It has been a busy year for this blog and for doctors in general. While the number of posts have dwindled compared to my earlier experience in this space, I have enjoyed "diving deep" into topics with greater research behind them. Like others, I suspect my impact in the medical blog-o-sphere has been far more influential here than if I had stuck to a conventional medical journal format for publication of these topics. So far, 2015 promises to be no different.
So, for what it's worth, here are my most-read "top ten" blog posts of 2014:
10. The Effects of Maintenance of Certification and Crony Capitalism
9. Paid NEJM Subscriptions: There's No Such Thing As a Free Lunch
8. Reviewing the Regulators
7. The Importance of Demonizing Specialists
6. The New CMS National Coverage Decision for Pacemakers
5. The Business of Testing Physicians
4. For Medical Students, It Seems Nothing Has Changed
3. What Is Non-valvular Atrial Fibrillation?
2. How Much Do Doctors Really Earn? The public's interest in this topic seems insatiable.
1. The ABIM Foundation, Choosing Wisely, and the $2.3 Million Condominium The grand-daddy of them all, with already over 17,100 page views as of today and just posted a little over a week ago.
Yes, I'd say it's been a very productive year indeed.
-Wes
Sunday, December 28, 2014
Wednesday, December 24, 2014
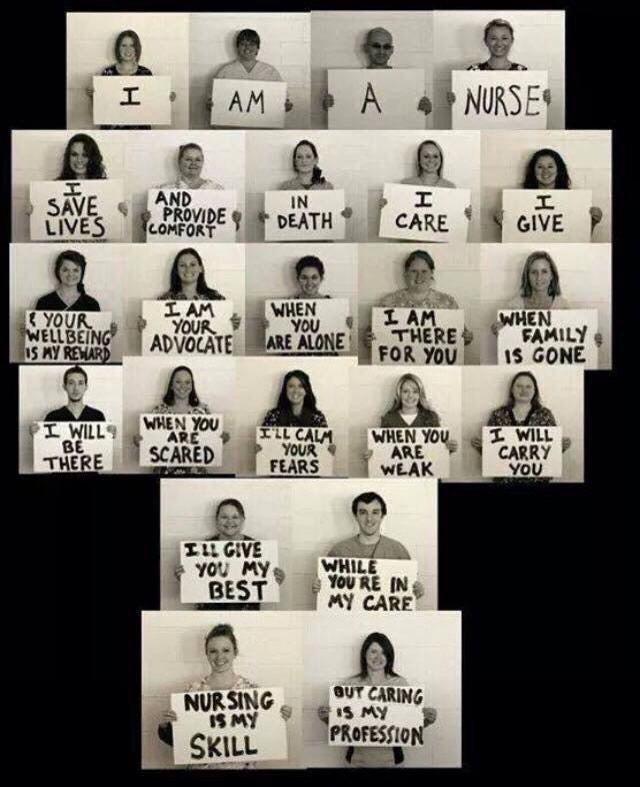
Merry Christmas to All
To every person who finds themselves sick or alone this holiday season. To the many caregivers who toil without recognition this day and the next. May the peace and joy of this holiday season transcend it all as we pause and reflect on what really matters.
Merry Christmas and Happy Holidays to all.
-Wes
Merry Christmas and Happy Holidays to all.
-Wes
Monday, December 22, 2014
Medical Journals Should Disclose Conflicts Just Like Their Authors
In every medical journal, authors must disclose all conflict of interests that might exist to the editors of that journal as a condition of publication. However, as we are increasingly becoming aware, journal editors do not have to disclose payments they receive from outside sources (pharmaceutical industry, special interests, the government) to publish content in their own journal. I think they should.
Medical journals, especially those with large physician "reach," are being used less for scientific endeavors and more for political or marketing agendas. Of course, this is nothing new, in medicine, but it's high time medical journals understand that with the availability of information on the internet, that "special arrangements" with various entities might not remain so private any longer. As I noted in my earlier blog post regarding the simultaneous publication of a non-peer reviewed white paper in the Annals of Internal Medicine and The Lancet and this publication's association to recent revelations concerning the finances of the American Board of Internal Medicine and their Foundation, such a practice risks jeopardizing their scientific credibility, especially if those revelations are found to be credible. Legitimacy is an important asset to medical journals and medical journal editors should be aware that physicians who are increasingly being subject to political agendas are growing increasingly frustrated at this covert practice.
More recently, we've seen the editorial decision of another medical journal, the Journal of the American Medical Association (JAMA), decide to allow the conflict of interests of choosing Press Ganey Chief Medical Officer Thomas H Lee, MD as an editorial author for a discussion surrounding the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) in their 10 Dec 2014 issue. Also, the fact that pointed questions to a webcast supporting the ABIM's MOC process had many questions cherry-picked by the moderators. I have no problem with a journal siding with one opinion or the other provided there is full disclosure about the financial relationships of the authors of the paper AND those of the journal itself. But any legitimate discussion requires the disclosure of real or potential conflicts of interests held by the journal to critically review the credibility of what is published. Any double-standard regarding the disclosure of conflicts of interest should not be tolerated by the medical community, especially by physicians who struggle to improve the care of our patients in our evolving health care system, especially when that health care system appears to be increasingly hostile toward physicians and their patients.
-Wes
Medical journals, especially those with large physician "reach," are being used less for scientific endeavors and more for political or marketing agendas. Of course, this is nothing new, in medicine, but it's high time medical journals understand that with the availability of information on the internet, that "special arrangements" with various entities might not remain so private any longer. As I noted in my earlier blog post regarding the simultaneous publication of a non-peer reviewed white paper in the Annals of Internal Medicine and The Lancet and this publication's association to recent revelations concerning the finances of the American Board of Internal Medicine and their Foundation, such a practice risks jeopardizing their scientific credibility, especially if those revelations are found to be credible. Legitimacy is an important asset to medical journals and medical journal editors should be aware that physicians who are increasingly being subject to political agendas are growing increasingly frustrated at this covert practice.
More recently, we've seen the editorial decision of another medical journal, the Journal of the American Medical Association (JAMA), decide to allow the conflict of interests of choosing Press Ganey Chief Medical Officer Thomas H Lee, MD as an editorial author for a discussion surrounding the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) in their 10 Dec 2014 issue. Also, the fact that pointed questions to a webcast supporting the ABIM's MOC process had many questions cherry-picked by the moderators. I have no problem with a journal siding with one opinion or the other provided there is full disclosure about the financial relationships of the authors of the paper AND those of the journal itself. But any legitimate discussion requires the disclosure of real or potential conflicts of interests held by the journal to critically review the credibility of what is published. Any double-standard regarding the disclosure of conflicts of interest should not be tolerated by the medical community, especially by physicians who struggle to improve the care of our patients in our evolving health care system, especially when that health care system appears to be increasingly hostile toward physicians and their patients.
-Wes
Tuesday, December 16, 2014
The ABIM Foundation, Choosing Wisely®, and the $2.3 Million Condominium
Is it "medically professional" for a non-profit organization to use
physician testing fees to "choose wisely" a $2.3 million luxury
condominium complete with a chauffeur-driven BMW 7-series town car? In my view, obviously not. To most people such an action would conjure up images of hypocrisy, waste, and
corruption.
Yet, after a review of public and tax records, it appears to me this is exactly what has happened.
Background
In 1999 for reasons that are unclear, the American Board of Internal Medicine (ABIM), itself a tax-exempt 501 (c) (3) independent non-profit physician evaluation organization domiciled in Iowa, created (Editor's note 10/20/2015: referenced web page has since been edited by the ABIM Foundation; the original referenced web page can be viewed here) a second non-profit tax-exempt 501 (c) (3) organization, the ABIM Foundation (Foundation), to first define and later promote the term "medical professionalism." Both the ABIM and the Foundation share a common address in Pennsylvania and common officers:
Ten years later after accumulating some $76 million in assets, the Foundation began their hard-to-disagree-with "Choosing Wisely®" campaign to encourage physicians and providers to question the value of medical testing in an effort to eliminate unnecessary tests and procedures. The campaign has grown to include 70 societies and some non-physician organizations, including Consumer Reports, AARP, SEIU, and Univision among others. As part of the campaign, monetary grants from the Robert Wood Johnson Foundation are awarded to institutions willing to "educate practicing physicians about the recommendations from specialty societies, and building physician communication skills to facilitate conversations with their patients about the care they need."
The Money Trail
So how did the ABIM Foundation accumulate all that money? Reviewing public tax records of the ABIM and its Foundation reveals a significant portion of the Foundation's revenues came directly from the ABIM. Recall that ABIM receives 97% of its annual revenues from physician certification (62%) and re-certification fees (35%), with only 14% of these fees going toward physician examination development. In 2007 and 2008 alone, cash grants from the ABIM to its Foundation of $7 million and $6 million respectively were issued. The public records disclosed that $17,360,000 from the ABIM were made to its Foundation in the 7 years ending 6/30/2008. As a three-time participant in the ABIM certification process (candidate #127308), I can attest that to the best of my knowledge physicians were never made aware of this use of the testing fees they paid the ABIM.
The Luxury Condominium
So why did the ABIM Foundation need all this cash from physicians? We can't be certain, but the Foundation disclosed in their 2008 Form 990 that a portion of the
money they received from the ABIM via physicians fees was used to purchase a 2,579 square foot 3-bedroom luxury
condominium (Unit #11NW, in the "Ayer" Building, 210 W. Washington Square, Philadelphia) in December 2007 for $2.3 million. The luxury property borders Washington Square Park of the most historic areas of Philadelphia, across the street from the Tomb of the Unknown Revolutionary War Soldier and the Eternal Flame. The condominium building previously advertised a chauffeur driven Mercedes Benz S-series town car (more pictures here).
Since then, the Foundation has reported "condominium expenses" totaling $850,340 from December 2007 through June 30, 2013 (FY 2008: $42,522, FY 2009: $164,460, FY 2010: 161,957, FY 2011: $165,982, FY 2012: $161,980, FY 2013: $153,439 (most of these reported as "program service expenses")). In my view, these expenses were accrued while the ABIM appears to have been on an inherently unsustainable financial course from 2001 to 2012 with its net asset or fund balances on 6/30/2002 beginning with a negative balance of $10,762,954 and growing to a negative balance of $43,150,390 ending 6/30/2013. Meanwhile, over the same period its shadow organization, the ABIM Foundation, fund balance was $73,841,719 on 6/30/2013.
It should be noted that in the year of the condominium purchase the President and CEO of the ABIM, Christine Cassel, MD, earned $484,883 from the ABIM and $161,627 from the Foundation. Dr. Cassel continues to serve as President and CEO of the National Quality Forum despite a history of other seemingly conflicted financial dealings. Other executives of ABIM that year included F. Daniel Duffy, MD who served as Executive Vice President of the ABIM earning $379,915 from the ABIM, and Cary Sennett, MD, PhD who served as Senior Vice President earning $185,122 from the ABIM and $185,122 from the Foundation and now serves as a Vice President of Anthem, Inc., formerly Wellpoint. That year Dr. Richard Baron, the current President and CEO of the ABIM and Foundation, served as the secretary/treasurer of the ABIM Board earning $59,729 until 7/1/2008 when he became an unpaid Director of the Board. By comparison, according to one reliable source, the median general internal medicine physician salary in the U.S. was $205,441 in 2009.
More Questions
Reviewing the public record on when and where the ABIM Foundation was actually created discloses another discrepancy. We observe that the Foundation has recorded on their tax returns as being founded in 1999 with its "legal domicile" in Iowa, like the ABIM. However, a search for the organization in Iowa comes up empty, while a search in Pennsylvania Department of State (screen shot here) shows the Foundation was actually created in Pennsylvania in 1989. Which is correct?
We should note that non-profits are not required to file financial statements with the state of Iowa, while Pennsylvania requires them. This raises uncomfortable questions. Is the Foundation's Iowa domicile sheltering the sources and uses of its funds? Why does a non-profit promoting "medical professionalism" need to accumulate this much revenue? Is this how the Foundation demonstrates their "medical professionalism" to the public? To whom is the ABIM and Foundation "accountable?" Anyone?
My Call to the ABIM
On 4 December 2014 I contacted the ABIM and requested an explanation regarding the condominium, the ongoing condominium expenses, and the discrepancy of the ABIM Foundation domicile and founding date. Richard Baron, MD, the current President and CEO of the ABIM returned my call and explained the following:
Larger Implications
Sadly, the medical profession has become a house divided. On one side are many non-clinical physicians who have become far removed from patient care and are firmly embedded in the non-profit, academic, and public policy circles making handsome salaries while seeing little problem with coercing their colleagues to pay fees to support their various economic, policy, or personal agendas. In the words of my colleague Jordan Grumet, MD: "they talk about 'accountability' as if they are the ones in the ICU having the family meetings. They pray at the altar of 'quality' yet fail to define the specifics of such a term. They resent 'over treatment' but never have suffered the consequences of not doing enough."
On the other side are the physicians buried in the work-a-day world of patient care, busy doing the best they can for their patients in our increasingly complicated health care system, working as "excellent sheep" as they do their difficult job and try not to rock the boat. While such a dichotomy is not unique to medicine (look to education, the public service sector, and politics, for instance), is ignoring this new reality useful to our profession? Might the unintended consequences of these unaccountable non-profit organizations and revolving-door employment practices with government and business interests be causing unimaginable harm to the integrity and credibility of our profession while simultaneously wasting valuable resources?
