It is tough playing man-to-man when coaches on the sideline keep insisting your team plays zone.
Such is it with health care.
For doctors, the man-to-man defense never ends. Stay with them. Glue to them. Move with them. Run with them. Defend against the bounce pass, or the dribble to avoid the admission. Hands up! Watch their waist, ignore the head fake. You shift your coverage to accommodate their needs. One on one, mana-a-mano.
But for the business of medicine, it's all about the zone. Defend the admission basket against as many people as possible with the least number of defenders. Stay in your position. Work it 2-1-2, 2-3, or if you're really adventurous: 1-2-2. Stick to our limited number of defenses using small variations with the same number of people. Keep your hands up so you look bigger than you are! Don't let them near the hospitalization goal! We've seen all their plays and watched all their moves with our electronic record, so let's win this game! If the patients move left, you move left. If the patient moves right, you move right. Anticipate! How hard can it be?
When you only look from the sidelines, everything seems obvious.
But what happens when the patients change tactics? What if the patient's psyche or medical issues don't follow the typical playbook? Will our zone defense apply enough pressure on patients to affect change? Or will it apply too much pressure upon them, causing them to drop out of the game? Who wins then? When the bench is left too limited and the game extends too long, will the exhausted physician defenders be able to convince the coaches that there's a better way to play defense against these admissions?
Every frontline health care professional knows that the health care game is played one patient at a time and on one court at a time. And yet, we see more courts being built and technologic advances being funded as spectators are sold on the illusion that doctors can suddenly play multiple games on multiple courts with multiple patients with an infinite game clock while never dropping the ball. Even now, the storyline remains: we cannot afford to play health care one-on-one.
So the players become confused. They wonder (more than ever) who they're really playing for. The players wonder why they continue to see more money than God spent on the courts, the lights and the corporate skyboxes instead of the critical players themselves. Will our health care game be won by building more courts or by actually playing the game? How many administrative coaches do we need?
Most of all, since its now come down to money versus care, how will we ever put doctors, hospitals and patients on the same team?
-Wes
Friday, December 30, 2011
Tuesday, December 27, 2011
Where Medicine and Aviation Meet
From Cory Franklin, MD in today's Chicago Tribune:
-Wes
The tragic tale of Flight 447 should not only be a case study in aviation but also in medicine. Medicine is becoming less of a hands-on science and more dependent on sophisticated tests and high-tech scans. As in aviation, there is an overall benefit; diagnosis and treatment are better than ever. But the same problem bedevils medicine, perhaps more commonly — in difficult situations, inexperienced doctors are often uncertain of how to interpret sophisticated information presented to them, resulting in incorrect diagnoses or inappropriate treatment.Read the whole thing.
-Wes
Monday, December 26, 2011
A Look Ahead
Call it an après-holiday reflection, but as I look back at 2011 and anticipate the year ahead it is only natural to ponder what the New Year will bring in of our evolving field of medicine.
What might we expect in the year ahead?
Data Increasingly Becomes King
As the New Year begins, I suspect we will first see more of the same: more market consolidation with larger hospitals eating smaller, financially–strapped hospitals and doctors throwing in the towels of financial independence in favor of corporate employment or retirement. 2011 was the year that cardiologists realized their practice rug was irreversibly pulled out from under them by a 2009 national “stimulus package” whose changes to payments for office based imaging services kicked in on 1 January. Private cardiologists were left with few options to maintain their incomes besides joining with larger hospital systems. It was that same 2009 legislation that provided funds for Electronic Medical Records that gave government-mandated data collection legs.
But the real effects of health care reform have yet to sink in. I expect healthier hospital systems will look for new ways to leverage their current financial largess with national name-brand centers of regulatory excellence to be maintain their public perception as “cutting edge.” With that, the use of data to improve clinical efficiencies while simultaneously using the data to market services will become 2012’s data-driven mantra. Like the fortune-teller’s crystal ball, those centers with the foresight and wherewithal to process and puree the large volume of clinical data spewed forth by today’scaregivers data entry personnel will be richly rewarded as new pressures to the cost curve surface. There will be a distinct competitive advantage to those who can simultaneously compare treatment, demographic, and socioeconomic trends in near real-time with an eye for more financially efficient care.
Privacy Lost
The demand for this data to help to cut costs and maximize profits has already superseded the government’s ability to maintain patient privacy. Oh sure, we’ll still see a handful of large-dollar HiTECH Act and HIPAA violation penalties assessed to make it look like things are under control, but there’s a different reality now: clinical data leaks are worse than ever and not likely to be slowed any time soon. One only has to realize the extent of the mobile-medical movement and the innovations in hand-held devices capable of fully managing patients at a distance to appreciate the futile nature of the government’s ability to enforce the HIPAA/HiTECH acts. After all, despite the government’s heavy-handed wrist-slapping in this regard, I have yet to see a story of how the government recovered any of the data lost or how they rectified damages to those whose medical information has already been compromised. Shouldn’t that be the focus? Sadly, these rules have had another important downside: they put care providers in the impossible catch-22 of trying to maintain data security while health care is provided over larger geographic locations in near real-time, twenty-four hours a day. What do you mean they can’t use their cell phones to send clinical data to each other?
“Repeal and Replace” Has Already Been Replaced
The big news story of 2012 will be the Supreme Court’s ruling on the constitutionality of our new health care law’s mandate to purchase health insurance. Much of the fragmented Republican presidential candidates have vowed to “repeal and replace” the new health care law, but they would be better served to acknowledge that our health care system has already made massive irrevocable changes as far as doctors are concerned. Hence, repealing and replacing the PPACA will not change what has happened to our prior health care delivery mechanism.
Americans should not think for a minute that going back to the days of old doctor’s offices on every corner is possible – it’s become too cumbersome and too expensive to do so. Instead, the local minor care will be by the likes of Rite-Aid, Walmart or Walgreens. For those who want to see a doctor, from now on a nurse might have to do. Appointments for skilled “care providers” will increasingly be made online or via kiosk. If a phone call is desired, large call centers with phone trees with built-in logic and recordings to check for “quality” will be our new reality as disposable administrative health care personnel are increasingly replaced by technology.
Still, some independent doctors’ practices will survive for a while in the more affluent regions of the country. Cash-based practices will flourish thanks to a persistent demand for this care. Their challenge to this model will not be in providing care but rather getting the data to do so. Larger health systems in control of larger laboratory and medical record operations are unlikely to relinquish this data-driven power willingly. Whether these independent physician models will evolve to counteract this reality remains to be seen.
Primary Care Evolves to Specialty Care; Specialists Evolve to Administrators
Want a primary care doctor in 2012? See your specialist. No longer is primary care a visit to the doctor. Need a school physical? See your Walmart nurse. Need a vaccination for overseas travel? See your Rite-Aid pharmacist. Need cholesterol management? See your endocrinologist. You get the point. Primary care doctors (family practice doctors, pediatricians, internists, and even some ob-gyns) will continue their evolution to become managers of fleets of nurse-practitioners or nurse-doctors. The influx of patients and demands on their time will require this. And because data flows to today’s specialists faster than ever, so too will computer-mandated primary health care. In response, specialists will quickly offload these computer-generated demands to their less-skilled counterparts in favor of maintaining new patient appointments more likely to generate their favorite procedural care. But as more and more “procedures” are eyed as ‘expensive,’ proceduralists will increasingly collaborate with hospital administrators as the onus of limiting costs is spread to them. Skilled proceduralists that also carry MBA’s will be viewed by our current cauldren of hospital administrators as 'the bomb.'
