUE was involved in the online proctoring. But there is an important disconnect in the announcement made by ABIM about this incident. Note that the press release issued to the public mentions that physicians at home AND at Pearson VUE testing centers were affected:
At approximately 9:45 AM (EST), on December 1, 2018, ABIM began receiving reports from Pearson VUE and individual test takers that they were unable to begin the exam or were unable to continue it if they had already started.Their explanation is incomplete.
Might the problem have gone beyond Pearson VUE since individuals at home were similarly affected?
Recall that security of ABIM's examination is of utmost importance to them. They've even had a "Director of Test Security" and even sent their own director of test content to spy on physicians attending a board review course without their knowledge and later sanctioned or suspended over 130 physicians' board certification certificates accusing them of "cheating" in 2009. At that time, the same Director of Test Security for ABIM also worked for a litle known test security firm, Caveon Test Security. It was David Foster, PhD, CEO and President of Caveon Test Security, who was also a Chief Scientist at Kryterian Global Testing Services that touted the security and reliability of their patented keyboard and eyeball monitoring services to the American Board of Pediatrics Foundation on 15 May 2015. It was Kyterion's home testing platform that the ABIM's entire KCI initiative was based.
ABIM diplomates like myself want to know what role the link to Kryterian Global Testing Services had in the events of December 1, 2018 KCI meltdown. ABIM is obligated to come clean on this issue, since it appears more than just testing was occuring that Saturday in December. If the link to Kryterion's keyboard and eyeball tracking technology were involved, physicians' privacy rights may have been violated as well in the name of test security during this latest MOC® debacle.
-Wes
Saturday, December 01, 2018
ABIM Fees Place Physician Bank Accounts on High Continuous Suction
The American Board of Internal Medicine's (ABIM) ongoing seemingly endless changes to their Maintenance of Certification® (MOC®) product is affecting physicians who re-certified a short five years ago - like myself.
Let's review precisely what has taken place since time-limited certification was implemented by the ABIM in 1990:
Through self-serving rule changes, the ABIM has become a tax-exempt for-profit money machine that has placed physician bank accounts on high continuous suction. They coerce physicians by threatening them with the loss of their credentials or ability to receive insurance company payments to keep the money flowing.
We know why: thanks to their own hubris and avarice, they are failing financially. They have lost the trust of US physicians. And are a partisan organization beholden to the Medical Industrial Complex, not patients.
Given then above information, I believe the ABIM's tax-exempt status should be revoked. Their fees have skyrocketed from $795 to $2200 over 18 years (2000 to 2018) - or 276% - while providing the same product, "certification" of working internists since 1936, nothing more.
-Wes
Let's review precisely what has taken place since time-limited certification was implemented by the ABIM in 1990:
- From 1936 to 1990, ABIM Board certification was a lifetime credential.
- From 1990 to 2005, ABIM ended lifetime certification, and began issuing only time-limited certification to physicians for those certified after January 1, 1990, requiring re-testing (and renewed payments to them valued at more than a thousand dollars) every 10 years.
- In 2006, "Maintenance of Certification," a product rebranded from "Continuous Professional Development" (note the similarities of these two linked webpages) was implemented. MOC was later trademarked by the American Board of Medical Specialties who stipulated programatic alignment from ALL physician subspecialty boards and required them to perform additional practice performance tasks and earn 100 "MOC points" AND re-take their board certification test every 10 years. Additional fees were often required to earn points from "MOC-eligible" courses.
- In 2013, the ABIM imposed more burdensome changes to MOC, not only having to re-take their examination every 10 years, but a "MOC activity" had to be completed every 2 years with patient safety, patient "voice", and survey modules or "Practice Improvement Modules" performed every 5 years and they also had to accumulate 100 MOC points every 5 years.
- Now the ABIM requires internists to pay not only an annual program fee to participate in MOC, but an "Assessment Fee" for MOC examinations. Internists can sign up for Knowledge Check-in examination every two years, or still take the 10 year examination.
Through self-serving rule changes, the ABIM has become a tax-exempt for-profit money machine that has placed physician bank accounts on high continuous suction. They coerce physicians by threatening them with the loss of their credentials or ability to receive insurance company payments to keep the money flowing.
We know why: thanks to their own hubris and avarice, they are failing financially. They have lost the trust of US physicians. And are a partisan organization beholden to the Medical Industrial Complex, not patients.
Given then above information, I believe the ABIM's tax-exempt status should be revoked. Their fees have skyrocketed from $795 to $2200 over 18 years (2000 to 2018) - or 276% - while providing the same product, "certification" of working internists since 1936, nothing more.
-Wes
Sunday, November 25, 2018
ABIM To Diplomates: Merry Christmas! Participate in MOC or Else
This weekend, I received this orange notice from the American Board of Internal Medicine (ABIM) in the mail:
At first I was going to ignore this flier, since I am board certified until 2023 in Cardiology and 2024 in Cardiac Electrophysiology.
But then I read the reverse side of the flier, and noticed this threatening sentence:
It appears the ABIM will revoke the "time-limited" certification(s) I have paid for through 2023 in Cardiovascular Diseases and through 2024 in Cardiac Electrophysiology because I have refused to earn 100 Maintenance of Certification® (MOC®) points by 12/31/2018.
Must diplomates who have "pre-paid" for their certifications now ALSO have to participate in MOC just to maintain their pre-paid certificates?
I certainly hope not. If so, things could get ugly very quickly for everyone involved.
-Wes
 |
| (Click to enlarge) |
At first I was going to ignore this flier, since I am board certified until 2023 in Cardiology and 2024 in Cardiac Electrophysiology.
But then I read the reverse side of the flier, and noticed this threatening sentence:
"Your deadline is approaching, so we wanted to follow-up on the email reminders we've sent to you about earning 100 MOC points by 12/31/2018 to stay certified." (emphasis mine)
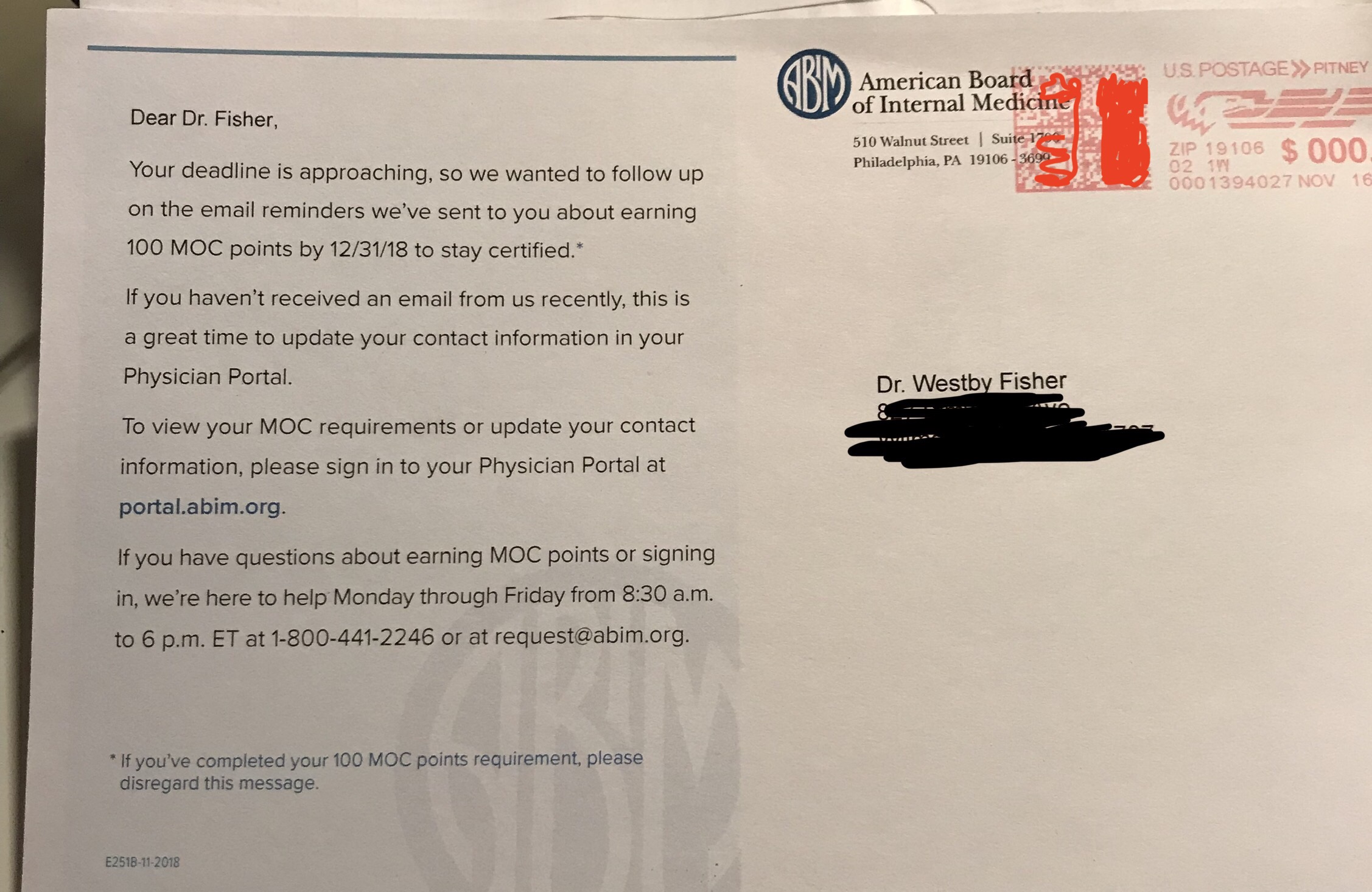 |
| (Click image to enlarge) |
It appears the ABIM will revoke the "time-limited" certification(s) I have paid for through 2023 in Cardiovascular Diseases and through 2024 in Cardiac Electrophysiology because I have refused to earn 100 Maintenance of Certification® (MOC®) points by 12/31/2018.