It is a shame that most physicians, particularly younger doctors saddled with exorbitant training debt and concerns of job acquisition and job security, are not in a position to protest the actions of the ABIM and its sycophants, particularly since their ability to practice medicine is increasingly tied to these ABIM board certification and their new perpetual maintenance of certification payments. But this is the point, isn't it? Regulatory capture. As these younger doctors gain experience and awaken to the realities of their new health care arena that is increasingly dominated by unaccountable organizations led by non-clinical members of our own profession, we risk creating cynicism in our ranks and physicians who must be more concerned with passing a test than providing direct patient care. Even worse, we risk promoting ourselves, career or cause over the complicated needs of our patients as the divide grows ever deeper. As a result, the brittle credibility and hard-earned trust with our patients is squandered beyond repair. In my opinion, this is what we risk when we have corruption within.
Is this what our profession and the public wants?
I can only hope that practicing US physicians and the public will demand a full accounting of the ABIM and their Foundation's entire financial dealings and non-transparent co-mingling of funds. I hope that Congress decides to investigate the ABIM's role in including their MOC program as a physician quality reporting measure in the Affordable Care Act (see pages 247 and 844-845) to determine its legitimacy in light of these findings. Furthermore, an investigation into possible violations of federal policy on the protection of human subjects (in this case practicing physicians involved in direct patient care) regarding the American Board of Medical Specialties' requirement for practice and patient survey collection for Part IV of their trademarked Maintenance of Certification® program that the ABIM helps conduct should occur, especially in light of lack of informed consent afforded to physicians regarding how the fees and data they collect are used.
It is time we hold the non-clinical members of our own profession that lead these organizations accountable to all physicians and the public at large. Until this occurs, physician-members of every ABIM subspecialty organization that profits from educational content provided to the ABIM should divest themselves and work to create their own, more credible, simplified and transparent life-long learning pathways. The American Association of Clinical Endocrinologists has already set a good example. While I understand that refusing to buck the coercion created by the multimillion dollar ABIM and its Foundation will be difficult, our credibility as stewards of our patients' best interests and the preservation of the integrity of our profession demands nothing less.
-Wes
Acknowledgement
I am indebted to Charles P. Kroll, CPA for his invaluable assistance collecting tax records of the ABIM and ABIM Foundation before 2007 and assisting in the understanding of the nuances of not-for-profit accounting methods. Mr. Kroll provided forensic accounting analysis to the Minnesota attorney general's office during the Medica-Allina scandal and testified at the Minnesota Senate hearing on the matter.
Yet, after a review of public and tax records, it appears to me this is exactly what has happened.
Background
In 1999 for reasons that are unclear, the American Board of Internal Medicine (ABIM), itself a tax-exempt 501 (c) (3) independent non-profit physician evaluation organization domiciled in Iowa, created (Editor's note 10/20/2015: referenced web page has since been edited by the ABIM Foundation; the original referenced web page can be viewed here) a second non-profit tax-exempt 501 (c) (3) organization, the ABIM Foundation (Foundation), to first define and later promote the term "medical professionalism." Both the ABIM and the Foundation share a common address in Pennsylvania and common officers:
"The American Board of Internal Medicine (ABIM) is related to the ABIM Foundation (Foundation) in that The Foundation is the sole voting member of the ABIM. As such, the two organizations share a common president, a common CFO, and a common senior vice president whose base salaries are allocated between ABIM and The Foundation based on the time spent by each executive."To define "medical professionalism," the new Foundation enlisted other members of the non-profit world including the ABIM, the paid "directors" of the Foundation, the Robert Wood Johnson Foundation, the American College of Physicians-American Society of Internal Medicine and the European Federation of Internal Medicine. The group was chaired by Troy Brennan, MD, JD a paid "Director" of the Foundation who was also President and CEO of Brigham and Women's Physician Organization at the time. (He later became the Chief Medical Officer of Aetna in 2006, and now serves as the Executive Vice President and Chief Medical Officer of CVS Caremark). In 2002 this group published a white paper entitled "Medical Professionalism in the New Millenium: A Physician Charter" without peer review in the Annals of Internal Medicine (here) and The Lancet (here). At least the Annals editor, Harold C. Sox, MD mustered the courage to express concerns about the manuscript in his introductory remarks to his readers:
"The introduction contains the following premise: Changes in the health care delivery systems in countries throughout the industrialized world threaten the values of professionalism. The document conveys this message with chilling brevity. The authors apparently feel no need to defend this premise, perhaps because they believe that it is a universally held truth. The authors go further, stating that the conditions of medical practice are tempting physicians to abandon their commitment to the primacy of patient welfare. These are very strong words. Whether they are strictly true for the profession as a whole is almost beside the point. Each physician must decide if the circumstances of practice are threatening his or her adherence to the values that the medical profession has held dear for many millennia."The paper centered on three fundamental principles that the authors claimed defined "medical professionalism:" (1) the primacy of patient welfare, (2) patient autonomy, and a new concept, (3) the principle of social justice - that is, "the medical profession must promote justice in the health care system, including the fair distribution of health care resources." With this definition, physicians could no longer just be unwavering patient advocates concerned with the "primacy of their patient's welfare," they had also had to serve the financial needs of The System of medicine lest they be labeled "medically unprofessional."
Ten years later after accumulating some $76 million in assets, the Foundation began their hard-to-disagree-with "Choosing Wisely®" campaign to encourage physicians and providers to question the value of medical testing in an effort to eliminate unnecessary tests and procedures. The campaign has grown to include 70 societies and some non-physician organizations, including Consumer Reports, AARP, SEIU, and Univision among others. As part of the campaign, monetary grants from the Robert Wood Johnson Foundation are awarded to institutions willing to "educate practicing physicians about the recommendations from specialty societies, and building physician communication skills to facilitate conversations with their patients about the care they need."
The Money Trail
So how did the ABIM Foundation accumulate all that money? Reviewing public tax records of the ABIM and its Foundation reveals a significant portion of the Foundation's revenues came directly from the ABIM. Recall that ABIM receives 97% of its annual revenues from physician certification (62%) and re-certification fees (35%), with only 14% of these fees going toward physician examination development. In 2007 and 2008 alone, cash grants from the ABIM to its Foundation of $7 million and $6 million respectively were issued. The public records disclosed that $17,360,000 from the ABIM were made to its Foundation in the 7 years ending 6/30/2008. As a three-time participant in the ABIM certification process (candidate #127308), I can attest that to the best of my knowledge physicians were never made aware of this use of the testing fees they paid the ABIM.
The Luxury Condominium
 |
| Street View, "The Ayer Buidling," 210 W. Washington Square |
Since then, the Foundation has reported "condominium expenses" totaling $850,340 from December 2007 through June 30, 2013 (FY 2008: $42,522, FY 2009: $164,460, FY 2010: 161,957, FY 2011: $165,982, FY 2012: $161,980, FY 2013: $153,439 (most of these reported as "program service expenses")). In my view, these expenses were accrued while the ABIM appears to have been on an inherently unsustainable financial course from 2001 to 2012 with its net asset or fund balances on 6/30/2002 beginning with a negative balance of $10,762,954 and growing to a negative balance of $43,150,390 ending 6/30/2013. Meanwhile, over the same period its shadow organization, the ABIM Foundation, fund balance was $73,841,719 on 6/30/2013.
It should be noted that in the year of the condominium purchase the President and CEO of the ABIM, Christine Cassel, MD, earned $484,883 from the ABIM and $161,627 from the Foundation. Dr. Cassel continues to serve as President and CEO of the National Quality Forum despite a history of other seemingly conflicted financial dealings. Other executives of ABIM that year included F. Daniel Duffy, MD who served as Executive Vice President of the ABIM earning $379,915 from the ABIM, and Cary Sennett, MD, PhD who served as Senior Vice President earning $185,122 from the ABIM and $185,122 from the Foundation and now serves as a Vice President of Anthem, Inc., formerly Wellpoint. That year Dr. Richard Baron, the current President and CEO of the ABIM and Foundation, served as the secretary/treasurer of the ABIM Board earning $59,729 until 7/1/2008 when he became an unpaid Director of the Board. By comparison, according to one reliable source, the median general internal medicine physician salary in the U.S. was $205,441 in 2009.
More Questions
Reviewing the public record on when and where the ABIM Foundation was actually created discloses another discrepancy. We observe that the Foundation has recorded on their tax returns as being founded in 1999 with its "legal domicile" in Iowa, like the ABIM. However, a search for the organization in Iowa comes up empty, while a search in Pennsylvania Department of State (screen shot here) shows the Foundation was actually created in Pennsylvania in 1989. Which is correct?
We should note that non-profits are not required to file financial statements with the state of Iowa, while Pennsylvania requires them. This raises uncomfortable questions. Is the Foundation's Iowa domicile sheltering the sources and uses of its funds? Why does a non-profit promoting "medical professionalism" need to accumulate this much revenue? Is this how the Foundation demonstrates their "medical professionalism" to the public? To whom is the ABIM and Foundation "accountable?" Anyone?
My Call to the ABIM
On 4 December 2014 I contacted the ABIM and requested an explanation regarding the condominium, the ongoing condominium expenses, and the discrepancy of the ABIM Foundation domicile and founding date. Richard Baron, MD, the current President and CEO of the ABIM returned my call and explained the following:
- Dr. Baron stated that the condominium was purchased as a "investment property" and part of the investment portfolio of the Foundation. He mentioned that real estate holdings were not uncommon with other similar non-profits. The condominium was used for several purposes, including housing ABIM personnel who resided out of state and returned to Philadelphia for meetings, by contractors (for instance, to house an IT team from India), and for off-site retreats and meetings with the Communications Group of the ABIM, for instance. He noted that when ABIM members use the Foundation's condominium, the Foundation is paid $150/night from the ABIM (compared to the "usual" Philadelphia hotel rate of about $190/night) and there was cash flow to the Foundation from the ABIM for the use of their facility.
- After revelations of the luxury condominium were disclosed at a 2 Dec 2014 Pennsylvania Medical Society town hall meeting, Dr. Baron mentioned in passing that the ABIM was putting the condominium up for sale. I asked Dr. Baron the name of the listing agent and the price. He stated he could not comment because "the paperwork was not in order" and the those details had not been finalized because they were advised that the real estate market would be better in the Spring.
- When asked about the high ongoing condominium expenses and the discrepancy about the ABIM Foundation's creation date and domicile, Dr. Baron could not immediately respond but sent this follow-up e-mail 4 Dec 2014 at 2:39PM (CST):
"Hi Dr. Fischer (sic)-
Attached please find the breakdown of the condo expenses. As I explained the depreciation $$ are a required reporting artifact for the condo as a business investment. The other costs are covered by the condo usage fees.
Regarding the 1989/1999 question - In 1999 ABIM Foundation became a separate operating foundation.
Thanks,
Rich
Richard J. Baron, MD
MACP
President and Chief Executive Officer
American Board of Internal Medicine" - In closing, Dr. Baron expressed his willingness to be open to further questions.
- Today I learned that the condominium is now listed with the following description:
"Extremely Spacious Three Bedroom, 3.5 Bath Home at the Ayer Condominium. Tremendous Entertaining Space. 11’7’’ ceiling heights. Bulthaup b-3 kitchen system, Miele and Subzero Appliances. Huge windows with northwest views. High floor offering stupendous sunsets. Gorgeous stone bathrooms. Abundant closet space. One garage parking space included. Concierge, doormen, valets, gym, chauffeur driven BMW 7-Series." (More details here.)
Larger Implications
Sadly, the medical profession has become a house divided. On one side are many non-clinical physicians who have become far removed from patient care and are firmly embedded in the non-profit, academic, and public policy circles making handsome salaries while seeing little problem with coercing their colleagues to pay fees to support their various economic, policy, or personal agendas. In the words of my colleague Jordan Grumet, MD: "they talk about 'accountability' as if they are the ones in the ICU having the family meetings. They pray at the altar of 'quality' yet fail to define the specifics of such a term. They resent 'over treatment' but never have suffered the consequences of not doing enough."
On the other side are the physicians buried in the work-a-day world of patient care, busy doing the best they can for their patients in our increasingly complicated health care system, working as "excellent sheep" as they do their difficult job and try not to rock the boat. While such a dichotomy is not unique to medicine (look to education, the public service sector, and politics, for instance), is ignoring this new reality useful to our profession? Might the unintended consequences of these unaccountable non-profit organizations and revolving-door employment practices with government and business interests be causing unimaginable harm to the integrity and credibility of our profession while simultaneously wasting valuable resources?
It is a shame that most physicians, particularly younger doctors saddled with exorbitant training debt and concerns of job acquisition and job security, are not in a position to protest the actions of the ABIM and its sycophants, particularly since their ability to practice medicine is increasingly tied to these ABIM board certification and their new perpetual maintenance of certification payments. But this is the point, isn't it? Regulatory capture. As these younger doctors gain experience and awaken to the realities of their new health care arena that is increasingly dominated by unaccountable organizations led by non-clinical members of our own profession, we risk creating cynicism in our ranks and physicians who must be more concerned with passing a test than providing direct patient care. Even worse, we risk promoting ourselves, career or cause over the complicated needs of our patients as the divide grows ever deeper. As a result, the brittle credibility and hard-earned trust with our patients is squandered beyond repair. In my opinion, this is what we risk when we have corruption within.
Is this what our profession and the public wants?
