She was a 42-year old mother of three children who presented with a chief complaint of exertional shortness of breath and progressive swelling of her lower extremities for the past two months. She could not lie flat at night and required three pillows to sleep comfortably. She never had syncope or near syncope, but did note lightheadedness if standing quickly from a sitting position. She had no family history of heart disease or sudden death. She was on no medications, did not drink alcohol, smoke, or use illicit substances.
Her physical examination showed a rapid, irregular pulse of about 120 b/min and a blood pressure of 94/62, jugulovenous distention to the angle of her jaw at 30 degrees, and bilateral rales half-way up both lung fields. She had moderate lower extremity edema. Here's her EKG:
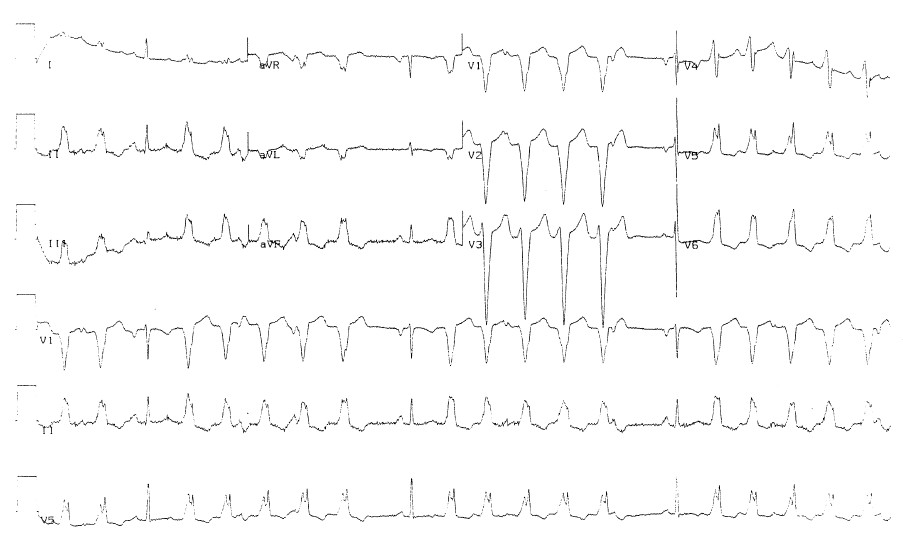
Click to Enlarge
She was admitted and placed on telemetry, a 60-minute strip from which is shown here:
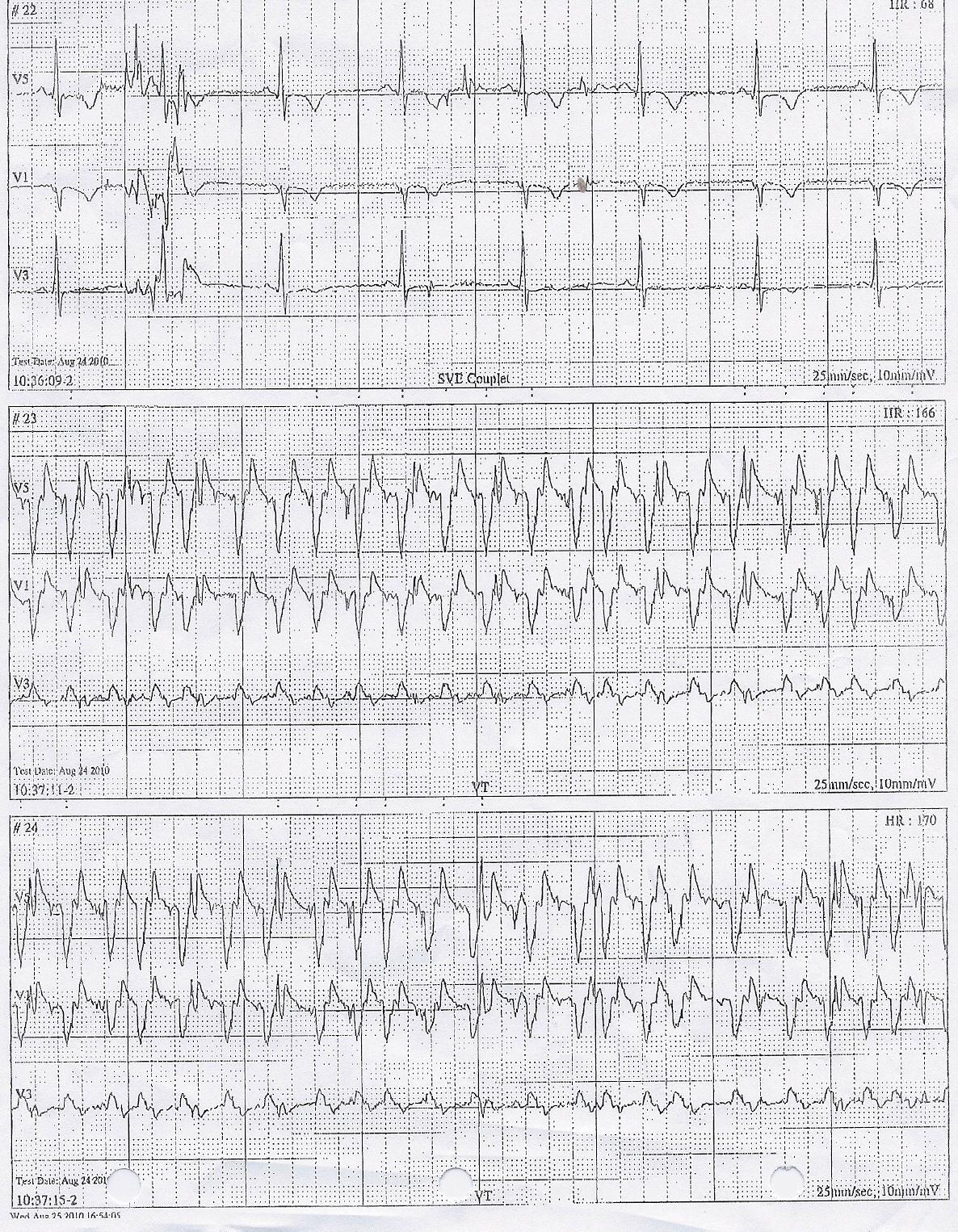
Click to Enlarge
Her echo demonstrated a markedly dilated right and left ventricle with moderate-to-severe mitral regurgitation and left atrial enlargement. Her estimated ejection fraction was 22%.
Sooooo. What is this and what therapy (therapies) would you recommend?
-Wes
First question: VT or abberancy (LBBB)? Probably VT, since there's evidence of AV dissociation (I think I can se dissociated P waves in there).
ReplyDeleteYou can go a step further and say it's probably of right ventricular origin.
That raises 2 possibilities:
One (not my favorite) would be right ventricular cardiomyopathy. Treatment: Medication to calm the electrical storm followed by device therapy.
A more intriguing possibility, and better for the patient, would be RV outflow tract tachycardia which, due to its incessant nature, caused a tacycardia mediated cardiomyopathy. Treatment would be ablation, thus curing the arrhythmia and possibly event the cardiomyopathy.
i'm just an M1...maybe a good dosing of furosemide or the like to start off? maybe also some bundle branch blocking going on as well? that ekg looks kind of ferocious to me...
ReplyDeleteBiV failure in a 42 year old previously healthy without drug or ETOH.
ReplyDeleteShe has acute decompensated systolic heart failure.
viral cardiomyopathy or thyroid would be at my top of the list.
I suppose the MR could be secondary to the ventricular dilation. The RV failure may be secondary to the LV failure. Or as RW Donnell says, may be a primary etiology.
Thats a pretty dang neat looking EKG. It looks like she has a sinus bradycardia, interrupted by a rhytmic wide complex tachycardia, perhaps of a different foci of initiation.
I can't wait for the answer.