Must diplomates who have "pre-paid" for their certifications now ALSO have to participate in MOC just to maintain their pre-paid certificates?
I certainly hope not. If so, things could get ugly very quickly for everyone involved.
-Wes
Tuesday, November 06, 2018
Ending MOC Nationwide
Continuing education for physicians is important (and we've been doing it all our lives on our own), but when working physicians' right to care for their patients is threatened by unaccountable non-profit testing organizations that have serious undisclosed conflicts of interest, we will take action.
-Wes
P.S.: Patients, doctors: want to help? You can still donate.
-Wes
P.S.: Patients, doctors: want to help? You can still donate.
Saturday, October 27, 2018
MOC as Physician Stick and Carrot
Remember when the American Board of Medical Specialties (ABMS) Maintenance of Certification (MOC®) was sold to physicians by our specialty societies and ABMS member boards as a "pathway to know that they are staying current in the medical knowledge they use to treat patients and make important care decisions daily?"
Congress was sold the same thing in 2013:
Yesterday, Blue Cross and Blue Shield of Michigan announced (via their friends at the Michigan State Medical Society), that lowly family practice physicians, internists, and pediatricians that are "designated" patient centered medical home physicians won't have to participate in MOC® after all:
Patient care value?
Now you see it, soon you won't.
-Wes
Congress was sold the same thing in 2013:
"ABMS MOC® is a system of specialty-specific assessment and professional development activities that require medical specialists to reflect on their practice performance, identify gaps, and adopt new practices to improve care."It seems physicians and the public were purposefully mislead. MOC® was always a stick that is now being introduced as a carrot to direct physician behavior.
Yesterday, Blue Cross and Blue Shield of Michigan announced (via their friends at the Michigan State Medical Society), that lowly family practice physicians, internists, and pediatricians that are "designated" patient centered medical home physicians won't have to participate in MOC® after all:
"Effective Jan. 1, 2019, the board certification status of family medicine, internal medicine and pediatric practitioners will be reviewed annually. If their board certification status has lapsed and they are a designated patient centered medical home physician, Blue Cross will grant an exception and allow the practitioner to remain in their Blue Cross and BCN managed care networks. This exception does not apply to new practitioner enrollments. Blue Cross and BCN will continue to require all providers to have board certification upon initial enrollment for affiliation."Meanwhile, the ABMS "Vision Commission" tap dances and distracts by seeking more public comment 2019 timeline magically appears, just as the transition to Medicare's next unproven "value-based" physician pay model is implemented.
Patient care value?
Now you see it, soon you won't.
-Wes
Sunday, October 21, 2018
The Fallacy of dEthics
Meet dHealth (video).
dHealth is digital, algorithmic, group-based health care delivery using blockchain technology.
Who are the dHealth promotors and visionaries? The exact same ones who lead the ABIM and ABIM Foundation in 1999 when it set out to "define medical professionalism" for us. Their final product, the 2002 Physician Charter on Medical Professionalism still stands tall as the guiding light of dEthics for much of organized medicine.
dEthics demands that devotion to the best interests of each individual be replaced by an ethic of devotion to the best interests of the group for which the physician is personally responsible.
dEthics is now driving corporate medicine. Data control. Information control. Education control. More with less; profit before person.
No one saw this more clearly that Dr. Richard Fogoros on his now quiet Covert Rationing blog:
What could possibly go wrong?
-Wes
h/t: to james gaulte at the Retired Doc's Thoughts blog.
dHealth is digital, algorithmic, group-based health care delivery using blockchain technology.
Who are the dHealth promotors and visionaries? The exact same ones who lead the ABIM and ABIM Foundation in 1999 when it set out to "define medical professionalism" for us. Their final product, the 2002 Physician Charter on Medical Professionalism still stands tall as the guiding light of dEthics for much of organized medicine.
dEthics demands that devotion to the best interests of each individual be replaced by an ethic of devotion to the best interests of the group for which the physician is personally responsible.
dEthics is now driving corporate medicine. Data control. Information control. Education control. More with less; profit before person.
No one saw this more clearly that Dr. Richard Fogoros on his now quiet Covert Rationing blog:
The intent of the 2002 Charter on medical professionalism was to repair the problem (i.e., to cure the “frustration”), not by confronting the forces of evil doing the coercion, but rather, by simply changing medical ethics to make bedside rationing OK. And that’s just what the document did, though only after careful re-editing to make this radical change to medical ethics sound as benign as possible.dHealth is the next great hope. The vision for world health sees blockchain technology allowing nurses (video) to access to a "complete file" of a patient's health information and to "see into the future in health" to deliver scalable care worldwide remotely using corporate dEthics as their guide.
What could possibly go wrong?
-Wes
h/t: to james gaulte at the Retired Doc's Thoughts blog.