I can only hope that practicing US physicians and the public will demand a full accounting of the ABIM and their Foundation's entire financial dealings and non-transparent co-mingling of funds. I hope that Congress decides to investigate the ABIM's role in including their MOC program as a physician quality reporting measure in the Affordable Care Act (see pages 247 and 844-845) to determine its legitimacy in light of these findings. Furthermore, an investigation into possible violations of federal policy on the protection of human subjects (in this case practicing physicians involved in direct patient care) regarding the American Board of Medical Specialties' requirement for practice and patient survey collection for Part IV of their trademarked Maintenance of Certification® program that the ABIM helps conduct should occur, especially in light of lack of informed consent afforded to physicians regarding how the fees and data they collect are used.
It is time we hold the non-clinical members of our own profession that lead these organizations accountable to all physicians and the public at large. Until this occurs, physician-members of every ABIM subspecialty organization that profits from educational content provided to the ABIM should divest themselves and work to create their own, more credible, simplified and transparent life-long learning pathways. The American Association of Clinical Endocrinologists has already set a good example. While I understand that refusing to buck the coercion created by the multimillion dollar ABIM and its Foundation will be difficult, our credibility as stewards of our patients' best interests and the preservation of the integrity of our profession demands nothing less.
-Wes
Acknowledgement
I am indebted to Charles P. Kroll, CPA for his invaluable assistance collecting tax records of the ABIM and ABIM Foundation before 2007 and assisting in the understanding of the nuances of not-for-profit accounting methods. Mr. Kroll provided forensic accounting analysis to the Minnesota attorney general's office during the Medica-Allina scandal and testified at the Minnesota Senate hearing on the matter.
Stop Wasting Doctors' Time (and Money)
From the New York Times today:
In my opinion, there will be much more coming soon about this sordid and very sad MOC story.
-Wes
"To rely solely on memory, especially for rarer illnesses or complicated patients, would be malpractice. Which is why the huge exam that culminates each decade of recertification should be abolished. Memorizing reams of information to be regurgitated in a “secure testing center” is a waste of time and resources, and does not reflect how medicine is practiced. Most doctors agree with having some sort of process that updates and refreshes medical knowledge. But the process has become unmanageable."Unfortunately, the well-meaning physician author of this piece does not mention the additional costs and questionable ethics of the relatively recently expanded four-step Maintenance of Certification® (MOC) process that the American Board of Medical Specialties has trademarked (and the ABIM helps implement), especially as it pertains to the research being performed on working physicians without their consent. Furthermore, the recent revelations that a shadow organization of the ABIM, the ABIM Foundation, purchased a $2.3 million luxury condominium in December 2007 after the new, more onerous MOC requirements were announced in 2005 raises many more very troubling questions about the legitimacy of this program. For instance, is MOC more about improving corporate portfolios than patient outcomes?
In my opinion, there will be much more coming soon about this sordid and very sad MOC story.
-Wes
Saturday, December 13, 2014
Electronic Medical Record and the Threat of Physician Skill Fade
As I watch the business world's fascination with the electronic medical record (EMR) and all of the Big Data that it accumulates, I see more and more processes codified and treatment pathways carefully honed. Only one small thing remains until the computer can tell doctors how to behave based on the developed algorithms: to turn free text in the patient chart into easily-definable binary pushbutton selections, so now, this is being done.
The theory, of course, is for computers to understand doctor's free text and medical decision making. By making a myriad of discrete data entry choices, we are told, recommendations for care can be made based (of course) on the best "evidence-based" guidelines the world has to offer. Data can then be quantified. Physician selections, easily followed and tracked. "Quality measures" (as defined by guidelines) "simply" quantified. This is our latest "New Vision" for health care. And as our nation hurries to implement electronic health care delivery through government mandates and regulations to assure "meaningful use" of computers, the gushing assurances of improved care spews forth from many who stand to profit from the system.
Imagine: doctors won't have to think. They'll just click the buttons and be in compliance. Stay between the lines and you're quality scores will be perfect,. Your care will be impeccable in the eyes of the developer; efficient, timely, thorough.
What could go wrong? After all, the guesswork is gone. The knowledge base clearly defined. The treatment of the disease efficiently rendered. And now, everything can be perfectly quantified.
I should acknowledge that there are clearly efficiencies gained by such a tact. But there is also a downside that really hasn't been seriously considered by most: we risk developing physician skill-fade. This, in turn, introduces a new unforseen risks to our patients since practice freedom is restricted as each algorithm demands conformity rather than innovation, improvisation, and any semblance of risk taking on the patient's behalf. After all, the computer code is optimized for its creator, the health care Iron Triangle, not the patient.
I was struck by a recent article by Nicholas Carr in the Wall Street Journal entitled, "Automation Makes Us Dumb." In it, Mr. Carr describes the benefits and challenges that automation has produced and mentions the EMR:
In fact, who needs doctors at all if care is reduced to point and click? While our new breed of physicians have never known medicine without a computer, will all of their study and preparation to become clinicians at the bedside be rendered moot as these young doctors find themselves little more than data entry clerks? How will we keep them clinically skilled? Homogenized mannequins programmed to respond to regimented scenarios?
Creating disease-directed algorithms might be efficient at treating a medical problem but this does not really treat the patient. With the infinitely variable human condition, might we be fooling ourselves with a false promise of unwavering algorithmic simplicity? Since patients rarely have one health problem but many, do these simplified treatment pathways consider the effects of other confounding ailments? Do our programmers and engineers care?
This myopic vision for medicine is where we are currently heading. Scores of centrally-created computer mandates continue to restrict the freedom of developers to move where computer-aided treatment advances need to go. As we create our linear and static algorithms that are unyielding to nuance or change (and created during a tiny snapshot of history), we should remember these limitations since physicians' freedom to act in the best interest of their patients is lost if doctors become complacent and also financially incentivized to do so. Such restriction might lower costs, but at a risk to patient care.
Realizing computers in medicine are here to stay, I can only hope that in the years ahead as computerized health records develop, a new era of computerized algorithms will evolve that adapt to any number of physician-directed exceptions and exclusions appropriately. Computers and EMRs must inform the physician rather than mandate, instruct rather than impugn, encourage adaptation rather than thwart it, and always facilitate rather than inhibit patient care. This way physician skill-fade will be minimized and a more efficient care delivery that is patient-centered rather than industry-centered can thrive.
-Wes
The theory, of course, is for computers to understand doctor's free text and medical decision making. By making a myriad of discrete data entry choices, we are told, recommendations for care can be made based (of course) on the best "evidence-based" guidelines the world has to offer. Data can then be quantified. Physician selections, easily followed and tracked. "Quality measures" (as defined by guidelines) "simply" quantified. This is our latest "New Vision" for health care. And as our nation hurries to implement electronic health care delivery through government mandates and regulations to assure "meaningful use" of computers, the gushing assurances of improved care spews forth from many who stand to profit from the system.
Imagine: doctors won't have to think. They'll just click the buttons and be in compliance. Stay between the lines and you're quality scores will be perfect,. Your care will be impeccable in the eyes of the developer; efficient, timely, thorough.
What could go wrong? After all, the guesswork is gone. The knowledge base clearly defined. The treatment of the disease efficiently rendered. And now, everything can be perfectly quantified.
I should acknowledge that there are clearly efficiencies gained by such a tact. But there is also a downside that really hasn't been seriously considered by most: we risk developing physician skill-fade. This, in turn, introduces a new unforseen risks to our patients since practice freedom is restricted as each algorithm demands conformity rather than innovation, improvisation, and any semblance of risk taking on the patient's behalf. After all, the computer code is optimized for its creator, the health care Iron Triangle, not the patient.
I was struck by a recent article by Nicholas Carr in the Wall Street Journal entitled, "Automation Makes Us Dumb." In it, Mr. Carr describes the benefits and challenges that automation has produced and mentions the EMR:
In a study conducted in 2007-08 in upstate New York, SUNY Albany professor Timothy Hoff interviewed more than 75 primary-care physicians who had adopted computerized systems. The doctors felt that the software was impoverishing their understanding of patients, diminishing their “ability to make informed decisions around diagnosis and treatment.”But what is the real issue? While the development of treatment rubrics can improve health care efficiency and productivity for their creators, I fear rote implementation of these algorithms will also also atrophy a physician's clinical and reasoning skills. Binary decisions buttons might facilitate note creation and data gathering, but they discourage the use of physical examination (remember that?) and the evaluation of nuance or clinical exceptions. With creation of our current iteration of care pathways and guidelines, there is now little need for exceptional thinkers, only adequate thinkers. What would skill fade look like in medicine? And at what point do the exceptional experienced physicians start becoming vulnerable to skill fade?
Harvard Medical School professor Beth Lown, in a 2012 journal article written with her student Dayron Rodriquez, warned that when doctors become “screen-driven,” following a computer’s prompts rather than “the patient’s narrative thread,” their thinking can become constricted. In the worst cases, they may miss important diagnostic signals.
The risk isn’t just theoretical. In a recent paper published in the journal Diagnosis, three medical researchers—including Hardeep Singh, director of the health policy, quality and informatics program at the Veterans Administration Medical Center in Houston—examined the misdiagnosis of Thomas Eric Duncan, the first person to die of Ebola in the U.S., at Texas Health Presbyterian Hospital Dallas. They argue that the digital templates used by the hospital’s clinicians to record patient information probably helped to induce a kind of tunnel vision. “These highly constrained tools,” the researchers write, “are optimized for data capture but at the expense of sacrificing their utility for appropriate triage and diagnosis, leading users to miss the forest for the trees.” Medical software, they write, is no “replacement for basic history-taking, examination skills, and critical thinking.”
In fact, who needs doctors at all if care is reduced to point and click? While our new breed of physicians have never known medicine without a computer, will all of their study and preparation to become clinicians at the bedside be rendered moot as these young doctors find themselves little more than data entry clerks? How will we keep them clinically skilled? Homogenized mannequins programmed to respond to regimented scenarios?
Creating disease-directed algorithms might be efficient at treating a medical problem but this does not really treat the patient. With the infinitely variable human condition, might we be fooling ourselves with a false promise of unwavering algorithmic simplicity? Since patients rarely have one health problem but many, do these simplified treatment pathways consider the effects of other confounding ailments? Do our programmers and engineers care?
This myopic vision for medicine is where we are currently heading. Scores of centrally-created computer mandates continue to restrict the freedom of developers to move where computer-aided treatment advances need to go. As we create our linear and static algorithms that are unyielding to nuance or change (and created during a tiny snapshot of history), we should remember these limitations since physicians' freedom to act in the best interest of their patients is lost if doctors become complacent and also financially incentivized to do so. Such restriction might lower costs, but at a risk to patient care.
Realizing computers in medicine are here to stay, I can only hope that in the years ahead as computerized health records develop, a new era of computerized algorithms will evolve that adapt to any number of physician-directed exceptions and exclusions appropriately. Computers and EMRs must inform the physician rather than mandate, instruct rather than impugn, encourage adaptation rather than thwart it, and always facilitate rather than inhibit patient care. This way physician skill-fade will be minimized and a more efficient care delivery that is patient-centered rather than industry-centered can thrive.
-Wes
Thursday, December 04, 2014
Vignettes From A Brief Foray Into Knee Surgery
The phone rang one evening and a pleasant voice was on the other end. "Hi, my name is nurse So-and-so and I'm the educational coordinator for your upcoming knee surgery. Do you want to go to the patient orientation session?" she asked. "It's very helpful to go over things before and after your surgery and to answer any questions you might have."
I thought about this. The 11am session was right smack dab in the middle of my clinical day. But I thought it best to attend and agreed.
It is not easy deciding to have an elective surgery, especially one that will sideline you from your vocation for an extended period. Some said I waited too long. Others said you should wait as long as possible. For me: two good years of limping, looking at long halls that kept getting longer and seeing my formerly active social life dwindle spurred me to proceed. It was time to surrender myself to The System.
Unfortunately, clinical demands caused me to arrive 20 minutes late to my pre-op orientation. I entered a room filled with people and their spouses, all arranged in a large semicircle facing a middle-aged nurse educator in the middle of the room. Men and women of all ages - some younger, some older. Some with partners, some without. Teams. Total knee, partial knees, hips galore!
I had no idea.
"Here's and information packet," she said as she handed me an envelope as I became one of the crowd. "I'll review what your missed at the end of the session." I took a seat as discretely as I could.
Surely if they can do this," I pondered, "I can do this."
***
"Take everything off, then wipe yourself down with one of these towelettes, then put this on," she said, handing me a neatly folded hospital gown. "Follow the directions printed here on this diagram: there are eight of these towelettes, four in each package, use one towelette for both arms, one for your chest, one for your back, one for your abdomen, then one for each leg, one for your privates, one for your butt, your wife can help you with your back…"
Welcome to being a patient!
She left and I removed my clothes. Standing buck naked in a cubicle as I changed, quite a "patient-appreciation day." It was clear this was carefully choreographed preparatory dance, held solo by a doctor who stood naked and a bit confused about the intricacies of sterile towelette application to various body parts, then wiping this part and that - especially since she forgot to tell me that the warmed towelettes cooled quickly and their evaporative loss helped redefine the term "shrinkage" as my chemical pre-operative shower concluded.. Then came the comical assembly of the hospital gown he'd seen his patients endure so many times before. In a word: dashing!
***
"Hello, doctor."
I looked up to see an man somewhat older than me, who spoke with an accent - maybe he was from India? - I wasn't sure.
"I am here to shave your leg."
"She's all yours," I said.
