A dual chamber pacemaker was implanted the prior day by a local surgeon in the operating room. The next morning, an EKG is obtained that showed the following:
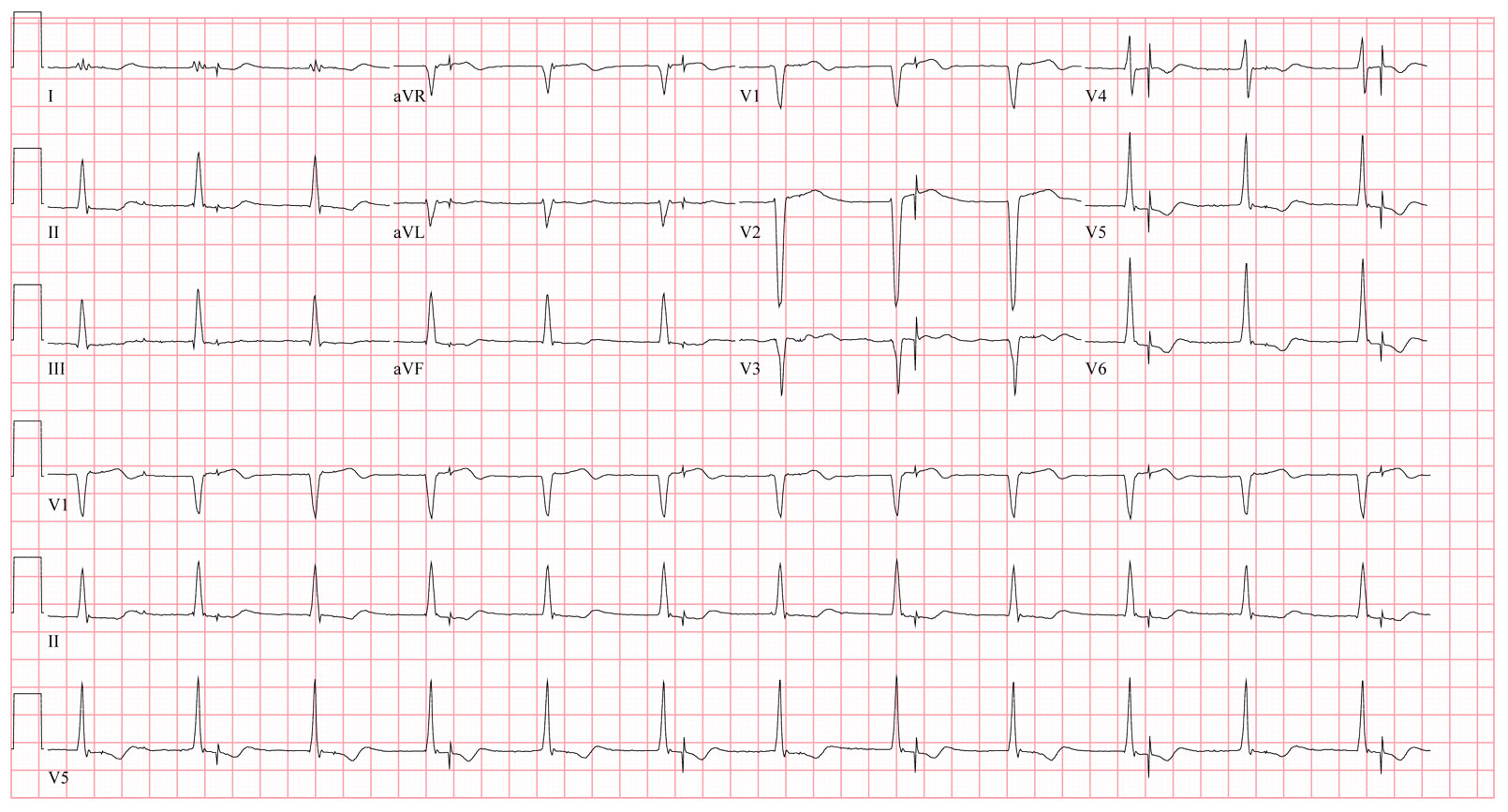 |
| Click to enlarge |
You checked the CXR and all leads appeared to be in the proper location.