Sunday, October 07, 2018
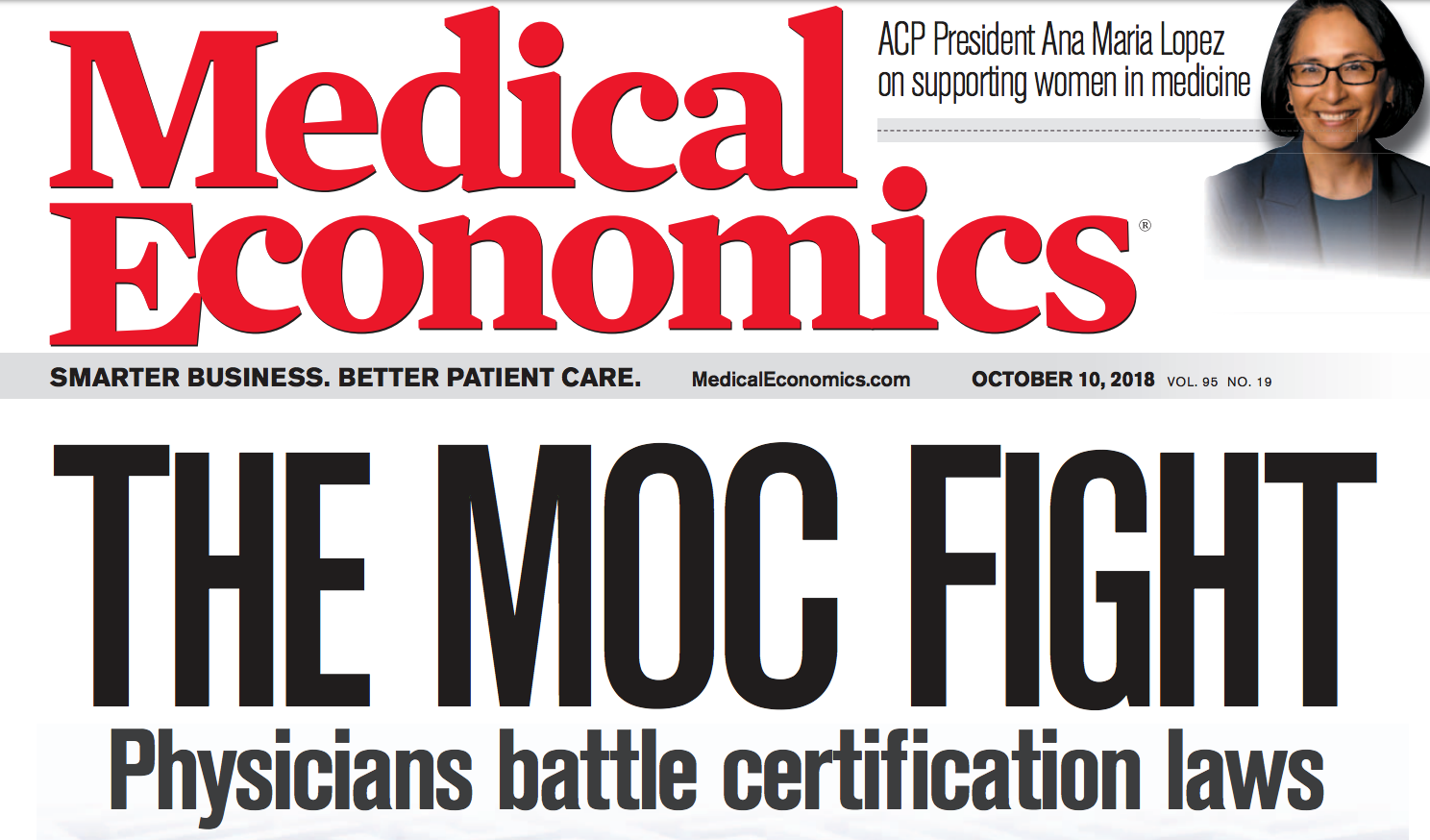
The MOC Fight
From Medical Economics:
“Physicians are pushing legislation on the state level because they don’t trust the ABMS [American Board of Medical Specialties] and its financial conflicts of interest,” says Paul Mathew, MD, a volunteer board member of the NBPAS in Cambridge, Mass. “Many feel the only way to declaw the tiger is legislative action due to insurance companies and academic institutions having no reason to change their pro-MOC policies.” The ABMS oversees MOC for its 24 boards.-Wes
Friday, October 05, 2018
For Whom MOC Tolls
He saw me in the hall between cases and our eyes connected, however briefly. I probably looked a bit tired, hair askew, and rushed after a long ablation case as I scurried to grab a quick bite to eat before my next case started. He was one of our best fellows in cardiology - hard working, innovative, never one to skip a clinical detail or shirk a responsibility, who clearly wanted to chat. He approached respectfully, smiling timidly, and said quietly:
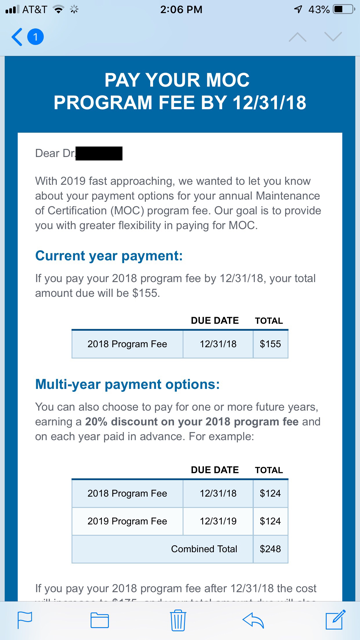
"Dr. Fisher, is it true that I have to pay ABIM $155 to maintain my certification even though I passed my boards? And do I have to do this for life? I went to the ABIM website and it really isn't clear what we have to do."
I explained the ABIM's current iteration of fees and testing as best I could in the brief time we crossed paths. The ever-shifting sands of the ABIM parsed fee and "point" structures, "discounts," programs, credits, and value of participating (or not) in Maintenance of Certification have lead, I believe intentionally, to the current chaotic state of US physician Board certification. I felt sorry for him but was not surprised he was confused, especially since explaining the board process was equally difficult. I sensed he knew that speaking candidly about his concerns with others in positions of leadership might compromise his reputation as a hard-working, reliable cardiology trainee and was grateful he felt he could approach me with his concerns.
This is what US physician board certification has become: little more than a shakedown of our best and brightest to fund a bloated bureaucratic credentialing system that adds little to no value to our trainees' learning experience. After our conversation, I grabbed a salad and returned to do my pre-operative checklist for my next patient. My phone received a text message:
"$155 is my annual savings during fellowship..."
-Wes
"Dr. Fisher, is it true that I have to pay ABIM $155 to maintain my certification even though I passed my boards? And do I have to do this for life? I went to the ABIM website and it really isn't clear what we have to do."
I explained the ABIM's current iteration of fees and testing as best I could in the brief time we crossed paths. The ever-shifting sands of the ABIM parsed fee and "point" structures, "discounts," programs, credits, and value of participating (or not) in Maintenance of Certification have lead, I believe intentionally, to the current chaotic state of US physician Board certification. I felt sorry for him but was not surprised he was confused, especially since explaining the board process was equally difficult. I sensed he knew that speaking candidly about his concerns with others in positions of leadership might compromise his reputation as a hard-working, reliable cardiology trainee and was grateful he felt he could approach me with his concerns.
This is what US physician board certification has become: little more than a shakedown of our best and brightest to fund a bloated bureaucratic credentialing system that adds little to no value to our trainees' learning experience. After our conversation, I grabbed a salad and returned to do my pre-operative checklist for my next patient. My phone received a text message:
-Wes
Tuesday, September 25, 2018
ABMS and ABU Spin on DOJ Letter
Board certification of US physicians continued on its path of deceptive and misleading propaganda following the Department of Justice's (DOJ) letter issued on behalf of a request by the National Board of Physicians and Surgeons (NBPAS) in its effort to thwart the monopoly practices of the American Board of Medical Specialties (ABMS) and its 24 member boards. Despite that letter, the ongoing collusion between the member boards and the ABMS was particularly evident in the email circulated two days ago by the Executive Secretary of the American Board of Urology (ABU), Gerald H. Jordan, MD. The ABU's email attempts to spin the ABMS position as the same as what is stated in the DOJ letter by conflating initial lifetime ABMS Board Certification with the self-created separate time-limited Board certification market product (called Maintenance of Certification®):
-Wes
The ABMS position that legislative interference which limits the use of physician certification is inappropriate is consistent with the position set forth in the DOJ letter. The ABMS and the ABU have always supported a fair and competitive marketplace for physician specialty certification and continue to do so, encouraging accurate comparison of our programs with other certification programs available.This continued deception of the ABMS and its member boards by conflating lifetime certification with time-limited "continuous" certification will not go unchallenged. I encourage all physicians adversely affect by their member boards complicit in this ruse to consider contributing to our ongoing legal challenge against the ABMS board certification monopoly.
ABMS agrees with the DOJ’s support of the right of patients and health systems to determine which certification programs best meet their expectations for providing information about high quality specialty care. The ABMS and ABU promote communications practices that allow the public to easily identify and compare the program standards used to certify that a physician has demonstrated, through training and assessment, that he or she in fact has demonstrated the knowledge, skill and judgment to practice in a medical specialty or subspecialty.
-Wes
Sunday, September 16, 2018
Resident Recall - "Cheating" or Part of Free Speech?
Read the opinion piece referenced below carefully. It discusses the widespread use of "resident recall" to study for the American Board of Radiology's board certification examinations by both residents AND faculty/senior physicians:
https://pubs.rsna.org/doi/full/10.1148/radiol.12120251
Then read the back story on how the American Board of Medicine threatened internists in 2010 on the basis of the threat to their training monopoly:
http://drwes.blogspot.com/2016/06/maintenance-of-certification-medicines.html
Then ask yourself: who has "cheated" whom?
It is clear that the American Board of Medical Specialties, who continues to promote its lavish ABMS Conferences with "stakeholders" in Las Vegas (full schedule here), has a serious problem on its hands. This problem is exacerbated when it claims to work collectively with "500 professionals from across the health care community who, working together, will accelerate the transformation of Board Certification and the delivery of quality patient care."
Where's the data a computer test and secret data collection scheme does anything except raise prices and stroke the egos/bank accounts of the boards' leadership?
What do these Las Vegas boondoggles do to reestablish trust in the ABMS board certification process?
The answer is quite simple:
Nothing.
-Wes
https://pubs.rsna.org/doi/full/10.1148/radiol.12120251
Then read the back story on how the American Board of Medicine threatened internists in 2010 on the basis of the threat to their training monopoly:
http://drwes.blogspot.com/2016/06/maintenance-of-certification-medicines.html
Then ask yourself: who has "cheated" whom?