Social Media’s Influence On Medicine Grows
Social medicine will continue its parallel track to conventional medicine. People will find support and suggestions from others. Need a good doctor? Ask your friends. Need some information? Ask a friend on line. If they don’t know the answer, they are likely to know someone who they know and trust who will. Think you were gouged on price for a procedure? Ask your friends. The truth will set us free. As patients are presented with more information faster than ever, social media will continue provide a potent concierge service to patients as they negotiate the ever-changing system before them.
* * *
So there you have it. A few of my broad-based pie-in-the-sky projections for 2012. Will they materialize? I can’t be sure. But it's clear the health care cost piñata has burst. Sure there's still a scramble to pick up the few remaining financial health care candies lying around. But the end of our bountiful health care game is fast approaching and what next year's game will become is anybody's guess.
-Wes
What might we expect in the year ahead?
Data Increasingly Becomes King
As the New Year begins, I suspect we will first see more of the same: more market consolidation with larger hospitals eating smaller, financially–strapped hospitals and doctors throwing in the towels of financial independence in favor of corporate employment or retirement. 2011 was the year that cardiologists realized their practice rug was irreversibly pulled out from under them by a 2009 national “stimulus package” whose changes to payments for office based imaging services kicked in on 1 January. Private cardiologists were left with few options to maintain their incomes besides joining with larger hospital systems. It was that same 2009 legislation that provided funds for Electronic Medical Records that gave government-mandated data collection legs.
But the real effects of health care reform have yet to sink in. I expect healthier hospital systems will look for new ways to leverage their current financial largess with national name-brand centers of regulatory excellence to be maintain their public perception as “cutting edge.” With that, the use of data to improve clinical efficiencies while simultaneously using the data to market services will become 2012’s data-driven mantra. Like the fortune-teller’s crystal ball, those centers with the foresight and wherewithal to process and puree the large volume of clinical data spewed forth by today’s
Privacy Lost
The demand for this data to help to cut costs and maximize profits has already superseded the government’s ability to maintain patient privacy. Oh sure, we’ll still see a handful of large-dollar HiTECH Act and HIPAA violation penalties assessed to make it look like things are under control, but there’s a different reality now: clinical data leaks are worse than ever and not likely to be slowed any time soon. One only has to realize the extent of the mobile-medical movement and the innovations in hand-held devices capable of fully managing patients at a distance to appreciate the futile nature of the government’s ability to enforce the HIPAA/HiTECH acts. After all, despite the government’s heavy-handed wrist-slapping in this regard, I have yet to see a story of how the government recovered any of the data lost or how they rectified damages to those whose medical information has already been compromised. Shouldn’t that be the focus? Sadly, these rules have had another important downside: they put care providers in the impossible catch-22 of trying to maintain data security while health care is provided over larger geographic locations in near real-time, twenty-four hours a day. What do you mean they can’t use their cell phones to send clinical data to each other?
“Repeal and Replace” Has Already Been Replaced
The big news story of 2012 will be the Supreme Court’s ruling on the constitutionality of our new health care law’s mandate to purchase health insurance. Much of the fragmented Republican presidential candidates have vowed to “repeal and replace” the new health care law, but they would be better served to acknowledge that our health care system has already made massive irrevocable changes as far as doctors are concerned. Hence, repealing and replacing the PPACA will not change what has happened to our prior health care delivery mechanism.
Americans should not think for a minute that going back to the days of old doctor’s offices on every corner is possible – it’s become too cumbersome and too expensive to do so. Instead, the local minor care will be by the likes of Rite-Aid, Walmart or Walgreens. For those who want to see a doctor, from now on a nurse might have to do. Appointments for skilled “care providers” will increasingly be made online or via kiosk. If a phone call is desired, large call centers with phone trees with built-in logic and recordings to check for “quality” will be our new reality as disposable administrative health care personnel are increasingly replaced by technology.
Still, some independent doctors’ practices will survive for a while in the more affluent regions of the country. Cash-based practices will flourish thanks to a persistent demand for this care. Their challenge to this model will not be in providing care but rather getting the data to do so. Larger health systems in control of larger laboratory and medical record operations are unlikely to relinquish this data-driven power willingly. Whether these independent physician models will evolve to counteract this reality remains to be seen.
Primary Care Evolves to Specialty Care; Specialists Evolve to Administrators
Want a primary care doctor in 2012? See your specialist. No longer is primary care a visit to the doctor. Need a school physical? See your Walmart nurse. Need a vaccination for overseas travel? See your Rite-Aid pharmacist. Need cholesterol management? See your endocrinologist. You get the point. Primary care doctors (family practice doctors, pediatricians, internists, and even some ob-gyns) will continue their evolution to become managers of fleets of nurse-practitioners or nurse-doctors. The influx of patients and demands on their time will require this. And because data flows to today’s specialists faster than ever, so too will computer-mandated primary health care. In response, specialists will quickly offload these computer-generated demands to their less-skilled counterparts in favor of maintaining new patient appointments more likely to generate their favorite procedural care. But as more and more “procedures” are eyed as ‘expensive,’ proceduralists will increasingly collaborate with hospital administrators as the onus of limiting costs is spread to them. Skilled proceduralists that also carry MBA’s will be viewed by our current cauldren of hospital administrators as 'the bomb.'
Social Media’s Influence On Medicine Grows
Social medicine will continue its parallel track to conventional medicine. People will find support and suggestions from others. Need a good doctor? Ask your friends. Need some information? Ask a friend on line. If they don’t know the answer, they are likely to know someone who they know and trust who will. Think you were gouged on price for a procedure? Ask your friends. The truth will set us free. As patients are presented with more information faster than ever, social media will continue provide a potent concierge service to patients as they negotiate the ever-changing system before them.
* * *
So there you have it. A few of my broad-based pie-in-the-sky projections for 2012. Will they materialize? I can’t be sure. But it's clear the health care cost piñata has burst. Sure there's still a scramble to pick up the few remaining financial health care candies lying around. But the end of our bountiful health care game is fast approaching and what next year's game will become is anybody's guess.
-Wes
Sunday, December 25, 2011
Merry Christmas!
Click image to enlarge
Thanks to all the doctors and nurses who contributed. Wishing you all the happiest of holiday seasons!
-Wes
Friday, December 23, 2011
Thursday, December 22, 2011
Dr Wes: Top Ten Posts of 2011
Seems everyone is doing the Top Ten of 2011 thing:
#10. The Results Are In: Age vs. Typing Speed
#9. Appointment Phishing
#8. Rebuttal: NEJM's Justistification for Medical Mystery Shoppers
#7. What They Know
#6. For Interns: Ten Rules to Go By
#5. How to Teach Facebook to an Eighty-Five Year Old
#4. Could a Bra Interfere With A Pacemaker or Defibrillator?
#3. EKG Du Jour #22: A Rare Classic
#2. Our Polite New World of Rationing
#1. How My iPhone Prevented and ER Visit (with Screenshots)
Thanks for all of you who have taken time to improve these posts by leaving your comments and criticisms. You have made it a truly enjoyable and informative year.
Happy holidays and here's to a great New Year of blogging in 2012!
-Wes
- Wall Street Journal: YouTube's Top Ten Videos of 2011 (Can you say Rebecca Black?)
- theheart.org: Top Ten Cardiology Stories of 2011 (registration required)
- PC World: The Top Ten Cell Phones
- CNN: Top Ten Biggest Story in Mobile Media
#10. The Results Are In: Age vs. Typing Speed
#9. Appointment Phishing
#8. Rebuttal: NEJM's Justistification for Medical Mystery Shoppers
#7. What They Know
#6. For Interns: Ten Rules to Go By
#5. How to Teach Facebook to an Eighty-Five Year Old
#4. Could a Bra Interfere With A Pacemaker or Defibrillator?
