It is helpful for blog authors to reflect on what readers have found most interesting in 2012 to help sculpt a tone for the upcoming year. While there are a number of ways to "value" a piece of writing (most page views vs. number of comments, for instance) stories that recieve the largest numbers of page views probably reflect the posts of most interest to readers since their content is not only read but shared with others.
Here were my five most-read posts from 2012:
#1: DOJ Hands Heart Rhythm Society and Hospitals Its Decision on Defibrillators
#2: The Growing Culture of Hostile Dependency Toward Caregivers
#3: How A Sudden Cardiac Arrest Survivor Handles the World Cup
#4: The DSM-Tw: Handbook of Twitter Personality Types
#5: EKG Du Jour #29: Tangoing with Two
As you can see, news, fun, and EKGs continue to dominate.
Thanks to all of you who drop by this site. May each of you have a healthy and Happy New Year in 2013!
-Wes
Monday, December 31, 2012
Friday, December 28, 2012
The Punative Evolution of Board Certification
Once upon a time, doctors looked forward to the opportunity to become “board certified” in their specialty of interest in medicine. Time was plentiful. In the lost days of Never-never Land, doctors would leave their office at lunch time while their secretaries manned the phones. Patients still got their appointments while doctors had time to play golf on Wednesdays. It was an idyllic time with plenty of time to read, brush up on the latest innovations in medicine, attend scientific conferences, and still be able to make a living. Board certification was simple: study hard, take a test, and move on. Patient care didn't suffer.
These days, Never-never Land no longer exists. Time is the most valuable commodity for doctors now as they see more patients in less time than ever before. Pushed to perform in an era of exploding health care costs, the days of leisurely lunches, unlimited patient appointments, and easy access to caregivers have given way to a frenetic pace of 7-minute appointments, decreased length of stays, productivity quotas, and cuts in ancillary personnel as costs are shaved. At the same time, regulatory burdens have exploded.
Since 2000 the American Board of Internal Medicine, citing the need to stay abreast of the many innovations in medicine, decided to limit the duration one could remain “board certified” to ten years. That way, the logic was spun, doctors could be brought up to date on the lastest and greatest concepts of their field so they could “maintain” their certification by passing a maintenance of certification (MOC) process. Of course, this “maintenance” never took into consideration the ten additional years of clinical experience, anxiety, legal risk that doctors were exposed to in the meantime. The “maintenance” never took into consideration the ongoing CME requirements doctors are required to maintain for state licensure. And the "maintenance" was ever clinically validated at having an effect on patient care. And the cost varied from doctor to doctor specialty.
And so it has gone: certifying board after certifying board, entering the fray – each with their own self-interest (and financial solvency) in play to assure their particular form of “certification” and doctor education is the best in the eyes of regulators and "stakeholders" (i.e., the people controlling the money). Even an unscrupulous self-proclaimed "reverend-doctor" joined the fray, promising a “board certification” certificate for just $500 by completing a simple questionnaire and mailing it to a post office box - all for far less hassle and time spent away from patients.
This week’s New England Journal of Medicine has an excellent article reviewing the Maintenance of Certification process for “board certification” and reviews both the complexity and regulatory burdens imposed by the new collaboration between the ABIM’s MOC process and the Federation of State Licensure Boards (FSLB’s) maintenance of licensure (MOL) process. Ironically, the article sites an earlier published fictitious vignette from 2010 involving a subspecialist who held time-unlimited ABIM certificates in both internal medicine and endocrinology. In the vignette, the physician wrestled with whether he should enroll in the MOC program of the ABIM voluntarily to become recertified, and readers were invited to vote on the question. Of 2512 votes case, 63% advised the doctor against enrolling in the MOC program.
My bet is the number of doctors who would advise against the process would be far greater now. The process has grown so time-consuming, expensive, and arduous (without any proven clinical benefit) that doctors are feeling the effects on their practices, income, and patient care. Time away from practices has become very expensive for BOTH doctors and their patients. After all, patient appointments, already hard to come by, are necessarily taking a back seat to these board-certification-turned-licensure requirements.
Board certification should return to a personal goal, rather than a regulatory one. More doctors would be likely to participate voluntarily as transparency to credentials increases. As a result, patients would benefit and payers would benefit. Let doctors complete these requirements on recommended schedules, not mandatory ones. Credit for safe, effective care should serve as an even more valid substitute for certification compared to sitting for tests before a computer and performing chart reviews.
Unless regulators comprehend how their evolving punitive, time-consuming, and expensive board and licensure recertification process has become for doctors, they might miss how its increasingly compromizing patient care rather than improving it.
-Wes
Disclosure: I am currently undergoing the MOC process for the third time because I don't live in Never-never Land.
References:
Iglehart JK and Baron RB. Ensuring Physician Competence - Is Maintenance of Certification the Answer? New Engl J Med 2012; 367:2543-2549 December 27, 2012.
American Board of Internal Medicine Maintenance of Certification Program New Engl J Med 2010; 362:948-952.
Monday, December 24, 2012
A Christmas Poem
So comes the clear and cold and weather wintry,
To cast in stark relief the trees against the sky,
Reviving long forgotten lacy beauty,
Submerged before the leaves of Autumn fall to die.
So need we really find it all so odd,
That when some dark and wintry burden comes around,
Some comepensating gracious gift of God,
Some darker beauty, silent joy, strange hope is found.
An ancient instinct knew to call for song,
Amid the chilling deep December cold,
To tell again that in the deepest wrong,
Eternal love still lives as surely as of old.
For ancient Babe came not to candlelight,
Was welcomed not by soft and sentimental glow,
His love he lived into the darkest night,
Held fast against life's eerie ebb and flow.
So seek to make your season what you want,
Pile high the joys and sing the songs you should,
Remember tho', should feast be as you planned
Or not, your God is there and life is ever good.
-- Gilbert W. Bowen, D. Min.
Merry Christmas.
-Wes
Saturday, December 22, 2012
You Are Christmas
To all the caregivers
Who make Christmas happen
Even when their hearts are heavy
Moments of rest too few…
You are Christmas.
To all the suffering
Who rise to the occasion
With a smile or a simple gift
Or permission for others
To celebrate without them…
You are Christmas.