It is clear that the American Board of Medical Specialties, who continues to promote its lavish ABMS Conferences with "stakeholders" in Las Vegas (full schedule here), has a serious problem on its hands. This problem is exacerbated when it claims to work collectively with "500 professionals from across the health care community who, working together, will accelerate the transformation of Board Certification and the delivery of quality patient care."
Where's the data a computer test and secret data collection scheme does anything except raise prices and stroke the egos/bank accounts of the boards' leadership?
What do these Las Vegas boondoggles do to reestablish trust in the ABMS board certification process?
The answer is quite simple:
Nothing.
-Wes
Friday, September 14, 2018
When the Walls Start Crumbling Down
From the Department of Justice via the NBPAS website:
-Wes
'The DOJ explained that the ABMS Program on MOC may have the effect of “harming competition and increasing the cost of healthcare services to customers.” ABMS may do so “by imposing overly burdensome conditions on physicians who wish to maintain their certification.” The DOJ added, with respect to ABMS, “[the] vast majority of [its] board members are medical doctors”—i.e., “active market participants”—who may have incentives to limit competition through “industry self-regulation.” As a result, the DOJ warned, “there would be competition concerns, if dominant certifying bodies [like ABMS] set de facto participation requirements that did not sufficiently correspond to health, safety, or other procompetitive justifications.”'While this letter is very helpful to the National Board of Physicians and Surgeons (NBPAS) and detrimental to the efforts of the American Board of Medical Specialties and their subsidiary boards to monopolize the physician continuous credentialing system in states' legislation accross the country, it might not be entirely advantageous to employed physicians because of this paragraph on page 14:
"At the same time, the Division discourages the legislature from interfering with unilateral business decisions—such as an individual hospital’s decision about what criteria to use for granting hospital privileges or an individual insurance carrier’s decision about what criteria to use for allowing participation in the insurer’s network, as restricted in the Workgroup’s Bill—unless a restriction is determined to be necessary and narrowly tailored to redress well- founded consumer harms or risks. ... The Division encourages the Maryland legislature to consider whether other tools, such as facilitating entry by competitive certifying bodies, can address concerns with certification without imposing restrictions on the unilateral business decisions of hospitals and carriers."Still, this letter represents a significant blow to ABMS in their efforts to prevent NBPAS's entry into the physician maintenance of certification (or "continuous certification") market as 30 states have some form of anti-MOC legislation either pending or passed.
-Wes
Friday, September 07, 2018
Thank You, Colleagues
I would be remiss if I did not thank my friends and colleagues nationwide who contributed to our GoFundMe page to initiate our pre-litigation investigation of the American Board of Internal Medicine and the ABIM Foundation. While I was upgrading a DDDR pacemaker to a biventricular ICD today, I received a text from a colleague that we had reached our funding goal for this initial phase.
I cannot express my gratitude enough. Thank you all.
It is very reaffirming to know that others feel as I do about Maintenance of Certification and what it has done to physician autonomy, morale, and even our right to work. I know that the dollars contributed could have been used for so many other things. I hope you will soon see that it your money was well spent.
But as Winston Churchill famously said:
"Now this is not the end. It is not even the beginning of the end. But it is, perhaps, the end of the beginning."
Thanks again -
-Wes
I cannot express my gratitude enough. Thank you all.
It is very reaffirming to know that others feel as I do about Maintenance of Certification and what it has done to physician autonomy, morale, and even our right to work. I know that the dollars contributed could have been used for so many other things. I hope you will soon see that it your money was well spent.
But as Winston Churchill famously said:
"Now this is not the end. It is not even the beginning of the end. But it is, perhaps, the end of the beginning."
Thanks again -
-Wes
Thursday, September 06, 2018
Video: 7007 US Physicians Weigh In on US Board Certification
From January through March 2018, a voluntary Internet-based survey of US physicians and surgeons was conducted by Practicing Physicians of America concerning ABMS Board Certification. 7007 completed surveys were available for analysis. Here is a brief video summary of many of the survey's findings as promised:
-Wes
Reference: pdf file of PPA Physician survey questions that formed the basis of this report.
-Wes
Reference: pdf file of PPA Physician survey questions that formed the basis of this report.
Sunday, August 26, 2018
Two Surveys: US Physician and Surgeon Perspectives on ABMS Board Certification
At the beginning of this year, Practicing Physicians of America (PPA), a 501c6 physician membership organization (with whom I serve as an unpaid board member), collected results of a voluntary survey via social media channels on ABMS physician and surgeon Board certification. The method of data collection using social media. The data collection is novel compared to previous surveys conducted on this topic and for a while represented the largest reported survey on Board certification ever performed. We submitted the results to JAMA (and later to the Annals of Internal Medicine) in hopes they would be published. They were not. As is true with most surveys, bias was a prevailing concern.
Shortly after our survey was being circulated, the American Board of Medical Specialties introduced their own survey on Board certification to pre-chosen "stakeholders" on Board certification. In July 2018 they announced the results of their survey. They had received responses from "36,392 people, including 34,616 physicians, 1,373 non-physician providers and stakeholders involved in the delivery of health care, and 403 members of the general public." To the best of my knowledge, the text of their survey was not made available to the public.
Since we were waiting the reviews of PPA's survey for months, we were prohibited from publishing our results. After considering the reviewers' comments (which were very thoughtful), I think the odds of ever publishing such a survey of this type in a peer-reviewed scientific journal are low. Hence, the board of PPA has allowed me to announce the results of our survey publicly via this blog and (hopefully) Doximity so these results may be interpreted alongside the survey results reported by the American Board of Medical Specialties' Vision Commission. Admittedly, our survey asked different questions than that conducted by the ABMS, but the results are not only notable for their differences, but also for some similarities.
By way of background, here are the 32 questions we asked in the PPA survey.
Here is the full paper (with some minor edits) we submitted for peer review that was NOT accepted for publication. This pdf includes the background for the survey, the methods used, the results obtained, and a discussion of those results, as well as references, figures and tables.
Similarities of PPA survey to the ABMS Survey on Board Certification:
Major Findings of the PPA Survey
7007 physicians responded (52% male, 48% female)
Demographics
Major Findings
I hope these data are informative and provide a balanced perspective of a large cohort of US physicians' and surgeons' perspectives on ABMS Board initial and "continuous" certification.
Physicians and others are welcome to use these data under a Creative Commons license (see below), we just ask for appropriate attribution.
-Wes
P.S.: Physicians desiring state-specific data regarding the PPA survey results are welcome to contact me via Twitter or email.

Survey of US Physicians and Surgeons Perspectives on US Board Certification by Practicing Physicians of America is licensed under a Creative Commons Attribution 4.0 International License.
Based on a work at http://www.practicingphysician.org.
Shortly after our survey was being circulated, the American Board of Medical Specialties introduced their own survey on Board certification to pre-chosen "stakeholders" on Board certification. In July 2018 they announced the results of their survey. They had received responses from "36,392 people, including 34,616 physicians, 1,373 non-physician providers and stakeholders involved in the delivery of health care, and 403 members of the general public." To the best of my knowledge, the text of their survey was not made available to the public.
Since we were waiting the reviews of PPA's survey for months, we were prohibited from publishing our results. After considering the reviewers' comments (which were very thoughtful), I think the odds of ever publishing such a survey of this type in a peer-reviewed scientific journal are low. Hence, the board of PPA has allowed me to announce the results of our survey publicly via this blog and (hopefully) Doximity so these results may be interpreted alongside the survey results reported by the American Board of Medical Specialties' Vision Commission. Admittedly, our survey asked different questions than that conducted by the ABMS, but the results are not only notable for their differences, but also for some similarities.
By way of background, here are the 32 questions we asked in the PPA survey.
Here is the full paper (with some minor edits) we submitted for peer review that was NOT accepted for publication. This pdf includes the background for the survey, the methods used, the results obtained, and a discussion of those results, as well as references, figures and tables.
Similarities of PPA survey to the ABMS Survey on Board Certification:
- Both ABMS and PPA surveys used SurveyMonkey to collect responses
- A large number of physicians responded to both surveys. Still, the PPA survey represented only 0.92% and the ABMS survey represented only 4.5% of the total US physician population in 2016. Neither survey mitigates potential under-coverage bias and non-response bias.
- In the PPA survey, 93% of physician respondents were board certified vs 96% in the ABMS survey.
