Here's a few pages of one I read not too long ago that disclosed some, shall we say, interesting findings and a considerable clinical conundrum.
To orient the reader, when a doctor reads the information collected by the Xio XT patch, he or she first reviews a summary sheet of all the heart rhythm data measured by the device. A clever graphic is supplied that permits rapid overview of the tracing with parallel vertical lines closely arranged next to each other. Each tiny vertical line represents a 20-minute interval of heart rate whose ends represent the minimum and maximum heart rate over those 20 minutes. A dot in the center of the line represents the mean heart rate. Below these closely-arranged parallel lines are other dots that fall on a row representing an arrhythmia or action taken by the patient. Here's what the overview picture of the patient I reviewed looked like (note that only 5 days of heart rhythm data were collected):
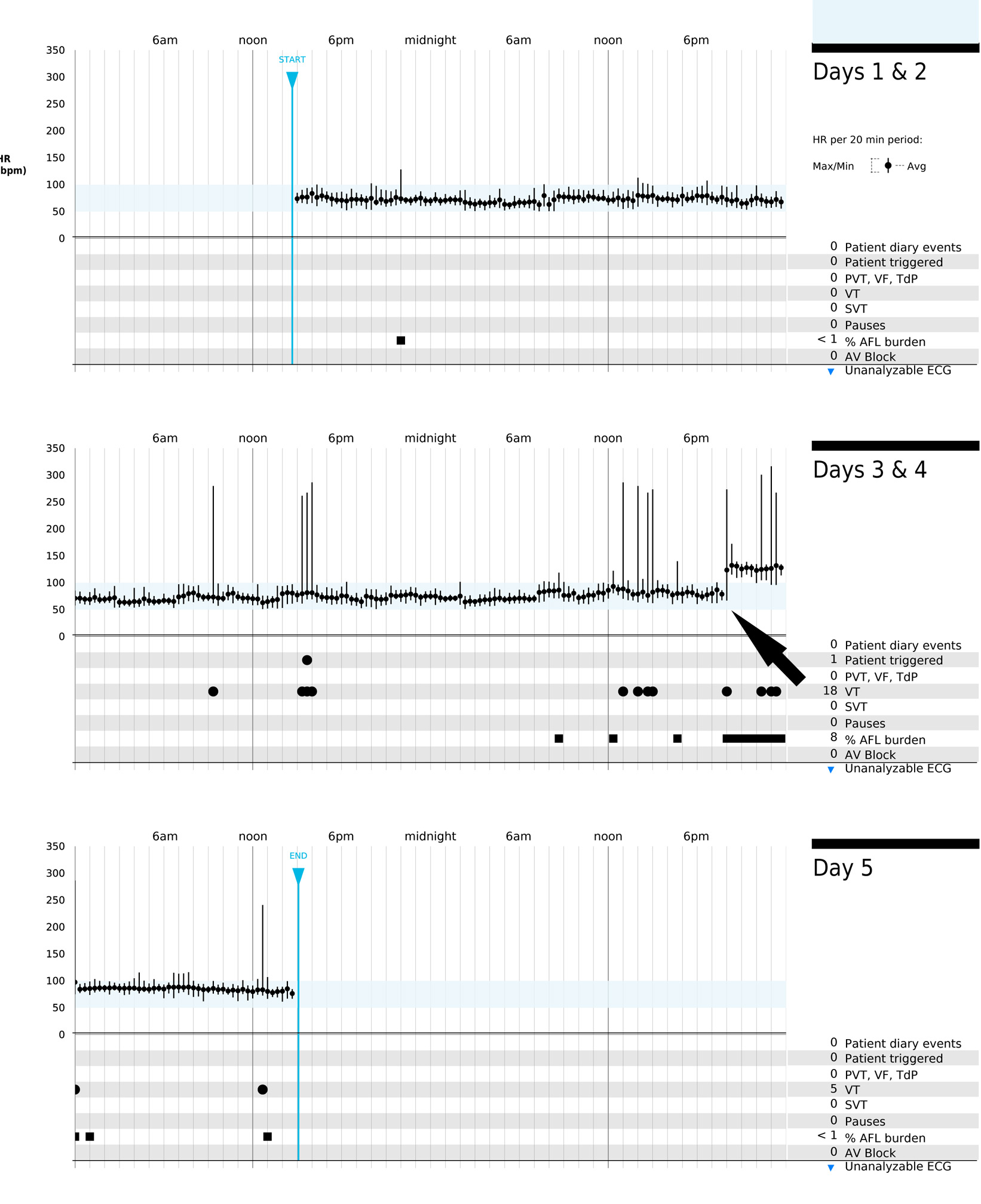 |
| Click to enlarge. Note the increase in average heart rate that occurred at the arrow. |
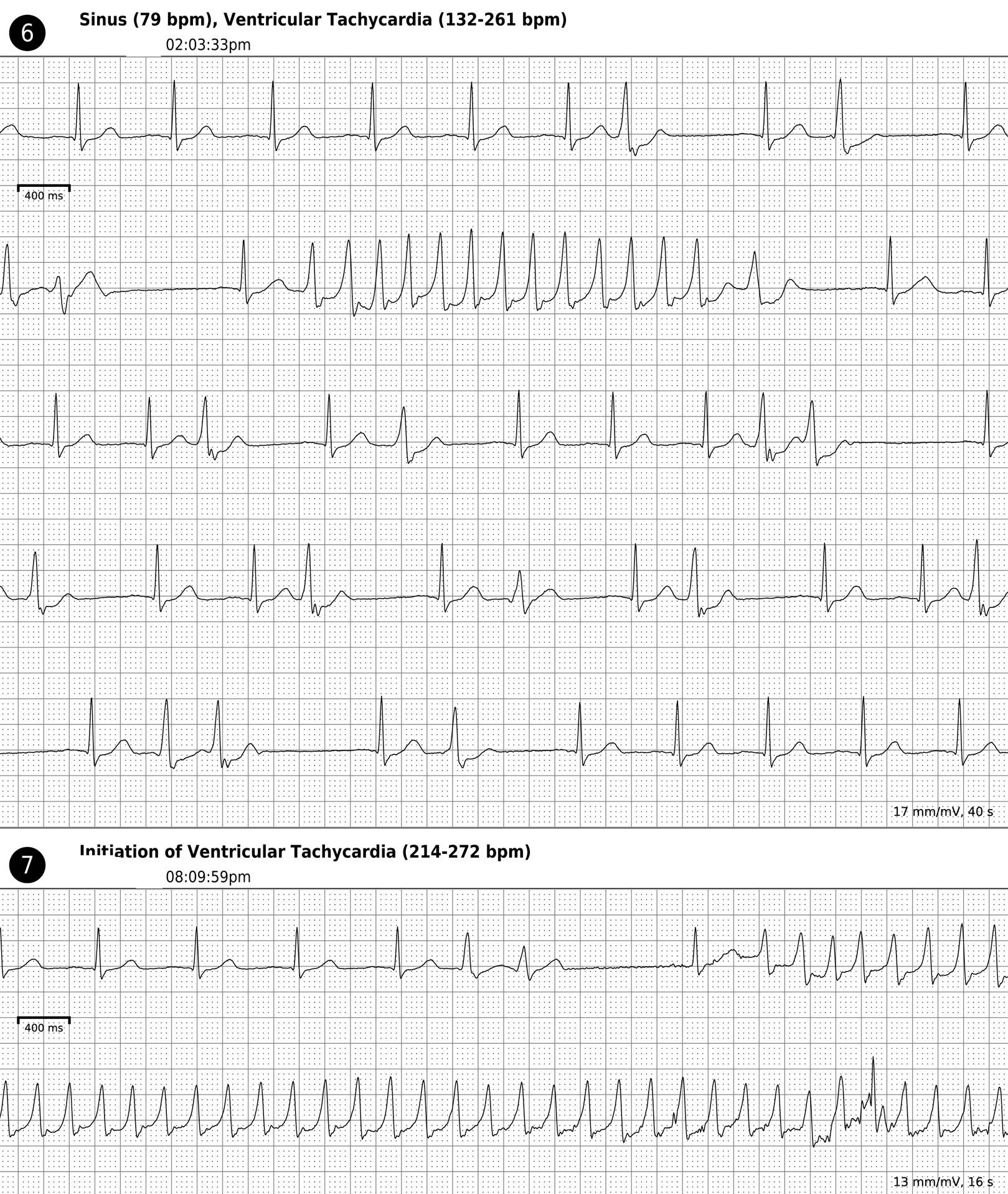 |
| Click to enlarge |
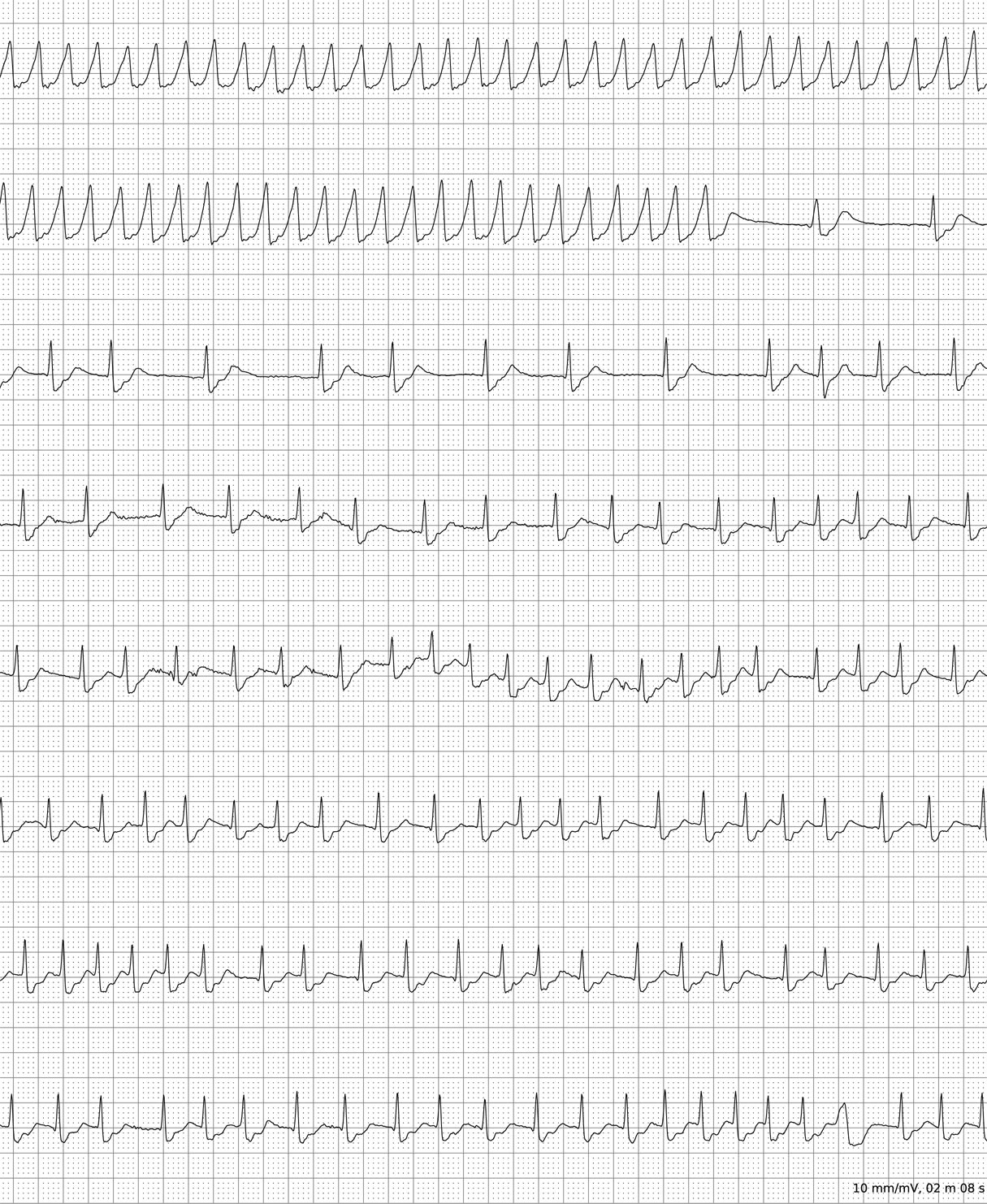
The bottom part of the tracing continues on to the next page:
