I'll be traveling to the far reaches of the earth for an extended weekend with little Internet access. As a result, comment moderation (and certainly the frequency of posts) will suffer.
Back Tuesday.
Happy Summer!
-Wes
Friday, July 30, 2010
Senator Grassley to Mr. Berwick: Show Us the Money
In a letter to Dr. Donald Berwick, the newly appointed Director of the Center for Medicaid and Medicare Services (CMS), Senator Charles Grassley asks for clarification of Mr. Berwick's potential conflicts of interest as Director of his Institute of Health Care Improvement:
Imagine an auto mechanic not taking his car to his own shop.
Imagine a hospital administrator not receiving care in his own hospital.
And yet the American people are to receive care in a system where it's own directors, tasked with making literally life and death decisions on their behalf, are exempt from receiving care in the same system.
-Wes
Reference: IHI's 2009 Federal Tax Form 990.
One of the many significant issues related to your nomination that remains unresolved is the potential for conflicts arising from donors to the Institute for Healthcare Improvement (IHI), the organization you founded and led a Chief Executive Officer. The public has the right to know whether the numerous and significant policy decisions that you make are vulnerable to these potential conflicts of financial interest.More importantly, Mr. Grassley asks:
In addition, please indicate whether IHI continues to provide benefits to you and your family including health care coverage as indicated in IHI's audited financial statement.Imagine a cook not eating at his own restaurant.
Imagine an auto mechanic not taking his car to his own shop.
Imagine a hospital administrator not receiving care in his own hospital.
And yet the American people are to receive care in a system where it's own directors, tasked with making literally life and death decisions on their behalf, are exempt from receiving care in the same system.
-Wes
Reference: IHI's 2009 Federal Tax Form 990.
Wednesday, July 28, 2010
Health Care Reform: Research on Human Subjects?
Every time an experiment on human subjects in proposed in our hospital (or any hospital in the United States for that matter), there is an exquisitely sensitive tuning fork that exists to protect human subjects: the investigational review board or "IRB." Any researcher who has ever brought a research proposal before an IRB knows that any hint of potential harm to a human subject that exists in a research project will kill the proposal faster than you can say "boo."
An IRB submission is required for all research projects using human subjects in accordance with the Federal Policy for the Protection of Human Rights 45 CFR 46, the Food and Drug Administration (FDA) regulations 21 CFR 50, 56 , and with the Federalwide Assurance granted by the H.H.S. Office of Human Research Protections (OHRP).
Every doctor, nurse, hospital administrator, drug or device company involved in human research knows this.
As a researcher on human subjects, I am required to re certify that I understand certain inalienable principles that govern experimentation on human subjects. I re-learn about the 10 principles of the Nuremberg Code and the Belmont Report that grew from our own US Public Health Service's Tuskegee syphilis experiment performed between 1932 and 1972 that studied the natural progression of untreated syphilis on 399 African-American sharecroppers. (The 40-year study was controversial primarily because researchers failed to treat patients appropriately after the 1940s validation of penicillin as an effective cure for syphilis.)
From this grew the six fundamental ethical principles used by the Department of Health and Human services for using any human subjects for research:
Health Care Reform's Upcoming Research
With the passage of the Patient Protection and Affordable Care Act (PPACA) Congress developed the construct for our new health care system going forward, but many, many portions of the law require further study. For instance, experiments (called "pilots" in the legislation) include a national payment pilot on payment bundling (Sec 3202), evaluation of community-based prevention and wellness programs for Medicare beneficiaries (Sec 4202), Pilot testing pay-for-performance programs for certain Medicare providers (Sec 10326), testing the law's affordability provisions, medical home pilot project, and medical liability and medical liability demonstration projects to be undertaken by the states, to name a few. This research will be conducted by a nacient branch of the Department of Health and Human Services called the Center for Medicare and Medicaid Innovation (CMI). It goes without saying that many of the pilots proposed could have grave consequences (either positively or negatively) for our patients. From a recent paper in the New England Journal of Medicine describing the function of the CMI (emphasis mine):
Who will sit on the Investigational Review Board overseeing the government's principle investigator, the Secretary of the Department of Health and Human Services, to assure our patients' most fundamental ethical principles are maintained?
-Wes
An IRB submission is required for all research projects using human subjects in accordance with the Federal Policy for the Protection of Human Rights 45 CFR 46, the Food and Drug Administration (FDA) regulations 21 CFR 50, 56 , and with the Federalwide Assurance granted by the H.H.S. Office of Human Research Protections (OHRP).
Every doctor, nurse, hospital administrator, drug or device company involved in human research knows this.
As a researcher on human subjects, I am required to re certify that I understand certain inalienable principles that govern experimentation on human subjects. I re-learn about the 10 principles of the Nuremberg Code and the Belmont Report that grew from our own US Public Health Service's Tuskegee syphilis experiment performed between 1932 and 1972 that studied the natural progression of untreated syphilis on 399 African-American sharecroppers. (The 40-year study was controversial primarily because researchers failed to treat patients appropriately after the 1940s validation of penicillin as an effective cure for syphilis.)
From this grew the six fundamental ethical principles used by the Department of Health and Human services for using any human subjects for research:
(1) Respect for persons: protecting the autonomy of all people and treating them with courtesy and respect and allowing for informed consent;These principles are the basis for the Health and Human Services human subject protection regulations.
(2) Beneficence: maximizing benefits for the research project while minimizing risks to the research subjects; and
(3) Justice: ensuring reasonable, non-exploitative, and well-considered procedures are administered fairly (the fair distribution of costs and benefits to potential research participants.)
(4) Fidelity: fairness and equality.
(5) Non-maleficence: Do no harm.
(6) Veracity: Be truthful, no deception.
Health Care Reform's Upcoming Research
With the passage of the Patient Protection and Affordable Care Act (PPACA) Congress developed the construct for our new health care system going forward, but many, many portions of the law require further study. For instance, experiments (called "pilots" in the legislation) include a national payment pilot on payment bundling (Sec 3202), evaluation of community-based prevention and wellness programs for Medicare beneficiaries (Sec 4202), Pilot testing pay-for-performance programs for certain Medicare providers (Sec 10326), testing the law's affordability provisions, medical home pilot project, and medical liability and medical liability demonstration projects to be undertaken by the states, to name a few. This research will be conducted by a nacient branch of the Department of Health and Human Services called the Center for Medicare and Medicaid Innovation (CMI). It goes without saying that many of the pilots proposed could have grave consequences (either positively or negatively) for our patients. From a recent paper in the New England Journal of Medicine describing the function of the CMI (emphasis mine):
First, the CMI would run pilot programs rather than demonstration projects. The proposal would give the secretary of health and human services authority to expand pilots that she determines would reduce spending or improve the quality of care. This provision is critical, because the need for congressional approval has delayed or derailed past initiatives.Now given this broad authority granted in this legislation, the poorly defined "objectives" (is cost, quality or quantity of care the "objective?) and no disclosed requirements for the members of CMI, we should ask ourselves a very important question:
. . .
Second, although the CMI proposal lists 18 payment or delivery models for consideration, the center would have broad authority to select the programs best suited to its objectives. In contrast, the CMS’s Office of Research, Development, and Information has far less flexibility, because a large proportion of its resources are devoted to congressionally mandated projects.
A third critical difference is that the CMI would not have to require projects to be budget-neutral during their initial testing period. Many health care innovations require initial investments in staff, training, and infrastructure to achieve long-term efficiencies. But federal budget-neutrality requirements frequently discourage potential applicants, leave valuable concepts on the cutting-room floor at the Office of Management and Budget, and cut short promising programs that appear to be increasing Medicare costs.
Who will sit on the Investigational Review Board overseeing the government's principle investigator, the Secretary of the Department of Health and Human Services, to assure our patients' most fundamental ethical principles are maintained?