#3. EKG Du Jour #22: A Rare Classic
#2. Our Polite New World of Rationing
#1. How My iPhone Prevented and ER Visit (with Screenshots)
Thanks for all of you who have taken time to improve these posts by leaving your comments and criticisms. You have made it a truly enjoyable and informative year.
Happy holidays and here's to a great New Year of blogging in 2012!
-Wes
Tuesday, December 20, 2011
My New Holiday Wear
I just received fantastic holiday surgical caps from the incomparable Ramona Bates, MD of the newly re-named Sutured For a Living blog. Here's Mark Metzl, MD (my current fellow) and yours truly sporting the newest OR fashion:
Thanks, Ramona!
-Wes
Thanks, Ramona!
-Wes
The Pressure's On: Last Day to Send a Picture of Your Favorite Holiday Wear
As a reminder, today's the last day to submit a quick picture of your favorite holiday tie, sweater, scrubs, shirt, underwear, socks - whatever - that I can use to photoshop a collage of gear worn by health care professionals all over the world for the holidays. (The original announcement has morphed by popular demand to allow submission of more creative forms of fashion expression.) Deadline is midnight (CST) TONIGHT.
Remember to send a relatively small (<=350K or so) picture of the item to me at wes - at - medtees - dot - com.
We've got a few pictures so far (tie pictured above was from Nick Genes, MD), but plenty more for the color pallate would be greatly appreciated.
Thanks again and Happy holidays!
-Wes
Remember to send a relatively small (<=350K or so) picture of the item to me at wes - at - medtees - dot - com.
We've got a few pictures so far (tie pictured above was from Nick Genes, MD), but plenty more for the color pallate would be greatly appreciated.
Thanks again and Happy holidays!
-Wes
Drug Reps Turned Hospital Reps
From Authentic Medicine:
But we're not talking about patient care here. We're talking about market consolidation and competition for the few remaining revenue sources out there as overbuilt hospitals race to feed the health care and consulting beasts that financially cannibalize the very people they claim to serve.
-Wes
So what happened to the other 75% of reps? Some of them are now working for hospitals to make sales calls on doctors. Why? The hospitals want those docs, usually surgeons, to send their patients to that facility. Uh oh, this may be a problem. Reps are trained well. They are usually aesthetically pleasing (hospitals aren’t stupid) and they go after the doctors with the best insured patients. They mine data just like the drug companies did to find the target doctors. Read this article in the USA Today for more info. I understand why hospitals are doing this but there is something here that just doesn’t sit right with me. I sure wish they would reinvest their money into nurses so that their patient load is less instead of paying beautiful looking reps to flirt with doctors. Seems wrong.It seems wrong, because to doctors, it is wrong.
But we're not talking about patient care here. We're talking about market consolidation and competition for the few remaining revenue sources out there as overbuilt hospitals race to feed the health care and consulting beasts that financially cannibalize the very people they claim to serve.
-Wes
Monday, December 19, 2011
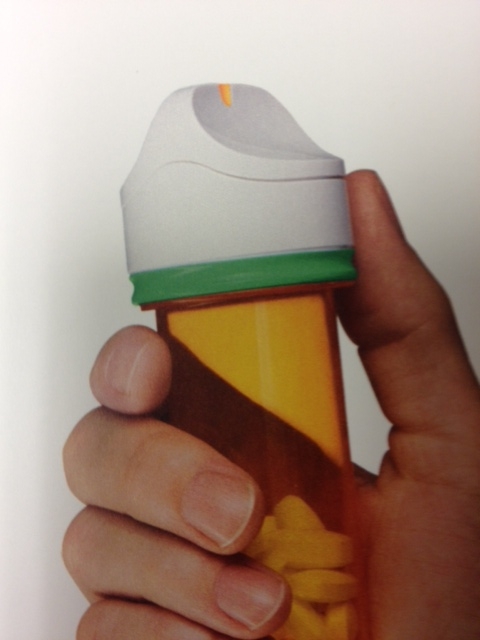
Interactive Pill Bottle Caps
Just saw this advertised for patients taking Multaq (dronedarone): interactive pill bottle caps called "GlowCaps:"
How It Works
GlowcapTM, manufactured by Vitality, Inc, has an embedded computer chip that communicates via low frequency RF with a cellular connected nightlight. The nighlight sends information to Vitality via a GE864-QUAD chip, over the AT&T GSM/GPRS network. Hence you must be in an AT&T wireless network area.
But I do worry about alarm fatigue. And how much does this cost? Will patients just ignore their pills or even grow to hate their melodies? And what happens when everyone's pill bottles go off at the symphony? Or what about pill identification: "Doc, it's the one that sounds like a wind-chime." Finally, if I start getting e-mail reports (spam?) from patients regarding their Multaq pills, I really, really won't be happy.
Just because technology can do all these things, doesn't mean it always should.
Still, it shows where technology is taking us in a hurry.
-Wes
GlowCapsTM is a bottle with built-in wireless communication... When you receive your GlowCapTM, you program it with your schedule. It will then remind you when it's time to take Multaq by lighting up, playing a melody, or calling your home phone. If you and your physician choose, your GlowCapTM can also send weekly reminder e-mail to you and a caregiver, send reports to your doctor, and refills can be initiated with the push of a button, if you provide a phone number when registering.Okay. That's pretty cool.
How It Works
GlowcapTM, manufactured by Vitality, Inc, has an embedded computer chip that communicates via low frequency RF with a cellular connected nightlight. The nighlight sends information to Vitality via a GE864-QUAD chip, over the AT&T GSM/GPRS network. Hence you must be in an AT&T wireless network area.
But I do worry about alarm fatigue. And how much does this cost? Will patients just ignore their pills or even grow to hate their melodies? And what happens when everyone's pill bottles go off at the symphony? Or what about pill identification: "Doc, it's the one that sounds like a wind-chime." Finally, if I start getting e-mail reports (spam?) from patients regarding their Multaq pills, I really, really won't be happy.
Just because technology can do all these things, doesn't mean it always should.
Still, it shows where technology is taking us in a hurry.
-Wes
Christmas's Lessons
"What's your favorite color?" my brother asked me.
I had never been asked that question before, so I had never thought about it. I considered my options: green (everyone's favorite at the time), yellow (somewhat bland), blue (depends on the shade), orange (the color of a fruit? No...), and then came my answer for no apparent reason at the time.
"Red."
Little did I know my older brother was colluding with my family (and Santa, of course) to decide upon the color of a new bicycle. The ruse was revealed at the end of Christmas morning when I followed a string whose one end had been attached to an ornament through every room in our house. It was only after following it to the dank confines of our basement was the surprise revealed.
Ah, the memories.
But for many, the Christmas season will be far removed from this Utopia. Some will hear the terrified cry if a woman screaming for help after her husband collapses before her. For others will come the wailing cry of a mother who learns her child just died. For others, they will witness the silent tears of a man who learns his certain fate after the diagnosis of cancer. For each of these, the depts of despair will seem insurmountable; the sadness, intolerable.
So as I return to work this week, I count my blessings. For it won't be about the gifts that I receive, but rather the giving that will matter. As health care workers, we are invited to glimpse the inner workings of this complicated, messy story called life, a story that never stops. But in doing this, we are taken backstage to witness not just the frailty of the human body and spirit, but its remarkable strength, too. And while we know we won't be able to save everyone's pain this holiday season, know that we are honored to be given the privilege to try.
-Wes
I had never been asked that question before, so I had never thought about it. I considered my options: green (everyone's favorite at the time), yellow (somewhat bland), blue (depends on the shade), orange (the color of a fruit? No...), and then came my answer for no apparent reason at the time.