Does the patient have to go back to the operating room? Why or why not?
-Wes
Are the leads reversed in the can?
ReplyDeleteIt seems V-events are sensed as A-events causing it to fire at a fixed interval afterwards in the atria.
To be honest I'm not that an expert on pacemaker ECG's.
ReplyDeleteTo me it looks like a junctional rhythm with retrograde depolarization of the atrium, this being misinterpreted by the pacemaker as an intrinsic atrial activity and so the pacemakers tries to depolarize the ventricles after a artificial "PR-Segment". Fortunately not firing in the vulnerable phase of repolarization which could induce VT.
Does that make any sense?
Atrial lead was placed in port for ventricular lead. Ventricular lead was placed in port for atrial lead. This requires operative revision. Years ago, I proposed incorporation of switches to allow non-invasive revision.
ReplyDeleteV under-sensing (v output is is happening at a constant interval after the R wave)
ReplyDeleteThe R R interval is also constant. which leads me to think that there is a functioning and reliable pacemaker of some sort. No discernable p waves. my guess is that atrial lead is what is pacing however ?atrial depolarization is not capured by surface ECG?
Short answer is probably no, does not need to go back to OR. Adjusting v sensing will prove my my hypothesis or rule it out :)
Clue time!
ReplyDeleteThe pacemaker was interrogated and demonstrated the atrial lead paced the atrium and the ventricular lead paced the ventricle. P wave amplitude was 2.8 mV, R wave 11.0 mV, and capture thresholds were normal.
Hmmm.
How do we explain the EKG now?
Wes,
ReplyDeletethis is a Most Vexing Problem.
Hmm.
Jay
@EJSMD
What about if there is some kind of preexcitation or some kind of accessory pathway that makes the atrial lead depolarizing both the atrium and the ventricle. But because the depolarization of the ventricle occurs during the "AV-Interval" of the pacemaker it does not sense it as an ventricular activity and thus firing again after the "AV-Interval" during the repolarization of the ventricle?
ReplyDeleteWe do not know what mode is programmed. I jumped too quickly and now notice atrial pacing occurs as a bigeminal rhythm. The atrial spikes are about 700 mS from the prior T-wave, possibly indicating T-wave oversensing on alternate beats. Atrial spikes linked to v-sensing might suggest a dual chamber mode, DDD, DDI, ...
ReplyDelete2.8 mV is a large P-wave and suspicious if measured by the pacemaker post-implant. The generator seems to sense a T-wave in the ventricular channel, time a V-A delay (rate minus AV interval) and then pace the atrium. The next cardiac cycle, however, the generator does not pace the atrium, possibly because it does not sense the T-wave and inhibits appropriately in A and V.
Is this DDD(R)?
Toby -
ReplyDeleteThe pacemaker was a dual-chamber pacer, programmed DDDR with lower rate 60 b/min, upper rate 130 b/min, paced AV interval 180 msec, and sensed AV interval 150 msec.
OK, let's try another approach. Patient has a junctional rhythm (which always embarasses pacemakers) as there are no obvious P-waves. Starting from the left and looking at the continuous V5, the pacemaker senses a QRS that inhibits and resets the timing. There is a small deflection about 200 ms after the peak of the QRS that is barely visible in V1 but not other lead. there is another small deflection about 250 mS later that is visible in II, V1, II and III. If there is a junctional rhythm, is the first small deflection a retrograde P-wave? If so, what is the next, another P-wave? The second deflection does not repeat in the rest of the strip so let's ignore it.
ReplyDeleteThe next deflection of interest is a QRS followed about 200 ms later with the "bigeminal" deflection. If there were an atrial pace on top of the QRS such that the QRS were hidden in a ventricular blanking period, the "bigeminal" deflection might be ventricular pacing from Ventricular Safety Pacing. The V-A interval of the pacemaker is 820 mS assuming the rate response sensor is sensing the patient at rest.
Moving backward 800 ms from the bigeminal deflection brings us to the small deflection that is about 200 mS after the QRS. However, the small deflection is not consistent within the strip so this explanation does not seem viable.
I'll go (with a lot of doubt) with a junctional rhythm, the timing of which produces atrial pacing every other beat, causing blanking mediated ventricular safety pacing.