-Wes
Tuesday, July 27, 2010
Super Sexy (Adult) CPR
Employment Alert: While there is no frank nudity, viewing video might be best done after hours.
Although this ad for lingerie might not be sanctioned by the American Heart Association, I'll bet you'll never forget CPR after seeing it:Yeah, I know: I'm a dog. And the ad doesn't use the latest no-breath CPR technique.
Still, you have to admit...
... it beats the heck out of the Bee Gees...
-Wes
Dispatching Quangos: Taking a Lesson From Across the Pond
From a recent white paper from England's Prime Minister, Deputy Prime Minister, and Secretary of State for Health about the National Health Service (NHS) we find maybe it's not so great (emphasis mine):
Should be interesting...
Meanwhile, as if blind to England's "model" health care system's struggles, we've just passed a law that emulates their system in its earlier iteration and adds all kinds of yet-undefined and un-budgeted quangos in the name of "cost savings."
Yep, should be interesting...
-Wes
“... the NHS has achieved relatively poor outcomes in some areas. For example, rates of mortality amenable to healthcare, rates of mortality from some respiratory diseases and some cancers, and some measures of stroke have been amongst the worst in the developed world. In part this is due to differences in underlying risk factors, which is why we need to re-focus on public health. But international evidence also shows we have much further to go on managing care more effectively. For example, the NHS has high rates of acute complications of diabetes and avoidable asthma admissions; the incidence of MRSA infection has been worse than the European average; and venous thromboembolism causes 25,000 avoidable deaths each year.And so, the NHS is embarking on a new initiative to reduce their bureaucracy by asking their doctors to not only care for patients, but serve as government contractors for the procurement of supplies using the government's money.
The NHS also scores relatively poorly on being responsive to the patients it serves. It lacks a genuinely patient-centred approach in which services are designed around individual needs, lifestyles and aspirations. Too often, patients are expected to fit around services, rather than services around patients. The NHS is admired for the equity in access to healthcare it achieves; but not for the consistency of excellence to which we aspire."
Should be interesting...
Meanwhile, as if blind to England's "model" health care system's struggles, we've just passed a law that emulates their system in its earlier iteration and adds all kinds of yet-undefined and un-budgeted quangos in the name of "cost savings."
Yep, should be interesting...
-Wes
If You're Wondering Where That Cheap Stethoscope Went
Malaria Vivax Causing Heart Attacks?
Malaria vivax (caused by the usually more indolent plasmodium vivax) is causing a stir in India because of a rash of what sounds like disseminated intravascular coagulation affecting the coronary arteries:
Blood clotting due to malaria till now was seen to occur only in small vessels. An artery getting clogged in new," he said.-Wes
At the Hinduja Hospital, five cases of heart trouble induced by malaria vivax have been treated in the past ten days. Chest specialist Dr Khusrav Bajan said, "Normally we have malaria vivax-positive patients coming in with high fever and body ache.
But this time, almost 30 per cent patients are coming with heart problems, severe breathlessness and restlessness. Some had suffered heart attacks too. Echo clearly indicated depressed heart functions."
Dr Bajan said the number of malaria vivax cases far outsrip that of malaria falciparum this year. "The malaria strain in the city is rapidly mutating and thus the symptoms exhibited by patients are different. The vivax malaria, which earlier was mild in nature, has turned very potent," he added.
Sunday, July 25, 2010
Living Poets Society
 Dr. Charles is hosting a science and medicine poetry contest over at his blog, The Examining Room of Dr. Charles.
Dr. Charles is hosting a science and medicine poetry contest over at his blog, The Examining Room of Dr. Charles. It's a great way to exercise your synapses and maybe earn $500 cool ones and a cherry tomato from his garden.
-Wes
Saturday, July 24, 2010
More Questions About Donald Berwick Surface
With the unvetted recess appointment of Donald Berwick to the Centers for Medicare and Medicaid Services (CMS), some interesting questions that would have been asked at his Senate confirmation hearing were skuttled, like this one:
So it begs the question: who did?
-Wes
This is no small issue since this man now controls nearly half of the half the US health care budget. I can assure you, doctors did not contribute that kind of money to Mr. Berwick's coffers.
Beyond that, the GOP is especially curious about a nonprofit organization Berwick founded, the Institute for Healthcare Improvement. A 501(c)(3) tax-exempt organization, the institute reported receiving $12.2 million in contributions and grants, among other revenues, in 2008 (the most recent year for which figures are publicly available). Given all the money that has flown around in the health care debate, Republicans wanted to know where the $12.2 million came from. The recess appointment meant that Berwick didn't have to answer.
The institute has also been very good to Berwick personally. He received $2.3 million in compensation in 2008 (a figure that included retirement funds), and was paid $637,006 in 2007 and $585,008 in 2006. On top of that, investigators discovered a little-noticed paragraph in an audit report revealing that in 2003 the institute's board of directors gave Berwick and his wife health coverage "from retirement until death."
So it begs the question: who did?
-Wes
Thursday, July 22, 2010
Doctors Debate Obamacare Tonight
Should be an interesting debate on WGN Radio 720 TONIGHT from 10pm-12 midnight Central Standard Time with Milt Rosenberg moderating.
The "favor" physician will be Dr. Arnie Widen, Medical Director of the Office of the Illinois Attorney General and is the immediate past president of CommunityHealth of Chicago. Dr. Widen has been a tireless advocate for CommunityHealth, spending countless hours at the facility, mentoring medical students and treating patients. Like all the doctors there, he believes in the founding statement of CommunityHealth: "Nobody should go without health care." CommunityHealth is the largest volunteer-based, non-profit health care provider in Illinois and one of the largest free clinics in the country.
To "opposing" physician will be Dr. Mark Neerhof, a practicing high-risk obstetrician/fetal medicine specialist and member of Docs4PatientCare, an organization of thousands of concerned physicians committed to the establishment of a health care system that preserves the sanctity of the doctor-patient relationship, promotes quality of care, supports affordable access to all Americans, and protects patients' personal health care decisions.
You should be able to click here to listen in.
-Wes
The "favor" physician will be Dr. Arnie Widen, Medical Director of the Office of the Illinois Attorney General and is the immediate past president of CommunityHealth of Chicago. Dr. Widen has been a tireless advocate for CommunityHealth, spending countless hours at the facility, mentoring medical students and treating patients. Like all the doctors there, he believes in the founding statement of CommunityHealth: "Nobody should go without health care." CommunityHealth is the largest volunteer-based, non-profit health care provider in Illinois and one of the largest free clinics in the country.
To "opposing" physician will be Dr. Mark Neerhof, a practicing high-risk obstetrician/fetal medicine specialist and member of Docs4PatientCare, an organization of thousands of concerned physicians committed to the establishment of a health care system that preserves the sanctity of the doctor-patient relationship, promotes quality of care, supports affordable access to all Americans, and protects patients' personal health care decisions.
You should be able to click here to listen in.
-Wes
The Public Option is Not Dead
No, in fact it is very much alive.
According to the CBO:
My suggestion for Chairman Stark: show us the government can fix Medicare first.
-Wes
According to the CBO:
This morning CBO released a letter to Chairman Fortney Pete Stark analyzing a proposal to add a “public plan” to the options available through the health insurance exchanges that will be established under the recently enacted health care legislation—the Patient Protection and Affordable Care Act, or PPACA (Public Law 111-148).Only problem is, since our government bureaucrats couldn't balance the health care budget with the much smaller Medicare program, what makes them think their next ploy will be any better?