"Red."
Little did I know my older brother was colluding with my family (and Santa, of course) to decide upon the color of a new bicycle. The ruse was revealed at the end of Christmas morning when I followed a string whose one end had been attached to an ornament through every room in our house. It was only after following it to the dank confines of our basement was the surprise revealed.
Ah, the memories.
But for many, the Christmas season will be far removed from this Utopia. Some will hear the terrified cry if a woman screaming for help after her husband collapses before her. For others will come the wailing cry of a mother who learns her child just died. For others, they will witness the silent tears of a man who learns his certain fate after the diagnosis of cancer. For each of these, the depts of despair will seem insurmountable; the sadness, intolerable.
So as I return to work this week, I count my blessings. For it won't be about the gifts that I receive, but rather the giving that will matter. As health care workers, we are invited to glimpse the inner workings of this complicated, messy story called life, a story that never stops. But in doing this, we are taken backstage to witness not just the frailty of the human body and spirit, but its remarkable strength, too. And while we know we won't be able to save everyone's pain this holiday season, know that we are honored to be given the privilege to try.
-Wes
Saturday, December 17, 2011
Friday, December 16, 2011
12 Days of Christmas - EP Style
In a brief burst of holiday enthusiasm, we worked on a special song today that came together after our fifth case for your enjoyment: The Twelve Days of Christmas, EP Style. Feel free to sing this song in your Electrophysiology Laboratory this Christmas season.
A pacer for a-sys-to-le.
On the second day of Christmas, my true love gave to me,
Two Long QT's
And a pacer for a-sys-to-le
On the third day of Christmas, my true love gave to me,
Three time outs
Two Long QT's
And a pacer for a-sys-to-le.
(You know how the rest goes... Here's the rest of the verses:)
Four LV leads
FIVE HUNDRED JOULES!
Six vessels bleeding
Seven sheath a-splitting
Eight consults waiting
Nine second pauses
Ten incisions weeping
Eleven patients crashing
Twelve hearts a-fibbin'
(Heh. Okay, not perfect, but it helped keep us laughing...)
Merry Christmas!
-Wes
(To the tune of 12 Days of Christmas)
On the first day of Christmas, my true love gave to me,A pacer for a-sys-to-le.
On the second day of Christmas, my true love gave to me,
Two Long QT's
And a pacer for a-sys-to-le
On the third day of Christmas, my true love gave to me,
Three time outs
Two Long QT's
And a pacer for a-sys-to-le.
(You know how the rest goes... Here's the rest of the verses:)
Four LV leads
FIVE HUNDRED JOULES!
Six vessels bleeding
Seven sheath a-splitting
Eight consults waiting
Nine second pauses
Ten incisions weeping
Eleven patients crashing
Twelve hearts a-fibbin'
(Heh. Okay, not perfect, but it helped keep us laughing...)
Merry Christmas!
-Wes
Al Fine
It's busy this time of year for me, so I offer this prior piece, previously published 3 Aug 2010:
“The family wants the pacemaker turned off.”“We don’t typically turn them off.”
“They want it off.”
“It’s 2 am, can it wait?”
“I don’t think so.”
“I’ll head in.”
Bleary-eyed, I rose from bed, dressed, and was out the door. The cool air from the car window served as nature's wake-up call. The sky was clear, the moon hung brightly on the horizon and the cicadas’ shrill songs undulating high above. Driving in, the tires clapped rhythmically from one pavement segment to the next.
* Kla-lup, kal-lup, kal-lup *
For some reason the Emergency Room seemed farther away this night – perhaps because of my reluctance to go there. If the patient was pacemaker dependent, yet alive with a pulse and neurologic signs, the ethical dilemma was a real one: should I be responsible for stopping the patient's heart? Did the family really understand the implications of these actions?
* Kla-lup, kal-lup, kal-lup *
I turned the final time. The ER sign disrupted the dark sky. I parked and fumbled for my ID. The security guard looked remarkably cheery for that time of night.
Reviewing the case, it was a horrible fall, cerebral hemorrhage, neurosurgeon empathically discussed the prognosis with the family and me – little could be done.
On entering the room, what seemed like twenty pairs of eyes were upon me. Some older, some younger, older kids too. Questioning at first. Tearful. Some closed. It had been a long day. So glad I came. Others pointing the way to her, quietly huddled by his side, clutching his hand. She turn her gaze from him for a moment, offered a brief smile, then back to him again. "He was a great man," she said.
Except for the c-collar in place, he looked regal - staring up without movement. He looked younger than his age, an active lifestyle I guessed. His endotrachial tube had already been removed. "We don't want him to suffer."
I glanced at the monitor. 100% ventricular pacing.
Damn.
"We'd like the pacemaker turned off," they reinforced.
"You understand that he might die as a result."
"Yes."
"There's a chance his heart could slow significantly, and not stop."
"We understand. If that's God's will."
I turned to his wife. She seemed at peace. I asked her:
"Are you sure this is how he'd want it?"
"Yes."
"And you understand what we're doing?"
"Yes."
"Would you like to be the one to turn off his pacemaker?"
"Honestly, no. But I'm his wife. This is how he'd want it."
"I'll grab the programmer and be right back. I'm so sorry."
I left the room, wrote a thorough note and pondered the situation as I walked to get the programmer. Usually some other metabolic derangement assists us in stopping the heart of patients with pacemakers - we don't usually turn them "off." The natural consequence of other confounding diseases work to cause a lack of oxygen, too much potassium, or another metabolic problem that disconnects the electrical activity from the mechanical. When the mechanical stops, it really doesn't matter what the electrical system does, since the pumping stops irrespective of the electrical impulses applied to the heart.
* sigh *
I returned and checked the device. Naturally, there was still plenty of battery life left. The rhythmic sound of the monitor was heard in the background as I noted his underlying atrial fibrillation with ventricular pacing.
Da Capo
The family huddled together. They gave Grampa a kiss. More tears. What was I doing? She held his hand, leaned forward, and whispered something in his ear. She did not cry. She was turned and shuffled to the programmer, assisted by her daughter. They stood together, arms entwined. The monitor was hushed, the waveform still visible.
Pianissimo
I handed her the pen and pointed to the spot to touch to program his pacemaker to "off." She looked at the others. They stood together, resolute, tears flowing. She touched the screen. The programmer responded to make sure that this is what she wanted. She confirmed, "Yes."
The pacemaker responded in kind. A long pause, then a slow escape rhythm.
Larghissimo
We were all granted a reprieve. It was not time. A few more notes of the concert called life were still to be played. They thanked me. "Would you mind if we were alone with him?"
"No. Not at all."
I packed up the programmer and pulled the curtain to provide privacy. The monitor out side the room showed an escape rhythm just faster than before. I appended my note with the recent events, spoke with the ER staff, returned the programmer, and headed home.
D.C. al fine.
I was grateful that I could not predict the tempo of death. It was His concerto, not mine after all. As I drove home I noticed the moon was no longer visible on the horizon and in its place were millions of radiant stars.
His metaphor, too.
-Wes
Wednesday, December 14, 2011
A Special Request for the Holidays
In the spirit of good cheer, I have an idea, but I need your help.
I need a picture of your favorite holiday tie or sweater. Not you, mind you, just a close-up picture or your tie or sweater. If you want, I'll try to include your name somehow, just let me know. Try to keep the image under 300K or so in size if you can (my inbox can only hold so many). And please, only one entry per person.
The idea here is to make a collage of items worn by health care personnel during the holidays around the world that I will Photoshop together. I plan to post the image before Christmas for all to enjoy. Deadline for submission is midnight (CST) 20 Dec 2011. Send your entries to: wes - at - medtees dot com.