If the patient has junctional rhythm, the pacemaker rate can be elevated to restore AV synchrony but this is a temporary solution at best.
Atrial signal is not sensed, perhaps from a PVARP that has been programmed too long. A's are not seen, V is cross sensed first in the atrial lchannel (set too sensitive) before it is sensed in the ventricle. Tracks, 150 ms later the ventricle is paced in the refractory QT interval, setting a new long PVARP. Not sure what is going on the atrium, V3 shows some noise or fib, a possibility is that the atria have too small or no signal, which would in any case lead to same situation described, if atrial channel set sensitively.
ReplyDeleteDoes this person have a previous pacemaker that was not removed? But the leads were reused in the new device? And we are seeing the output from the old device pacing unipolar at 35 bpm (they programmed a low rate trying to keep it out of the way)? Since the old device has no leads attached it cant sense the real rate, and likely the new device isn't sensing the old device's outputs even though they can be seen on a surface signal.
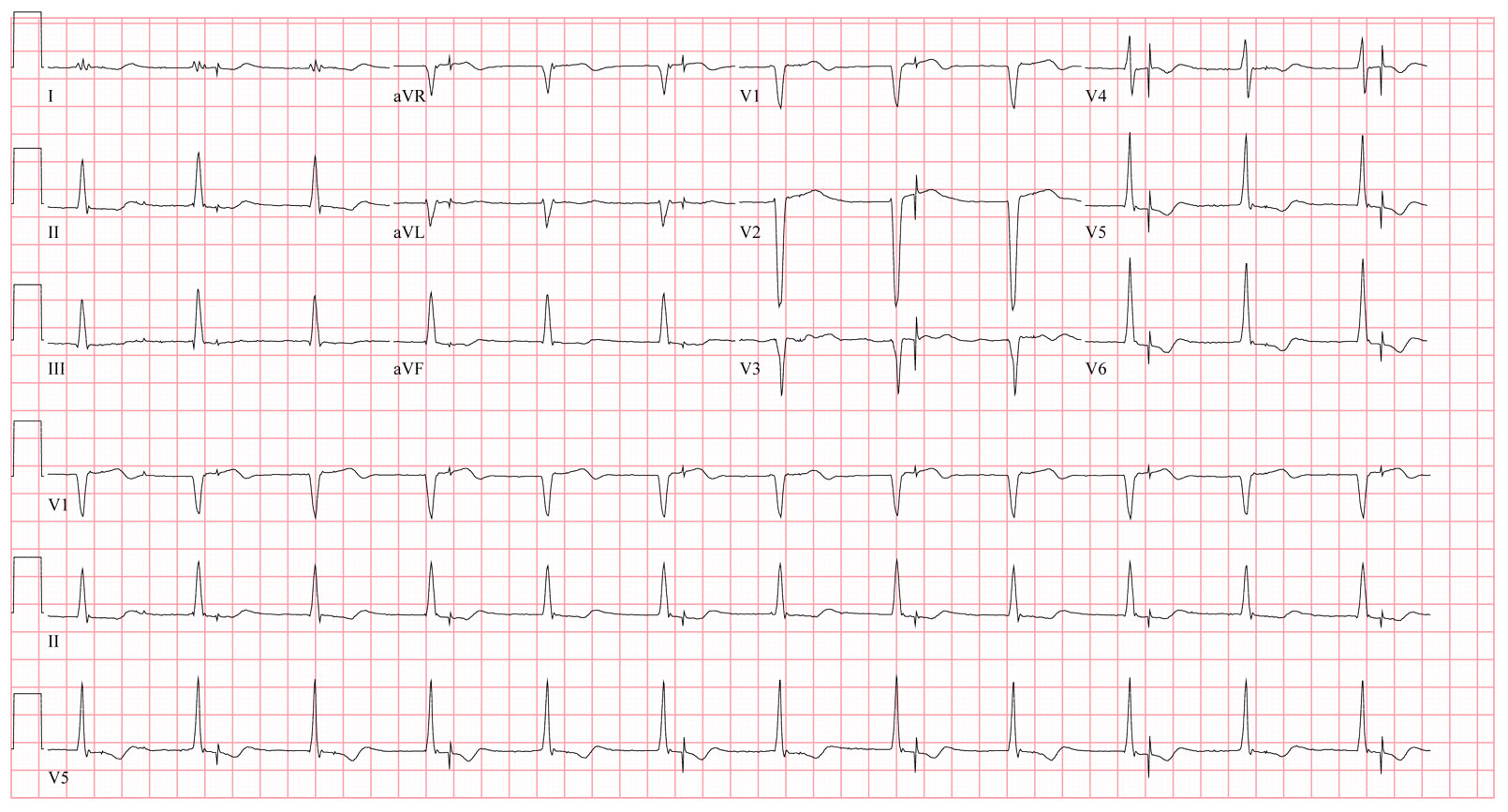
ReplyDeleteFinal "clue" (that contains the answer):
ReplyDeleteHere's a link to an associated tele strip of the same patient's rhythm found on their monitor that helps explain what is seen on the EKG shown.