Under the proposal, the Department of Health and Human Services would establish and administer a public health insurance plan and would charge premiums to fully cover its costs for benefit payments and administrative expenses. The plan’s payment rates for physicians and other practitioners would be based on Medicare’s current rates but would not be subject to the future reductions required by Medicare’s sustainable growth rate formula; instead, those rates would initially increase by 5 percent and then would rise annually to reflect estimated increases in physicians’ costs. The plan would pay hospitals and other providers the same amounts that would be paid under Medicare, on average, and would establish payment rates for prescription drugs through negotiation. Health care providers would not be required to participate in the public plan in order to participate in Medicare.
My suggestion for Chairman Stark: show us the government can fix Medicare first.
-Wes
Yet Another Boston Scientific Defibrillator Advisory
With their stock struggling to survive, the latest Boston Scientific defibrillator advisory could not come at a worse time:
-Wes
Addendum:
08:20AM 23 Jul 2010: The Boston Scientific 'Dear Doctor' letter (pdf) regarding the advisory.
Boston Scientific Corp. warned physicians that three of its implantable defibrillators have a defect that can prevent them from working properly, in the latest problem for the company's heart devices.The original physician communication, dated today, can be found in pdf format here.
A magnetic switch on the implantable cardiac defibrillators can get stuck, stopping the devices from delivering an electric shock to the hearts of patients who need the therapy, the company said in a letter to doctors.
The Contak Renewal 3, Contak Renewal 4 and Vitality HE ICDs were made in 2006 and 2007, and about 34,000 remain implanted in patients, according to the Natick, Mass., company, which said on Thursday that it had issued the advisory.
It is unclear how Boston Scientific learned about the problem, and why it issued the advisory now. A company spokeswoman didn't immediately respond to requests for comment.
Boston Scientific said in its product advisory that the risk of harm was remote, and it hasn't received any reports of deaths or injuries. Doctors have replaced some of the devices, according to the advisory, but the company recommends against it.
-Wes
Addendum:
08:20AM 23 Jul 2010: The Boston Scientific 'Dear Doctor' letter (pdf) regarding the advisory.
Wednesday, July 21, 2010
Cell Phone Karma
It was innocent enough. A patient. Syncope. Enough AV block to make you wish the pacemaker was implanted yesterday. Next to the patient: a team of concerned family members in the exam room.
The ER summary and EKG were reviewed. The history taken. The patient politely asked if they might be examined in the presence of family members. "No problem," was the reply.
Examination completed, a blank piece of paper is assembled. A pen, nowhere to be found, was retrieved from the front desk.
Returning, a figure is drawn. The entire room focused. Waiting. Staring at the figure. Total silence.
The explanation begins, then...
With that, a family member dives for their cell phone and hurries to stop the ringtone.
Too late.
The bad karma was released.
-Wes
The ER summary and EKG were reviewed. The history taken. The patient politely asked if they might be examined in the presence of family members. "No problem," was the reply.
Examination completed, a blank piece of paper is assembled. A pen, nowhere to be found, was retrieved from the front desk.
Returning, a figure is drawn. The entire room focused. Waiting. Staring at the figure. Total silence.
The explanation begins, then...
..."Ooh, ooh, ooh, ooh, oohWhat the...?
And she's buying a stairway to heaven."
With that, a family member dives for their cell phone and hurries to stop the ringtone.
Too late.
The bad karma was released.
-Wes
Tuesday, July 20, 2010
The Error In Our Ways
It seems doctors can never do enough. Not only must we diagnose and treat medical illness, this morning in the Chicago Tribune we learn from a study in the Annals of Internal Medicine that used actors posing as patients that seventy-eight percent of doctors make medical errors because we obtain no "contextual history" (another word for "social history?") and adjust our treatment strategies accordingly:
One thing I'm sure of, however, is a doctor's time with a patient is finite. For every click on a computerized quality check-box, we're stealing from the face-to-face time with the patient. Instead of appreciating this fact, our governmental overlords have consistently swollen the number of "quality measures" from 74 in 2007, 119 in 2008, 153 in 2009, to a whopping 179 in 2010. I figure at this rate, using linear regression, we will have about 319 measures by 2014, the same year another 30 million uninsured will be joining our new health care system.
And the government will be proud we're providing such "quality care."
Click. Click. Click.
Never mind these "quality" clicks might just be doing more harm than good.
-Wes
"A lot of doctors are going to say, 'God almighty, it's not enough to be a brilliant clinician? You're telling me I've got to be a financial counselor or social worker on top of that or I'm doing something wrong? Give me a break!'" said John Banja, a medical errors expert at Emory University.Of course, the lack of social history (or many other aspects of the patient's history) is the predictable consequence of shortened office visits, increased administrative burdens, shift-style medical care, and the push to see more patients in less time. It's hard to cover all the bases in seven minutes.
One thing I'm sure of, however, is a doctor's time with a patient is finite. For every click on a computerized quality check-box, we're stealing from the face-to-face time with the patient. Instead of appreciating this fact, our governmental overlords have consistently swollen the number of "quality measures" from 74 in 2007, 119 in 2008, 153 in 2009, to a whopping 179 in 2010. I figure at this rate, using linear regression, we will have about 319 measures by 2014, the same year another 30 million uninsured will be joining our new health care system.
And the government will be proud we're providing such "quality care."
Click. Click. Click.
Never mind these "quality" clicks might just be doing more harm than good.
-Wes
Why Every Heart Patient Should Order Pizza
... because the delivery man might just save your life:
Linn's wife says he had just gone into cardiac arrest Friday when the pizza deliveryman knocked on the door of their Colorado home to bring their order. Kami Linn says she opened the door to "some burly-looking dude" and immediately asked for help.-Wes
Monday, July 19, 2010
Boundaries
Doctor and patient, running a marathon together. Such an inviting story, it just warms the cockles of your heart:
But in reality, blurring the divide between doctor and patient can present considerable problems, too. Psychoanalysts have long understood this problem; they call it countertransference. Maintaining boundaries in our relationships with patients maintains one's ability to remain objective while assessing conditions and while providing recommendations for appropriate therapies. Further, doctor-patient boundaries avoid the potential for a perception of favoritism between patients. For instance, what might other patients that are not invited into the cozy comfort of their doctor's personal life perceive?
This is not to say it is not important to develop professional relationships built on trust with patients. But trust requires us to sometimes recommend things patients might not want to hear if we feel it's in their best interest. This might be harder to do if a relationship becomes enmeshed. Our job is not to be people's friends, but their doctors - and maintaining a healthy divide between professional and social "friends" can be very difficult at times.
So if people wonder why I don't "friend" them on Facebook, it's not because I don't like them. On the contrary, it's because I must respect the delicate boundary that must be maintained between a doctor and patient in order to maintain our professional relationship.
-Wes
“I got to thinking, Hey, I’m going to take full advantage of my health now — I’m going to do a triathlon,” he said.And on the surface, it seems like such an ideal story.
To raise the stakes, he decided to challenge Stewart, who was not a likely triathlete, either. As a doctor who performs 400 heart surgeries a year, each about six hours long, Stewart did not have much spare time to spend at the gym. His usual dinner, he said, was pizza or Taco Bell.
But he accepted O’Keeffe’s challenge, even if he had doubts.
But in reality, blurring the divide between doctor and patient can present considerable problems, too. Psychoanalysts have long understood this problem; they call it countertransference. Maintaining boundaries in our relationships with patients maintains one's ability to remain objective while assessing conditions and while providing recommendations for appropriate therapies. Further, doctor-patient boundaries avoid the potential for a perception of favoritism between patients. For instance, what might other patients that are not invited into the cozy comfort of their doctor's personal life perceive?
This is not to say it is not important to develop professional relationships built on trust with patients. But trust requires us to sometimes recommend things patients might not want to hear if we feel it's in their best interest. This might be harder to do if a relationship becomes enmeshed. Our job is not to be people's friends, but their doctors - and maintaining a healthy divide between professional and social "friends" can be very difficult at times.