So get out your iPhone or Droid and get snappin'!
-Wes
I need a picture of your favorite holiday tie or sweater. Not you, mind you, just a close-up picture or your tie or sweater. If you want, I'll try to include your name somehow, just let me know. Try to keep the image under 300K or so in size if you can (my inbox can only hold so many). And please, only one entry per person.
The idea here is to make a collage of items worn by health care personnel during the holidays around the world that I will Photoshop together. I plan to post the image before Christmas for all to enjoy. Deadline for submission is midnight (CST) 20 Dec 2011. Send your entries to: wes - at - medtees dot com.
So get out your iPhone or Droid and get snappin'!
-Wes
Remembering: The Concertos
Today's one of those days this time of year where there just doesn't seem to be enough time, so I offer you a bit of reading from another Christmas season:
The Concertos.
Happy holidays.
-Wes
The Concertos.
Happy holidays.
-Wes
Tuesday, December 13, 2011
Be Wary of Press Releases
Why we need to be wary of press releases, especially when they contain so-called "scientific" content that "pushes the envelope," courtesy of Conan O'Brien:
-Wes
h/t: my brother-in-law on Facebook.
-Wes
h/t: my brother-in-law on Facebook.
Decisions
It is a decision that is not made easily each morning.
It takes a careful consideration of the anticipated caseload or clinic volume. It requires uncanny discretion as one weighs the acuity of the clientele to be encountered – a sensitivity, if you will, to their needs.
He recalls the negativism toward the day’s concern and wonders if his choice has ever really hurt anyone. Imagine the horror if that were true! They are, after all, part of a larger collective, accumulated over the years that hang close to their war-torn brethren. He scoffs at the idea, but still wonders.
He chooses, not one, but all of them and marvels at their assortment, their artistic complexity, their repetition, and the memories: each had it’s own story to tell. He considers the day’s partner like Bob Barker selecting the prize: “Will it be Door Number 1, Door Number Two, or Door Number Three?”
Still, he will never forgot the face of the man whose wife had just died this same week, tears overtaking his lower eyelid as he described their love for each other, the children, the kids all there as she took her last breath. Home was so quiet now. “I just can’t bear going into her closet….” He paused as he tried to composed himself. Then he stopped, eyes full of tears but glowing.
“You know, I like your tie,” he said. “Reminds me of her. Every year she’d give me one of those at Christmas. We’d laugh because she’d try to outdo herself from year to year: green ones, red ones, reindeer, Santa, the whole shebang. Last year’s was the worst! I hated wearing then, but there was no choice. She’d kill me otherwise. But the funny thing was, I never saw a face that didn’t light up in the store or at work as a result. Works that way, ya know? Life is too short, otherwise.”
Yeah, the red reindeer-and-Santa one should do today.
-Wes
It takes a careful consideration of the anticipated caseload or clinic volume. It requires uncanny discretion as one weighs the acuity of the clientele to be encountered – a sensitivity, if you will, to their needs.
He recalls the negativism toward the day’s concern and wonders if his choice has ever really hurt anyone. Imagine the horror if that were true! They are, after all, part of a larger collective, accumulated over the years that hang close to their war-torn brethren. He scoffs at the idea, but still wonders.
He chooses, not one, but all of them and marvels at their assortment, their artistic complexity, their repetition, and the memories: each had it’s own story to tell. He considers the day’s partner like Bob Barker selecting the prize: “Will it be Door Number 1, Door Number Two, or Door Number Three?”
Still, he will never forgot the face of the man whose wife had just died this same week, tears overtaking his lower eyelid as he described their love for each other, the children, the kids all there as she took her last breath. Home was so quiet now. “I just can’t bear going into her closet….” He paused as he tried to composed himself. Then he stopped, eyes full of tears but glowing.
“You know, I like your tie,” he said. “Reminds me of her. Every year she’d give me one of those at Christmas. We’d laugh because she’d try to outdo herself from year to year: green ones, red ones, reindeer, Santa, the whole shebang. Last year’s was the worst! I hated wearing then, but there was no choice. She’d kill me otherwise. But the funny thing was, I never saw a face that didn’t light up in the store or at work as a result. Works that way, ya know? Life is too short, otherwise.”
Yeah, the red reindeer-and-Santa one should do today.
-Wes
Monday, December 12, 2011
Imagining Chicago's Skyline Without Health Care
Walking downtown yesterday in Grant Park, I looked up and marveled at Chicago's skyline. As I looked north, there before me was the huge towering white Aon building (formerly the Standard Oil building) in Chicago, and next to it to the right, a building that seemed, well, pretty huge as well. Only then did I notice it was the Blue Cross Blue Shield building (expanded in 2008 during health care "reform," remember?), and, to the left, the Prudential insurance buildings:
So then I wondered. What would Chicago's skyline look like without medicine?
Chicago's skyline would look very different, indeed.
-Wes
So then I wondered. What would Chicago's skyline look like without medicine?
Chicago's skyline would look very different, indeed.
-Wes
Sunday, December 11, 2011
Hallelujah from Alaska
It was just supposed to be a school computer project from the small Yupiq Eskimo Village of Quinhagak, Alaska, but it's become a YouTube sensation (and for good reason):
-Wes
-Wes
Saturday, December 10, 2011
Preventing Hospital Readmissions for Heart Failure
"How are you feeling Ms. Jones?"Exertional dyspnea. It conjures up a large differential of potential cardiovascular or pulmonary causes. And as the above commonly-encountered doctor-patient conversation demonstrates, the problem is a dynamic one: at rest things are often fine, on exertion or with recumbency less so.
"Fine."
"Have you been more short of breath lately?"
"Not really, just when I exercise."
"How much exercise?"
"I dunno. But after I go to the mailbox and walk back up to the house, I’ve got to stop now where before I didn’t."
Now imagine that the doctor then sees elevated neck veins, hears rales in the lower lung fields, and sees swollen ankles on their patient. Heart failure, right?
Perhaps. But we should recall that heart failure is not a disease, but a condition caused by an underlying pathology. So a slew of diagnotic studies are under taken and if no easily correctable cause identified, symptomatic therapy started. If it's caught early or the ause identified, perhaps an admission will be avoided. But if things progress, Admission Number 1 for "heart failure" is chalked up on the books.
Our new health care law requires (Page 8) doctors avoid expensive hospital readmissions by “intervening” on heart failure since this problem is one of the leading causes of readmissions to hospitals. These readmissions cost our health care system billions of dollars. To prove the point, millions upon millions of dollars have been spent to try to prevent heart failure admissions with the assumption that, surely, many readmissions are preventable and cost savings reflected to our health care system.
We should acknowledge that better compliance with medications, careful management of one’s diet, and avoidance or behaviors known to exacerbate heart failure could be better avoided. For the motivated and highly engaged patient, improvements in readmissions can be made, but I wonder how much so: after all, they’re already the Compliant Ones. It’s the Non-compliant Ones and the Medically Challenging Ones that are the problem for our health care system from a cost standpoint.
The Non-compliants are a particularly difficult bunch. They don’t want to think about their health. They want to think about this weekend’s football game, child’s graduation, their upcoming trip to Europe, or being able to pay this month’s bills. And there are many more Non-compliants than Compliants out there. They are not all Non-compliants because they mean to malign their doctor but rather because life gets in the way of dealing with daily health issues for them. And we’re not even talking about the problems inherent to people with severe shelter, social, education, family and economic challenges. Can we expect our health care system to impact all of these areas to prevent hospital readmissions?