I'd agree with incessant RVOT VT likely resulting in a tachycardia induced cardiomyopathy. Another possibility, of course, is arrhthmogenic RV dysplasia (ARVD) or another primary cardiomyopathic process.
ReplyDeleteIt might make sense to go straight to EPS for mapping and ablation before things settle down too much with beta blockers. She'll need to have her volume status optimized of course so she can lay flat and tolerate the procedure. If there is a single site that can be ablated, then do so. After that continue treatment with ACE-I and Coreg titration and hope to see her improve.
Somewhere along the way, an MRI could be considered to rule out ARVD. I guess you should probably do this before the EPS. If she definitely has ARVD, you might be more inclined to treat medically with amiodarone and think hard about ICD rather than ablate. Certainly an ablation strategy could still be considered in ARVD for palliation, but she'd probably still have high risk for malignant VT. We generally still follow guidelines, and hold off on ICD in our cardiomyopathic patients until they have been optimized for three months (unless they have syncope or cardiac arrest). I've seen so many of these patients improve with medical therapy, that I'd hate to obligate her to lifelong device therapy. As much as I hate them, this might be a time I'd consider using a LifeVest wearable defibrillator while things settle down.
Great case Wes, hard to work out on paper with all of the "if . . then . . . " scenarios available.
I hope you tell us she got better. I had an attending in residency who said he used to cringe anytime he heard the words "great case." That usually meant somebody wasn't going to do well.
Jay
We met this woman years ago, and the differential was broad and most have been mentioned: idiopathic or viral cardiomyopathy, hyperthyroid cardiomyopathy, arrhythmogenic right ventricular dysplasia, and peripartum cardiomyopathy that might have gone unrecognized. Less likely, I suppose ischemic cardiomyopathy in the setting of familial hyperlipidemia might have also been in the diferential.
ReplyDeleteShe was generally healthy, except for her severe heart failure. Her thyroid levels were normal, and we were struck by the repetitive and near incessant nature of her arrhythmia. A close look at her Holter showed the same findings for 24 hours: repetitive wide-complex tachycardia.
RW Donnell wisely picked up on the VA dissociation seen on the EKG, confirming that the arrhythmia was ventricular tachycardia, rather than SVT with aberrancy (which would have a 1:1 AV relationship).
She was treated with beta blockers, ACE inhibitors and diuretics (furosemide - strong work frylime!) with improvements in her symptoms, but her arrhythmia persisted.
The patient first went to right and left heart catheterization (probably overkill), but it confirmed normal coronary arteries and moderate mitral insufficiency and elevated right and left heart pressures with bi-atrial enlargement.
Because of concern of a tachycardia-induced cardiomyopathy, she underwent electrophysiology study and catheter ablation of her tachycardia focus. We previously reported the technique used to map and ablate this arrhythmia. A single radiofrequency application successfully terminated the tachycardia. Here's her Holter monitor recording the following night - compared it to the prior holter, it does not show a single premature ventricular beat.
The patient was seen in follow-up six weeks after the ablation procedure. She felt wonderful and follow-up echocardiogram was totally normal, with an ejection fraction of 65% and normal atrial sizes. I was stunned at how quickly her ventricle recovered. She never received an ICD and her medications were discontinued.
A "great case" that had a happy ending. It doesn't get better than this.
If you'll excuse another off-topic comment, I was wondering if you would comment on this "research" by Dr. Langsjoen, a member of THINCS. Dr. Langsjoen states in the press release, er, I mean news article, that a "major scientific journal" is going to be publishing the results of his study. This I gotta see.
ReplyDeletehttp://www.medicalnewstoday.com/articles/100405.php
http://www.kanekaqh.com/pdf/Langsjoen_abstract.pdf
Marilyn
has the penn/marchlinski criteria for localizing the vt by ekg been useful to you in planning these cases? ie notching of the qrs, transition points, width of qrs, etc?
ReplyDeletegreat case! let's see some more of the hall of fame!