To all the doctors and nurses and hospice workers
Whose own trees go undecorated and gifts go unsent
Because it seems every year
The hospitals are full at holiday time...
You are Christmas.
To all the parents
Who recapture the innocence of the season
For the sake of their children
With a song, a story, a silly ritual…
You are Christmas.
After all, it was never about the strong, the powerful, the rich,
The proud,
It was always about the humble, the faithful, the courageous,
The quiet, hopeful ones.
The scared young family standing in wonder at the manger,
Trusting, holding faith, believing in good,
Believing in love.
From both of us – Merry Christmas,
Di and Wes Fisher
Who make Christmas happen
Even when their hearts are heavy
Moments of rest too few…
You are Christmas.
To all the suffering
Who rise to the occasion
With a smile or a simple gift
Or permission for others
To celebrate without them…
You are Christmas.
To all the doctors and nurses and hospice workers
Whose own trees go undecorated and gifts go unsent
Because it seems every year
The hospitals are full at holiday time...
You are Christmas.
To all the parents
Who recapture the innocence of the season
For the sake of their children
With a song, a story, a silly ritual…
You are Christmas.
After all, it was never about the strong, the powerful, the rich,
The proud,
It was always about the humble, the faithful, the courageous,
The quiet, hopeful ones.
The scared young family standing in wonder at the manger,
Trusting, holding faith, believing in good,
Believing in love.
From both of us – Merry Christmas,
Di and Wes Fisher
Friday, December 21, 2012
Wednesday, December 19, 2012
No Longer Living in Denials
I received this notice, dated 1 March 2012, from our billing department after a denial for reimbursement following a successful right ventricular outflow tract ablation I performed:
We should first ask ourselves if Paul Rossi, DO, whose google search reveals he was an emergency room doctor working in "preventative medicine," should have ability to determine what constitutes standards of care in the field of cardiac electrophysiology when he, himself, is not credentialed in this subspecialty.
But that's not all.
Even Cigna's own recently published "guidelines" for approval state:
Furthermore, those same recommendations detail at least 8 different studies where 3-dimensional mapping was used for VT ablation and include this statement from the Joint Heart Rhythm Society/American College of Cardiology guidelines for ablation (2006):
Welcome to the world of social media, Cigna. I can only hope that every employee out there with an option to choose insurers strongly consider picking another insurance carrier since they will be much better (and more safely) served when they need their ventricular tachycardia successfully ablated. Rest assured, my response to Dr. Rossi's coverage denial decision is forthcoming.
Thanks so much for wasting my time.
-Wes
"Paul Rossi DO, a Cigna Medical Director, reviewed Use of an intracardiac electrophysiological 3-dimensional mapping system in the diagnosis, treatment, or management of ventricular arrhythmias or any other condition because there is insufficient scientific evidence to support use and determined the service(s) is not a covered benefit as indicated below:These denials are part of life for doctors - it's all part of the game. But the era of social media is upon us, and with it, revenge.
Service referenced: Electrophysiological 3-Dimensional Mapping and Catheter, electrophysiology, diagnostic/ablation, 3D or vector mapping
The use of an intracardiac electrophysiological 3- dimensional mapping system is considered medically necessary when used to guide supraventricular arrhthmias. Based upon current available information, coverage cannot be approved to support the use of intracardiac electrophysiological 3-dimensional mapping in the diagnosis, treatment, or management of ventricular arrhythmias or any other condition because there is insufficient evidence to support its use. At the present time, it is considered non-standard testing and falls under the category of experimental/investigational/unproven."
We should first ask ourselves if Paul Rossi, DO, whose google search reveals he was an emergency room doctor working in "preventative medicine," should have ability to determine what constitutes standards of care in the field of cardiac electrophysiology when he, himself, is not credentialed in this subspecialty.
But that's not all.
Even Cigna's own recently published "guidelines" for approval state:
The CARTO® EP Navigation System (Biosense Webster, Inc., Diamond Bar, CA) received 510(k) premarket approval in December 1999 by the U.S. Food and Drug Administration (FDA) as a Class II device for catheter-based cardiac mapping (FDA, 1999). The FDA indications for use state the intended use of the CARTO EP Navigation System is catheter-based cardiac mapping. The CARTO EP Navigation System and accessories have had numerous enhancements with the latest device, the CARTO 3 Version 1.05 EP Navigation System and accessories, receiving 510(k) premarket approval in 2009 (FDA, 2009; FDA, 2006; FDA, 2000).Hardly experimental.
Furthermore, those same recommendations detail at least 8 different studies where 3-dimensional mapping was used for VT ablation and include this statement from the Joint Heart Rhythm Society/American College of Cardiology guidelines for ablation (2006):
"Electroanatomic magnetic mapping capabilities are being applied to aid in the diagnosis and nonpharmacological treatment of arrhythmias. The authors state, 'although not yet established as requisite or "core" equipment for the EP laboratory, these and other emerging technologies have had, and will continue to have, a major impact on the practice of cardiac arrhythmia management.'"I'm sorry, but I do not see the words "experimental" in Cigna's own documentation nor does their document suggest that appropriate standard of care for 3D mapping be reserved exclusively for "supraventricular" arrhythmias.
Welcome to the world of social media, Cigna. I can only hope that every employee out there with an option to choose insurers strongly consider picking another insurance carrier since they will be much better (and more safely) served when they need their ventricular tachycardia successfully ablated. Rest assured, my response to Dr. Rossi's coverage denial decision is forthcoming.
Thanks so much for wasting my time.
-Wes
Sunday, December 16, 2012
Trying to Make Sense of the Senseless
I believe that every human soul is teaching something to someone nearly every minute here in mortality.
- M. Russell Ballard
Aside from being a bit warmer than usual, it was a typical Friday afternoon. A patient with syncope, a paucity of heart beats, the need for pacemaker. The lab techs rolled their eyes as the room was prepped. An early as exit was not going to happen after all.But the later hour promised efficiency for the only way out was through. We each did our thing and like so many times before, sighed in relief that things went smoothly. Home at a reasonable hour was to happen after all.
Until the ER called while I was closing.
"Another patient, 97, heart rate 21, needs a pacer, too," they said.
“What does the family want? He is 97 after all…” I asked as I placed the final layer of sutures.