So if people wonder why I don't "friend" them on Facebook, it's not because I don't like them. On the contrary, it's because I must respect the delicate boundary that must be maintained between a doctor and patient in order to maintain our professional relationship.
-Wes
Sunday, July 18, 2010
EMR Lingo
Quick EMR quiz:
Just thought you should know.
-Wes
Which is the most different?Programmers: the semantics of the subtleties between a "result," "unresult," or "overdue result" (not to mention why a medication cosign should any different from all our other order cosigns) leaves all of us who do real medicine completely in the dark.(1) An "unresulted order"Answer:
(2) An "overdue result"
(3) A "result"
(4) An "order cosign"
(5) or a "medication cosign?"
Group highlights (and hence group sign-offs) are not allowed for "unresulted orders" whereas they are for all the others.
(This means I must click every single "unresulted order" one-at-a-time, even though I have no clue how an unresulted order is different from any other order or result.)
Just thought you should know.
-Wes
Social Media Tonality
I sit before the computer this morning struggling to write. It happens from time to time, I know, but for come reason I find myself at a particularly difficult impasse.
No doubt being on call this weekend has contributed to my state of ennui, but I often stop to think about the direction of this blog and it's tone. After all, the tone of any blog (heck, any social media venue) not only defines your writing style, but it increasingly defines you to the public. Too light and you're not authoritative. Too heavy and you lose people. Too pessimistic and you sound like a cry baby. Too optimistic and people will wonder what you're smoking.
For this reason, blog tone (and the tone of any social media venue for that matter) should probably be appreciated more by bloggers and social media enthusiasts. After all, not only does the tone of the blog define the writer, but it likely defines the type of person who reads the blog, too.
These days in health care, I find this to be particularly true.
I worry about sounding too pessimistic about the changes I see in health care. I don't want to sound like a "Debbie Downer." If I talk about the discouraging changes to health care under way, I'll be labeled a whiner - just another disgruntled, impotent doctor who has nothing to contribute. Worse: that's not a leadership stance to take in our new Accountable Care Organization.
Who wants to be that guy?
Instead, I should be a cheerleader for health care in the interest of my patients and health care system going forward. I must overcome, improvise, adapt. "When the going gets tough, the tough get going." We must do more with less and do it with quality - 179 measures of nothing but the best. So go ahead. Check the boxes. Show the world the wonderful things we do in health care every day! Look at our gorgeous new facilities and beautiful clinics! We can do it with fewer people than ever before because we keep finding new efficiencies! Everyone's a winner!
And let my online persona reflect my enthusiasm, the opportunity, the wonderful!
I'm just glad to know that I'm not the only one who's discovered this secret to success.
-Wes
No doubt being on call this weekend has contributed to my state of ennui, but I often stop to think about the direction of this blog and it's tone. After all, the tone of any blog (heck, any social media venue) not only defines your writing style, but it increasingly defines you to the public. Too light and you're not authoritative. Too heavy and you lose people. Too pessimistic and you sound like a cry baby. Too optimistic and people will wonder what you're smoking.
For this reason, blog tone (and the tone of any social media venue for that matter) should probably be appreciated more by bloggers and social media enthusiasts. After all, not only does the tone of the blog define the writer, but it likely defines the type of person who reads the blog, too.
These days in health care, I find this to be particularly true.
I worry about sounding too pessimistic about the changes I see in health care. I don't want to sound like a "Debbie Downer." If I talk about the discouraging changes to health care under way, I'll be labeled a whiner - just another disgruntled, impotent doctor who has nothing to contribute. Worse: that's not a leadership stance to take in our new Accountable Care Organization.
Who wants to be that guy?
Instead, I should be a cheerleader for health care in the interest of my patients and health care system going forward. I must overcome, improvise, adapt. "When the going gets tough, the tough get going." We must do more with less and do it with quality - 179 measures of nothing but the best. So go ahead. Check the boxes. Show the world the wonderful things we do in health care every day! Look at our gorgeous new facilities and beautiful clinics! We can do it with fewer people than ever before because we keep finding new efficiencies! Everyone's a winner!
And let my online persona reflect my enthusiasm, the opportunity, the wonderful!
I'm just glad to know that I'm not the only one who's discovered this secret to success.
-Wes
Friday, July 16, 2010
Anesthesiologists See the Cool Stuff
... like this atrial myxoma after it's been resected.
-Wes
P.S.: A pretty good review on myxomas can be found here.
-Wes
P.S.: A pretty good review on myxomas can be found here.
Thursday, July 15, 2010
Clevand Clinic In Chicago?
All I can say is, best of luck:
Unless, of course, it costs a whole lot less to buy a Ford.
-Wes
In a move likely to shake up the market for heart care in the Chicago area, the well-known Cleveland Clinic’s cardiac surgery program said Thursday that it has signed an affiliation agreement with Central DuPage Hospital in the western Chicago suburbs.This won't shake up the market in Chicago. After all, when you have a bunch of Cadillac's in garage, why go after a Ford?
The internationally known Cleveland Clinic draws patients from more than 85 countries around the world for everything from open-heart surgery and valve replacement to heart transplants. Its deal with Central DuPage, in Winfield, is designed to enhance the heart care provided at the 313-bed community hospital and potentially bring Cleveland Clinic patient referrals at a time heart surgeries are less needed than they were a decade ago.
Unless, of course, it costs a whole lot less to buy a Ford.
-Wes
Wednesday, July 14, 2010
Looks Like My Job Will Be Secure
All it takes to assure you will keep your local cardiologist employed is 19 strips of bacon and one egg and you've got yourself one heck of a solid bacon burger:
-Wes
Having read about the difficulties people making such burgers have had keeping them together, I decided to add one large egg to the food processor along with the 19 slices of bacon. I ground the bacon and the egg together, then, using my hands, pulled the mixture out and used a hamburger press to make a burger. It is possible that my hands have been greasier at some point in my life, but if so I have (fortunately) forgotten it. I was not quite prepared for the raw burger to look like pure fat, and I must admit that it didn’t look very appealing. But it was for science, so I soldiered on!My family and I thank you, America!
I put the burger on the rack-Pyrex assembly and slid it under the broiler. Having learned a lesson from last week, I turned the stove exhaust fan to high immediately. I peeked in on it as it cooked, and it seemed to be cooking nicely, with tons of little fat bubbles sizzling on top. After seven minutes or so, I took it out to turn it over, and was pleased how easily it flipped. Five minutes later, it looked done, so I took the temperature of the inside (you need to be careful with pork, of course), and it registered at 160 degrees Fahrenheit, so out it came. Now it looked like food, and smelled delicious.
-Wes
Tuesday, July 13, 2010
Remote ICD Interrogation and the Challenges of Telemedicine
This week in Circulation an article was published (before print) about the safety and efficacy of remote monitoring for implantable cardioverter-defibrillator (ICD) follow-up in the industry-sponsored TRUST (Lumos-T Safely RedUuceS RouTine Office Device Follow-up) Trial. This trial randomized 1339 patients in a 2:1 fashion between internet-based “home-monitoring" of patient’s ICD’s and conventional office-based follow-up of ICD’s. While the results of the trial were interesting in regards to ICD follow-up management using the two venues, the trial is even more interesting if one considers the implications of this trial to telemedicine in general.
By way of background, patients with ICD’s are burdened with frequent follow-up to their doctors with guidelines requiring visits very three to six months. With more patients receiving implanted devices that contain more capabilities beyond just pacing and defibrillation (like arrhythmia and fluid-status monitoring), the volume of patients risks outstripping the number of available appointments. Further, it is no secret that device companies would love to reduce their manpower burden for follow-up to reduce their costs since many small doctors offices turn to the device companies for the technical aspects of follow-up support.