And with that a pair of electric shears appeared and he went to work. It was clear he enjoyed his work. "Soon you will look like Miley Cyrus," he said softly, smiling quietly to himself . Looking down at my leg a short while later, I saw a sheen on my legs that I had never seen before - damn thing looked as smooth as a baby's butt. He proudly applied adhesive tape over the area to remove the excess hair. He walked away briefly to throw the tape away and then returned. He leaned over to my wife whispering loudly enough so I could hear: "I'm so sorry," he said shaling his head, "I made a mistake."
My wife, somewhat puzzled, looked briefly concerned.
He grinned: "He looks more like Madonna."
***
"Okay, I discussed the anesthesia plan with your doctor and he and I think the best option for you would be to have a spinal for this procedure, then we'll give you some propofol and you should do fine. First, I'm going to inject you leg above your knee to give you some ongoing pain relief after your surgery. I'm going to use an ultrasound machine to infuse this area, okay?"
"Uh, sure. Less pain, more gain for me!"
I watched as he localized the vascular bundle in my adductor canal using ultrasound, then injected local. It stung just a tiny bit as he local was infused, but wasn't too severe. Piece of cake, I thought.
"Now, I'd like you to sit at the edge of the bed."
I sat dutifully at the edge of the bed, placing my head in this contraption that contained a headrest and was clearly designed for this moment - complete with foot rests and the places to place your hands. As I leaned forward, I could feel him preparing the area on my lower back, draping it with a sterile drape, then feeling for the iliac crests bilaterally. Once, then again. Then…
"You might feel a little electric shock sensation down your leg - let me know…"
And almost instantly, I felt the slightest of electric shock sensations shoot down my left leg. I brought this to his attention. He did something to relieve the mild sensation.
"There, is that better?"
"Yes," I replied, comfortable as ever.
Moments later I could feel both my legs feel warm almost instantly. They helped be lie back in bed. Within seconds, the strangest sensation occurred: paralysis. No matter how hard my brain asked my legs to move, they refused. I felt just below my belly button. Nothing to feel there, either! Paralysis, particularly while you are conscious, is a bizarre sensation. Try as you might you try to move your legs: nothing. Like a Vulcan mind meld that goes bad you try to tell you legs to do anything and… nothing. I was able to feel a tiny piece of my right 2nd toe for a bit - at least I thought I could, but nothing else. I felt oddly peaceful despite it all - probably Versed, I thought.
"We're ready to take him to the OR," they told her as the transporter and anesthesiologist assisted. "Give him a kiss."
I remembered my wife's kiss, and later moving to the OR table, and from the corner of my eye a scrub nurse in an isolation suit that looked like an Ebola isolation outfit. "Can we get him to sleep now?" I heard someone say. "Let me get his systolic above 75 first," another female voice said. "Oh great," I remembered thinking, but somehow didn't care. Clearly it was a team effort. A guy was working on my foley, but I wasn't sure - couldn't feel a thing. Somehow that part scared me the most and it was nothing. Then...
I woke bit later - minutes it seemed. To the right of me was a lady - was it a nurse? - in a lit football helmet-like head gear. What the …? The drape over her face had been removed. Others were similarly garbed: modified Ebola outfits. Cool. I want these in my OR, I thought. Drugs are an amazing thing.
"We're going to move you off the table now, Wes." And they lifted me over to a gurney. I wheeled back to the holding area, feeling victorious. The procedure I had wanted, but dreaded, was over. Now the recovery.
"You can eat when you get upstairs."
I really wasn't that hungry.
***
"Welcome to your new room. I think it's the biggest on the floor!" she exclaimed. I'm here to give you your meds. Can I have your name and date of birth?"
She clicked this and that, then gave be the pills in a small plastic cup - all kinds of them!
"The pain team has a specific regimen of medications they want you on," she explained. Not wanting to rock the boat, especially when it came to pain, I complied. If you need anything, let us know. We'll keep the ICE machine full. Let us know if you think you need more ice. Here's you incentive spirometer - 3200 cc's every hour, okay?
It was a new room, equipped with all the amenities. Classy, welcome, bigger than I needed, but I was sure it would impress the family. I could hear the saline infusion cranking quietly in the background all night. I remembered my days on the ortho ward as an intern and promised to myself: "I'll be damned if I get in-land salt water drowning! Watch the fluids."
A continuous parade of individuals from the hospital, the nurses, the technicians, PT, OT paraded through. "We try to check on you once an hour," I heard them say. I wondered when I'd get sleep. A bit after midnight it finally happened, and with another Norco sleep came easily.
***
05:50AM: "Good morning, I'm hear to draw your blood."
Heck of a wake-up call. She was young, skilled, soft-spoken. She found my vein in an instant. I learned she left home at every day at 5am, made her rounds drawing blood, then went to school.
She came early every morning, then went on her way. It was easier once we knew each other and knew what to expect each day: a confident harpooning.
***
Being a patient is a good exercise for a doctor. You an see what works, and what doesn't. You can appreciate your vulnerability and the vulnerability of your patients. I saw the coldness of the EMR and the distant computer stares as they never looked up, clicking: "Name and date of birth, please." "Tell me your name and date of birth." The another time: "Name?" "Date of birth?"
Like someone taking a mini-mental status exam on a robot.
But I also saw a team of people who were genuinely concerned with my well-being, many of whom were the people you never hear about: the orderlies, the cleaning personnel, the medical assistants, the pharmacists, and food service personnel. Not to say that the nursing, physical therapy and physician staff weren't great (they were), but it was great to see so many people not just doing their jobs, but enjoying them too.
Perhaps more than this, though, there was a humbling revelation: that like our patients, we are aging. The unlimited days of racing to a code or standing in the cath lab correcting an arrhythmia for hours at a time aren't unlimited after all. As a doctor, we've known this intellectually. But as a patient, we see this and come to appreciate this reality first-hand. And as a result, I suppose I've found a new appreciation: an appreciation for what we do and the the brevity of the time we have to do it as a doctor, the wonder of caring for patients, teaching students, and having family and loved ones that have shared this journey with us. Perhaps most of all, becoming a patient gives us a new appreciation for the finite time we have doing what we love here on this earth.
-Wes
I thought about this. The 11am session was right smack dab in the middle of my clinical day. But I thought it best to attend and agreed.
It is not easy deciding to have an elective surgery, especially one that will sideline you from your vocation for an extended period. Some said I waited too long. Others said you should wait as long as possible. For me: two good years of limping, looking at long halls that kept getting longer and seeing my formerly active social life dwindle spurred me to proceed. It was time to surrender myself to The System.
Unfortunately, clinical demands caused me to arrive 20 minutes late to my pre-op orientation. I entered a room filled with people and their spouses, all arranged in a large semicircle facing a middle-aged nurse educator in the middle of the room. Men and women of all ages - some younger, some older. Some with partners, some without. Teams. Total knee, partial knees, hips galore!
I had no idea.
"Here's and information packet," she said as she handed me an envelope as I became one of the crowd. "I'll review what your missed at the end of the session." I took a seat as discretely as I could.
Surely if they can do this," I pondered, "I can do this."
***
"Take everything off, then wipe yourself down with one of these towelettes, then put this on," she said, handing me a neatly folded hospital gown. "Follow the directions printed here on this diagram: there are eight of these towelettes, four in each package, use one towelette for both arms, one for your chest, one for your back, one for your abdomen, then one for each leg, one for your privates, one for your butt, your wife can help you with your back…"
Welcome to being a patient!
She left and I removed my clothes. Standing buck naked in a cubicle as I changed, quite a "patient-appreciation day." It was clear this was carefully choreographed preparatory dance, held solo by a doctor who stood naked and a bit confused about the intricacies of sterile towelette application to various body parts, then wiping this part and that - especially since she forgot to tell me that the warmed towelettes cooled quickly and their evaporative loss helped redefine the term "shrinkage" as my chemical pre-operative shower concluded.. Then came the comical assembly of the hospital gown he'd seen his patients endure so many times before. In a word: dashing!
***
"Hello, doctor."
I looked up to see an man somewhat older than me, who spoke with an accent - maybe he was from India? - I wasn't sure.
"I am here to shave your leg."
"She's all yours," I said.
And with that a pair of electric shears appeared and he went to work. It was clear he enjoyed his work. "Soon you will look like Miley Cyrus," he said softly, smiling quietly to himself . Looking down at my leg a short while later, I saw a sheen on my legs that I had never seen before - damn thing looked as smooth as a baby's butt. He proudly applied adhesive tape over the area to remove the excess hair. He walked away briefly to throw the tape away and then returned. He leaned over to my wife whispering loudly enough so I could hear: "I'm so sorry," he said shaling his head, "I made a mistake."
My wife, somewhat puzzled, looked briefly concerned.
He grinned: "He looks more like Madonna."
***
"Okay, I discussed the anesthesia plan with your doctor and he and I think the best option for you would be to have a spinal for this procedure, then we'll give you some propofol and you should do fine. First, I'm going to inject you leg above your knee to give you some ongoing pain relief after your surgery. I'm going to use an ultrasound machine to infuse this area, okay?"
"Uh, sure. Less pain, more gain for me!"
I watched as he localized the vascular bundle in my adductor canal using ultrasound, then injected local. It stung just a tiny bit as he local was infused, but wasn't too severe. Piece of cake, I thought.
"Now, I'd like you to sit at the edge of the bed."
I sat dutifully at the edge of the bed, placing my head in this contraption that contained a headrest and was clearly designed for this moment - complete with foot rests and the places to place your hands. As I leaned forward, I could feel him preparing the area on my lower back, draping it with a sterile drape, then feeling for the iliac crests bilaterally. Once, then again. Then…
"You might feel a little electric shock sensation down your leg - let me know…"
And almost instantly, I felt the slightest of electric shock sensations shoot down my left leg. I brought this to his attention. He did something to relieve the mild sensation.
"There, is that better?"
"Yes," I replied, comfortable as ever.
Moments later I could feel both my legs feel warm almost instantly. They helped be lie back in bed. Within seconds, the strangest sensation occurred: paralysis. No matter how hard my brain asked my legs to move, they refused. I felt just below my belly button. Nothing to feel there, either! Paralysis, particularly while you are conscious, is a bizarre sensation. Try as you might you try to move your legs: nothing. Like a Vulcan mind meld that goes bad you try to tell you legs to do anything and… nothing. I was able to feel a tiny piece of my right 2nd toe for a bit - at least I thought I could, but nothing else. I felt oddly peaceful despite it all - probably Versed, I thought.
"We're ready to take him to the OR," they told her as the transporter and anesthesiologist assisted. "Give him a kiss."
I remembered my wife's kiss, and later moving to the OR table, and from the corner of my eye a scrub nurse in an isolation suit that looked like an Ebola isolation outfit. "Can we get him to sleep now?" I heard someone say. "Let me get his systolic above 75 first," another female voice said. "Oh great," I remembered thinking, but somehow didn't care. Clearly it was a team effort. A guy was working on my foley, but I wasn't sure - couldn't feel a thing. Somehow that part scared me the most and it was nothing. Then...
I woke bit later - minutes it seemed. To the right of me was a lady - was it a nurse? - in a lit football helmet-like head gear. What the …? The drape over her face had been removed. Others were similarly garbed: modified Ebola outfits. Cool. I want these in my OR, I thought. Drugs are an amazing thing.
"We're going to move you off the table now, Wes." And they lifted me over to a gurney. I wheeled back to the holding area, feeling victorious. The procedure I had wanted, but dreaded, was over. Now the recovery.
"You can eat when you get upstairs."
I really wasn't that hungry.
***
"Welcome to your new room. I think it's the biggest on the floor!" she exclaimed. I'm here to give you your meds. Can I have your name and date of birth?"
She clicked this and that, then gave be the pills in a small plastic cup - all kinds of them!
"The pain team has a specific regimen of medications they want you on," she explained. Not wanting to rock the boat, especially when it came to pain, I complied. If you need anything, let us know. We'll keep the ICE machine full. Let us know if you think you need more ice. Here's you incentive spirometer - 3200 cc's every hour, okay?
It was a new room, equipped with all the amenities. Classy, welcome, bigger than I needed, but I was sure it would impress the family. I could hear the saline infusion cranking quietly in the background all night. I remembered my days on the ortho ward as an intern and promised to myself: "I'll be damned if I get in-land salt water drowning! Watch the fluids."
A continuous parade of individuals from the hospital, the nurses, the technicians, PT, OT paraded through. "We try to check on you once an hour," I heard them say. I wondered when I'd get sleep. A bit after midnight it finally happened, and with another Norco sleep came easily.
***
05:50AM: "Good morning, I'm hear to draw your blood."
Heck of a wake-up call. She was young, skilled, soft-spoken. She found my vein in an instant. I learned she left home at every day at 5am, made her rounds drawing blood, then went to school.
She came early every morning, then went on her way. It was easier once we knew each other and knew what to expect each day: a confident harpooning.
***
Being a patient is a good exercise for a doctor. You an see what works, and what doesn't. You can appreciate your vulnerability and the vulnerability of your patients. I saw the coldness of the EMR and the distant computer stares as they never looked up, clicking: "Name and date of birth, please." "Tell me your name and date of birth." The another time: "Name?" "Date of birth?"
Like someone taking a mini-mental status exam on a robot.
But I also saw a team of people who were genuinely concerned with my well-being, many of whom were the people you never hear about: the orderlies, the cleaning personnel, the medical assistants, the pharmacists, and food service personnel. Not to say that the nursing, physical therapy and physician staff weren't great (they were), but it was great to see so many people not just doing their jobs, but enjoying them too.
