The second occurred after riding his bike home from the gym. Just after riding his bike home, he became very lightheaded and felt he had to sit on his front porch and nearly lost consciousness. His symptoms passed after resting for about 20 minutes.
While having his blood pressure checked, the nurse noted an irregular pulse. He felt fine and was unaware of his heart rhythm. A 12-lead rhythm strip was obtained and two representative 12-lead rhythm strips from the recording are shown below:
Click image to enlarge
Click image to enlarge
Any ideas? What therapy (therapies?) would you recommend?
-Wes
Strips used with patient permission.

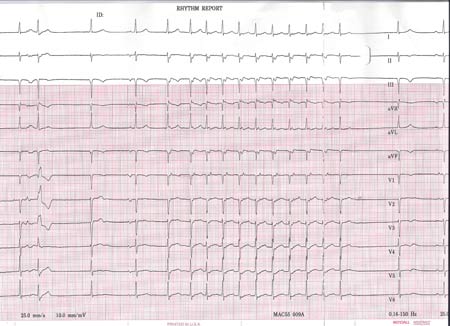
AVNRT? It looks like it is set off with a PVC in the first strip. It looks like the P-waves are visible just after the QRS complex. If that's the case, send him off to the electrical subcontractor :).
ReplyDeleteSick Sinus Syndrome. Especially if it's been occurring regularly. He's going to buy himself a dual chamber pacer, and a daily dose of whatever anticoag the doc wants. For prehospital, manage symptoms as they arise, treat for for hypotension, manage his chest pain, serial 12 leads, and quick transport to the local ED with PCI capabilities, and better yet, one with an EP lab.
ReplyDeleteI think it could be either a focal atrial tachycardia, possibly originating from the right sided pulmonary veins, or a junctional (automatic) tachycardia - I think I'd discuss about an EPS to be able to diagnose and possibly treat it. Rate control isn't that feasible, the basal rhythm being a slow sinus bradycardia alternated with a junctional escape rhythm. Rhythm control, I wouldn't know which drug..
ReplyDeleteI am just an ecg enthusiast and has been watching tracings in real time for alost 5 yrs (but had a previous med training). Here is my take, his arrhythmia starts with junctional bradycardia then a sinus beat follows then a narrow complex wtih a nearly superimposed P wave. After delay of about 600 ms the tachyarrythmia starts. This seems to be a short RP tachycardia (RP about 80 ms). The 2 intial P waves is almost superimplosed on the QRS but later the P waves seems to be distinct after the QRS. An abberantly conducted QRS (ashmann's phenomenon) can be seen with a P nearly superimpose on it. There is spontaneous termination of the arrhtymia. There could be 2 competing pacemakers here (AV dissociation).One from the jucntion and the other inferior and from the left atrium (negative P waves II, III and aVF and positive P in V1). So could this a tachy-brady syndrome (junctional tachycardia on top of atrial tachycardia. If this proves to be the cause of the pre-syncope so PM can help. Drugs maybe not. Just an idea.
ReplyDeletedual AV nodes and a very slow slow pathway creating a 1 P wave to 2 QRS response at baseline. The slow pathway jump allows retrograde re entry up the fast pathway with a retrograde p wave seen on all but the last QRS of the SVT, suggesting re entry as the mechanism. The patient needs a slow pathway ablation or a trial of an AV nodal agent to make re entry and the 1:2 response less likely.
ReplyDeleteHis tachycardia is a response to his bradycardia. Why does he become bradycardic after exercise ? I saw a guy years ago ho became bradycardic during stress test, no other symptoms and normal stress test. He ended up with a pacemaker and an MI 3 months later.
ReplyDeletehow about some love Dr. Wes, what did you find on the EP study?
ReplyDeleteAnony 06:25 PM-
ReplyDeleteMy love can be found here.
Enjoy!