Enter home monitoring via the Internet. Using this technology, patients can upload their device data from home, have it reviewed online, and since 90% of device checks require no “actionable” follow-up, forgo a trip to the device clinic if no problems are identified. In fact, the TRUST trial concluded that “Home monitoring is safe and allows more rapid detection of actionable events compared with conventional monitoring in patients with implantable electronic devices.” The authors clearly achieved their stated goals, demonstrating a significant reduction in hospital encounters from 3.8 visits per patient/yr in the control group to 2.1 visits per patient/yr in the intervention group, with no increase in death, stroke, or surgical interventions in patients treated with home monitoring.
What’s not to like, right?
But there are some potential challenges ahead.
For one, in the TRUST trial the decrease in scheduled hospital encounters was partially offset by a significant increase in unscheduled encounters from 0.5 per patient/yr to 0.78 per patient/yr, mostly due to visits following event notifications from the home monitoring device.
Secondly, in his editorial on the study, Dan Matlock, MD from the University of Colorado cautioned that the quality of the TRUST trial fell short in it’s “patient-centeredness” and suggests that “the trial was designed with the belief that multiple follow-up visits are a burden that primarily falls on the providers.” He offers the following cautionary analogy:
Certainly, there appears to be great potential for improved access for care with remote monitoring and telemedicine in our increasingly cost-constrained health care system. Still, doctors and telemedicine developers must assure our recommended treatment strategies that result from improved detection do not conflict with our patients' perspectives, needs and values for their care.
-Wes
References:
Varma N, Epstein AE, Irimpen A, Schweikert R, Love C, for the TRUST Investigators. "Efficacy and Safety of Automatic Remote Monitoring for Implantable Cardioverter-Defibrillator Follow-Up: the Lumos-T Safely Reduces Routine Office Device Follow-Up (TRUST) Trial." Circulation. 2010;122:325–332.
Matlock DD. "Big Brother Is Watching You - What Do Patients Think About ICD Home Monitoring? Circulation 2010;122:319-321.
By way of background, patients with ICD’s are burdened with frequent follow-up to their doctors with guidelines requiring visits very three to six months. With more patients receiving implanted devices that contain more capabilities beyond just pacing and defibrillation (like arrhythmia and fluid-status monitoring), the volume of patients risks outstripping the number of available appointments. Further, it is no secret that device companies would love to reduce their manpower burden for follow-up to reduce their costs since many small doctors offices turn to the device companies for the technical aspects of follow-up support.
Enter home monitoring via the Internet. Using this technology, patients can upload their device data from home, have it reviewed online, and since 90% of device checks require no “actionable” follow-up, forgo a trip to the device clinic if no problems are identified. In fact, the TRUST trial concluded that “Home monitoring is safe and allows more rapid detection of actionable events compared with conventional monitoring in patients with implantable electronic devices.” The authors clearly achieved their stated goals, demonstrating a significant reduction in hospital encounters from 3.8 visits per patient/yr in the control group to 2.1 visits per patient/yr in the intervention group, with no increase in death, stroke, or surgical interventions in patients treated with home monitoring.
What’s not to like, right?
But there are some potential challenges ahead.
For one, in the TRUST trial the decrease in scheduled hospital encounters was partially offset by a significant increase in unscheduled encounters from 0.5 per patient/yr to 0.78 per patient/yr, mostly due to visits following event notifications from the home monitoring device.
Secondly, in his editorial on the study, Dan Matlock, MD from the University of Colorado cautioned that the quality of the TRUST trial fell short in it’s “patient-centeredness” and suggests that “the trial was designed with the belief that multiple follow-up visits are a burden that primarily falls on the providers.” He offers the following cautionary analogy:
A good basis for interpreting the TRUST trial is to draw comparisons with the prostate-specific antigen (PSA) controversy. There was never a debate that the PSA test detects prostate cancer earlier, and the test was widely adopted by the medical community without any evidence of improved outcomes. Finally, after two decades of use, two large, randomized trials studying the effects of PSA screening were published. Only one of the two trials actually demonstrated a benefit, showing a reduction in death from prostate cancer of seven per 10 000 men screened over nine years. This benefit was coupled with an additional 340 diagnoses of prostate cancer, 177 prostatectomies, and 97 radiation therapies. The second trial did not demonstrate any benefit of PSA testing at all. Rather than being a story of saving lives, the story of PSA testing has been one of false positives, frequent biopsies, indolent cancer, patient anxiety, impotence, and incontinence.It is easy for those of use who are computer-savvy to assume that patients will all leap to home monitoring or telemedicine as their preferred means to address many of their medical concerns. But as the sensitivity for “actionable” items increases thanks to the capabilities of this technology, there is the potential that treatments that ensue adds other unforeseen risks for our patients. For instance, take the example of asymptomatic atrial fibrillation detected by a heart failure patient’s ICD who is already on warfarin: do they really need an immediate cardioversion (and the costs, risks of sedation, and anxiety surrounding the finding) or might the patient have be just as well served by less aggressive conventional follow-up?
Considering the lessons learned from PSA, the TRUST trial leaves some important questions unanswered. Namely, what are the benefits and harms of detecting “actionable events,” and what do patients think of home monitoring?”
Certainly, there appears to be great potential for improved access for care with remote monitoring and telemedicine in our increasingly cost-constrained health care system. Still, doctors and telemedicine developers must assure our recommended treatment strategies that result from improved detection do not conflict with our patients' perspectives, needs and values for their care.
-Wes
References:
Varma N, Epstein AE, Irimpen A, Schweikert R, Love C, for the TRUST Investigators. "Efficacy and Safety of Automatic Remote Monitoring for Implantable Cardioverter-Defibrillator Follow-Up: the Lumos-T Safely Reduces Routine Office Device Follow-Up (TRUST) Trial." Circulation. 2010;122:325–332.
Matlock DD. "Big Brother Is Watching You - What Do Patients Think About ICD Home Monitoring? Circulation 2010;122:319-321.
Monday, July 12, 2010
Bundled Payments To Start Next Year
Doctors better make nice with hospital systems since it looks like bundled payments to "Accountable Care Organizations" in Illinois will start very soon (emphasis mine):
-Wes
The federal Medicare program will test lump-sum payments, known as "bundled payments," in certain markets, and probably wouldn't adopt them more broadly for years. But Chicago hospitals need to hurry: Blue Cross & Blue Shield of Illinois aims to roll out bundled payments in contracts with some hospital systems and physician groups starting next year.For patients who present with more than one medical problem at a time, please be kind enough to notify your doctor which payment bundle you'd like them to address, since only one payment per patient per episode of care will be permitted.
The city's dominant insurance carrier expects that by the end of 2011, 10% of its membership will be covered by contracts that pay providers on an episode-of-care basis, says Steve Hamman, the insurer's vice-president of network management. UnitedHealth Group Inc., the No. 2 insurer in Chicago, also plans to test bundled-payment here and elsewhere, Chief Medical Officer Sam Ho says.
-Wes
Sunday, July 11, 2010
The End of "Rescue Medicine"
Like many others, I am still reeling from the "recess appointment" of Dr. Donald Berwick as the new Director of the Center for Medicare and Medicaid Services (CMS). But unlike others who feel his appointment was a "sneeky move," I would have to admit that it was brilliant political display of "The Chicago Way."
You see in Chicago, if you hold a position of great stature politically, you don't have to ask permission from anyone to do things. You just do them.
Don't like an airport and want it closed? Just call The Boys and have them go out and rip up its runway under the cover of darkness. You just have to have some forward-looking perspective: like a cool $1.4 million a year in revenues that can be gained from the amphitheatre The Boys build there.
Problem handled.
When things like this happen here, people kick and scream and fuss and fume, but they're ultimately left powerless to do anything about it, so they just take some money and move on.