This is a tough one, but a few folks seem to have the right idea...
We think the A & V leads are switched (in the header?)
ReplyDeleteI think Toby is right about the junctional rhythm causing atrial paces to be scheduled every other beat, coinciding with the QRS. But the interval is too long to be safety pacing which is typically 110 ms. Maybe the R-wave is really narrow tip-ring egm and gets hidden by the cross chamber blanking of 30 ms in the V after an AP. This is rare, but I have seen before.
ReplyDeleteOkay. The strip just made it more complicated!
ReplyDeleteThe A-pace happened (with no capture) then the v sense was "too quick" so device v-paced! Previous beats have a bleb before QRS (?Acessory pathway)
Why did A pace happen??
Maybe we deal with VA crosstalk during junctional rhythm - the A channel is sensing far-field R wave, and this pseudoatrial "event" initiates PAVB (non-sensed QRS on V channel) and SAV (V pace after each QRS, non-capturing due to ventricular refractoriness)
ReplyDeleteIt looks like OOO pacing (the apparent paces on the original strip are spaced too exactly at regular intervals) so I suspect a magnet.
ReplyDeleteWes,
ReplyDeleteEven after hearing all these tech support guys pontificate in another direction, I still think your original strip is just an example of Medtronic's MVP pacing algorithm resulting in an extremely long AV interval after atrial capture. Although it's hard to see pacer spikes after every QRS, I suspect they are just not evident due to the digital signal processing of modern ECG machines. I think this patient has sick sinus and advanced AV nodal conduction disease with pacing mode switched into AAI mode due to the MVP algorithm.
Hence my clue "Most Vexing Problem."
That said, I've having a hard time seeing how your second ECG helps. That one looks like junctional rhythm just at the base rate of the pacer. On occasion the atrium times out and paces just before the native QRS. That results in a safety pace. I think this is consistent with my answer, I'm just not sure how that "contains the answer" as you say.
I'd been sheepishly holding off in the hopes that you'd finally cave and put up the answer, but I couldn't wait.
I'm either very smart or very stupid on this one. PLEASE stop the suspense.
Jay
@EJSMD
I would guess it's V safety pacing. When a pacemaker senses a ventricular signal around the same time there is an atrial signal (like during a junctional rhythm) there is concern that the V signal is just farfield oversensing of an atrial signal. In someone with CHB it would be dangerous if the V lead inhibited pacing based on oversensing, so pacemakers deliver the ventricular pace just to make sure that the patient isn't asystole.
ReplyDeleteThe additional clue strip is 3oAVB with accelerated junctional rhythm....early on you can see the p waves marching through. With that I'm assuming the pt has no retrograde conduction. The original strip was accelerated junctional rhythm with sinus rate equal to the junctional rate. It paces the RV based on which "side" of the junctional R wave the P wave is sensed. If the R wave is sensed first, its considered a PVC. If the native P wave is sensed first it starts the AVI, then the sudden R wave, which is non physiologic, then safety pace.
ReplyDeleteMDT will be the first to tell you MVP is not DDDR
ReplyDeleteYes, I stopped thinking MVP when he said DDD. Anyway the backup VP in MVP is 80ms after the AP. This Paced AV interval looks like the programmed one. And I dont think it is safety pacing either as that AP-VP interval is 110ms at slow rates and 70ms at fast rates.