“The patient wants it. Takes care of his wife…,” they said.
“I’ll finish here and you guys get the room ready. I’ll see the ER patient. Has the family of this patient been called?”
Once again, the staff excelled. Patient transported from the table, family contacted, then the room cleaned and readied for the next potential patient.. For me, the note would wait. A brief discussion, orders entered, then ER visit, wondering all the while if the next pacemaker needed to be done.
It was easy to find the ER bay as every nurse and technician pointed the way to a small-framed man who was alert and conversant, but clearly not feeling himself. His symptoms started earlier in the morning and just didn’t get better- his medications hadn't changed.
“Do we have a potassium?” I asked.
“’lytes are fine,” someone said, “K’s 4.5.”
History, physical, review of the data – all pointed to one thing: a pacemaker. We talked risks, alternatives, pros and cons. He looked at his wife, quietly seated in the corner. “Of course you need it!” she bellowed.
And that was that.
And so it was. A temp wire, then permanent pacer with tripling of his heart rate. He became more talkative, his blood pressure easier to obtain.
But as the tension lifted, the chatter grew.
“Did you hear?”
“Hear what?”
“About the kids…”
Detail after horrible detail came to those of us shielded from the day’s events. The shock. The evil. The senselessness of it all.
I looked down at the tissue beneath my hands: thinned, frail, bleeding still as the closure was being completed. As time passed, the lab grew strangely silent, the irony clearly palpable...
... one old heart mended, while the others...
God, there are no words...
God bless them. God bless their families.
God bless us all.
-Wes
Wednesday, December 12, 2012
Medical History Revisited: What Is This?
My Grand, Sweeping Cardiovascular Predictions for 2013
Cardiovascular predictions for next year are always fun to contemplate this time of year. So much is happening to the practice of medicine as we've known it that it can be helpful to highlight some of those changes, both good and bad, as our medical world continues to evolve. While these predictions contain pure guesses, they also contain one doctor's observations of our new evolving medical world. Many of these changes will profoundly shape how doctors interact with their patients.
So grab some coffee and strap in. Here are my 2013 predictions of life as a cardiologist in 2013. (Please feel free to add your own predictions in the comments section.)
Valvular Heart Disease
Ischemic Heart Disease
Electrophysiology
Heart Failure
Patient Care
Administration
Health Care Terrain
Education / Research
Summary for 2013
-Wes
So grab some coffee and strap in. Here are my 2013 predictions of life as a cardiologist in 2013. (Please feel free to add your own predictions in the comments section.)
Valvular Heart Disease
- TAVR for critical aortic stenosis will be applied to progressively younger and healthier patients.
- As smaller delivery systems for percutaneous heart valves gain widespread acceptance, government payers will look for new and inventive techniques to restrict patient access to these devices. No heart valve will remain untouched as creative uses of the approved devices are attempted in non-surgical patients.
- Innovations valve design will improve the safety and effectiveness of this therapy.
Ischemic Heart Disease
- The push for more drugs and less stenting will continue in stable ischemic coronary disease.
- Acceptable (payable) door-to-balloon times will shrink from 90 to 60 minutes as payers give the most reimbursement for centers with the faster times.
- Radial artery catheterization and interventions will grow in acceptance and CABG will continue to have a more prominent roll for severe 3v disease (continuing the "reduced stenting" theme) compared to multi-vessel stenting.
- Lipid therapy recommendations will remain unchanged.
Electrophysiology
- Pressure on AF ablation to prove its superiority over medical therapy will continue, especially given ablations re-do requirements, up-front cost of therapy and uncertain utility compared to medical therapy. Still, until enrollment of the multi-center NIH-sponsored CABANA trial completes, catheter ablation of atrial fibrillation will remain a mainstay of therapy for symptomatic patients with paroxysmal atrial fibrillation.
- Novel oral anticoagulants (NOA) will see an expanding role the management of AF patients over aspirin and warfarin. Apixaban will be FDA approved and quickly command the largest market share of the available agents based on clinical data. Antidotes for reversing these agents will continue development and once developed and proven effective, NOAs will completely change the standard of care for management of stroke-prevention in non-valvular atrial fibrillation.
- Subcutaneous ICDs will show a slow growth in acceptance as doctors insist on a smaller device with fewer early battery depletions before adopting the first-generation devices more widely. Also, look for other companies to enter the subcutaneous ICD market with devices of their own.
- Standard pacemaker and ICD implant rates will remain flat.
Heart Failure
- Readmission rates will be reduced by increasing admission rates to extended-care facilities when heart failure relapses (at least it's not a hospital!)
- LVADs will see a slow increase in utilization, but expenses will limit wide-spread adoption at lower-volume centers.
- Ultrafiltration will die its slow, inevitable technological death.
- Biventricular pacing might see a slight uptick as hospitals seek every possible opportunity to prevent readmissions while maximizing revenues with the first heart failure admission.
Patient Care
- In 2013, physician computer screen time will officially far exceed all direct patient care time.
- The Electronic Medical Record will look more like Microsoft Office as basic features of letter writing, e-mailing, scheduling assume higher priorities for communication and coordination in patient care.
- Reliance on Big Data to shape proper medical care will consistently be shown to be a poor surrogate for carefully constructed prospective randomized trial due to the inability to code physician logic from progress notes. Furthermore, associated widespread diagnosis and procedural coding flaws will continue to plague the field. The implementation of ICD-10 will only make this problem worse. More data does not mean better data. Despite these facts, the heavy marketing of Big Data to doctors and hospital administrators will continue.
- Speaking of guidelines: New guidelines recommending the appropriate guidelines to use will emerge (Should a doctor use guidelines from the AMA, American Heart Association, European Society of Cardiology, American College of Cardiology, American College of Chest Physicians or the Society for Cardiovascular Angiography and Intervention? Oh, and which year?)
- Physicians will tire of completing data entry field for such random and byzantine criteria like appropriateness criteria, safety checkboxes, and quality measures. But because these criterias' completion will be increasingly insisted upon by Central Planners, administrative employees in medicine will continue their brisk hire rates in 2013. Doctors will then be forced to complete these fields at home.