And so it is likely to be with medicine.
For quite a while.
Oh sure, we can all kick and scream and fuss and fume, but it would be far better for us understand what we've really just gained.
It is not just the shift from "rescue care" to the philosophy of a "redistribution of wealth" as Mr. Berwick has espoused earlier:
"You could have protected the wealthy and the well, instead of recognizing that sick people tend to be poorer and that poor people tend to be sicker, and that any healthcare funding plan that is just, equitable, civilized and humane must -- must -- redistribute wealth from the richer among us to the poorer and less fortunate," Berwick said in a 2008 speech in London on the virtues of the British healthcare system. "Excellent healthcare is by definition redistribution. Britain, you chose well."No, it is far more sinister.
My concern is that rather than achieving a overt means of health care rationing vetted by the populous, the covert nature of health care rationing will continue via administrative fiat. As such, people and large health care institutions will continue to be given their government payments to "play nice" by the many, many new "rules," or else. In effect, our health care system has the potential to evolve into a macabre reenactment of bloated, bureaucratic system that defines "The Chicago Way."
After all, since Mr. Berwick won't insist on his own appointment be publicly vetted before our elected representatives, what will that mean for the health care decisions that come from his office and costs of the bureaucracy behind it all?
-Wes
How to Become a Practice Administrator
First, you have to work in hematology/oncology and be able to read a script for a video on how to become a cardiologist:
(Sadly, he somehow fails to mention the costs involved and the ongoing recertification requirements.)
-Wes
(Sadly, he somehow fails to mention the costs involved and the ongoing recertification requirements.)
-Wes
Saturday, July 10, 2010
If Doctors Billed Like Laywers
From a discussion thread on Medscape (registration required) posted in response to comments on my earlier post entitled "If Lawyers Billed Like Doctors:"
-Wes
Mr Clark it appears quite likely you are having a heart attack and will require my services. I will need a retainer of $1500 via either cash or cashier's check. This does not cover any treatment but merely retains me as your physician.Ouch.
Then you will need to deposit $5000 into an escrow account. I will bill this account for services rendered. My charges are $400 an hour and I bill in 15 minute increments. Which means if it takes me 5 minute to review your EKG I still bill for 15. When the escrow account reaches $1000 you will need to deposit an additional $4000 to the account or I will cease to be your physician and you forfit the money in the escrow as well as the retainer and if you continue to require my care you will need to retain me again.
Would you like me to treat your heart attack?
-Wes
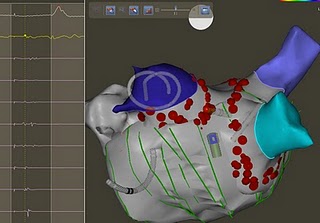
Atrial Fibrillation: To Ablate or Not Ablate - That Is the Question
I should have referenced this earlier: 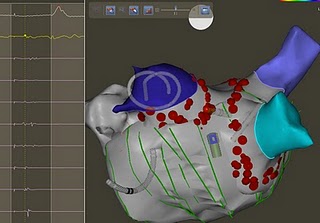 Dr. John Mandrola, cardiac electrophysiologist from Lousville, KY offers his thoughts on the complexities of trying to decide when atrial fibrillation ablation therapy is appropriate (as opposed to medical therapy) and provides an excellent overview of the varying factors that weigh upon that decision.
Dr. John Mandrola, cardiac electrophysiologist from Lousville, KY offers his thoughts on the complexities of trying to decide when atrial fibrillation ablation therapy is appropriate (as opposed to medical therapy) and provides an excellent overview of the varying factors that weigh upon that decision.
I would only like to reinforce his suggestion for patients to consider enrolling in the NIH-sponsored prospective randomized CABANA trial that compares drug versus ablative therapy in symptomatic patients with atrial fibrillation. Only through careful, systematic study of this disorder can we hope to improve our understanding of the best treatment recommendations for atrial fibrillation.
-Wes
h/t: Reminder offered by @HRSOnline via Twitter.
Image courtesy the Dr. John M blog.
 Dr. John Mandrola, cardiac electrophysiologist from Lousville, KY offers his thoughts on the complexities of trying to decide when atrial fibrillation ablation therapy is appropriate (as opposed to medical therapy) and provides an excellent overview of the varying factors that weigh upon that decision.
Dr. John Mandrola, cardiac electrophysiologist from Lousville, KY offers his thoughts on the complexities of trying to decide when atrial fibrillation ablation therapy is appropriate (as opposed to medical therapy) and provides an excellent overview of the varying factors that weigh upon that decision.I would only like to reinforce his suggestion for patients to consider enrolling in the NIH-sponsored prospective randomized CABANA trial that compares drug versus ablative therapy in symptomatic patients with atrial fibrillation. Only through careful, systematic study of this disorder can we hope to improve our understanding of the best treatment recommendations for atrial fibrillation.
-Wes
h/t: Reminder offered by @HRSOnline via Twitter.
Image courtesy the Dr. John M blog.
Friday, July 09, 2010
The Perils of Anti-Social Media
10 pm: Somewhere, under the faint glow of an incandescent light in a back bedroom echoes a voice:
11:01pm: What the ...? Damn. They said THAT? Just a few words on the blog… Shouldn’t take too long…”
(Tweetdeck minimized. Blogger fired up...)
* click click click click click click clickity click …*
Midnight: “Takin' shape. Now, just need a tie up the piece with a linked references. ”
* click clickity click click click clickity click …*
12:20 am:
Silence. Proofreading. Then:
“I can’t publish this! It's horrible! * sigh * I've got to look at this again in the morning.”
12:40 am: Windows are minimized, computer left on. Incandescent light extinguished. Tiptoes back to bedroom. Places head on pillow. Tweetdeck chirps heard. No way he's going back in there.
Have. To. Get To. Sleep.
“Yes, dear! Be right there! Yes, I know what time it is… I’m just checking a few emails…"E-mail links to Facebook. Then Twitter follower - who's he? Sermo notice. iMedExchange follower. Funny video on YouTube.
11:01pm: What the ...? Damn. They said THAT? Just a few words on the blog… Shouldn’t take too long…”
(Tweetdeck minimized. Blogger fired up...)
* click click click click click click clickity click …*
Midnight: “Takin' shape. Now, just need a tie up the piece with a linked references. ”
* click clickity click click click clickity click …*
12:20 am:
“Sorry, dear. Getting to bed now…"Darn it: can’t publish ‘til I spell-check it… But if I do that now…she’ll KILL me!....
"What’s that honey? Oh... yeah… Powering down now…”* click click click …*
Silence. Proofreading. Then:
“I can’t publish this! It's horrible! * sigh * I've got to look at this again in the morning.”
12:40 am: Windows are minimized, computer left on. Incandescent light extinguished. Tiptoes back to bedroom. Places head on pillow. Tweetdeck chirps heard. No way he's going back in there.
Have. To. Get To. Sleep.
"Did you forget we have to leave for the the track meet at 6:30?"-Wes
My Comment Moderation Delay
For those who have been kind enough to place comments on this blog, I apologize for not posting your comments sooner. It seems Google's Blogger is experiencing e-mail notification issues and it seems this blog is one so affected.
So rest assured, I'll try to post comments faster once the problem is resolved and I finish my next 5-hour atrial fibrillation ablation.
Thanks for your patience.
-Wes
So rest assured, I'll try to post comments faster once the problem is resolved and I finish my next 5-hour atrial fibrillation ablation.
Thanks for your patience.
-Wes
Wednesday, July 07, 2010
Disease Coalitions
In order to assure I avoid any potential for legal action against this blog, I will follow pre-specified rules for web-linking imposed by a particular disease coalition's sponsor that must be carefully followed... or else. Therefore, I will BOLD and HIGHLIGHT portions of this post that comply with these rules.