Perhaps more than this, though, there was a humbling revelation: that like our patients, we are aging. The unlimited days of racing to a code or standing in the cath lab correcting an arrhythmia for hours at a time aren't unlimited after all. As a doctor, we've known this intellectually. But as a patient, we see this and come to appreciate this reality first-hand. And as a result, I suppose I've found a new appreciation: an appreciation for what we do and the the brevity of the time we have to do it as a doctor, the wonder of caring for patients, teaching students, and having family and loved ones that have shared this journey with us. Perhaps most of all, becoming a patient gives us a new appreciation for the finite time we have doing what we love here on this earth.
-Wes
Wednesday, November 19, 2014
My Interview at AHA 2014 on ABIM's Maintenance of Certification Program
Thanks for C. Michael Gibson, MD for hosting an interview with me on my concerns with the American Board of Medical Specialties (ABMS) / American Board of Internal Medicine's Maintenance of Certification Program earlier today on his Clinical Trial Results website. A direct link to the interview is included here (if you're using a mobile phone, click the "Download video" link on the webpage).
As the physician groundswell of opposition to the ABMS's proprietary MOC program grows, physicians (especially younger physicians) must understand the complex forces that are intervening between the doctor and patient. The ABMS/ABIM Maintenance of Certification Program is just one of these forces. I encourage all doctors to educate themselves by reviewing the materials collected about MOC at changeboardrecert.com. It's an excellent resource from a variety of physician voices around the United States. Overseas doctors, too, should be aware that the ABIM is extending its tentacles there as well (video), all without any independently-verified evidence base upon which to impose their program as a physician quality or patient safety measure. Doctors must understand the importance of becoming more involved in preserving our profession by becoming more politically engaged.
It is interesting that the AMA just adopted the following new "Principles for MOC" in their press release of 10 Nov 2014:
Similarly, the Pennsylvania Medical Society, just released their "statement of principles" for MOC that sound eerily similar:
Neither of these "principles" insist on researching the unintended negative consequences of the MOC program on physicians should they fail to re-certify, especially since failure rates of this program is 22%.
So why have these two prominent organizations suddenly produced these two similar documents? Might it be to distance themselves from anti-trust concerns with MOC that continue to weave themselves through the courts? Might it be because they see the ABIM becoming irrelevant as more revelations of the management of these organizations comes to light? Might the AMA still want to perpetuate the loss of physician autonomy to gain favor with large hospital systems that are being created by our new health care law today?
We must wonder.
These are big issues. For young doctors overwhelmed with the realities of beginning practice, taking another test seems the easier option than confronting these realities. But all of us as treating doctors must not sit idly by as our autonomy is increasingly usurped and corrupted to benefit the system rather protecting the real health care needs of our patients.
-Wes
As the physician groundswell of opposition to the ABMS's proprietary MOC program grows, physicians (especially younger physicians) must understand the complex forces that are intervening between the doctor and patient. The ABMS/ABIM Maintenance of Certification Program is just one of these forces. I encourage all doctors to educate themselves by reviewing the materials collected about MOC at changeboardrecert.com. It's an excellent resource from a variety of physician voices around the United States. Overseas doctors, too, should be aware that the ABIM is extending its tentacles there as well (video), all without any independently-verified evidence base upon which to impose their program as a physician quality or patient safety measure. Doctors must understand the importance of becoming more involved in preserving our profession by becoming more politically engaged.
It is interesting that the AMA just adopted the following new "Principles for MOC" in their press release of 10 Nov 2014:
The MOC principles will now include:On first blush, this seems so promising. But we should appreciate that the ABMS and ABIM was an earlier spin-off of the AMA, making those of us familiar with these facts suspect.
The American Board of Medical Specialties (ABMS) is the organization responsible for developing the MOC process. ABMS works with its 24 member boards in the ongoing evaluation and certification of physicians.
- MOC should be based on evidence and designed to identify performance gaps and unmet needs, providing direction and guidance for improvement in physician performance and delivery of care.
- The MOC process should be evaluated periodically to measure physician satisfaction, knowledge uptake, and intent to maintain or change practice.
- MOC should be used as a tool for continuous improvement.
- The MOC program should not be a mandated requirement for licensure, credentialing, payment, network participation or employment.
- Actively practicing physicians should be well-represented on specialty boards developing MOC.
- MOC activities and measurement should be relevant to clinical practice.
- The MOC process should not be cost-prohibitive or present barriers to patient care. The policy encourages specialty boards to investigate alternative approaches to MOC and directs the AMA to report annually on the MOC process.
AMA policy supports physician accountability, life-long learning and self-assessment. The AMA will continue to work with the appropriate organizations to ensure the MOC process does not disrupt physician practice or reduce the capacity of the overall physician workforce. In June, the AMA and ABMS convened stakeholders in Chicago to discuss Part III of the MOC exam, focusing on the value of MOC Part III and innovative concepts that could potentially enhance or replace the current thinking around the secure exam requirement of MOC.
Similarly, the Pennsylvania Medical Society, just released their "statement of principles" for MOC that sound eerily similar:
The Pennsylvania Medical Society is committed to lifelong learning, cognitive expertise, practice quality improvement, and adherence to the highest standards of medical practice. The Pennsylvania Medical Society supports a process of continuous learning and improvement based on evidence-based guidelines, national standards, and best practices, in combination with customized continuing education.While these "principles" from the AMA and the Pennsylvania Medical Society address many of physicians' concerns regarding these programs, both potentiate the concept of Maintenance of Certification (MOC), despite the many problems we've identified with this "program" to date (see here, here, here, and here for starters).
The Maintenance of Certification (MOC) process should be designed to identify performance gaps and unmet needs, providing direction and guidance for improvement in physician performance and delivery of care.
The Maintenance of Certification (MOC) process should be evaluated periodically to measure physician satisfaction, knowledge uptake and intent to maintain or change practice. Board certificates should have lifetime status, with Maintenance of Certification (MOC) used as a tool for continuous improvement.
The Maintenance of Certification (MOC) program should not be associated with hospital privileges, insurance reimbursements or network participation.
The Maintenance of Certification (MOC) program should not be required for Maintenance of Licensure (MOL).
Specialty boards, which develop Maintenance of Certification (MOC) standards, may approve curriculum, but should be independent from entities designing and delivering that curriculum, and should have no financial interest in the process.
A majority of specialty board members who are involved with the Maintenance of Certification (MOC) program should be actively practicing physicians directly engaged in patient care. Maintenance of Certification (MOC) activities and measurement should be relevant to real world clinical practice.
The Maintenance of Certification (MOC) process should not be cost prohibitive or present barriers to patient care.
Neither of these "principles" insist on researching the unintended negative consequences of the MOC program on physicians should they fail to re-certify, especially since failure rates of this program is 22%.
So why have these two prominent organizations suddenly produced these two similar documents? Might it be to distance themselves from anti-trust concerns with MOC that continue to weave themselves through the courts? Might it be because they see the ABIM becoming irrelevant as more revelations of the management of these organizations comes to light? Might the AMA still want to perpetuate the loss of physician autonomy to gain favor with large hospital systems that are being created by our new health care law today?
We must wonder.
These are big issues. For young doctors overwhelmed with the realities of beginning practice, taking another test seems the easier option than confronting these realities. But all of us as treating doctors must not sit idly by as our autonomy is increasingly usurped and corrupted to benefit the system rather protecting the real health care needs of our patients.
-Wes
Monday, November 17, 2014
J. Rod Gimbel: Crowdsourcing a Consumer Safety Issue
The following is a guest post by J. Rod Gimbel, MD, a cardiac electrophysiologist from Knoxville, TN who has written extensively on the issue of electronic surveillance systems and electromagnetic interference with cardiac implantable electronic devices:
-Wes
I’d like to express my appreciation for allowing me to guest post in this space.This is an important effort that Rod is undertaking on behalf of patients with CIEDs. I hope patients and health care providers will come forward with examples of EAS systems or EAS interference in their locales to assist him in this important consumer safety effort.
This is about crowdsourcing a consumer safety issue; specifically the public safety of consumers who happen to have CIEDs (cardiac implantable electronic devices) such as pacemakers or implantable defibrillators (ICD). Nearly 2 million such consumers (patients) have CIEDs in the U.S. alone. As you know, these devices are susceptible to EMI (electromagnetic interference). Simply put, the lead(s) act like antennas and can pick up stray EMI from any number of sources and cause the device to malfunction by either withholding therapy (no pacing or ICD rescue therapy) or through delivery of inappropriate therapy (delivering pacing output or shocks where none is needed). Either situation can be life threatening.
One source of EMI that can affect a CIED patient is electronic article surveillance system (EAS). Such systems are widely used by retailers (ref) to deter and prevent store theft, a problem commonly referred to as “shrinkage”.
About 8 years ago, an ICD patient that I was caring for received inappropriate shocks from his ICD after being near an EAS system located in a big box retailer. A colleague of mine related a similar situation where a pacemaker dependent patient reported syncope in the proximity of an EAS system after her pacemaker inhibited in response to the EMI from the EAS system. These were two disturbing, potentially life threatening events. In hopes of raising awareness of this serious problem (EAS-CIED interaction), we generated a manuscript detailing the events that was published in 2007 in the Mayo Clinic Proceedings. Notably, the New York Times picked up the story. Others have published similar unfortunate misadventures between patients and EAS systems.
Several common sense recommendations have been made in this area; recommendations that preserve a retailer’s right to deter and reduce theft (a legitimate concern), but still protect CIED patients from adverse interactions with EAS systems. For instance, after receiving reports of several adverse events caused by EAS systems the Food and Drug Administration (FDA) issued a “Safety Communication” and noted:
Beyond this, we and others also suggested:
- Be aware that EAS systems may be hidden/camouflaged in entrances and exits where they are not readily visible in many commercial establishments.
- Do not stay near the EAS system or metal detector longer than is necessary and do not lean against the system.
- Retailers should not "camouflage" the EAS pedestals with advertising as this may prevent customers with devices from recognizing the threat and may actually draw device patients toward the EAS pedestal.
- Retailers should not place goods and services near the EAS systems that effectively encourage the patients to violate the "don't linger, don't lean" dictum that physicians tell patients who have devices.
It seems entirely reasonable to suggest a shared responsibility between medical device professionals, device patients, retailers, and EAS system manufacturers. It was hoped EAS manufactures and retailers would do their part and embrace these simple recommendations and help make retail spaces safe for those with implantable devices. Unfortunately, this does not seem to always be the case.
Figure 1: Bench to "relax" placed adjacent to a camouflaged EAS pedestal at big box retailer.
Figure 2: Chair to "relax" placed adjacent to EAS pedestal while patient waits for prescription to be filled at retail pharmacy store. These pictures were taken in the last several months around the country. Clearly, the juxtaposition of EAS systems and consumer areas may undermine the dictum “don’t linger, don’t lean” and leave device patients in harm’s way. Who then, is responsible for the safety of device patients in this situation?
Figure 3: Complimentary coffee station where device patients might linger placed adjacent to EAS pedestal at big box retailer
Finally, perhaps in an attempt to thwart a determined and “informed shoplifter” who may employ several methods that might undermine the effectiveness of EAS systems, “there are also concerns that some installations are purposefully configured to exceed the rated specifications of the manufacturer, thereby exceeding tested and certified magnetic field levels.” This may increase further the risk of adverse reactions experienced by device patients when near EAS systems.
Now for the crowdsourcing part:
A presentation on this topic (CIED-EAS interactions) to an extra governmental regulatory group helping set standards for the device industry is to be given soon. This presentation will be to a number of interested parties including representatives of the EAS manufactures, device manufactures, and the FDA. As noted above, the “event rate” of these interactions is rather low, but as has been suggested significant under-reporting may obscure the true significance of the problem. It is surely recognize that not everyone has the time or inclination to write up adverse events for publication or inclusion in a database. Perhaps, some events go entirely unrecognized for what they really are, being passed off as “Oh, Mom passed out at the store today, but she’s OK now”.
With your help a strong presentation and case can be made emphasizing CIED-EAS interactions are an important public safety issue. Your voice and concerns can be heard. First off, send pictures where you see EAS systems placed in a manner that might endanger a device patient (like the ones shown above). Cell phone pictures are just fine. Second, if you are a health care provider or patient, please send any “events” that you may have experienced describing an adverse interaction between an EAS system and pacemakers and or ICDs. Please post the items here or send items of interest to J. Rod Gimbel, MD (gimbeljr@gmail.com). Your response is of course appreciated and in confidence and any presentation of the material provided will be anonymized. Upon completion of the presentation, a link will be posted here.
-Wes
Tuesday, November 11, 2014
Happy Veteran's Day
 |
| (Click image to enlarge) |
It's fun to look back and see the the old cath lab equipment - including (dare I say it) the FILM canisters! My, how far we've come!
Here's wishing all of these great doctors and corpsman a Happy Veteran's Day, wherever their paths have led them since.
-Wes
Thursday, November 06, 2014
Excellent Sheep
"I was teaching a class at Yale on the literature of friendship. One day we got around to talking about the importance of being alone. The ability to engage in introspection, I suggested, is the essential precondition for living life of the mind, and the essential precondition for introspection is solitude. Many students took this in for a second - introspection, solitude, the life of the mind, things they had not been asked to think about before - then one of them said, with a dawning sense of self-awareness, "So are you saying that we're all just, like, really excellent sheep?"