- The smart phone (and its apps) will officially supersede the stethoscope in importance to practicing doctors of all types (even cardiologists). Guidelines for appropriate app use will be developed. The FDA will require their tentacles to extend to this space and stifle innovation here.
- Patients will be responsible for a higher and higher portion of their health care costs which will lead to a rising voice for price transparency. This push will be in direct opposition to large medical center/insurance industry efforts to shield their privately-negotiated pricing arrangements.
- Look for online health care pricing to grow in popularity.
- Appointment availability will dwindle as more patients enter the system.
- Patient expectations for continued relatively immediate, exceptional care will persist despite the reality of more bureaucratic requirement for physicians. This will continue to grow the sense of hostile dependency toward physicians and their staff.
- Finally, the push to pay only for outcome-based care will create incentives for facilities to tacitly triage the sickest patients away from some hospitals to their competitors.
Administration
- Doctors will get increasingly tired of attending administrative meetings - especially those that generate more meetings.
- Doctors will assume more administrative responsibilities as business policy foot soldiers as they join forces with hospital systems.
- The tendency for administratively-minded doctors to clash with clinically-minded doctors will be an inevitable consequence of this new administrating physician prototype.
- Despite the outward appearance of more involvement with decisions, administrative physician decision-making autonomy will dwindle as payers exercise their growing sway over drug and device choices and pay only based on clinical outcomes.
Health Care Terrain
- Rich hospitals will get richer as poor hospitals get poorer.
- Indigent patients who will soon qualify for care will have to travel further for that care.
- Emergency rooms will continue to experience larger volumes of patients as the full effects of health care reform have yet to be implemented.
- The building spree that has consumed many of the larger health care facilities will taper as financial pressures mount.
- Employers will seek ways to cut health care costs by negotiating their own prices directly with hospital systems without insurance company intermediaries.
Education / Research
- Clinical cardiologists (who are increasingly employed) will find less time and money for educational pursuits compared to the time and money required for licensure requirements. Since most employed cardiologists will have expense allotments that cover both endeavors, higher licensure and credentialing fees will limit professional meetings doctors can attend. The long-term effects of this reduction of continuing education as it pertains to patient care is uncertain. Doctors are likely to turn to online courses rather than meeting attendance to fulfill CME education requirements. As such, abstract submissions to meetings is likely to fall.
- Clinical research opportunities will continue to concentrate at the largest centers with the largest clinical volumes.
- Academic cardiologists will have growing pressures to become more clinical as the prospect of expanding patient access looms in 2014.
- Academic cardiologists will also find research funds in shorter supply as medical device companies and pharmaceutical companies wean expense items like research protocols. Government grants, too, will be more competetive than ever.
Summary for 2013
- Patients will continue to get sick.
- Patients will continue to die.
- Each of the above will continue to occur despite millions of dollars spent on prevention initiatives and early-detection programs.
- Despite all of the changes, the hassles, and the headaches coming next year, doctors will continue to care for their patients.
- Doctors will continue to have sleepless nights worrying about their patients.
- Doctors will still enjoy the reward of seeing their patients improve.
- And when the dust settles in the years ahead, doctors will remain the only ones ultimately (and yes, still legally) responsible for their patients' health and well-being.
- Some things, you see, never change.
-Wes
Sunday, December 09, 2012
The End of Our Health Care Happy Meal
With the publication in the New York Times of how taxes would be affected because of the Affordable Care Act, our health care Happy Meal was officially pulled from the menu.
Suddenly, the colorful trinkets and tchotchkes that were the first items pulled from the health care law's brightly colored bag are now being followed by a hefty bill that most people aren't too happy with paying: their personal tax bill.
The political backlash was so swift, so sure, that even the White House noticed.
So how did the White House respond?
Look where this approach has gotten physicians: each year, since 1997, CMS threatens to cut Medicare payments to physicians some 2.5%. Instead of making the cuts each year as directed by law, Congress caved to political pressure and has delayed the cuts year after year. But the cuts don't go away: they're just added the the following year's paycut amount. Now the amount has grown to nearly 30% or so with no easy solution in sight.
Imagine what could happen to America's patients if the same approach delay tactic for collecting taxes to pay for our new health care entitlement law is taken. Can America's health care cost crisis really afford this political approach that ignores reality?
I'm just a doctor, but methinks this idea of leaving withholdings from people's paychecks unchanged is not a good idea just so the White House can dodge a political bullet.
Since the White House and democratically-controlled Congress helped push our new law through, they should deal with its ramifications responsibly. To do otherwise is fiscally irresponsible and risks making our horrible health care cost crisis even larger.
-Wes
Suddenly, the colorful trinkets and tchotchkes that were the first items pulled from the health care law's brightly colored bag are now being followed by a hefty bill that most people aren't too happy with paying: their personal tax bill.
The political backlash was so swift, so sure, that even the White House noticed.
So how did the White House respond?
... Treasury Secretary Timothy Geithner has the power to adjust how much is withheld from paychecks for tax purposes — for all taxpayers or just for some. By doing so, Geithner could ensure paychecks reflect the White House position that wealthier taxpayers with annual income higher than $250,000 see their taxes rise. Geithner at the same time could leave withholding tables where they are for the middle class, ensuring those workers don’t see a higher cut from their paychecks.But America's doctors should remind the White House why this is not a good idea. After all, Congress uses this kick-the-can-down-the-road approach with us each time they grant a reprieve to the scheduled physician pay cuts mandated by law as part of the Medicare sustainable growth rate adjustments contained within the Balanced Budget Act of 1997.
Look where this approach has gotten physicians: each year, since 1997, CMS threatens to cut Medicare payments to physicians some 2.5%. Instead of making the cuts each year as directed by law, Congress caved to political pressure and has delayed the cuts year after year. But the cuts don't go away: they're just added the the following year's paycut amount. Now the amount has grown to nearly 30% or so with no easy solution in sight.
Imagine what could happen to America's patients if the same approach delay tactic for collecting taxes to pay for our new health care entitlement law is taken. Can America's health care cost crisis really afford this political approach that ignores reality?
I'm just a doctor, but methinks this idea of leaving withholdings from people's paychecks unchanged is not a good idea just so the White House can dodge a political bullet.