I don't watch TV much, but was invited to watch the double-episode of Fox's Hell's Kitchen with my son last evening. (Not that there would be any resemblance to my kitchen, mind you, but I guess if you like to watch lots of people smoke and swear and behave badly to each other in the name of cooking, then it's perfectly fun entertainment.)
Somewhere during the show, I was most struck by a commercial were two actors were in deep, staged conversation: one as a purported radio station deejay, and the other a very sincere doctor discussing how people with P.A.D. where twice as likely to die of heart attack or stroke. "Just another drug ad," I thought. "I wonder which drug company's spending this kind of money?"
So I waited until the end to see which company logo would appear, but instead, saw none. Instead, the name of a "coalition" appeared very briefly: The PAD Coalition, a subsidiary of The Vascular Disease Foundation. The Vascular Disease Foundation is a national non-profit organization whose mission is to help reduce disability and death from vascular disease that also sponsors the Venous Disease Coalition. The Vascular Disease Foundation is committed to improving health for all by reducing death and disability from vascular disease.
What a great idea!
I'm sure we'll be seeing coalitions in support of the heartbreak of psoriasis or scourge of acne any minute!
But, sorry, there are other rules that must be followed in the interest of teaching people about these entitites:
The Organization does not allow other Web sites to copy and reuse information or material(s) from its Web site unless otherwise permitted by a separate written agreement.So much for sharing. Sheesh.
Glad to know that Abbott, AstraSeneca, Bard Peripheral Vascular, Summit Doppler, Gore, Biomedics Vascular Solutions, BristolMyersSquibb, ev3 and so many others are so careful about what's said about P.A.D. that they can violate the The Vascular Disease Foundation's own "two click rule" that stipulates:
Any link from VDF’s Web site to an external Web site must abide by a two-click rule. This means that the first link goes to a "jump page" that explains the relationship between VDF and the other party.But then again, the "two-click rule" permits "one-click" from their site in certain circumstances:
A link to the external Web site can be placed on this jump page (editor's note: the jump page seems to be the PAD Coalition website's home page); however, it must land on a general homepage, not a page that includes information about specific products or services.So don't worry, rest assured these companies have no vested interest in making sure you know all about P.A.D. and it's relation to heart disease and stroke. They are unbiased, independent and have no interest in capturing more patients to use their medications and products but rather want you to know about these diseases just for your health and well-being.
... all without having to broach the unseemly topics like the costs of the screening procedures nor the risks of contrast nephropathy and peripheral artery interventional procedures.
-Wes
Tuesday, July 06, 2010
How Do Cardiologists Want to Get Paid?
According to the American College of Cardiology, here's what you get when you ask nearly 400 of 'em:
Of course the whole damn physician payment mess is complicated by a billing coding scheme that is so ridiculous, arbitrary, and insane that no matter which method you pick, it can be gamed to everyone's benefit except the patient. Get rid of THAT system and we might be able to talk about REAL physician payment reform.
How?
Pay ALL doctors, be they specialists or not, a fair, market-based hourly wage for work performed. That's ALL work: from the most mundane e-mail response or medication refill to the most time-consuming history-taking or complex neurosurgical procedure. Pay them time-and-a-quarter or time-and-a-half for after hours duty.
Since most of our legislature are lawyers, even they should understand this concept, right?
Imagine: no diagnosis codes, no procedure codes, no coding specialists, no 500,000 permutations and combinations of procedure codes that must match pre-determined and frequently varying diagnosis codes. If hospitals and government want to screw with that system - go for it - but keep the physician workforce separate from these coding shenanigans. Pay us what our time and intellectual capabilities are worth. Period.
And what might these hourly wages be?
That would have to be worked out based on training, years of practice, malpractice risk, board-certification, etc. But compared to the mess we have now, I'm betting this system would be a whole hell-of-a-lot more understandable and transparent than the monkey business we're doing now.
-Wes
Nearly two-thirds (63%) of cardiologists in private practices are currently compensated on a fee-for-service basis (FFS) exclusively; and, similarly, nearly two-thirds (65%) of these private practice cardiologists indicate that their ideal compensation is fee-for-service. Some of this response seems to be related to fear that doctors are due to be shafted regardless of what form of reimbursement is used. Therefore stick with the devil you know -- even if it is constantly declining.In my view, fee-for-service is effectively (and appropriately) on life-support and fading fast. Oh sure, "concierge" fees can make up a difference between medicare payments and drops in fees for a while in affluent areas, but these fees do nothing to address the very real needs for doctors in less affluent or rural health care delivery areas. On first blush, the market is moving to a health care system salary-based structure, but straight salaries do little to promote team collaboration nor reward exceptional personal effort. If productivity incentives are added to straight salary structures, there is a risk of promoting of even more testing to benefit the hospital (and hence employee-doctor's) bottom line at the expense of the patient or their insurer.
Conversely, more than three-fourths (78%) of the cardiologists who are not in private practice currently receive a salary as their primary source of income. However, interesting to note is that only 57% of these cardiologists state that a salary is their ideal form of compensation. Fee-for-service (19%) and a mixed compensation system (22%) actually gain strength among them for ideal compensation. This makes sense. Salaried cardiologists deserve incentives for productivity (everybody doesn’t work as hard) and quality (everybody doesn’t strive as effectively for better outcomes). Incentives have to be based on relevant data comparisons—not conjecture.
Of course the whole damn physician payment mess is complicated by a billing coding scheme that is so ridiculous, arbitrary, and insane that no matter which method you pick, it can be gamed to everyone's benefit except the patient. Get rid of THAT system and we might be able to talk about REAL physician payment reform.
How?
Pay ALL doctors, be they specialists or not, a fair, market-based hourly wage for work performed. That's ALL work: from the most mundane e-mail response or medication refill to the most time-consuming history-taking or complex neurosurgical procedure. Pay them time-and-a-quarter or time-and-a-half for after hours duty.
Since most of our legislature are lawyers, even they should understand this concept, right?
Imagine: no diagnosis codes, no procedure codes, no coding specialists, no 500,000 permutations and combinations of procedure codes that must match pre-determined and frequently varying diagnosis codes. If hospitals and government want to screw with that system - go for it - but keep the physician workforce separate from these coding shenanigans. Pay us what our time and intellectual capabilities are worth. Period.
And what might these hourly wages be?
That would have to be worked out based on training, years of practice, malpractice risk, board-certification, etc. But compared to the mess we have now, I'm betting this system would be a whole hell-of-a-lot more understandable and transparent than the monkey business we're doing now.
-Wes
Monday, July 05, 2010
On Kindness
Life has loveliness to sell,
All beautiful and splendid things,
Blue waves whitened on a cliff,
Soaring fire that sways and sings,
And children's faces looking up
Holding wonder like a cup.
Life has loveliness to sell,
Music like a curve of gold,
Scent of pine trees in the rain,
Eyes that love you, arms that hold,
And for your spirit's still delight,
Holy thoughts that star the night.
Spend all you have for loveliness,
Buy it and never count the cost;
For one white singing hour of peace
Count many a year of strife well lost,
And for a breath of ecstasy
Give all you have been, or could be.
- Sara Teasdale
Today I travel to a small town outside Chicago to help my mother with her move from an assisted living facility to Alabama so she can live with my sister. I suspect many people, thanks to current economic times, have realized that the savings that were supposed to be there are not and change must happen. Such is the case with my mother.
It is sure to be an emotional time, one which both of us had hoped to avoid. For her, she will be moving from the region of her childhood, her college, her marriage, her first home, her dream home, her caldron of first-grade student graduates and her dearest friends. For me, I will miss our spontaneous visits, morning coffee conversations, trips to the local restaurant in the town of my childhood, her gentle smile, and her helpful advice.