And the Medically-Complex Ones have their own challenges: maybe it's heart failure this week, then maybe a bout with a COPD exacerbation the next. Are they a readmission, too?
You bet.
But this has not influenced attempts at expensive innovation in this area. This past week we saw the second clever innovation for measuring physiologic parameters to predict the development of heart failure suffer a devastating blow at the hands of the FDA:
An FDA advisory panel decided that CardioMEMS failed to prove that its wireless, implantable heart monitor's benefits outweigh its risks, casting a shadow on a potential $375 million acquisition by St. Jude Medical (NYSE:STJ) – which already owns nearly a fifth of CardioMEMS.Recall that this is the same fate that Medtronic's earlier right ventricular hemodynamic pressure monitor, the Chronicle device, suffered in 2007.
The watchdog agency's cardiovascular devices committee decided that a clinical trial of the device, designed to be the first permanent heart implant for a solely diagnostic purpose, was warped by the assiduous care given to its participants. (emphasis mine) That's because the clinicians administering the single-blind trial knew which patients were implanted with the device and made sure they got specialized care.
The panel voted 9-1 that the device is safe, but decided that the trial failed to prove its effectiveness on a 7-3 vote. The committee voted 4-6 that the benefits of the device, which measures pulmonary artery pressure, have been proven to outweigh its risks.
But maybe we can make lemonade our of lemons when it comes to innovation to prevent heart failure. Maybe we can realize the importance of people interacting with people and the time necessary to assure better outcomes in heart failure. And maybe, just maybe, we should realize that even with all the technology in the world, expensive medications and expensive testing, that penalizing doctors and health care providers who spend the time with patients just because they present again to a hospital might be exactly the wrong approach to address our readmission issue.
And maybe we should acknowledge that a good portion of the problem with hospital readmissions starts outside hospitals, not in them.
-Wes
Thursday, December 08, 2011
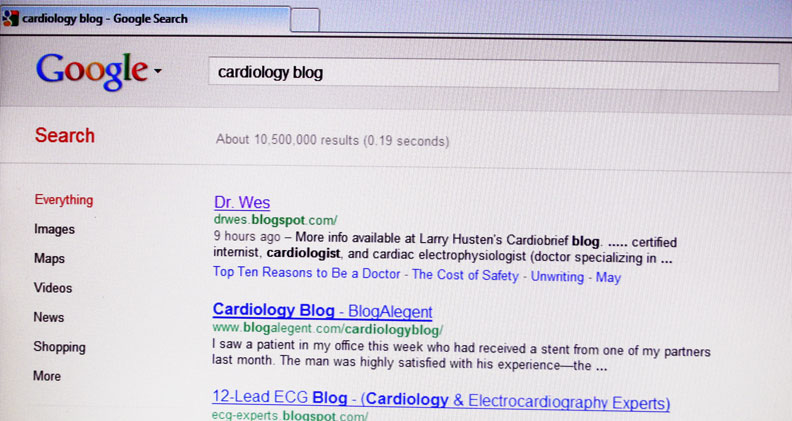
Why Hospitals Should Permit Physician Blogs
Hospitals that permit physicians to participate responsibly on social media can reap significant benefits:
-Wes
Click to enlarge
-Wes
Wednesday, December 07, 2011
When Autocracy Rules
Given the number of sections of the Patient Protection and Affordable Care Act that read "The Secretary shall...", today's single-handed overruling by the Secretary of Health and Human Services' Kathleen Sibelius of the FDA's recommendation to permit the emergency contraceptive Plan B One-Step to go over-the-counter based on years of scientific analysis, should put us on notice. Recall that Ms. Sibelius has no medical or scientific degree. To my knowledge, today's action is unprecedented.
Could the FDA, with their requirements for funding from pharmaceutical companies to review cases like this, have a conflict of interest in regards to their decision?
Of course.
But such an autocratic, non-scientific veto by a single individual in charge of the entire United States' health care policy smacks of dictatorial power and should not be taken lightly by the scientific community or the citizens of this great country.
-Wes
Could the FDA, with their requirements for funding from pharmaceutical companies to review cases like this, have a conflict of interest in regards to their decision?
Of course.
But such an autocratic, non-scientific veto by a single individual in charge of the entire United States' health care policy smacks of dictatorial power and should not be taken lightly by the scientific community or the citizens of this great country.
-Wes
As Goes the Post Office, So Too Medicare?
With the announcement that the Center for Medicare and Medicaid Services (CMS) will begin auditing 100% of expensive cardiovascular and orthopedic procedures in certain states earlier this week, we see their final transformation from the beneficient health care funding bosom for seniors to health care rationer:
But the government has no idea how to do this, really. They don't have the data, the cerebral wattage, acceptable information systems, nor manpower. So, the government will grow further to offset it's shortcomings in order to assure they can "save money" for our health care system.
But CMS, like the U.S. Post Office, has a dirty little secret: they don't pay very well. To offset their low pay, they have to offer some pretty nice benefits to attract their best and brightest. And because the government is now going to bite off trying to manage an entire country's medical procedure rationing during a limited eight-hour government workday, they are going to be flooded with calls, many of which will be frustrated, angry calls that have been on hold a very, very long time.
And so they'll hire more people to improve services.
And pretty soon it will dawn on them: this is expensive to do. It will just be a matter of time when, like the Post Office that was seiged by their inability to keep up with pension and health care costs, they'll surrender and turn over their efforts to private enterprise.
That's because health care is local. Health care is complicated and needs lots of data, systems, and capable facile people to make decisions on data the government wants but knows it doesn't have. (Remember when the Department of Justice had to "consult" with the Heart Rhythm Society to "understand" defibrillator implant practices by tapping into their NCDR database?) Further, because the government moves slowly, can print money when it runs short, and must work through politics, government rarely works under budget. (In fact, when money runs out in government, they just shut down - not a great idea when working in health care.)
Of course the insurers don't want this. They already know it's too damn expensive to take on the risk of our paying for the health care of our aging seniors. (They were one of the main proponents of health care reform, remember?) So the government will have to have their back somehow. (Those details still have to be worked out, but it'll happen because politically, it must).
And the final transformation of our health care system of the future will be complete.
Amen.
-Wes
More info available at Larry Husten's Cardiobrief blog.
This is not at all unexpected. In fact, in our field of cardiac electrophysiology, we have known this day would be coming; our expensive, life-saving gadgets and gizmos are easy targets upon which the government can cut its rationing teeth. And so as it will go for us at first, and then for many other areas of health care.
The Center for Medicare and Medicaid Services will require pre-payment audits on hospital stays for cardiac care, joint replacements and spinal fusion procedures, according to the American College of Cardiology in a letter to members. Shares in both industries fell with Tenet Healthcare Corp., the Dallas- based hospital operator, plunging 11 percent to $4.18, the most among Standard & Poor's 500 stocks. Medtronic Inc., the largest U.S. maker of heart devices, dropped 6 percent to $34.61.
The program means hospitals won't receive payment for stays that involve cardiac care or orthopedic treatment until auditors have examined the patient records and confirmed that the care was appropriate, Jerold Saef, the reimbursement chair for the Florida chapter of the American College of Cardiology, wrote in a Nov. 21 letter to members. The review process is expected to take 30 days to 60 days, beginning January 1, Saef said.
But the government has no idea how to do this, really. They don't have the data, the cerebral wattage, acceptable information systems, nor manpower. So, the government will grow further to offset it's shortcomings in order to assure they can "save money" for our health care system.
But CMS, like the U.S. Post Office, has a dirty little secret: they don't pay very well. To offset their low pay, they have to offer some pretty nice benefits to attract their best and brightest. And because the government is now going to bite off trying to manage an entire country's medical procedure rationing during a limited eight-hour government workday, they are going to be flooded with calls, many of which will be frustrated, angry calls that have been on hold a very, very long time.