Since the White House and democratically-controlled Congress helped push our new law through, they should deal with its ramifications responsibly. To do otherwise is fiscally irresponsible and risks making our horrible health care cost crisis even larger.
-Wes
Friday, December 07, 2012
Guest Post: Physicians Beware on the Twittersphere
Thank you for hosting my response to a recent blog post by Carolyn Thomas at www.myheartsisters.org. Ms. Thomas is a well respected medical blogger with an emphasis on cardiac care and women’s cardiac issues in particular. She has certainly helped many patients and been a great advocate for women’s cardiac issues. We recently had a 3-Tweet interaction that lead to her writing a blog about me. Though Ms. Thomas made excellent points about patient privacy issues and the use of Twitter in general, I feel that her words justify a clarifying response.The following is a guest post by William Dillon, MD, a relatively new cardiologist to Twitter. He describes his experience with a recent patient-doctor interaction on Twitter that sounds an important message. -Wes
Let me introduce myself. I am an interventional cardiologist and new to using Twitter. Two areas of focus for me in the last 18 months have been radial artery catheterization and heart attack care. Social media was recommended as a vehicle to get the word out on heart attack care. My state, Kentucky, ranks a dismal 49th out of 50 states for MI mortality. I aim to improve this.
The problem started after a particularly challenging and successful radial artery catheterization procedure. I tweeted that “Radial cath is like playing golf. You must do it often to be good. Some will never be good at it no matter how hard they try.”
Without going into the nuanced details of radial vs. femoral artery catheterization (already a controversial topic for interventionalists), Ms. Thomas responded with a thoughtful question of her own: “But how do heart patients being practiced on know if their interventionalist falls into the 'never will be good' category?”
This was one of the first times anyone had ever interacted with me on Twitter, so I tried to help. I am used to helping total strangers; that’s what we do everyday in treating acute heart attack patients.
But in retrospect, maybe I should have remembered mom’s advice: “Don’t talk to strangers!” Ms. Thomas wanted to know how patients know if their physician falls into the “never-will-be-good” category. Because I did not know Ms. Thomas, nor that she had had prior personal experience with a radial artery catheterization, I was left at a conversational disadvantage because of the loss of context that is inherent to 140-character interactions on Twitter. Unfortunately, the answer to Ms. Thomas’ question leads to a thorny area—the truth. As Gloria Steinem famously said "the truth will set you free but first it will piss you off."
The truth here is simple: it’s not easy to know if your physician is good. This is a complex issue, and surely not suitable for Twitter. Engaging on this medium on this topic was a mistake. I learned from it. But let’s be honest about a few things: most honest proceduralists would agree that a cath lab nurse or tech has valuable inside knowledge. These folks have first hand experience and interact with a variety of physicians on a daily basis. They know. The problem of course is that the general public does not have access to the inside scene. However, it surprises me that most patients research toaster ovens more than they do which physician to see.
But even if they did research their doctors it would be hard to sort out the best. Here’s why: Though all physicians complete certain minimum standards and maintain competency through continued medical education, that’s a low threshold. The credentialing process at hospitals weed out incompetent docs, but it is far from perfect or nuanced. It's like grading tests on a pass-fail scale.
Outcomes measures—if they existed—would also be flawed. If our procedure outcomes were scrutinized, you could be sure that high-risk patients would not have many willing doctors.
All cath labs have a Director that should be reviewing complications. Peer review also has merits, but that's tough to accomplish in the real world as well.
Back to the tweets.
Ms. Thomas said: “It never occurred to me in ER in mid-MI to ask, by the way is this guy any good?” I continued to try to explain. Again a mistake on Twitter. I recommended asking EMS to take you to the best center during an MI. This is actually a crucial comment and a vital step to surviving a heart attack. Call EMS! The best treatment is a percutaneous coronary intervention (PCI) done at the nearest center with around-the-clock coverage. EMS providers know which hospitals perform PCI for AMI and will direct patients to those centers.
After this last tweet I got uncomfortable with her line of questioning and elected to stop responding. Unfortunately, the damage was done.
What have I learned from this? I realize that one needs to be careful with comments placed on social media. While Ms. Thomas has likely helped many patients through her blog, my comments were greatly misconstrued. It was certainly not my intention to cause such a furor. I am stunned how a 3-tweet interaction can lead to such a defaming and inflammatory blog response from someone I have never met with, spoken to or interacted with beyond a total of 400 characters. A reputation is a lifelong and daily building process. To have it torn apart in a very public way is extremely damaging and upsetting.
I hope that something positive could come of this. Already I have learned and am sorry for any controversy I have caused. But I would like to sound a warning to patient advocates and physicians alike. If what we all want in healthcare is more truth and transparency, tearing down those who dare to speak, to join the conversation, surely will not help.