All? Surely not. But after twenty-four years in the Ivy League - college at Columbia; a PhD at the same institution, including five years as a graduate instructor; and ten years, altogether, on the faculty at Yale - that was more or less how I had come to feel about it. The system manufactures students who are smart and talented and driven, yes, but also anxious, timid, and lost, with little intellectual curiosity and a stunted sense of purpose: trapped in a bubble of privilege, heading meekly in the same direction, great at what they're doing but with no idea why they're doing it. I published an essay that sketched out a few of these criticisms. Titled "The Disadvantages of an Elite Education," the article appeared in the American Scholar, a small literary quarterly. At best, I thought, it might get a few thousand readers.
Instead, it started to go viral almost the moment it came out. Within a few weeks, the piece had been viewed a hundred thousand times (with many times that number in the months and years to come). Apparently I'd touched a nerve. These were not just the grumblings of an ex-professor. As it turned out from the many emails I began to get, the vast majority from current students and recent graduates, I had evoked a widespread discontent among today's young high achievers - a sense that the system is cheating them out of a meaningful education, instilling them with values they rejected but couldn't somehow get beyond, and failing to equip them to contract their futures."
- William Deresiewicz
"Excellent Sheep: The Miseducation of the American Elite and the Way to a Meaningful Life, Free Press, New York, 2014.Sounds an awful lot like the concerns I hear from medical students, residents, and young physicians today, doesn't it? They are excellent test-takers, rule-followers, and lock-step thinkers, for these things help people succeed in medical school. But add the burdens of seemingly insurmountable debt, regulatory testing and re-testing, and data entry mandates that mean more to their pay than actual visits to the bedside, I wonder how many our our new physicians will be willing to really work to evoke change on behalf of their patients rather than working with the system that drives them to do otherwise.
I worry when we're breeding really excellent sheep, I'd much rather they were breeding cowboys.
-Wes
Tuesday, October 28, 2014
The Wonders of Role Reversal
Another day, another pacemaker, at least so it seemed at first.
The usual greeting the patient, answering the last questions, consent signing, placement of the IV, EKG leads, prepping of the surgical site and initiation of the pre-operative antibiotics were all recent memories. He laid there, smiling, knowing he'd made the right decision after years of struggling with his arrhythmia in other ways. His heart was showing signs of slight weakening and his arrhythmias remained too fast despite a multitude of therapies, so he had agreed to proceed with placement of a biventricular pacemaker with later ablation of his AV node some weeks later after his surgical wound was well-healed.
The nurses and technicians in the room were wonderful, reassuring the patient as they moved him to the narrow procedural table. More wires were connected to monitors and a blood pressure cuff placed. The instrument table laid ready, and the patient's choice of soft rock could be heard faintly in the background. The pre-sedation note was completed and checklists reviewed.
Meanwhile, I donned by lead, bouffant hair net, headlamp, and face mask, then scrubbed for the procedure. Shortly thereafter I turned to open the procedure room door with my backside and was quickly greeted to a hearty "Time Out!" The patient's identity and procedure confirmed, I could see the patient smiling:
"We lawyers like to hear those things," he said. (Yes, he was a lawyer.*)
"Nurse, make sure you give him a ton of sedation - he'll need it, okay?" I joked. We laughed together at the thought.
"1 of Versed and 25 mcg of Fentanyl," the nurse shouted to the control room.
"1 and 25," the control room answered.
He and I had struggled together with his arrhythmia for years, finally agreeing that this option at this stage in his arrhythmia's progression would be best.
I made my way to his side and once again prepped his chest with chlorhexidine prep sticks, letting each dry before the next was applied. The surgical sight was then drapped to provide an island of an orange plastic film surrounded by a sea of blue paper covering. Other drapes were secured and a pocket for instruments was made. "Everybody have lead?" I asked. The x-ray system was enabled, then the pacemaker system analyzer cable, a SiteRite ultrasound probe and Bovie pen made ready. All was set to begin.
"Mr. Jones (not his real name), I'm going to start to numb your skin with the local anesthestic. This will sting," I said.
"Okay..." as he braced himself for inpact. Then:
"Come-on, doc, you can do better than that!..." as if to mock me, jokingly.
"Yes, I can, " I countered, then proceeded to administer more anesthetic to the area. As the area became more anesthetized, his shoulder seemed to relax. No doubt the Versed helped a bit, too.
I continued, locating the appropriate spot, then performing the incision. He was unaware. The pocket was created first, then I found the vein and placed the first lead without a problem. Badda bing, badda boom. Now for the next…
Then, out of the blue:
"Doc, I heard you're having a knee replacement ... "
"Just a partial, I hope ..."
"Hey, I just want to tell you. It's the best thing I ever did. Listen, it's not as bad as you think, but there's quite a bit you have to be ready for… Don't forget to preload the Miralax - that iron supplement before the procedure to slow you down and then the narcotics afterward to stop you up: it's a Machiavellian ploy by those orthopedic surgeons to assure your discomfort."
I chuckled as I thought about this.
"And whatever you do, take the pain medication before physical therapy. I had a physical therapist threaten to fire me when I failed to take the pain medication 45 minutes before therapy. And get rid of all those rugs. It really helps to plan your trips when you get up. Think about what you need and what you might need to limit your trips. I'm telling you, this saved my life. You know I'm writing a book about stuff like this... I'm waiting on the proof. Don't come back too soon. Have you completed your FMLA forms yet?"
"What?"
"FMLA. Look it up. Loads of fun. Anyhow, be nice to your wife - you're gonna need her. Trust me on this..."
And on and on it went: patient treating doctor, until his pacemaker was done. Then, finally, I had a chance to reciprocate:
"I'm closing."
"Thanks, doc, and good luck. You're going to do fine."
-Wes
* ... yes, he gave me permission to tell this story.
The usual greeting the patient, answering the last questions, consent signing, placement of the IV, EKG leads, prepping of the surgical site and initiation of the pre-operative antibiotics were all recent memories. He laid there, smiling, knowing he'd made the right decision after years of struggling with his arrhythmia in other ways. His heart was showing signs of slight weakening and his arrhythmias remained too fast despite a multitude of therapies, so he had agreed to proceed with placement of a biventricular pacemaker with later ablation of his AV node some weeks later after his surgical wound was well-healed.
The nurses and technicians in the room were wonderful, reassuring the patient as they moved him to the narrow procedural table. More wires were connected to monitors and a blood pressure cuff placed. The instrument table laid ready, and the patient's choice of soft rock could be heard faintly in the background. The pre-sedation note was completed and checklists reviewed.
Meanwhile, I donned by lead, bouffant hair net, headlamp, and face mask, then scrubbed for the procedure. Shortly thereafter I turned to open the procedure room door with my backside and was quickly greeted to a hearty "Time Out!" The patient's identity and procedure confirmed, I could see the patient smiling:
"We lawyers like to hear those things," he said. (Yes, he was a lawyer.*)
"Nurse, make sure you give him a ton of sedation - he'll need it, okay?" I joked. We laughed together at the thought.
"1 of Versed and 25 mcg of Fentanyl," the nurse shouted to the control room.
"1 and 25," the control room answered.
He and I had struggled together with his arrhythmia for years, finally agreeing that this option at this stage in his arrhythmia's progression would be best.
I made my way to his side and once again prepped his chest with chlorhexidine prep sticks, letting each dry before the next was applied. The surgical sight was then drapped to provide an island of an orange plastic film surrounded by a sea of blue paper covering. Other drapes were secured and a pocket for instruments was made. "Everybody have lead?" I asked. The x-ray system was enabled, then the pacemaker system analyzer cable, a SiteRite ultrasound probe and Bovie pen made ready. All was set to begin.
"Mr. Jones (not his real name), I'm going to start to numb your skin with the local anesthestic. This will sting," I said.
"Okay..." as he braced himself for inpact. Then:
"Come-on, doc, you can do better than that!..." as if to mock me, jokingly.
"Yes, I can, " I countered, then proceeded to administer more anesthetic to the area. As the area became more anesthetized, his shoulder seemed to relax. No doubt the Versed helped a bit, too.
I continued, locating the appropriate spot, then performing the incision. He was unaware. The pocket was created first, then I found the vein and placed the first lead without a problem. Badda bing, badda boom. Now for the next…
Then, out of the blue:
"Doc, I heard you're having a knee replacement ... "
"Just a partial, I hope ..."
"Hey, I just want to tell you. It's the best thing I ever did. Listen, it's not as bad as you think, but there's quite a bit you have to be ready for… Don't forget to preload the Miralax - that iron supplement before the procedure to slow you down and then the narcotics afterward to stop you up: it's a Machiavellian ploy by those orthopedic surgeons to assure your discomfort."
I chuckled as I thought about this.
"And whatever you do, take the pain medication before physical therapy. I had a physical therapist threaten to fire me when I failed to take the pain medication 45 minutes before therapy. And get rid of all those rugs. It really helps to plan your trips when you get up. Think about what you need and what you might need to limit your trips. I'm telling you, this saved my life. You know I'm writing a book about stuff like this... I'm waiting on the proof. Don't come back too soon. Have you completed your FMLA forms yet?"
"What?"
"FMLA. Look it up. Loads of fun. Anyhow, be nice to your wife - you're gonna need her. Trust me on this..."
And on and on it went: patient treating doctor, until his pacemaker was done. Then, finally, I had a chance to reciprocate:
"I'm closing."
"Thanks, doc, and good luck. You're going to do fine."
-Wes
* ... yes, he gave me permission to tell this story.
Tuesday, October 21, 2014
Reviewing The Regulators
In 1990 the American Board of Medical Specialties (ABMS) and the
American Board of Internal Medicine (ABIM) changed their requirements for
physician board certification from a voluntary life-long designation and
educational process to a time-limited designation lasting 10 years. This
decision to require repeated testing, the public was told, was based
on data from a single
highly flawed retrospective literature review that suggested physician
competence deteriorates over time. Despite this, over the ensuing years hospitals and insurance companies increasingly require physicians to be board certified for credentialing or billing purposes. And as a result of changing the life-long designation of board certification to a temporary one, physicians were left with little choice but to pay for and participate in the ABMS/ABIM MOC program to practice their trade.
In 2005, the ABMS modified their re-certification requirements and created a
program called "Maintenance of Certification" (MOC). This
program required completion of "Practice Improvement Modules" in
addition to the completion of certain knowledge-base testing modules before a
physician could sit for their secure re-certifying examination. This
decision to include "Practice Improvement Modules" was a
unilateral one by the ABMS and its subsidiaries and was never scientifically
challenged or validated by the independent physician community.
This year, the requirements for MOC changed again when allUS
Review of the ABIM’s "research" topics showed they cover a wide range of important clinical care issues including trust, teamwork, ethics, obligations of the Hippocratic Oath, characteristics of internal medicine physicians and their practices, teaching, staffing patterns, electronic health records, clinical skills, and the structure of medical homes. But closer inspection of much of this work shows it was not research, but rather opinion and editorial. Much of the "research" resides behind expensive online paywalls free to the academic community, but expensive for the non-academic physician and public to review. Given these realities, before casting aspersions on physicians' ability to evaluate their own weaknesses, it appears a review of the ABIM's "research" in regard to its clinical legitimacy is in order.
In 2014, the Center for Medicare and Medicaid Services (CMS) published the entire database of $77 billion dollars of payments made to US health care providers in 2012. The data are easily reviewed using a website created by the Wall Street Journal. In an effort to establish the credibility of the ABIM leadership and staff's journal publications as it pertains to the various aspects of medical practice they claim to actively monitor, each author published in the 2014 collection of journal articles published on the ABIM website was cross-referenced with their CMS 2012 Medicare provider payment data.
Methods
The ABIM publishes journal articles authored by ABIM staff and leadership for the years 2000-2014 on its website. The 31 articles published so far in 2014 were randomly selected for review. Each author of each paper was then compared to their 2012 Medicare payment data. If the payment data for a particular author were non-zero, then the total number of inpatient and outpatient new and existing patient encounters were totaled to determine the total 2012 annual Medicare patient care encounters seen by the author. Procedure counts were not added to this total of encounters, since the intent here was to "even the playing field" between "proceduralists" and hospital- or office-based clinicians in terms of the number of patient contact episodes they had each year. In the event more than one physician author's first and last names were identical, the source article was reviewed to assure the proper physician data was obtained based on their city, state, or academic institution.
Authors designated as employees of ABIM, those with acknowledged conflicts of interest or those with non-academic or policy affiliations were also recorded. The average, median and standard deviation of 2012 Medicare payments and patient encounters were then calculated.
As a point of reference, the author of this blog post received a total of $163,184.55 in Medicare payments representing 529 patient encounters (298+75+13 established outpatient visits, 31 outpatient new visits, 82+14 initial hospital/inpatient care and 16 subsequent hospital care visits) according to the 2012 Medicare database. This number of encounters represented 1.5 days of outpatient clinic visits per week in 2012 (personal data) as well as inpatient patient care encounters payments received from Medicare patients. This encounter volume represented 42% of this author’s total number of clinical encounters billed in 2012 (personal data).
Results
Thirty-one articles published by the ABIM staff and leadership in 2014 (so far) represented work by 150 authors. Of the 31 articles published on the ABIM's website to date for 2014, ten of them (33%) were published solely by ABIM employees or leadership. Only 80 of the 150 authors held an MD degree. The authors were a heterogeneous mix of US and non-US physicians, one veterinarian, nurses, students, statisticians, researchers, representatives from National Board of Medical Examiners, Center for Medicare and Medicaid Services, the Urban League, the Foundation for Advancement of International Medical Education and Research, Mathematica Policy Research, Inc., the National Collaborative for Improving Primary Care Through Industrial and Systems Engineering, the VA medical system, staff members of the American Board of Internal Medicine Foundation, and others from Consumer Reports Health.