But this is not what I will miss the most.
For me, I will miss the single greatest gift she could ever give a son: her kindness.
Mothers have a way of doing that to sons. While fathers are busy hardening us to be strong, stalwart, disciplined, and driven, mothers do quite the opposite. For this son, she showed me quite a different side: the strength of flowers, the miraculous coordination of millipede’s legs, the gentle pattern of a monarch’s wings, the geometric and gustatory splendor of artichokes, and the importance of a tender word, a held door, a pleasant smile, and a tender touch. “The gift of giving is with the giver,” she would say. “Big things come in little packages.”
I would like to think it was my father who gave me the drive to become a doctor. And in some way, it probably was - we do things to please our parents, after all. But just to achieve the title of doctor is not enduring. My mother is the reason I stayed one.
“Treat every patient as though they were your mother.”
Exactly.

-Wes
Sunday, July 04, 2010
Happy July 4th!
Friday, July 02, 2010
Health Care's Road Rage
Road and constructions projects have stopped all over town thanks to concerns about future health care benefits:
Construction companies and labor unions are divided over health care packages. The unions seek a 15 percent annual benefits increase over three years, while contractors have countered with a 1 percent annual increase.-Wes
The Corporate Practice of Medicine
Two opposing views, one for the corporate practice of medicine:
How do we keep the patients' best interests at the forefront when doctors are increasingly becoming corporate employees?
-Wes
The trend toward hospital employment became a stampede on Jan. 1, when CMS enacted drastically reduced payments for in-office echocardiograms and nuclear stress tests, and eliminated codes for consultations. Even worse, MedPac, an influential panel advising Congress on Medicare, has recommended complete elimination of the in-office exemption for physician-owned imaging services. Payment for the technical as well as the professional component of echocardiograms and nuclear cardiology procedures performed in their offices has been a major source of revenue for independent cardiologists, who are faced with ever increasing overhead to pay for complex billing services, malpractice insurance and an electronic health record.... and one against the corporate practice of medicine:
As expenses continue to increase and revenues decline, it is little wonder than an estimated 50% to 75% of all cardiologists in the country will be hospital employees by the end of 2010, up from less than 25% just 5 years ago. According to MedAxiom, which recently surveyed 5,400 cardiologists in 300 practices, cardiologists who have become hospital employees have seen their incomes stabilize, or even increase slightly, while independent practitioners continue to experience a steady decline in income.
Economics aside, the transformation from independent practice to hospital employment can offer real advantages to both cardiologists and hospitals when both parties have developed a joint vision of care models and global care delivery paradigms, truly sharing responsibility for decision-making based both on what is best for individual patients and for the health care system as a whole. A continuing challenge in virtually all integrated practices is the fusion of a facility-centric model with a physician-centric model, sharing not just governance, but control of everyday activities.
Nearly everyone agrees that the quality of health care benefits from a team approach, with seamless exchange of electronic data, systematic monitoring of appropriate resource utilization and realistic measurement of the quality of care delivered using clinical rather than billing data.The current legislative, legal and regulatory environment favors initiatives from integrated systems of hospitals and employed physicians. It is more difficult for hospitals and non-employed physicians to collaborate in order to meet ongoing demands for increased quality and decreased costs of health care.
The bar against the corporate practice of medicine has been in place in California since 1938 and continues to protect patients from corporate entities exerting control over the delivery of medicine. When hospitals are allowed to hire and charge for physician services, a division of the physician’s loyalty to the patient can be created, commercial exploitation of medical care can occur, and lay control over a physician’s professional medical judgment can be exerted, each of which resulting in higher healthcare costs and — what is worse — diminished quality of care provided to patients in California.Other states have similar statutes barring the corporate practice of medicine, but in many states hospitals are exempted.
How do we keep the patients' best interests at the forefront when doctors are increasingly becoming corporate employees?
-Wes
Thursday, July 01, 2010
The Pool's Open!
It's summertime and the government's high risk insurance pool (made available by the recent passage of the health care reform bill ironically called the "Patient Protection and Affordable Care Act") opens today. Uninsurable people should jump on in if they can "afford" the hefty $400-$900 cost per month. Be sure to bring the whole family so they can help pay the bill, too!
You can learn about the specifics over at HealthCare.gov.
While the need for the uninsured to obtain insurance exists, the opening of this insurance "pool" provides another stark reminder of how the health care reform bill was railroaded through Congress with waves of magic wands and unrealistics promises of cost controls:
Oh, and one more thing. That low price quoted above for monthly premiums? That doesn't include the $5000 deductible you'll have to pay to get that low price in Illinois. Not happy with this? You can find your rate at Illinois' Premium Rate Calculator.
-Wes
You can learn about the specifics over at HealthCare.gov.
While the need for the uninsured to obtain insurance exists, the opening of this insurance "pool" provides another stark reminder of how the health care reform bill was railroaded through Congress with waves of magic wands and unrealistics promises of cost controls:
The biggest question hanging over the program is whether the $5 billion allocated will be enough.It is now very clear that this bill, shoved through without critical review, is going to cost America a whole lot more than CBO's estimated $940 billion dollars.
Millions of people meet the basic qualifications for coverage, and technical experts who advise Congress and the administration have warned the funds could be exhausted as early as the end of 2011.
HHS officials sidestepped questions about what would happen if the money runs out. One option is for the government to limit enrollment. (Emphasis mine.)
Popper estimated about 200,000 people would be enrolled in the program at any one time, but other HHS experts estimated that 375,000 would sign up this year, and the Congressional Budget Office says the total could reach 700,000 in 2013.
Oh, and one more thing. That low price quoted above for monthly premiums? That doesn't include the $5000 deductible you'll have to pay to get that low price in Illinois. Not happy with this? You can find your rate at Illinois' Premium Rate Calculator.
-Wes
Your Doctor, the Insurance Broker
Call it sweet, delicious vindication.
It was clinic day yesterday. No longer had I completed my rant in this blog about UnitedHealthcare's program to require all cardiac elecrophysiologists to obtain a "notification number" before performing any pacemaker or defibrillator procedure, I discovered my letter from them dated 3 June 2010 on my desk stating that this requirement will begin 1 September 2010 for all Illinois electrophysiologists for "all electrophysiology procedures."
Not longer than an hour later, I was seeing a 67 year old patient in clinic who asked me, "I just got my Medicare (Part A) card and must decide about which insurer I should use for Part B, C, D, E, and F," he said jokingly. "Since I have the medical problem and might need some care in the future, is there any company you would recomend?"
I sat stunned, relishing my ever-so-brief, influential role. I told showed him UnitedHealthcare's letter.
"I'd avoid UnitedHealthcare," I found myself saying, "...and any other front man like AARP that peddles their supplemental insurance products and drains value from your policy."
My new role: insurance broker.
-Wes
It was clinic day yesterday. No longer had I completed my rant in this blog about UnitedHealthcare's program to require all cardiac elecrophysiologists to obtain a "notification number" before performing any pacemaker or defibrillator procedure, I discovered my letter from them dated 3 June 2010 on my desk stating that this requirement will begin 1 September 2010 for all Illinois electrophysiologists for "all electrophysiology procedures."
Not longer than an hour later, I was seeing a 67 year old patient in clinic who asked me, "I just got my Medicare (Part A) card and must decide about which insurer I should use for Part B, C, D, E, and F," he said jokingly. "Since I have the medical problem and might need some care in the future, is there any company you would recomend?"
I sat stunned, relishing my ever-so-brief, influential role. I told showed him UnitedHealthcare's letter.
"I'd avoid UnitedHealthcare," I found myself saying, "...and any other front man like AARP that peddles their supplemental insurance products and drains value from your policy."
My new role: insurance broker.
-Wes