William Dillon, MD
@Wmdillon
Wednesday, December 05, 2012
An Inside Look at AliveCor's iPhone ECG Case
 |
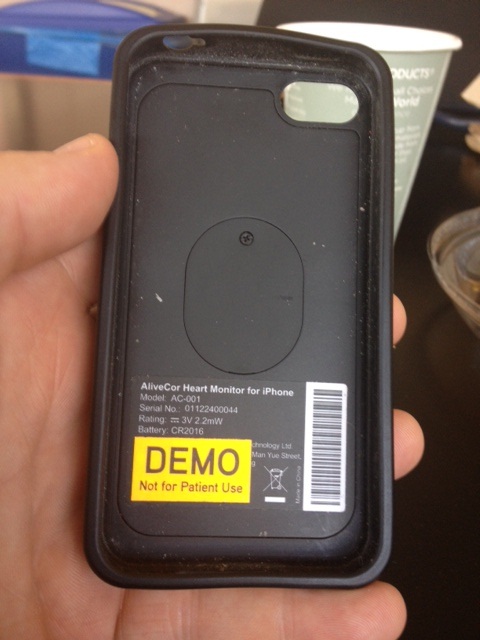
| The back of my demo AliveCor ECG iPhone 4s Case |
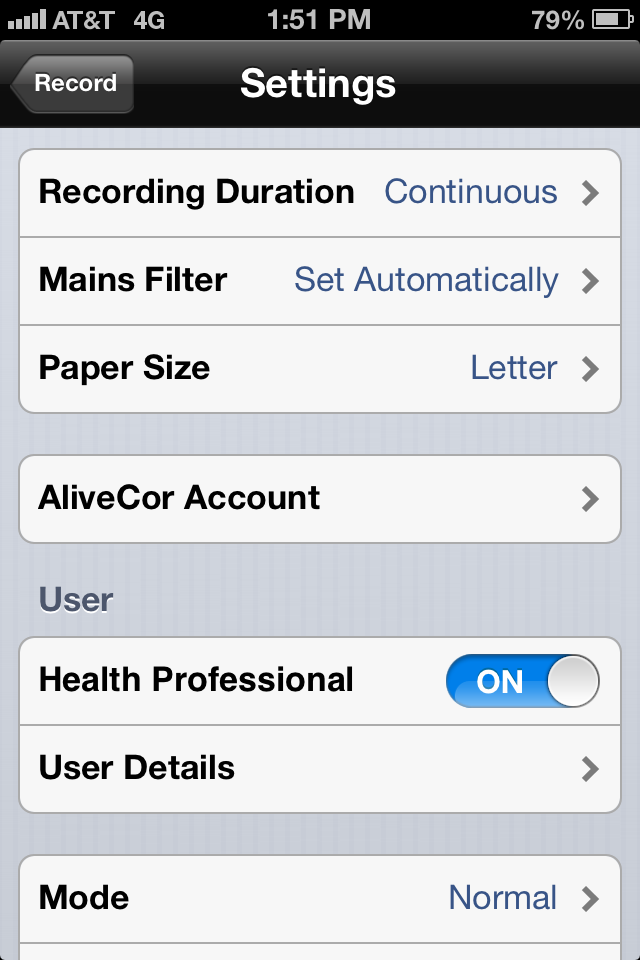 |
| AliveCor ECG Setup Screen (beta) |
 |
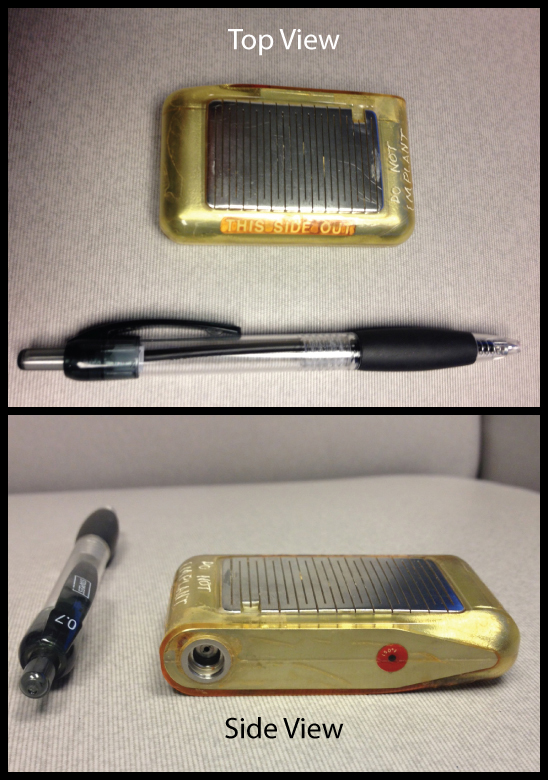
| Inside of My Demo AliveCor iPhone Case Note: no wires. |
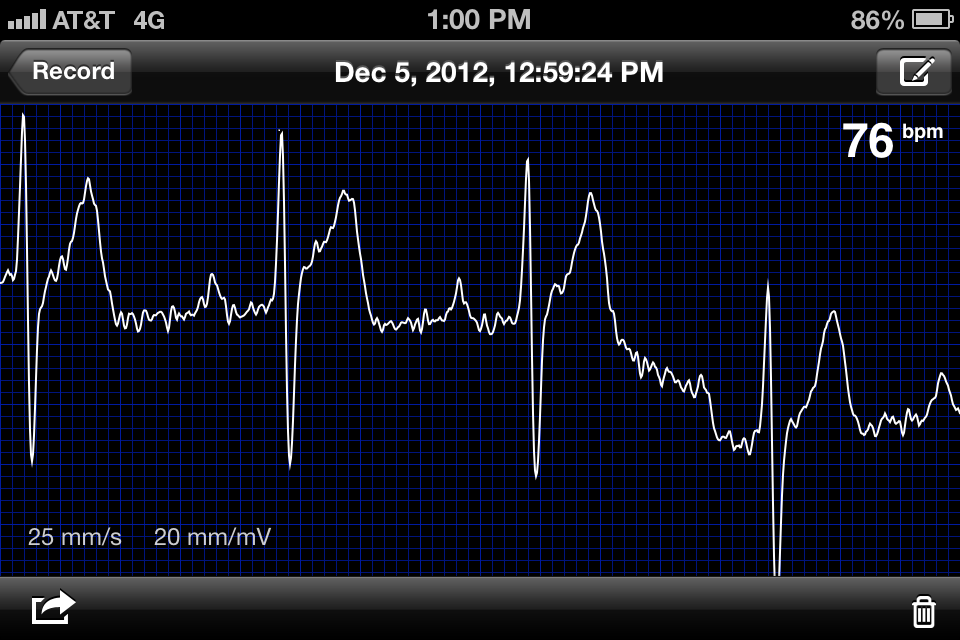 |
| My unretouched ECG recorded with my hands today (yep 1st degree AV block!) |
Lead I of the standard EKG was recorded with the left and right hand holding the device with the left and right hand fingertips touching the electrodes on the back of the case. It was important to hold the device with the iPhone's round button to the right to assure the device did not record an inverted lead I.