Clinical Involvement
Of physicians with an MD degree, the average 2012 Medicare payment amount was $18,196.97 ± $68,220.55 (median $0). Only thirty-seven of the 80 physician authors (46%) had Medicare payments paid to them in 2012. Three authors had payments exceeding $100,000 in 2012 while the vast majority (30 of the 37) received under $25,000. This average payment amount corresponded to an average of 131 ± 308 patient encounters (median 0) for the entire year 2012.
If all of the authors were included in the analysis, the average 2012 Medicare payment was $9705.05 ± $50,502.95. The median Medicare payment to the authors published in 2014 to date was $0. The average number of patient encounters per year in 2014 was 70 ± 234. The median number of patient encounters in 2012 by the authors published to date was 0.
The entire spreadsheet (pdf) of the 2012 Medicare payment and encounter data by each author that published with ABIM leadership and staff in 2014 can be reviewed here.
Discussion
This study is the first to cross-reference a portion of ABIM publishing authors to the 2012 Medicare provider payment database. While Medicare payment data might not represent the full workload of today's clinical physicians, it is the most complete database of US physician clinical work performed on patients in the United States published to date.
The ABMS/ABIM's Maintenance of Certification program has been criticized by many working physicians as onerous, expensive, time-consuming and a poor reflection of physician quality. In his response to physician concerns over the MOC process, the President and CEO of the ABIM stated:
Dramatic changes to the health care landscape have occurred over the past five years. If the mission of the ABIM is to truly certify internists who with “skills and attitudes essential for excellent patient care," we are left to question the legitimacy of recommendations made by physicians who no longer care for patients in today’s health care arena. The ABIM seems content with making recommendations to physicians while being woefully inxperienced about the challenges that face internists today. In fact, the data presented in their work confirms that physician quality is being regulated by an unqualified body.
While some might argue that regimented study and time-consuming non-clinical data acquisitions are required to assure physician quality, it remains quite possible that such a dishonest and lopsided approach will backfire as physicians refuse to participate in this process or retire early from medicine just as more patients are entering our health care system. Burdening clinical physicians with unrealistic and unproven demands for non-clinical tasks detracts from needed patient care. Recall that only three of the physicians included in the author list of ABIM's 2014 publications received over $100,000 of Medicare payments while 30 of 37 physicians in the published articles in 2014 received less than $25,000. Might the recommendations and data that the ABIM is making available to hospital groups and insurance organizations be seriously flawed?
Even a cursory review of the background of the authors of several published works of the ABIM staff and leadership reviewed suggests a troubling narrative. For instance, one article included with the ABIM's 2014 list of journal articles is entitled "Internists' attitudes about assessing and maintaining clinical competence" (J General Int Med 2014; 29(4):608-614). While this title might seem reassuring to the public that the ABIM is serious about their mission, their credibility becomes suspect when closer inspection of the background of the authors revealed only one of the six authors had any clinical encounters in 2012 and another author was a veterinarian. In another article entitled "Time to trust: longitudinal integrated clerkships and entrustable professional activities," (Academic Medicine, 89(2), pp 201-4) none of the authors received payments for patient care in 2012 and the authors acknowledge the ideas presented were provided by two political "think tanks." Should these be the people we entrust to develop clerkship ideals and "entrustable professional activities" (whatever that is) for our future physicians?
We should note that despite fourteen years of articles on the ABIM's website, none of the ABIM’s "research" has ever evaluated any negative consequence of their MOC program. Rather, these ABIM papers "drives and informs" additional unsubstantiated "program development" like a public relations firm. Without independent assessment of their practices, it remains completely possible that the MOC process causes more harm than benefit to actual patient care delivery as a result.
The Medicare payment data of ABIM authors also begs the question, how are the ABIM physicians and legislators spending their time? It is apparent that most physician members of the ABIM are not involved in clinical care. Given the conflicts of interest mentioned in the various citations, physician quality assurance is not the ABIM's priority. Perhaps the physician members of the ABIM would have more credibility advising struggling doctor-employees on beefing up their curriculum vitae, earning consulting fees, perfecting public relations skills, and creating multiple income streams since their annual revenue take with their MOC program implementation went from $46,131,129 in 2010 to $55,625,925 in 2012 (Data from the 2011 and 2013 IRS Form 990 published on guidestar.org/). Given these data, it is appears that the ABIM is more concerned about padding their resume to (1) create and air of legitimacy, (2) serve a political agenda, and (3) to provide a smoke screen for the high salaries of their board members.
Clearly, busy front-line full-time practicing physicians do not have the time for creating publishing mills or for scientifically meaningless survey collection. Patients want capable practicing physician availability, not survey collectors. Assuring physician quality should not be about creating and funding a political action committee subservient to a political agenda, but rather understanding the challenges physicians face in their workplace and knowledge base and working collaboratively to offer continuous professional improvement.
Limitations
There are several limitations to this study. First, because the CMS Medicare payment database does not capture work performed on patients under the age of 65, the database does not accurately reflect the total clinical work load a physician performs each year. Physicians who do not accept Medicare for payment would not appear on this database. However, since older patients commonly access our health care system more frequently as they age, it would be expected that internists writing policy for health care delivery would participate in the Medicare government program. Second, the 2012 Medicare payment data reviewed does not correlate to the year the articles were published in the literature. However, one would expect that experienced physicians who changed the testing requirements for MOC in 2014 would have recent direct patient care experience to appreciate the many factors that impact physicians today. Finally, reviewing only one year's literature published on the ABIM's website might have introduced sampling bias. Still, the sampling of the most recent year offers the advantage of reviewing articles that might affect upcoming policy decisions.
Conclusions
Physicians are not above proving their competence and establishing quality standards, especially if those standards are scientifically sound and transparent. The legitimacy of the MOC process to assure physician quality should be called into question based on a careful literature review of the many conflicts exposed by this review and the limited recent clinical experience of those that contribute to their evidence base. Citing numerous publications to legitimize the MOC program creates the illusion that this process of insuring quality care and has been vetted by actual scientific data. Nothing could be further from the truth.
-Wes
This year, the requirements for MOC changed again when all
"There is a good deal of research demonstrating the
value of MOC: from the validity of the examination, to the importance of
independent assessments – clinicians are not good at evaluating their own
weaknesses. All of this research drives and informs our program requirements
and product development."
Review of the ABIM’s "research" topics showed they cover a wide range of important clinical care issues including trust, teamwork, ethics, obligations of the Hippocratic Oath, characteristics of internal medicine physicians and their practices, teaching, staffing patterns, electronic health records, clinical skills, and the structure of medical homes. But closer inspection of much of this work shows it was not research, but rather opinion and editorial. Much of the "research" resides behind expensive online paywalls free to the academic community, but expensive for the non-academic physician and public to review. Given these realities, before casting aspersions on physicians' ability to evaluate their own weaknesses, it appears a review of the ABIM's "research" in regard to its clinical legitimacy is in order.
In 2014, the Center for Medicare and Medicaid Services (CMS) published the entire database of $77 billion dollars of payments made to US health care providers in 2012. The data are easily reviewed using a website created by the Wall Street Journal. In an effort to establish the credibility of the ABIM leadership and staff's journal publications as it pertains to the various aspects of medical practice they claim to actively monitor, each author published in the 2014 collection of journal articles published on the ABIM website was cross-referenced with their CMS 2012 Medicare provider payment data.
Methods
The ABIM publishes journal articles authored by ABIM staff and leadership for the years 2000-2014 on its website. The 31 articles published so far in 2014 were randomly selected for review. Each author of each paper was then compared to their 2012 Medicare payment data. If the payment data for a particular author were non-zero, then the total number of inpatient and outpatient new and existing patient encounters were totaled to determine the total 2012 annual Medicare patient care encounters seen by the author. Procedure counts were not added to this total of encounters, since the intent here was to "even the playing field" between "proceduralists" and hospital- or office-based clinicians in terms of the number of patient contact episodes they had each year. In the event more than one physician author's first and last names were identical, the source article was reviewed to assure the proper physician data was obtained based on their city, state, or academic institution.
Authors designated as employees of ABIM, those with acknowledged conflicts of interest or those with non-academic or policy affiliations were also recorded. The average, median and standard deviation of 2012 Medicare payments and patient encounters were then calculated.
As a point of reference, the author of this blog post received a total of $163,184.55 in Medicare payments representing 529 patient encounters (298+75+13 established outpatient visits, 31 outpatient new visits, 82+14 initial hospital/inpatient care and 16 subsequent hospital care visits) according to the 2012 Medicare database. This number of encounters represented 1.5 days of outpatient clinic visits per week in 2012 (personal data) as well as inpatient patient care encounters payments received from Medicare patients. This encounter volume represented 42% of this author’s total number of clinical encounters billed in 2012 (personal data).
Results
Thirty-one articles published by the ABIM staff and leadership in 2014 (so far) represented work by 150 authors. Of the 31 articles published on the ABIM's website to date for 2014, ten of them (33%) were published solely by ABIM employees or leadership. Only 80 of the 150 authors held an MD degree. The authors were a heterogeneous mix of US and non-US physicians, one veterinarian, nurses, students, statisticians, researchers, representatives from National Board of Medical Examiners, Center for Medicare and Medicaid Services, the Urban League, the Foundation for Advancement of International Medical Education and Research, Mathematica Policy Research, Inc., the National Collaborative for Improving Primary Care Through Industrial and Systems Engineering, the VA medical system, staff members of the American Board of Internal Medicine Foundation, and others from Consumer Reports Health.
Clinical Involvement
Of physicians with an MD degree, the average 2012 Medicare payment amount was $18,196.97 ± $68,220.55 (median $0). Only thirty-seven of the 80 physician authors (46%) had Medicare payments paid to them in 2012. Three authors had payments exceeding $100,000 in 2012 while the vast majority (30 of the 37) received under $25,000. This average payment amount corresponded to an average of 131 ± 308 patient encounters (median 0) for the entire year 2012.
If all of the authors were included in the analysis, the average 2012 Medicare payment was $9705.05 ± $50,502.95. The median Medicare payment to the authors published in 2014 to date was $0. The average number of patient encounters per year in 2014 was 70 ± 234. The median number of patient encounters in 2012 by the authors published to date was 0.
The entire spreadsheet (pdf) of the 2012 Medicare payment and encounter data by each author that published with ABIM leadership and staff in 2014 can be reviewed here.
Discussion
This study is the first to cross-reference a portion of ABIM publishing authors to the 2012 Medicare provider payment database. While Medicare payment data might not represent the full workload of today's clinical physicians, it is the most complete database of US physician clinical work performed on patients in the United States published to date.
The ABMS/ABIM's Maintenance of Certification program has been criticized by many working physicians as onerous, expensive, time-consuming and a poor reflection of physician quality. In his response to physician concerns over the MOC process, the President and CEO of the ABIM stated:
"ABIM's mission is to enhance the quality
of health care by certifying internists and subspecialists who demonstrate the
knowledge, skills and attitudes essential for excellent patient care."
Dramatic changes to the health care landscape have occurred over the past five years. If the mission of the ABIM is to truly certify internists who with “skills and attitudes essential for excellent patient care," we are left to question the legitimacy of recommendations made by physicians who no longer care for patients in today’s health care arena. The ABIM seems content with making recommendations to physicians while being woefully inxperienced about the challenges that face internists today. In fact, the data presented in their work confirms that physician quality is being regulated by an unqualified body.
While some might argue that regimented study and time-consuming non-clinical data acquisitions are required to assure physician quality, it remains quite possible that such a dishonest and lopsided approach will backfire as physicians refuse to participate in this process or retire early from medicine just as more patients are entering our health care system. Burdening clinical physicians with unrealistic and unproven demands for non-clinical tasks detracts from needed patient care. Recall that only three of the physicians included in the author list of ABIM's 2014 publications received over $100,000 of Medicare payments while 30 of 37 physicians in the published articles in 2014 received less than $25,000. Might the recommendations and data that the ABIM is making available to hospital groups and insurance organizations be seriously flawed?
Even a cursory review of the background of the authors of several published works of the ABIM staff and leadership reviewed suggests a troubling narrative. For instance, one article included with the ABIM's 2014 list of journal articles is entitled "Internists' attitudes about assessing and maintaining clinical competence" (J General Int Med 2014; 29(4):608-614). While this title might seem reassuring to the public that the ABIM is serious about their mission, their credibility becomes suspect when closer inspection of the background of the authors revealed only one of the six authors had any clinical encounters in 2012 and another author was a veterinarian. In another article entitled "Time to trust: longitudinal integrated clerkships and entrustable professional activities," (Academic Medicine, 89(2), pp 201-4) none of the authors received payments for patient care in 2012 and the authors acknowledge the ideas presented were provided by two political "think tanks." Should these be the people we entrust to develop clerkship ideals and "entrustable professional activities" (whatever that is) for our future physicians?
We should note that despite fourteen years of articles on the ABIM's website, none of the ABIM’s "research" has ever evaluated any negative consequence of their MOC program. Rather, these ABIM papers "drives and informs" additional unsubstantiated "program development" like a public relations firm. Without independent assessment of their practices, it remains completely possible that the MOC process causes more harm than benefit to actual patient care delivery as a result.