- In PPA survey, 80% (4973/6004) participated in MOC; in the ABMS survey, 69 percent of respondents were currently enrolled in a primary specialty MOC program, and 33 percent are currently enrolled in a subspecialty MOC program
- Costs, burden, and the lack of true reflection of their abilities as clinicians were of significant concern to physicians in both surveys
- PPA survey used logic to limit responses from clinically-active physicians only
- PPA survey attempted to geolocate physicians by IP address and excluded non-US physicians
- PPA survey included MDs and DOs; it is unclear how many ABMS physicians were MDs or DOs.
- PPA survey was simply distributed to physicians via social media, not targeted groups like the ABMS survey. Heavy contributors to the PPA survey included members of the Pennsylvania Medical Society and Doximity.
- Discontinuation of "continuous certification" was not offered as an option in ABMS survey. Ending MOC and reverting to lifetime certification with CME was offered as an alternative in the PPA survey.
- PPA survey assessed physician perceptions of the negative consequences, contract obligations, and potential conflicts of interest of MOC; ABMS survey did not address these issues.
- PPA survey specified physician-respondents' specialties and state of origin. ABMS survey did not.
Major Findings of the PPA Survey
7007 physicians responded (52% male, 48% female)
Demographics
- Every US state was represented, with the largest being PA (910), CA (506), TX (504), FL (406) being the largest physician participants
- Responses came from 24 different subspecialites, with the largest being family medicine and pediatrics
- 19% of physicians had at least one "grandfathered" certification.
- 65% of the respondents had 10 or more years of clinical experience
- Of the physicians with initial ABMS board certification, 80% participated in MOC.
Major Findings
- 90% of all respondents thought board certification should be a lifetime credential with CME used for ongoing education.
- 95% felt MOC increases burnout.
- 53% of respondents estimated costs (direct and indirect) were more than $4000.
- 94% were unaware their data were being sold.
- 80% felt IRB and informed consent should be required for research conducted by the boards.
- 86% perceived MOC could threaten their right to work.
- 8.4% failed a recertification examination.
- Of the 394 physician that failed recertification, harms experienced included psychologic harms (more than 56%), 10% lost of hospital privileges , 5% lost their job, 8% lost insurance panel participation, and 17% plan to retire rather than retaking the re-certification examination.
I hope these data are informative and provide a balanced perspective of a large cohort of US physicians' and surgeons' perspectives on ABMS Board initial and "continuous" certification.
Physicians and others are welcome to use these data under a Creative Commons license (see below), we just ask for appropriate attribution.
-Wes
P.S.: Physicians desiring state-specific data regarding the PPA survey results are welcome to contact me via Twitter or email.

Survey of US Physicians and Surgeons Perspectives on US Board Certification by Practicing Physicians of America is licensed under a Creative Commons Attribution 4.0 International License.
Based on a work at http://www.practicingphysician.org.
Saturday, August 25, 2018
How Practicing Physicians Can Double Their Money
From now until we reach our contribution goal, an anonymous donor(s) has/have graciously stepped up to match, dollar-for-dollar, physicians' contributions to Practicing Physicians of America's GoFundMe page to fund the litigation factual and legal investigation and the drafting of proposed complaint against the American Board of Internal Medicine, the ABIM Foundation, their directors, executives, and perhaps others under federal antitrust laws and state consumer fraud and deceptive trade practices acts to bring an end to MOC™ nationwide.
After four years of bring this issue to my readers on this blog, the AMA, and state legislatures, too many questions and conflicts of interest remain about the financial and political shenanigans of these organizations. While the ABIM claims they have "listened," they still have failed to stop the ability of the proprietary ABMS MOC™program from potentially affecting a physicians ability to retain hospital credentials and insurance payments if they don't pay for the program; in other words, their right to work.
Hundred of physicians have been adversely affected by this program already. For every physician who drops out of medicine because of refusal to play along, approximately 2000 patients are affected in turn.
So please give generously. After all it's a "two-for-one" special going forward!
Thanks everyone (and thanks to our special donor(s))!
-Wes
P.S.: Again, here's that link to donate: https://www.gofundme.com/practicing-physicians-of-america
After four years of bring this issue to my readers on this blog, the AMA, and state legislatures, too many questions and conflicts of interest remain about the financial and political shenanigans of these organizations. While the ABIM claims they have "listened," they still have failed to stop the ability of the proprietary ABMS MOC™program from potentially affecting a physicians ability to retain hospital credentials and insurance payments if they don't pay for the program; in other words, their right to work.
Hundred of physicians have been adversely affected by this program already. For every physician who drops out of medicine because of refusal to play along, approximately 2000 patients are affected in turn.
So please give generously. After all it's a "two-for-one" special going forward!
Thanks everyone (and thanks to our special donor(s))!
-Wes
P.S.: Again, here's that link to donate: https://www.gofundme.com/practicing-physicians-of-america
Wednesday, August 15, 2018
MOC's Greatest Lesson
Yesterday, I read with interest the American College of Obstetricians and Gynecologists widely circulated piece authored by Lucia DiVenere, MA entitled, "MOC: ACOG's role in developing a solution to the heated controversy" published in the August issue of OBG Management. By carefully listing the numerous physician concerns with MOC (costs, relevance to practice, lack of data to improve care, relationship to licensing, employment, privileging, and reimbursement), the article reinforced many of the issues on this blog while being simultaneously crafted to sound as if ACOG was really "listening" to physicians concerns about ABMS Maintenance of Certification (MOC).
It didn't take long for me to realize the article was really about the tired trope that the "ACOG asserts the importance of maintaining self-regulation." The leadership within the ACOG and Ms. DiVenere herself can hardly be described as "self" as far as working physicians are concerned. Ms. DiVenere is Officer, Government and Political Affairs, at the ACOG and OBG Management contributing editor. And while she "reports no financial relationships relevant to this article," her very job may have depended on writing it.
Which leads me to MOC's Greatest Lesson that it consistently teaches working physicians, both young and old: In medicine, it is okay to lie, cheat, and steal.
I do not say those words lightly. Everything MOC touches is corrupt. For a once simple medical accolade to be allowed to secretly morph into a one-billion-dollar-a-year enterprise and physician cudgel to fund the bloated bureaucratic and political aspirations of the Accreditation Council for Graduate Medical Education is beyond me. Yet this is precisely where working physicians find themselves. Are these the ethics to which we want our young doctors of tomorrow to aspire? Should they model turning a cheek the other way to ignore the implications of these actions on our patients just so specialty societies can maintain handsome salaries, political power, and "self-regulation?"
Despite all that has been uncovered by following the money, I still can't believe it's taken one simple GoFundMe page three months to raise $150,000 from working physicians to fight this corruption.
It seems MOC's Greatest Lesson has been taken to heart.
-Wes
It didn't take long for me to realize the article was really about the tired trope that the "ACOG asserts the importance of maintaining self-regulation." The leadership within the ACOG and Ms. DiVenere herself can hardly be described as "self" as far as working physicians are concerned. Ms. DiVenere is Officer, Government and Political Affairs, at the ACOG and OBG Management contributing editor. And while she "reports no financial relationships relevant to this article," her very job may have depended on writing it.
Which leads me to MOC's Greatest Lesson that it consistently teaches working physicians, both young and old: In medicine, it is okay to lie, cheat, and steal.
I do not say those words lightly. Everything MOC touches is corrupt. For a once simple medical accolade to be allowed to secretly morph into a one-billion-dollar-a-year enterprise and physician cudgel to fund the bloated bureaucratic and political aspirations of the Accreditation Council for Graduate Medical Education is beyond me. Yet this is precisely where working physicians find themselves. Are these the ethics to which we want our young doctors of tomorrow to aspire? Should they model turning a cheek the other way to ignore the implications of these actions on our patients just so specialty societies can maintain handsome salaries, political power, and "self-regulation?"
Despite all that has been uncovered by following the money, I still can't believe it's taken one simple GoFundMe page three months to raise $150,000 from working physicians to fight this corruption.
It seems MOC's Greatest Lesson has been taken to heart.
-Wes
Saturday, August 11, 2018
On Trust
(Re-)Building Trust." Oh, the irony. The fact they need to have such a conference is telling of the dire straights the staid and outdated medical credentialing complex has become.
As physicians who funded the ABIM Foundation, why do we fund such nonsense? The American Board of Internal Medicine has never sufficiently explained why this organization felt compelled to use over $78 million of physician testing fees to create the ABIM Foundation or how and why it uses that money. Is it really to fund such conferences? Or might conferences like this really be a distraction for the real reason the ABIM Foundation was created: their retirement fund. By the way, whatever happened to those funds shipped off to the Cayman Islands? Why will we lose our privileges at hospitals or insurance payments if we don't pay into this scheme? And why is the ABIM Foundation colluding with Kaiser Permanente directors? What does Kaiser get for this relationship?
