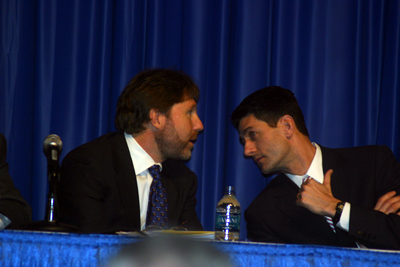
Chris Jennings and Congressman Paul Ryan confer before their 14 March 2010 session at the ACC10 meeting
This morning, Kevin Pho, MD has published on op-ed on a commonly-used tool to determine "quality medicine" from the patient's perspective: patient satisfaction surveys. Like pay-for-performance, this seems like a great idea. One might even logically conclude that doctor's pay should be tied to both pay-for performance measures and patient satisfaction.
But Kevin and Edwin Leap, MD (whose article is referenced in Kevin's piece) point out their concerns with this approach:
Quality health care sometimes means saying "no" to patients, denying them habit-forming pain medications that can feed an underlying, destructive drug addiction, or refusing to order unneeded CT scans that can facilitate harmful radiation exposure.While it's helpful to receive feedback from patients' experiences in the office to improve the quality of the patient's experience and the all-important "brand loyalty" of large health systems in an increasingly competetive health care marketplace, tying the tallied results of these surveys to physician's salaries is a flawed concept.
But Edwin Leap, a physician and columnist, notes that doctors "are constantly under the microscope to give patients what they want, since 'giving people what they want' has been tragically (and falsely) equated with good medicine."
Satisfaction scores give patients a needed voice to express their concerns, which can help medical professionals improve their patient relations. But it's a mistake to use patient satisfaction as a doctor's financial carrot.
-Wes
With patient satisfaction defined as above I totally agree. On the other hand there is immense value and well studied validity in what are called 'Patient Reported Outcome Measures' a.k.a PROM.
ReplyDeleteI have been lucky enough to work with John Wasson MD, Professor @ Dartmouth, one of the giants in this field. His studies dovetail very nicely with the work of Dana Safran (Tufts) and others who have worked on the ACHAPs surveys.
One example: Patient experience of waits and delays predicts follow-through on preventive care and chronic disease outcomes, so patient experience in this context becomes a meaningful measure of the practice performance.
The same is true for all core functions of primary care practices:
Access
Relationship over time
Comprehensiveness
Care Coordination
All of these attributes are highly correlated with the probability of good preventive care and chronic condition management and even hard outcome metrics like:
Missed days from school/work
Emergency room visits
Hospitalization
and outcomes highly meaningful to patients:
Quality of life
Mobility
Pain scores
Emotion scores
So just a caution: when (appropriately) minimizing the importance of patient satisfaction, recognize the immense value in patient experience data. PROM does a better job of predicting outcomes than NCQA's PCMH tool.
L Gordon Moore MD