 |
| Click to enlarge (Note the artifact at the arrow) |
Finally, on the next page, the wide complex rhythm stops, but a more rapid supraventricular rhythm is discovered:
 |
| Click to enlarge |
So now what? Clearly, one of the rhythms appears to be a rapid, potentially life-threatening episode of a wide-complex tachycardia. So I called the doctor who ordered the study, a solo doctor (yes, some still exist) and reach his answering service. I have him paged. There was no answer, so I leave a voicemail message urging a return of my phone call. I then attempt to call the patient. No answer. I call again. No answer to either the doctor or the patient's home/work/cell phone.
Uh oh.
So here's a question: When reading such a study, how much more should the reading doctor be expected to do?
-Wes
I'm surprised to be the first to comment, as I think this is an important consideration to adoption of new remote monitoring technologies in medicine.
ReplyDeleteIf no answer can be obtained at the patient's listed number, the thought has to run through the mind of the interpreting physician that the patient may be face down in a ditch, having succumbed to the arrhythmia.
It might be considered that such remote monitoring devices should have an additional function built in to facilitate two way communication, such that the EP could signal the patient that they need to contact their physicican or seek additional medical care. Something like a blinking red light that could be activated through a cell network. Perhaps more invasive, but also more robust, a GPS locating feature that could be employed in the event of the worst case scenario of a patient being incapacitated by the arrhythmia.
But once you're in the moment with this problem on your hands, you can seek out the patient yourself if you have their address, or call an EMS service and hope they'll help you out. Depending on your where you are, EMS may be more or less helpful.
It reminds me of this post on Skeptical Scalpel about follow up and liability.
http://skepticalscalpel.blogspot.com/2013/07/follow-up-on-whose-fault-is-it-if.html
Anony -
ReplyDeleteThanks for responding. Sorry it's taken so long to respond myself, but I thought I'd leave this case up a bit before describing how this was handled.
First, attempts were made to contact all parties. They were initially unsuccessful. Fortunately sometime later the ordering attending responded and was made aware of the findings.
But we should realize the patch was turned in for analysis. Someone, somewhere knew about the patient. In fact, the device was returned to the company for processing because the patient was admitted to another facility after a single-vehicle accident where the patient lost consciousness.
The arrhythmia that starts on the bottom of the second figure continues onto the third figure above. The artifact denoted by the arrow on the third figure was created by the car's airbag deploying. (Cool, huh? To my knowledge, it is rare to witness such a finding). The patient woke with his car totaled, unaware of how he got into the accident. He, luckily was dazed but otherwise unharmed. His admission to an outside hospital never showed further arrhythmias and his coronary angiogram showed only non-occlusive CAD and normal LV function. However, after these results became available, he received an ICD for secondary prevention of VT. (His afib that occured with the trauma was felt to be an result of the injury and is still being monitored for recurrence by his device.)
Because the patient returned to my clinic as a "new" ICD patient, I learned the full extent of what had happened.