If physicians trusted the ABIM, we would not have to ask such questions and the ABIM Foundation would not have to hold conferences on "re-building" trust.
Three years ago, Richard Baron, MD issued the now infamous: "We got it wrong" mea culpa press release when the 2014 iterations of Maintenance of Certification (MOC) foisted on US physicians resulted in a powerful working physician backlash. Lots of soft-shoe, "listening," and MOC program changes have occurred since then. But in reality four years later, little has changed other than parsing our payments into annual aliquots rather than a single lump sum every-10-year payment. The growth of fees is back on schedule, climbing an incredible 276% in the past 18 years. Even the ridiculous Part IV of MOC is back as before.
It is hard to trust any business, especially a nonprofit organization when they ignore the customer.
We should not lose sight that physicians are the customer of ABIM, not patients. We pay for their medical accolade and the paper certificate that ABIM issues when we successfully complete our initial Board certification and (now) subsequent MOC requirements.
There are many within the US medical board credentialing system who feel otherwise; for them, they are there to serve "the public." Yet this deflection is little more than a propaganda message created to justify their use of our money for their political and financial purposes.
When we see our funds continuing to be wasted at Las Vegas convention venues for American Board of Medical Specialties meetings with their "stakeholders" we realize that this old-school attitude of colleague disrespect and self-importance is endemic to the entire US medical board certification and medical credentialing industry. Hard to re-establish trust with overt demonstrations such as these.
-Wes
PS: Wonder what you can do to change things? Donate here and get a free book at the same time! We're 78% of the way there!
As physicians who funded the ABIM Foundation, why do we fund such nonsense? The American Board of Internal Medicine has never sufficiently explained why this organization felt compelled to use over $78 million of physician testing fees to create the ABIM Foundation or how and why it uses that money. Is it really to fund such conferences? Or might conferences like this really be a distraction for the real reason the ABIM Foundation was created: their retirement fund. By the way, whatever happened to those funds shipped off to the Cayman Islands? Why will we lose our privileges at hospitals or insurance payments if we don't pay into this scheme? And why is the ABIM Foundation colluding with Kaiser Permanente directors? What does Kaiser get for this relationship?
If physicians trusted the ABIM, we would not have to ask such questions and the ABIM Foundation would not have to hold conferences on "re-building" trust.
Three years ago, Richard Baron, MD issued the now infamous: "We got it wrong" mea culpa press release when the 2014 iterations of Maintenance of Certification (MOC) foisted on US physicians resulted in a powerful working physician backlash. Lots of soft-shoe, "listening," and MOC program changes have occurred since then. But in reality four years later, little has changed other than parsing our payments into annual aliquots rather than a single lump sum every-10-year payment. The growth of fees is back on schedule, climbing an incredible 276% in the past 18 years. Even the ridiculous Part IV of MOC is back as before.
It is hard to trust any business, especially a nonprofit organization when they ignore the customer.
We should not lose sight that physicians are the customer of ABIM, not patients. We pay for their medical accolade and the paper certificate that ABIM issues when we successfully complete our initial Board certification and (now) subsequent MOC requirements.
There are many within the US medical board credentialing system who feel otherwise; for them, they are there to serve "the public." Yet this deflection is little more than a propaganda message created to justify their use of our money for their political and financial purposes.
When we see our funds continuing to be wasted at Las Vegas convention venues for American Board of Medical Specialties meetings with their "stakeholders" we realize that this old-school attitude of colleague disrespect and self-importance is endemic to the entire US medical board certification and medical credentialing industry. Hard to re-establish trust with overt demonstrations such as these.
-Wes
PS: Wonder what you can do to change things? Donate here and get a free book at the same time! We're 78% of the way there!
Monday, August 06, 2018
Moving Mountains By Example: Doctor Inspires Others to Fund Anti-MOC Legal Effort
In a reaffirming gesture of solidarity, San Francisco cardiologist Michel Accad, MD has offered to supply an electronic copy of his book "Moving Mountains: A Socratic Challenge to the Theory and Practice of Population Medicine" (seen on Amazon) free of charge to anyone donating $50 or more in the next two weeks to our legal effort to end the onerous and unproven ABMS Maintenance of Certification (MOC™) program nationwide.
Dr. Accad's affable and insightful personal blog (Alert and Oriented) and podcast (Accad and Koka Report) co-produced with Philadelphia cardiologist Anish Koka, MD, have garnered wide physician followings by respectfully and thoughtfully discussing timely issues that matter to doctors. (My recent 46-min podcast discussing this funding drive with them can be heard here).
While the sponsor of the legal effort, Practicing Physicians of America (on whose board I serve), has already reached over 75% of the $150,000 funding goal, I hope Michel's generosity will inspire many other physicians to join this funding drive in hopes working physicians of all ages can help end - once and for all - the expensive, onerous, and corrupt ABMS MOC™ program that has the potential to unjustly limit a physician's right to work.
-Wes
Dr. Accad's affable and insightful personal blog (Alert and Oriented) and podcast (Accad and Koka Report) co-produced with Philadelphia cardiologist Anish Koka, MD, have garnered wide physician followings by respectfully and thoughtfully discussing timely issues that matter to doctors. (My recent 46-min podcast discussing this funding drive with them can be heard here).
While the sponsor of the legal effort, Practicing Physicians of America (on whose board I serve), has already reached over 75% of the $150,000 funding goal, I hope Michel's generosity will inspire many other physicians to join this funding drive in hopes working physicians of all ages can help end - once and for all - the expensive, onerous, and corrupt ABMS MOC™ program that has the potential to unjustly limit a physician's right to work.
-Wes
Sunday, August 05, 2018
Federation of State Medical Boards Attempts to Legislate Away Liability
In a press release, the Federation of State Medical Boards (FSMB) announced their support of the “Occupational Licensing Board Antitrust Damages Relief and Reform Act of 2018 (H.R. 6515),” introduced by Rep. Mike Conaway (R-TX) and co-sponsored by Rep. Lamar Smith (R-TX). According to the press release:
The FSMB President and CEO, Humayun Chaudhry, DO, MACP has quite a history of working with similar self-interested private businesses.
In fact, Dr. Chaudry has long supported the notion of Maintenance of Licensure (MOL) that required Maintenance of (board) Certification (MOC®) and "lifelong learning." Chaudhry chaired a CEO Advisory Council (comprised of a slew of non-governmental U.S. medicine regulatory organizations) that advised the FSMB's Board of Directors and worked with an FSMB MOL Implementation Group (with Richard Hawkins, MD, the current President and CEO of the American Board of Medical Specialties (ABMS), in 2009). That group recommended that physicians actively engaged in the Maintenance of Certification (MOC) program of the American Board of Medical Specialties, or the Osteopathic Continuous Certification (OCC) program of the American Osteopathic Association, should be recognized as "substantially in compliance" with any MOL program that is adopted by a state. Because of this tie between MOL and MOC, the activities of the FSMB in the state of Ohio were met with formal opposition from the Ohio State Medical Association in 2012.
No wonder the board members from various state medical boards have resigned from their positions out of liability concerns. They understood there is credibility to the Federal Trade Commission's concerns that were upheld by the U.S. Supreme Court.
Legislators (especially Rep. Mike Conaway and Rep. Lamar Smith) would be wise to realize that the multi-million dollar FSMB has financial conflicts of interest that may cause more harm than good to our patients.
-Wes
P.S.: Like the FSMB, ABMS collusion with state medical societies regarding MOC® is also evident in this recent ABMS press release.
H.R. 6515 eliminates fiscal antitrust damage liability for state licensing boards-including state medical boards- their members, and staff who are acting within their statutory mandate to protect the public. Currently, board members and staff are exposed to personal liability and treble damages for actions taken as part of their service on a board. The lack of protection has had a chilling effect on the willingness of some individuals to serve on boards, causing some board members to resign for fear of personal financial liability.It is interesting that this new bill attempts to circumvent the 2015 Supreme Court decision that held professional boards could not make decisions that potentially violated antitrust laws and quashed competition. The justices, in an opinion by Justice Anthony Kennedy, agreed with the government’s claim that although state entities are usually exempt from federal antitrust laws, the exemption did not apply because the board was not actively supervised by the state and because it was made up of self-interested private businesses.
The FSMB President and CEO, Humayun Chaudhry, DO, MACP has quite a history of working with similar self-interested private businesses.