And so they'll hire more people to improve services.
And pretty soon it will dawn on them: this is expensive to do. It will just be a matter of time when, like the Post Office that was seiged by their inability to keep up with pension and health care costs, they'll surrender and turn over their efforts to private enterprise.
That's because health care is local. Health care is complicated and needs lots of data, systems, and capable facile people to make decisions on data the government wants but knows it doesn't have. (Remember when the Department of Justice had to "consult" with the Heart Rhythm Society to "understand" defibrillator implant practices by tapping into their NCDR database?) Further, because the government moves slowly, can print money when it runs short, and must work through politics, government rarely works under budget. (In fact, when money runs out in government, they just shut down - not a great idea when working in health care.)
Of course the insurers don't want this. They already know it's too damn expensive to take on the risk of our paying for the health care of our aging seniors. (They were one of the main proponents of health care reform, remember?) So the government will have to have their back somehow. (Those details still have to be worked out, but it'll happen because politically, it must).
And the final transformation of our health care system of the future will be complete.
Amen.
-Wes
More info available at Larry Husten's Cardiobrief blog.
Tuesday, December 06, 2011
Meaningful Abuse
As health care reform rumbles along, it has become increasingly clear that electronic health records (EHRs) are here to stay. I dare say, most of us are relatively happy that the change has come: notes are legible, information moves quickly, communication channels between doctor and patient are improved, and work flows streamlined.
Well, not always.
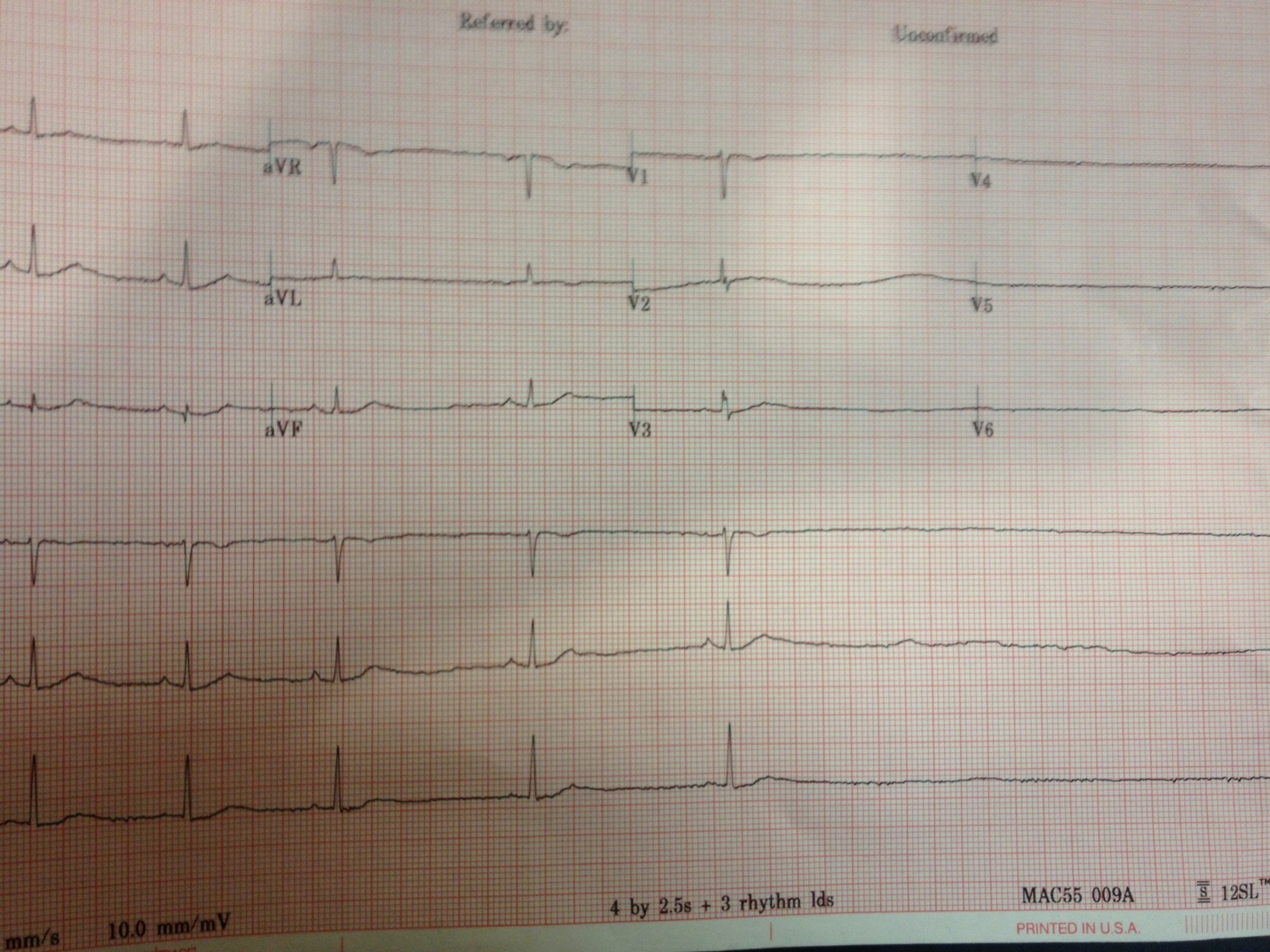
Take the example of the work flow required to process a simple office-based EKG:
Now, multiple that by ten EKG's, three echos, two chest-xrays, and a partridge in a pear tree that gets ordered on our patients each day and you've just created "result bloat" for doctors.
When a single test result must be "resulted" three or more times by the attending physician because of constraints of conjoined information technologies, not only do we demonstrate meaningful use of our electronic medical records, but we also demonstrate meaningful abuse of our doctors' and support staffs' precious time.
First we saw "note bloat."
Now we're seeing "result bloat."
Washington, are you listening?
-Wes
Well, not always.
Take the example of the work flow required to process a simple office-based EKG:
- Enter an order for an EKG
- perform the EKG
- A doctor edits, interprets and signs the computer-interpreted paper EKG
- EKG and it's edits are loaded on the central EKG server
- the results are electronically "signed" by the doctor on central EKG server to it can get posted as "final" on the EHR
- A notice appears in the doctor's EHR results in-box notifying him that a new EKG result is available for review.
- Ideally, the doctor attaches a "result note" explaining the results to the patient and the result forwarded to the patient electronically.
- Except many patients don't use a computer
- So the patient is called and another hand-typed electronic telephone note added to the patient's electronic health record to document that the patient was informed of the result.
Now, multiple that by ten EKG's, three echos, two chest-xrays, and a partridge in a pear tree that gets ordered on our patients each day and you've just created "result bloat" for doctors.
When a single test result must be "resulted" three or more times by the attending physician because of constraints of conjoined information technologies, not only do we demonstrate meaningful use of our electronic medical records, but we also demonstrate meaningful abuse of our doctors' and support staffs' precious time.
First we saw "note bloat."
Now we're seeing "result bloat."
Washington, are you listening?
-Wes
Monday, December 05, 2011
A Little Medical Crystal Ball
I heard this over the weekend:
And yet, when I started medical school, there were no iPhones. In fact, there weren't even cell phones. My first cellphone was acquired while I was in fellowship training and came with a shoulder bag to hold the battery pack. (Man, was I cool to have one!) When I started as an intern, if I wanted to see a patient's chest x-ray I headed down to the file room to check out the patient's xray folder containing all of the films performed on the patient at that hospital and physically removed the particular film of interest from the folder and placed on a lightbox to review. Gosh, we even still had had and used manual blood pressure cuffs.