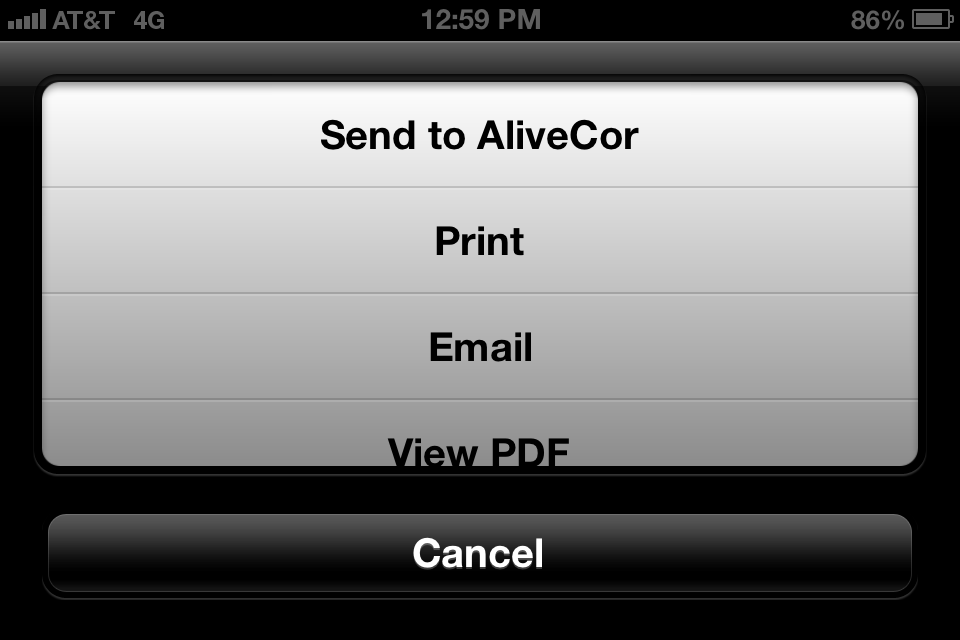 |
| Options for sending tracings (beta) |
Physician Reactions
Without exception, every physician I showed this device recognized this device as a compliment to the doctor's stethoscope. It was a uniform hit as they gazed in amazement at the device's ability to record their real-time ECG. I found this device was capable of instantly differentiating the irregular rhythm of atrial fibrillation from the irregular rhythm caused by premature atrial or premature ventricular beats or even atrial flutter with variable AV conduction. Some care was required to get noise-free tracings or to obtain the appropriate EKG vector on the chest with which to identify lower-amplitude atrial arrhythmias. But most limb leads can be replicated by the device (hold the R electrode with the hand and apply the left electrode to the knee to see lead II, for instance), or angle the leads in different directions on the patient's chest to obtain a new QRS vector. (Obviously, the angle the electrodes were placed on the chest to acquire a particular limb lead requires some rudimentary knowledge of ECG basics.)
Patient Reactions
Perhaps the most interesting aspect of this device is what happened when it is placed in the hands of patients and friends unfamiliar with ECG tracings. Their first reaction as they sit transfixed at their own ECG tracing dancing across the screen is "Cool! .... But what does it MEAN?" Then comes "Am I okay?" And then of course when tracings are compared between friends: "Why is my heart rate so much faster/slower than his/hers?" Or you might hear: "Man, I'm out of shape!" And if the device occasionally had difficulty calculating the heart rate from a noisy tracing, three little dashes would appear instead, leading the person to ask, "Does this mean I'm dead?" Any one of these reactions could came from generally healthy people who have never had a major medical problem.
What was more interesting to me was the nuanced reaction I noticed from patients who had had a complex medical history before but were seeing this device outside a medical facility for the first time. When they encountered this device in a social setting, it was common that these patients refused to have their tracing performed "for fun" for fear they might be sent packing to the nearest medical establishment. IT became immediately clear that discretion should be exercised if the device is to be passed about at cocktail parties. (Yes, doctor, not everyone wants to see your cool gizmo.) Hence, it appears that deploying this device on the general public has some challenges ahead, but I suspect it will come: gradually at first, then more generally. It is clear that this really does take an understanding of ECGs to use effectively, so doctors (or techs) familiar with ECGs will have to be involved. Liability and responsibility for reading remains a thorny issue one the device is released to the public. I suspect these are relatively easy issues to resolve for AliveCor going forward.
Still, for doctors and medically-savvy patients, this device is a game-changer. The number of ECG tracings obtained in clinics will probably diminish one day as this device enjoys a wider distribution amongst physicians since it doesn't require a special technician or equipment to obtain much of the information doctors need to manage their arrhythmia patients. But caution with this single lead ECG device should be maintained, too. Because multiple ECG leads are not collected simultaneously, the device could miss the subtle findings of a heart attack in locations remote from the there the single tracing is collected by the device. Still, for routine rhythm analysis, this device has huge potential for time-savings, practical rhythm interpretation, and maybe even the potential to provide for considerable technical health care cost savings.
-Wes
PS: I have no commercial interest in AliveCor (darn it).
The AliveCor iPhone ECG Case website
What Every Doctor Needs For Christmas
... it brings RFID tags to a whole new level (via Bluetooth) and guarantees you will always be able to locate your keys, pager, stethoscope, ... whatever... each morning: SticknFind.
(Santa, are you listening?)
-Wes
(Santa, are you listening?)
-Wes
Doctors' 2012 33% Tax Hidden Tax Hike
Physicians were the subject of a 33% tax hike that most of them weren't even aware they received this year.
That's right. Thirty-three percent.
Couched as "only five additional dollars each month" by the government, it passed because doctors don't make the Federal Register part of their weekly reading list and because our professional lobbying organizations were either asleep at the wheel or distracted by the whole health care reform mess.
You see if you want to get more money for government programs, you should tax the "rich" doctors - the very same doctors that are enjoying (and have experienced the delays in payment caused by) the joys of the annual congressional cat-and-mouse game of a threatened 30% pay cut wrapped up in the fiscal cliff negotiations. (Don't worry docs, *wink wink* it really won't happen).
The "tax" I'm speaking of? Why it's the new $731 DEA registration fee.
Until 2011, the three-year fee was $551. Now it's $731.
You do the math.
And why were the fees against doctors increased?
Because the DEA needed more money. According to the FDA Law blog, the DEA cited a number of factors justifying the fee increase including:
Brilliant.
And people wonder why doctors are burnt out and fed up.
-Wes
PS: For moreexcuses captivated reading, visit http://www.deadiversion.usdoj.gov/
That's right. Thirty-three percent.
Couched as "only five additional dollars each month" by the government, it passed because doctors don't make the Federal Register part of their weekly reading list and because our professional lobbying organizations were either asleep at the wheel or distracted by the whole health care reform mess.