In fact, Dr. Chaudry has long supported the notion of Maintenance of Licensure (MOL) that required Maintenance of (board) Certification (MOC®) and "lifelong learning." Chaudhry chaired a CEO Advisory Council (comprised of a slew of non-governmental U.S. medicine regulatory organizations) that advised the FSMB's Board of Directors and worked with an FSMB MOL Implementation Group (with Richard Hawkins, MD, the current President and CEO of the American Board of Medical Specialties (ABMS), in 2009). That group recommended that physicians actively engaged in the Maintenance of Certification (MOC) program of the American Board of Medical Specialties, or the Osteopathic Continuous Certification (OCC) program of the American Osteopathic Association, should be recognized as "substantially in compliance" with any MOL program that is adopted by a state. Because of this tie between MOL and MOC, the activities of the FSMB in the state of Ohio were met with formal opposition from the Ohio State Medical Association in 2012.
No wonder the board members from various state medical boards have resigned from their positions out of liability concerns. They understood there is credibility to the Federal Trade Commission's concerns that were upheld by the U.S. Supreme Court.
Legislators (especially Rep. Mike Conaway and Rep. Lamar Smith) would be wise to realize that the multi-million dollar FSMB has financial conflicts of interest that may cause more harm than good to our patients.
-Wes
P.S.: Like the FSMB, ABMS collusion with state medical societies regarding MOC® is also evident in this recent ABMS press release.
Saturday, July 28, 2018
The ABIM Has Lost Their Marbles
 From the institution that secretly funded itself with ABIM diplomate fees to the tune of over $78 million that culminated in the purchase of a $2.3 luxury condominium for itself complete with a Mercedes S class town car, and offshored funds to the Cayman Islands, comes this news release:
From the institution that secretly funded itself with ABIM diplomate fees to the tune of over $78 million that culminated in the purchase of a $2.3 luxury condominium for itself complete with a Mercedes S class town car, and offshored funds to the Cayman Islands, comes this news release:The 2018 ABIM Foundation Forum will consider the importance of trust in health care – and how to build and maintain it – against a backdrop of political and social turmoil and all-time lows in Americans’ trust in institutions across society.Make no mistake: this is our physician Board re-certification money they are playing with.
At the very least, the optics of such a conference are horrible given the ABIM Foundation's past.
I hope everyone will make good use of the hashtag #abimf2018 on Twitter and then contribute to our legal fund to permanently end this shameless gaslighting of US physicians and our patients.
-Wes
Wednesday, July 25, 2018
Board Certification: From Marketing Accolade to False Idol
I'm Board certified.
So is Carmen A. Puliafito, MD.
So is Farid Fata, MD.
So are plenty of other Medscape "Best and Worst" physicians from 2012-2016.
So what is "Board certification?"
Truth be known, it is little more than a marketing accolade.
And for a while, it worked. Doctors took board certification examinations to market themselves as competent in their field. They would take a written or oral examination created by their peers to demonstrate to others they knew their stuff. And while it remained a lifetime designation, it had some legitimacy. In reality, however, it was up to the residency training programs to train the physicians and verify they knew their stuff. Hospitals used to verify credentials by calling residency programs and verifying doctors participated. They had large credentialing departments that kept everything on file.
But competition between hospitals vying for patients soon grew fierce and hospital marketing departments jumped on the credentialing bandwagon. Soon billboards would appear: "Come to see our board-certified specialists!" and the race was on.
Lawyers joined the fray, too. "My expert witness is better than your expert witness - see how many board certificates he has?"
Truth is, we love this crap. Just look at how many nurse practitioners are "board certified" now!
In the 1960's to 1970's, the American Board of Internal Medicine recognized how lucrative this craze could be, but they had one big problem if they were going to make certifying doctors a full-time business: the number of doctors out there was finite. (It was about that time the board members started paying themselves). They also saw how much money the American Board of Family Medicine, founded in 1969, was generating using 7-year time-limited certifications.
But the ABIM knew internists would be on to them changing the rules for board certification from a lifetime to time-limited credential. So they first tried making a voluntary "super accolade" for internists, called the "Advanced Achievement in Internal Medicine." Needless to say, after four attempts that garnered progressively declining enrollment, the AAIM concept flopped. It was Lynn O. Langdon, MA (a non-physician and Chief Operating Officer of the ABIM) who declared the "End to Voluntary Recertification" and time-limited certification was born with the threat of "uncertain circumstances" if doctors did not participate.
Needless to say, with the help of conflicted members of the ACP who stood to make handsome returns from the Medical Knowledge Self-Assessment Program (MKSAP), they were off to the financial races. And what a race it has proven to be: a nearly $1 billion dollar-a-year enterprise for the entire ACGME.
Unfortunately, no one has ever stopped to study what happens to skilled, competent, board-certified doctors that fail their computerized "re-certification" examination or fail to garner enough "MOC points" to sit for their examination. No one asks about the damage this time-limited credential is having on our physician numbers and access to care. The money is too important to the system.
Not long ago, the chairman of our cardiology division had to relinquish his role as a teacher to medical students because he refused to re-certify in cardiology while also being "certified" in interventional cardiology. (He could keep performing catheterizations and stent placements and remain credentialed thanks to the change in double jeopardy rules that changed just in the nick of time). How many medical students lost out on his experience as a result? Are we happier that medical students are now being taught by younger (time-limited) Board-certified physician instructors rather than life-time certified physicians with decades of experience in the field?
Doctors and nurses know the truth. That's why when seeking out a "quality" physician for their own care, they NEVER ask if a colleague is board-certified since board certification is now a false idol - a hoop to complete whether they're competent, ethical, or not.
We know that it's now far better to ask a trusted colleague or health professional when seeking care because there's much more to being a "quality" physician than holding a computer-generated "certificate."
-Wes
Reference: Fisher WG, Schloss EJ. Medical specialty certification in the United States - a false idol? J Card Electrophys October 2016; 47(1): 37-43.
So is Carmen A. Puliafito, MD.
So is Farid Fata, MD.
So are plenty of other Medscape "Best and Worst" physicians from 2012-2016.
So what is "Board certification?"
Truth be known, it is little more than a marketing accolade.
And for a while, it worked. Doctors took board certification examinations to market themselves as competent in their field. They would take a written or oral examination created by their peers to demonstrate to others they knew their stuff. And while it remained a lifetime designation, it had some legitimacy. In reality, however, it was up to the residency training programs to train the physicians and verify they knew their stuff. Hospitals used to verify credentials by calling residency programs and verifying doctors participated. They had large credentialing departments that kept everything on file.
But competition between hospitals vying for patients soon grew fierce and hospital marketing departments jumped on the credentialing bandwagon. Soon billboards would appear: "Come to see our board-certified specialists!" and the race was on.
Lawyers joined the fray, too. "My expert witness is better than your expert witness - see how many board certificates he has?"
Truth is, we love this crap. Just look at how many nurse practitioners are "board certified" now!
In the 1960's to 1970's, the American Board of Internal Medicine recognized how lucrative this craze could be, but they had one big problem if they were going to make certifying doctors a full-time business: the number of doctors out there was finite. (It was about that time the board members started paying themselves). They also saw how much money the American Board of Family Medicine, founded in 1969, was generating using 7-year time-limited certifications.
But the ABIM knew internists would be on to them changing the rules for board certification from a lifetime to time-limited credential. So they first tried making a voluntary "super accolade" for internists, called the "Advanced Achievement in Internal Medicine." Needless to say, after four attempts that garnered progressively declining enrollment, the AAIM concept flopped. It was Lynn O. Langdon, MA (a non-physician and Chief Operating Officer of the ABIM) who declared the "End to Voluntary Recertification" and time-limited certification was born with the threat of "uncertain circumstances" if doctors did not participate.
Needless to say, with the help of conflicted members of the ACP who stood to make handsome returns from the Medical Knowledge Self-Assessment Program (MKSAP), they were off to the financial races. And what a race it has proven to be: a nearly $1 billion dollar-a-year enterprise for the entire ACGME.
Unfortunately, no one has ever stopped to study what happens to skilled, competent, board-certified doctors that fail their computerized "re-certification" examination or fail to garner enough "MOC points" to sit for their examination. No one asks about the damage this time-limited credential is having on our physician numbers and access to care. The money is too important to the system.
Not long ago, the chairman of our cardiology division had to relinquish his role as a teacher to medical students because he refused to re-certify in cardiology while also being "certified" in interventional cardiology. (He could keep performing catheterizations and stent placements and remain credentialed thanks to the change in double jeopardy rules that changed just in the nick of time). How many medical students lost out on his experience as a result? Are we happier that medical students are now being taught by younger (time-limited) Board-certified physician instructors rather than life-time certified physicians with decades of experience in the field?