The Medicare payment data of ABIM authors also begs the question, how are the ABIM physicians and legislators spending their time? It is apparent that most physician members of the ABIM are not involved in clinical care. Given the conflicts of interest mentioned in the various citations, physician quality assurance is not the ABIM's priority. Perhaps the physician members of the ABIM would have more credibility advising struggling doctor-employees on beefing up their curriculum vitae, earning consulting fees, perfecting public relations skills, and creating multiple income streams since their annual revenue take with their MOC program implementation went from $46,131,129 in 2010 to $55,625,925 in 2012 (Data from the 2011 and 2013 IRS Form 990 published on guidestar.org/). Given these data, it is appears that the ABIM is more concerned about padding their resume to (1) create and air of legitimacy, (2) serve a political agenda, and (3) to provide a smoke screen for the high salaries of their board members.
Clearly, busy front-line full-time practicing physicians do not have the time for creating publishing mills or for scientifically meaningless survey collection. Patients want capable practicing physician availability, not survey collectors. Assuring physician quality should not be about creating and funding a political action committee subservient to a political agenda, but rather understanding the challenges physicians face in their workplace and knowledge base and working collaboratively to offer continuous professional improvement.
Limitations
There are several limitations to this study. First, because the CMS Medicare payment database does not capture work performed on patients under the age of 65, the database does not accurately reflect the total clinical work load a physician performs each year. Physicians who do not accept Medicare for payment would not appear on this database. However, since older patients commonly access our health care system more frequently as they age, it would be expected that internists writing policy for health care delivery would participate in the Medicare government program. Second, the 2012 Medicare payment data reviewed does not correlate to the year the articles were published in the literature. However, one would expect that experienced physicians who changed the testing requirements for MOC in 2014 would have recent direct patient care experience to appreciate the many factors that impact physicians today. Finally, reviewing only one year's literature published on the ABIM's website might have introduced sampling bias. Still, the sampling of the most recent year offers the advantage of reviewing articles that might affect upcoming policy decisions.
Conclusions
Physicians are not above proving their competence and establishing quality standards, especially if those standards are scientifically sound and transparent. The legitimacy of the MOC process to assure physician quality should be called into question based on a careful literature review of the many conflicts exposed by this review and the limited recent clinical experience of those that contribute to their evidence base. Citing numerous publications to legitimize the MOC program creates the illusion that this process of insuring quality care and has been vetted by actual scientific data. Nothing could be further from the truth.
-Wes
What Signs Would Bureaucrats and Regulators Hold Up?
Nice to see front-line health care workers finding their voice.
I wonder what signs our health care bureaucrats and regulators would hold up?
-Wes
Thursday, September 25, 2014
The Last Reprogramming
He had called the other day to update me up on his condition. He did not sound upset, but resolute. "They offered me peritoneal dialysis," he said, "but I decided against it and figured I'd just let nature take its course. The hospice people are so wonderful - I've got things all set here at home, but I have two questions. What should I do about my warfarin? You know, I just don't want to have a stroke. And what I do about my defibrillator?"
We were colleagues once and grew to be friends later when life's circumstances brought us together. He, a revered senior neurologist and me, a relatively new doctor in town. I could remember overhearing his heated discussions about administrative snafus with colleagues in the hall, or watching a horde of residents and medical students following him into a patient's room to teach at the bedside.
"Of course he didn't want a stroke," I thought.
So we decided to keep the coumadin and let him continue his daily INR checks at home and to turn off just the tachyarrhythmia detections on his biventricular defibrillator.
"I'll come over tomorrow and we'll turn it off," I said.
There was a brief silence, perhaps because of momentary disbelief that I'd do such a thing. Then he proceeded to give me detailed directions and landmarks to watch for on my way over. "I'm sure I can find it," I said thanking him.
So the next afternoon after most of the day's events had finished, I grabbed the programmer and drove to his home. It was an unusually beautiful day - mid 70's, sunny - as if Someone had wanted it that way. There in the yard, was his wife, wearing a large-brimmed hat and holding a hose while pretending to water the shrubs. She came over to greet me: "Thanks so much for coming over," she said, "I know this means so much to him." Then she realized she was still holding the hose. "Oh, I'm so sorry, it's just that someone has to try to keep the place up," she said, voice cracking.
The "place," of course, was beautiful. A majestic grande dame of a house - one I would later learn they had occupied for the past 44 years and bought when they were "just kids on the block." It was meticulousy kept, stately. I entered with his wife and noticed a shadowy figure two rooms away sitting at the edge of a mechanized hospital bed. The bed was placed in what must have been his study with a large bay window with a couch next to it. A reading lamp was over the head of the bed and the walls held books from the floor to ceiling with icons and statues, likely from other, more active time.
"Thanks for coming, Wes," he said, looking up.
"How are you feeling?" I asked, somewhat stupidly.
"Pretty good, considering everything. See? My legs aren't quite so swollen and my abrasions all have eschars on them," he noted as only a doctor could.
"Is there a plug nearby?" and he proceeded to point me the way so I could plug in the programmer to do my job while he explained the device to his wife. The process was quick and I interrogated his defibrillator, then turned off the tachyarrhythmia detections, therapies and now needless alarms. "There, that didn't take long. All done," I said.
There was a moment of silence as I sat with this man whom I known for so long. Like a wise sage and hospitable host, it was clear he wanted to talk for a bit, so I slowed my exit.
"You know, I've always appreciated your frankness about my condition," he said. "You're a lot like me in many ways, I think. You never overstepped, let me have control, to manage things like I wanted to, and I've always appreciated that," he said.
Embarassed by his frankness, I wondered what to say. At a loss for words, I told him how much I enjoyed meeting his family, wife, daughters, and grand-daughters recently in the hospital. He looked puzzled, forgetting. "You know, that day I brought my daughter in your room with them?" His eyes brightened and his smile widened as he remembered.
"Oh, yes! That was wonderful! How fast times flies, doesn't it?" he said.
"You know, I wrote about that day in my blog," I mentioned, ".. and included some pictures of my daughter from 10 years ago - about what she thought about medicine - can I show you?"
"Of course!"
So I showed him the picture and we shared our thoughts about family. Then, to make reading from my iPhone easier, I read him the post I'd written about that day. We talked about family and what they meant to each of us. And then he shared with me another nugget, that he grew to become a writer, too.
"You know, I spent some time and wrote an autobiography for my kids not too long ago - over a hundred pages - about everything I could remember - from my earliest years as a child, about my immigrant father and American mother. My father made it as a successful lawyer - came over from eastern Europe - I even know the ship - I remember the picture of him standing there with his hat..., and I wrote about my family, influential teachers in grade school, fellow professors, and people that I knew throughout the years - everything. You should do that, too, you know. I'm so glad I did. I gave them to my kids and even made some some extra copies - maybe for the grandkids, in case they want it someday..." He looked away to see his wife leave the room, trying not to be noticed as tears filled her eyes once more. She didn't want to him to see her this way.
He stared down at the floor beneath his swollen feet, then continued.
"You know, it was therapeutic for me to write that autobiography. After all, what we do is terribly isolating for the most part. No one understands that. Like you do your procedural stuff and I do my diagnosing. We do most of it all alone, with no one else there. Just the patient and the doctor. Wonderful, to be sure, but isolating. So many memories. I guess it helped me to put some of those feelings and the thoughts I had about those I loved into words. It's hard to capture it all..."
He looked up from the floor and stared in my eyes. "Thank you," he said extending his hand.
I sat motionless for a bit digesting the gravity of his words, lost in them before I saw his hand. Once I noticed, I lept up to shake it and gave him a long hug to his increasingly skeletal frame. It was a brief moment to share together once more and one I now realized I had done too infrequently with other patients in a similar circumstance. Here he was, an incredible man who'd given so much to his family, fellow colleagues and patients, now teaching me once more so much about life as a doctor, about grace, and about real love. Just the two of us, isolated again, but as friends.
With great reluctance I packed things up and found his wife on my way out. "Thank you," she whispered with swollen eyes, "I just don't want him to be in pain."
"He's going to be fine," I told her, "... perfectly fine, especially now. He's such a wonderful guy." She smiled and opened the door.
As I drove away I realized we probably won't see each other again - his remaining time here will be saved for others now. There were so many thoughts, so much to remember, so much still to learn. Perhaps because I'd been through something like this before I was more prepared - it's never easy - but I still felt okay about it all - not sad - confident that we did the right thing...
... together.
-Wes
We were colleagues once and grew to be friends later when life's circumstances brought us together. He, a revered senior neurologist and me, a relatively new doctor in town. I could remember overhearing his heated discussions about administrative snafus with colleagues in the hall, or watching a horde of residents and medical students following him into a patient's room to teach at the bedside.
"Of course he didn't want a stroke," I thought.
So we decided to keep the coumadin and let him continue his daily INR checks at home and to turn off just the tachyarrhythmia detections on his biventricular defibrillator.
"I'll come over tomorrow and we'll turn it off," I said.
There was a brief silence, perhaps because of momentary disbelief that I'd do such a thing. Then he proceeded to give me detailed directions and landmarks to watch for on my way over. "I'm sure I can find it," I said thanking him.
So the next afternoon after most of the day's events had finished, I grabbed the programmer and drove to his home. It was an unusually beautiful day - mid 70's, sunny - as if Someone had wanted it that way. There in the yard, was his wife, wearing a large-brimmed hat and holding a hose while pretending to water the shrubs. She came over to greet me: "Thanks so much for coming over," she said, "I know this means so much to him." Then she realized she was still holding the hose. "Oh, I'm so sorry, it's just that someone has to try to keep the place up," she said, voice cracking.
The "place," of course, was beautiful. A majestic grande dame of a house - one I would later learn they had occupied for the past 44 years and bought when they were "just kids on the block." It was meticulousy kept, stately. I entered with his wife and noticed a shadowy figure two rooms away sitting at the edge of a mechanized hospital bed. The bed was placed in what must have been his study with a large bay window with a couch next to it. A reading lamp was over the head of the bed and the walls held books from the floor to ceiling with icons and statues, likely from other, more active time.
"Thanks for coming, Wes," he said, looking up.
"How are you feeling?" I asked, somewhat stupidly.
"Pretty good, considering everything. See? My legs aren't quite so swollen and my abrasions all have eschars on them," he noted as only a doctor could.
"Is there a plug nearby?" and he proceeded to point me the way so I could plug in the programmer to do my job while he explained the device to his wife. The process was quick and I interrogated his defibrillator, then turned off the tachyarrhythmia detections, therapies and now needless alarms. "There, that didn't take long. All done," I said.
There was a moment of silence as I sat with this man whom I known for so long. Like a wise sage and hospitable host, it was clear he wanted to talk for a bit, so I slowed my exit.
"You know, I've always appreciated your frankness about my condition," he said. "You're a lot like me in many ways, I think. You never overstepped, let me have control, to manage things like I wanted to, and I've always appreciated that," he said.
Embarassed by his frankness, I wondered what to say. At a loss for words, I told him how much I enjoyed meeting his family, wife, daughters, and grand-daughters recently in the hospital. He looked puzzled, forgetting. "You know, that day I brought my daughter in your room with them?" His eyes brightened and his smile widened as he remembered.
"Oh, yes! That was wonderful! How fast times flies, doesn't it?" he said.
"You know, I wrote about that day in my blog," I mentioned, ".. and included some pictures of my daughter from 10 years ago - about what she thought about medicine - can I show you?"
"Of course!"
So I showed him the picture and we shared our thoughts about family. Then, to make reading from my iPhone easier, I read him the post I'd written about that day. We talked about family and what they meant to each of us. And then he shared with me another nugget, that he grew to become a writer, too.
"You know, I spent some time and wrote an autobiography for my kids not too long ago - over a hundred pages - about everything I could remember - from my earliest years as a child, about my immigrant father and American mother. My father made it as a successful lawyer - came over from eastern Europe - I even know the ship - I remember the picture of him standing there with his hat..., and I wrote about my family, influential teachers in grade school, fellow professors, and people that I knew throughout the years - everything. You should do that, too, you know. I'm so glad I did. I gave them to my kids and even made some some extra copies - maybe for the grandkids, in case they want it someday..." He looked away to see his wife leave the room, trying not to be noticed as tears filled her eyes once more. She didn't want to him to see her this way.
He stared down at the floor beneath his swollen feet, then continued.
"You know, it was therapeutic for me to write that autobiography. After all, what we do is terribly isolating for the most part. No one understands that. Like you do your procedural stuff and I do my diagnosing. We do most of it all alone, with no one else there. Just the patient and the doctor. Wonderful, to be sure, but isolating. So many memories. I guess it helped me to put some of those feelings and the thoughts I had about those I loved into words. It's hard to capture it all..."
He looked up from the floor and stared in my eyes. "Thank you," he said extending his hand.
I sat motionless for a bit digesting the gravity of his words, lost in them before I saw his hand. Once I noticed, I lept up to shake it and gave him a long hug to his increasingly skeletal frame. It was a brief moment to share together once more and one I now realized I had done too infrequently with other patients in a similar circumstance. Here he was, an incredible man who'd given so much to his family, fellow colleagues and patients, now teaching me once more so much about life as a doctor, about grace, and about real love. Just the two of us, isolated again, but as friends.
With great reluctance I packed things up and found his wife on my way out. "Thank you," she whispered with swollen eyes, "I just don't want him to be in pain."
"He's going to be fine," I told her, "... perfectly fine, especially now. He's such a wonderful guy." She smiled and opened the door.
As I drove away I realized we probably won't see each other again - his remaining time here will be saved for others now. There were so many thoughts, so much to remember, so much still to learn. Perhaps because I'd been through something like this before I was more prepared - it's never easy - but I still felt okay about it all - not sad - confident that we did the right thing...
... together.
-Wes