You see if you want to get more money for government programs, you should tax the "rich" doctors - the very same doctors that are enjoying (and have experienced the delays in payment caused by) the joys of the annual congressional cat-and-mouse game of a threatened 30% pay cut wrapped up in the fiscal cliff negotiations. (Don't worry docs, *wink wink* it really won't happen).
The "tax" I'm speaking of? Why it's the new $731 DEA registration fee.
Until 2011, the three-year fee was $551. Now it's $731.
You do the math.
And why were the fees against doctors increased?
Because the DEA needed more money. According to the FDA Law blog, the DEA cited a number of factors justifying the fee increase including:
•Expanding the use of Tactical Diversion Squads comprised of DEA diversion investigators and special agents, state and local law enforcement and regulatory officers conducting criminal investigations;That's right, in addition to paying ever-higher taxes, licensure fees, credentialing and continuing education fees, doctors are footing a larger and larger tab of the nation's drug war while simultaneously trying to fight it on the front lines.
•Increased scheduled registrant investigations and inspections;
•Increased drug scheduling actions;
•Responding to the expanding number of synthetic substances such as synthetic cannabinoids and synthetic cathinones; and
•Establishing and maintaining information technology systems for registrants.
Brilliant.
And people wonder why doctors are burnt out and fed up.
-Wes
PS: For more
Monday, December 03, 2012
On Folding
Every surgeon has been there at some time in their career.
It's a horrible, exhausting feeling.
Yet one we all must come to grips with: knowing when to stop.
There you are, six hours into a case, legs rubbery, mind racing, and barely conscious of the world outside the narrow view of the operative field. A life, literally in your hands, asleep now, but hoping (with you) for the best of outcomes on this last try.
"Maybe if I just..." you think, and a new idea is tried to no avail.
"Now, let's look at that again," you ask your techs. "Which electrogram's earlier? That one is CLEARLY earlier...right?" as you try to convince yourself that another choice is better. "What about here?" You go back and recheck once more, just to be sure...
So you do.
And it's still a dangerous spot to burn.
"Maybe it's on the left side?" So you cross to the left side and repeat the process. Everything maps back to the spot your dreaded before.
"Maybe if I give just a little energy here...." You hold your breath.
No effect.
"But if I burn here, I risk giving the patient a pacemaker. We never talked about a pacemaker," you think.
Yet the tachycardia persists, as if laughing at you and your inability to locate its origin.
* Bruuuuhaaaahhaaaahhaaaa... *
"Bastard!" you think. "I can get this!"
So you map above, below, left and right, forward and back...
* Bruuuuhaaaahhaaaahhaaaa... *
Like stubborn mule, you fail to give in. Again.
And again...
Until finally...
... you quit. A white flag raised. It beat you. Yes, you lost.
The supporting team with you, ever helpful, feels the patient's loss with you. They are relieved, though, for a pacemaker will not be in the offing. Like you, they know there will be another day, another arrhythmia: another victory to quell the sting of this defeat.
And while the Defeated hangs his head low to talk to the family, you then realize the the family is just as exhausted and concerned as you. They thank you for trying. They understand.
That's when you know you did the right thing.
-Wes
It's a horrible, exhausting feeling.
Yet one we all must come to grips with: knowing when to stop.
There you are, six hours into a case, legs rubbery, mind racing, and barely conscious of the world outside the narrow view of the operative field. A life, literally in your hands, asleep now, but hoping (with you) for the best of outcomes on this last try.
"Maybe if I just..." you think, and a new idea is tried to no avail.
"Now, let's look at that again," you ask your techs. "Which electrogram's earlier? That one is CLEARLY earlier...right?" as you try to convince yourself that another choice is better. "What about here?" You go back and recheck once more, just to be sure...
So you do.
And it's still a dangerous spot to burn.
"Maybe it's on the left side?" So you cross to the left side and repeat the process. Everything maps back to the spot your dreaded before.
"Maybe if I give just a little energy here...." You hold your breath.
No effect.
"But if I burn here, I risk giving the patient a pacemaker. We never talked about a pacemaker," you think.
Yet the tachycardia persists, as if laughing at you and your inability to locate its origin.
* Bruuuuhaaaahhaaaahhaaaa... *
"Bastard!" you think. "I can get this!"
So you map above, below, left and right, forward and back...
* Bruuuuhaaaahhaaaahhaaaa... *
Like stubborn mule, you fail to give in. Again.
And again...
Until finally...
... you quit. A white flag raised. It beat you. Yes, you lost.
The supporting team with you, ever helpful, feels the patient's loss with you. They are relieved, though, for a pacemaker will not be in the offing. Like you, they know there will be another day, another arrhythmia: another victory to quell the sting of this defeat.
And while the Defeated hangs his head low to talk to the family, you then realize the the family is just as exhausted and concerned as you. They thank you for trying. They understand.
That's when you know you did the right thing.
-Wes
Sunday, December 02, 2012
To Dream the Impossible Dream
To dream the impossible dreamThe transformation has arrived: welcome Physician Leaders one and all! We are health care's future!
To fight the unbeatable foe
To bear with unbearable sorrow
To run where the brave dare not go
To right the unrightable wrong
To love pure and chaste from afar
To try when your arms are too weary
To reach the unreachable star
This is my quest, to follow that star
No matter how hopeless, no matter how far...
"The Impossible Dream" from the play "Man of La Mancha"
Our overriding mantra: "Patients first."
We are about quality. We are about safety. We are about patient satisfaction. We are about leadership, mentorship, inspiration. We are about the feel-good. These principles are how successful companies succeed. We are a team.
There is no use in resisting the transformation. It is here.
It is us.
So smile. Pitch in. Make it our own. Invest in the future. Teach. Research. Educate. Take call. Produce.
And enjoy the meetings, the flip charts, the consultants, the checklists.
All of them.
So much to do, so little time. There are difficult times ahead, but we can make it work when others can't because we're the new generation of Leaders. We know medicine. We get input. We involve the staff. We'll make the tough choices. We keep it upbeat. Always upbeat.
March on, dear Leader!
This is our future, our patients' future.
Now, get back to work, will you? And don't forget the meeting at 7 am.
You rock.
See you then!
Oh, and say "hi" to your kids for me.
Ciao!
-Wes