Doctors and nurses know the truth. That's why when seeking out a "quality" physician for their own care, they NEVER ask if a colleague is board-certified since board certification is now a false idol - a hoop to complete whether they're competent, ethical, or not.
We know that it's now far better to ask a trusted colleague or health professional when seeking care because there's much more to being a "quality" physician than holding a computer-generated "certificate."
-Wes
Reference: Fisher WG, Schloss EJ. Medical specialty certification in the United States - a false idol? J Card Electrophys October 2016; 47(1): 37-43.
Wednesday, July 18, 2018
US Physician ABMS Board Certification: From Voluntary to Mandatory
The American Board of Medical Specialties (ABMS) is very careful to claim their version of "Board certification" is a "voluntary process," otherwise, this Chicago-based non-profit 501(c)(6) organization might be accused of anti-trust behavior.
"ABMS Maintenance of Certification" and "ABMS MOC" were registered by the ABMS in the US Patent and Trademark Office August 21, 2007 after filing the terms February 23, 2007.
MOC for ABMS has value.
We also know Ms. Margaret O'Kane, founder and President of the non-profit "National Committee on Quality Assurance" and that created and owns the Healthcare Effectiveness Data and Information Set (HEDIS). HEDIS is a tool used by more than 90 percent of America's health plans to measure performance on "important dimensions of care and service." We also find that Ms. O'Kane was a "public member" of the Board of Directors of the ABMS and advertised the importance of the ABMS MOC program "to patients and the pubic" by video and implies the ABMS board's actions assures improved "outcomes" for patients.
So it should come as no surprise that some of those payers who stand to benefit by limiting patients' access to care (in this case, Blue Cross Blue Shield of Michigan) have made initial ABMS Board certification mandatory for physicians on their panels:
While claiming MOC as a requirement for physicians to receive payments because it assures their "quality," BCBS of Michigan does not demand the same of mid-level providers like physician assistants and nurse practitioners without similar subspecialty training. Additionally, physicians who received their "Board certification" before 1990 and are farthest away from their training are not required to perform ABMS Maintenance of Certification to remain on those same insurance panels, introducing a hypocritical and discriminatory double-standard that financially benefits insurers and hospital systems (more insurance claim denials and cheaper staffing requirements).
ABMS is the puppet of the insurance companies, just as they were the puppets of Big Tobacco in the 60's.
The IRS, FTC, and SEC need to get serious about investigating this ruse.
Why?
It's compromising patient care and our patients' access to care.
-Wes
P.S.: If you haven't contributed already, please consider donating to the legal fund sponsored by Practicing Physicians of America that hopes to bring an end the ABMS Board certification/MOC monopoly nationwide.
"ABMS Maintenance of Certification" and "ABMS MOC" were registered by the ABMS in the US Patent and Trademark Office August 21, 2007 after filing the terms February 23, 2007.
MOC for ABMS has value.
We also know Ms. Margaret O'Kane, founder and President of the non-profit "National Committee on Quality Assurance" and that created and owns the Healthcare Effectiveness Data and Information Set (HEDIS). HEDIS is a tool used by more than 90 percent of America's health plans to measure performance on "important dimensions of care and service." We also find that Ms. O'Kane was a "public member" of the Board of Directors of the ABMS and advertised the importance of the ABMS MOC program "to patients and the pubic" by video and implies the ABMS board's actions assures improved "outcomes" for patients.
So it should come as no surprise that some of those payers who stand to benefit by limiting patients' access to care (in this case, Blue Cross Blue Shield of Michigan) have made initial ABMS Board certification mandatory for physicians on their panels:
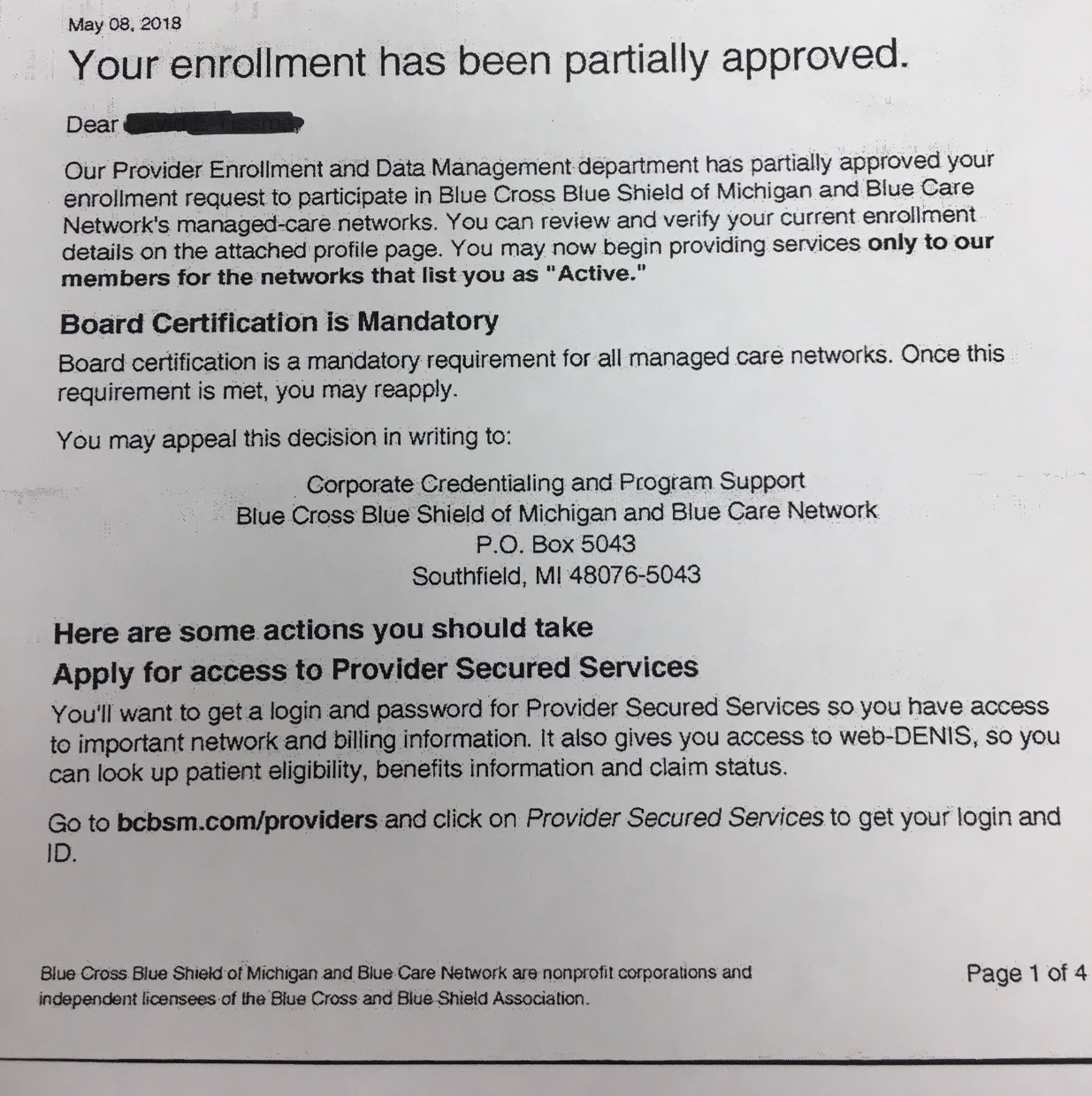 |
| (Click to enlarge) |
While claiming MOC as a requirement for physicians to receive payments because it assures their "quality," BCBS of Michigan does not demand the same of mid-level providers like physician assistants and nurse practitioners without similar subspecialty training. Additionally, physicians who received their "Board certification" before 1990 and are farthest away from their training are not required to perform ABMS Maintenance of Certification to remain on those same insurance panels, introducing a hypocritical and discriminatory double-standard that financially benefits insurers and hospital systems (more insurance claim denials and cheaper staffing requirements).
ABMS is the puppet of the insurance companies, just as they were the puppets of Big Tobacco in the 60's.
The IRS, FTC, and SEC need to get serious about investigating this ruse.
Why?
It's compromising patient care and our patients' access to care.
-Wes
P.S.: If you haven't contributed already, please consider donating to the legal fund sponsored by Practicing Physicians of America that hopes to bring an end the ABMS Board certification/MOC monopoly nationwide.