Things sure have changed. The pace of innovation in medicine has been staggering. Who would have thought you'd need to have typing proficiency to become a doctor? Electrophysiologists, once the boring antiarrhythmic testers of ischemic ventricular tachycardia, don't just test arrhtyhmias, but now routinely ablate them permanently. Stents, unheard of just 20 years ago, are now commonplace. And percutaneous aortic valve replacements and mitral valve repairs? You've got to be kidding me! Congestive heart failure too, once a pre-morbid condition, is now become chronic disease Public Enemy #1 (never mind the dirty truth that it's the innovative drugs and devices that keep people alive and have cost our health care system so dearly). As a result, "readmissions" for heart failure, the inevitable end run of all heart disease, have become a cardinal sin for hospitals thanks to our new health care reform law, punishable by non-payment.
Think practice patterns will change and senior "rehab centers" will benefit as a result? (Does a bear poop in the woods?)
Which leads me to contemplate where things will end up ten or twenty years from now under continued governmental belt-tightening. Will our medical students be better served to learn more medicine, or will should they be shifting their focus to business in an effort to forward themselves? Who will doctors find themselves serving more, their patients or their employers? Will the greatest challenge in health care be promoting life or will it be to promote a death with dignity and without expensive end-of-life care? How will doctors be paid: by salary? By specialty? Or maybe by an obscure, non-transparent concocted "work unit" that an outside hospital consultant group creates?
Even the the grand plan of hospitals called "build it and they will come" is crumbling. Like independent doctors' offices, many smaller hospitals, previously flush with cash and good credit lines, are suddenly finding it harder to stay afloat independently thanks to cuts to Medicare payments. Consolidation continues in health care where only the strongest richest and most politically-connected will survive. Young doctors need to understand these things, lest they work in an environment that might not have their best patient-care interests at heart and their workplace is sold to other larger hospital group intent on cost-saving and 'efficiencies.'
Like it or not, the medical world is rapidly morphing into a business-oriented world. Everything will have a cost and a benefit. It's the "to whom" that will be where doctors' influence will come in: the financial benefit to a hospital system will not always be in the patient's best personal interest. Strattling this divide will be doctors' greatest challenge for all doctors going forward.
But new medical students should not lament: there will still be tons of opportunities for them. Rather, they should accept that right now, this minute, they can have no idea where their current priorities and technical, clinical, and social skills will take them. But they should know this: they'll really need to stay flexible.
Because the only thing unchanging in medicine right now is change itself.
-Wes
"The students of today are training for a field that doesn't currently exist."Seems hard to believe, right?
And yet, when I started medical school, there were no iPhones. In fact, there weren't even cell phones. My first cellphone was acquired while I was in fellowship training and came with a shoulder bag to hold the battery pack. (Man, was I cool to have one!) When I started as an intern, if I wanted to see a patient's chest x-ray I headed down to the file room to check out the patient's xray folder containing all of the films performed on the patient at that hospital and physically removed the particular film of interest from the folder and placed on a lightbox to review. Gosh, we even still had had and used manual blood pressure cuffs.
Things sure have changed. The pace of innovation in medicine has been staggering. Who would have thought you'd need to have typing proficiency to become a doctor? Electrophysiologists, once the boring antiarrhythmic testers of ischemic ventricular tachycardia, don't just test arrhtyhmias, but now routinely ablate them permanently. Stents, unheard of just 20 years ago, are now commonplace. And percutaneous aortic valve replacements and mitral valve repairs? You've got to be kidding me! Congestive heart failure too, once a pre-morbid condition, is now become chronic disease Public Enemy #1 (never mind the dirty truth that it's the innovative drugs and devices that keep people alive and have cost our health care system so dearly). As a result, "readmissions" for heart failure, the inevitable end run of all heart disease, have become a cardinal sin for hospitals thanks to our new health care reform law, punishable by non-payment.
Think practice patterns will change and senior "rehab centers" will benefit as a result? (Does a bear poop in the woods?)
Which leads me to contemplate where things will end up ten or twenty years from now under continued governmental belt-tightening. Will our medical students be better served to learn more medicine, or will should they be shifting their focus to business in an effort to forward themselves? Who will doctors find themselves serving more, their patients or their employers? Will the greatest challenge in health care be promoting life or will it be to promote a death with dignity and without expensive end-of-life care? How will doctors be paid: by salary? By specialty? Or maybe by an obscure, non-transparent concocted "work unit" that an outside hospital consultant group creates?
Even the the grand plan of hospitals called "build it and they will come" is crumbling. Like independent doctors' offices, many smaller hospitals, previously flush with cash and good credit lines, are suddenly finding it harder to stay afloat independently thanks to cuts to Medicare payments. Consolidation continues in health care where only the strongest richest and most politically-connected will survive. Young doctors need to understand these things, lest they work in an environment that might not have their best patient-care interests at heart and their workplace is sold to other larger hospital group intent on cost-saving and 'efficiencies.'
Like it or not, the medical world is rapidly morphing into a business-oriented world. Everything will have a cost and a benefit. It's the "to whom" that will be where doctors' influence will come in: the financial benefit to a hospital system will not always be in the patient's best personal interest. Strattling this divide will be doctors' greatest challenge for all doctors going forward.
But new medical students should not lament: there will still be tons of opportunities for them. Rather, they should accept that right now, this minute, they can have no idea where their current priorities and technical, clinical, and social skills will take them. But they should know this: they'll really need to stay flexible.
Because the only thing unchanging in medicine right now is change itself.
-Wes
Saturday, December 03, 2011
MedTees is Now on Facebook
I just put up the long-overdue MedTees Facebook page last evening. Since May, 2005 it's been an amazing ride with literally thousands of people worldwide purchasing shirts for themselves or their loved ones. (To give you some idea of the number of people we've touched, we sell approximately 250 shirts per month). Insodoing, we contribute to various charities involved with the support of people afflicted with many ailments. Here's a few ways people have used MedTees from our testimonial webpage:
"I am a bi-lateral above knee amputee (I have no legs!). I would like to thank you for providing us with shirts that keep our sometimes sick sense of humor going. Joking around about it is a big part of my rehabilitation. I am a Marine and I lost both my legs in Iraq along with three of my friends who are also bi-lateral and one who is a single above knee. We laugh about it all the time and have fun with it, cause how else can you cope with something like this. "Happy holidays to you all and thanks for making this so much fun.
"Neil," Ishpeming, Michigan, Cpl/USMC, (Injured Dec 7th, 2005 Ar Ramadi , Iraq )* * *
"Loved the philosophy behind your t-shirts. I bought two, one for my oldest daughter Teresa and one for me. Teresa is a cancer survivor. She loves the shirt, but mostly she appreciates the care associated with it."
-Mart* * *
"I wanted to thank you for your efforts and creativity in the t-shirts that you have put out. I had a Long QT incident and was dead for about 7-10 minutes. I was saved by my 8 year old son who dialed 911 and was doing rescue breathing on me when the paramedics arrived. I really like the "Death" t-shirt and the QT shirt. My husband even said that the QT shirt would promote questions by people. Thank you for bringing laughter to such a serious subject."
"Jennifer", Age 36, Colorado
-Wes
Thursday, December 01, 2011
Preventing Sudden Cardiac Arrest Immediately Post-PCI
I participated in a recent case-based discussion via a Medscape audiocast with Ted Feldman, MD and Rina Silver, APN from our institution on the challenges of managing patients post-coronary intervention who also have weak heart muscle function.
-Wes
-Wes