ReplyDeleteI had a case with a Cardiac Contractility Modulation device from Impulse Dynamics implanted along with an ICD. The ecg looked like this:
ReplyDeletehttps://dl.dropboxusercontent.com/u/32878659/Impulse%20Dynamics.jpg
Isorhythmic AV dissociation is a such a vexing problem. It's most especially vexing when the junctional rate, atrial rate and pacing rate are about the same.
ReplyDeleteAS/VP with VP in the ERP of every other QRS complex?
My question is: was the iso-rhythmic AV dissociation diagnosed as AV block? And therefore, was the pacemaker...never mind with that.
Great case. Look forward to the intracardiacs.
Jay...I thought about atrial capture with long av delay too, but darn it, I can't see atrial capture. And humor me...Could the terminal portion of the QRS's of the complexes without the paced beat look different than the ones with pacer spikes? As in the terminal deflection in AVNRT. And maybe for those few beats there was every other beat wobble.
Look forward to Wes' final post.
I hope this will be a lesson that all av block is av dissociated, but not all av dissociation is av block.
Best guess:
ReplyDeleteIsorhythmic accelerated junctional rhythm in a pt with a DDDR ppm with A-pacing simultaneously at near equally timed rate, causing transient continuous VSP due to timing of junctional rhythm causing V-sensed event after the Post A-blanking period. The VSP in this MDT ppm feature nominally on to prevent cross-talk inhibition, thus this is normal device operation & lead position/function & device does not need revision.
As a pacemaker patient who doesn't understand any of this...I am so glad I am not THIS patient!
ReplyDeleteOkay, I’m sorry I have not divulged the answer sooner, but that darn work stuff just kept getting in the way!
ReplyDeleteFirst of all, this is an EKG of an accelerated junctional rhythm at (according to the EKG) 71 beats per minute. This rate becomes important, since it represents about 845 msec (60,000 milliseconds per minute divided by 71 b/min = about 845 msec).
Recall that the sensed AV interval was 150 msec and the paced AV interval was 180 msec. These days, pacemakers start with atrial-based timing unless a ventricular rhythm is sensed, then both atrial and ventricular timers reset. Therefore, since the lower rate was set to 60 beats per minute (1000 msec), to assure another ventricular beat is occurs at a rate of 60 beats per minute, the atrial channel must activate at least 850 msec after the last sensed ventricular beat (1000 msec minus the sensed AV interval of 150 msec equals 850 msec).
Because the junctional beat rate is so close to this 850 msec interval, the ventricular sensed event occasionally occurs in the atrial-paced blanking period so it is not detected by the device. As such, no ventricular safety pacing occurs. (Recall that ventricular safety pacing occurs when a ventricular-sensed signal is detected in the paced AV interval and occurs 110 milliseconds after the atrial pacing spike). Because the ventricular event was not sensed at the time the atrial pacing occurs, the pacemaker waits the programmed paced AV delay (180 msec) and delivers the pacing spike when the right ventricle is absolutely refractory (hence no pacing spike “capture.) The next junctional beat is then sensed by the RV lead and no pacing output occurs, and the process repeats.
The earlier rhythm strip that I provided as a hint contains proof that the rhythm was junctional (P waves slow and disappear into the junctional rhythm at it accelerates). The rhythm strip later shows occasional ventricular safety pacing and even AV pacing with the expected paced AV interval when the ventricular lead falls into the blanking period – it just so happens that the atrial pacing spike occurs early enough to still be seen. In the original EKG shown, the atrial pacing spikes are barely seen because they are buried in the QRS (with the exception of faint ones seen to the left side of the EKG on careful inspection.)
Sorry this one was so hard, but it shows the value of group thinking and helps reinforce DDDR pacemaker timing sequences. A full diagram of what I just described is shown here for your enjoyment, and believe me, a picture is worth a thousand words.
Great case.
ReplyDeleteJerry from BSX (@w04f40) wins, I lose.
Even when he showed me his correct answer, I didn't believe it because I couldn't see any atrial pacer spikes. In addition, it seemed pretty fortuitous that the patten would be so steady so long. One big coincidence captured on paper to torture us.
Nice job, Wes and Jerry,
Jay
@EJSMD